Abstract
Purpose
This pragmatic clinical study aimed to assess goal attainment among patients with schizophrenia treated with paliperidone palmitate 3-monthly (PP3M) and its relation to their level of disability, and whether patients achieved symptomatic remission at the study endpoint.
Patients and Methods
Goal attainment was assessed as a secondary endpoint using Goal Attainment Scaling (GAS) within a 52-week, prospective, single-arm, non-randomized, open-label, international, multicenter study evaluating the impact of transitioning stable patients with schizophrenia from paliperidone palmitate 1-monthly (PP1M) to PP3M. Additional exploratory analyses were performed to investigate the relationship between disability and functioning as measured by the World Health Organization Disability Assessment Schedule (WHODAS), Version 2.0, symptomatic remission, and goal attainment.
Results
Overall, 305 patients were enrolled, of whom 281 (92.1%) provided GAS data at baseline. Of these, 160 achieved symptomatic remission at the last observation carried forward (LOCF) endpoint. The most common category of goals was “self” related, of which work-related was most frequent. Two-thirds of patients (67.7%) achieved at least one goal at the LOCF endpoint. Goal achievement was positively associated with lower baseline symptoms and symptomatic remission at LOCF endpoint, and with lower WHODAS scores at baseline and LOCF endpoint and greater WHODAS score improvements from baseline. Age, duration of disease, and duration of PP1M treatment before the switch did not impact goal setting and goal attainment. The proportion of patients with remunerated work status increased by 11.3% at LOCF endpoint.
Conclusion
The results of this secondary endpoint analysis indicate that continued treatment of patients with schizophrenia with PP3M following stabilization with PP1M may facilitate attainment of patients’ personal goals and reduce disability, especially, but not exclusively, in patients with symptomatic remission achieved at LOCF.
Keywords: GAS, goal attainment, paliperidone palmitate 1-monthly formulation, paliperidone palmitate 3-monthly formulation, schizophrenia, WHODAS
Introduction
Schizophrenia is a progressive disease that worsens with each relapse, leading to substantial patient burden, from impairment of personal and social functioning and related unemployment to increased mortality.1–4 Achieving both symptomatic and functional remission is important for recovery and attaining patient goals.5–8
Goal setting is a routine component of rehabilitation and multidisciplinary approaches to clinical care, with proven utility as part of the communication and decision-making process, and as a person-centered outcome measure for rehabilitation.9–11 Defining patient goals helps to clarify individual priorities, which is key to both effective clinical management and establishing and maintaining patient engagement, satisfaction, and treatment adherence.12 Goal setting and attainment improve quality of life; have been linked with essential elements of recovery, such as hope, responsibility, meaning, and personal identity; and can increase patient autonomy, empowerment, and confidence.11
Second generation long-acting injectable antipsychotic treatments (LATs) overcome the need for people with schizophrenia to take daily oral antipsychotic medication and are a valuable option to improve treatment continuation and thereby patient outcomes.13 Improved clinical outcomes, such as fewer relapses, hospitalizations, and visits to the emergency room,14,15 with LATs compared with oral antipsychotics may significantly lower patients’ stress and disease burden and increase perceived normality.13 Further, the reduced need for daily monitoring of adherence to antipsychotic treatment allows for a greater focus on the patient’s personal goals, reduced disputes between patients and carers, and greater potential involvement in daily activities.13
Paliperidone palmitate 3-monthly (PP3M) is a LAT formulation approved in many countries, including the USA and Europe, for the maintenance treatment of adults with schizophrenia stabilized with the paliperidone palmitate 1-monthly (PP1M) formulation (EMA). PP3M is the only LAT to be administered 3-monthly, therefore offering greater convenience than other LATs.16 PP3M has demonstrated favorable efficacy and safety in the treatment of schizophrenia in two pivotal, randomized controlled trials.17,18 An increasing body of real-world evidence for PP3M is now available to supplement randomized clinical trial data.19–21 However, there is limited information specifically assessing how 3-monthly administration of antipsychotic medication might enable patients with schizophrenia to achieve their goals and how it could impact their level of disability and functioning.
Garcia-Portilla et al (2020) evaluated the efficacy and safety of switching patients from PP1M to PP3M for 52 weeks in a pragmatic clinical setting.22 The study enrolled adult patients with schizophrenia who were stable at baseline on PP1M. The primary efficacy endpoint, symptomatic remission at last observation carried forward (LOCF) endpoint, was defined according to Andreasen et al (2005) as a score of mild or less (ie, ≤3) on all selected Positive and Negative Syndrome Scale (PANSS) items (P1, P2, P3, N1, N4, N6, G5, and G9), maintained for at least 6 months. The primary results of this study have been published previously.22 Overall, 56.8% of patients (95% confidence interval [CI]: 51.0, 62.4) achieved symptomatic remission, and 31.8% achieved both symptomatic and functional remission (Personal and Social Performance scale total score >70) at LOCF endpoint.22 The completion rate of 95.4% is one of the highest observed for a 1-year real-world study in schizophrenia.22
In this publication, we assess so far unpublished secondary and exploratory outcomes of this study to establish whether continued treatment with PP3M might positively impact the quality of goal setting, help patients to achieve their goals, and reduce disability. We also assess how these outcomes are impacted by achievement of symptomatic remission.
Patients and Methods
This prospective, phase 3b, single-arm, open-label study in patients with schizophrenia switched from PP1M to PP3M in clinical practice was conducted between May 2016 and March 2018 at 57 sites across Europe, the Middle East, Africa, and the Asia-Pacific region (ClinicalTrials.gov identifier NCT02713282; EudraCT number 2015–004835-10; REMISSIO). Full details of the study methods are presented elsewhere22 and are only briefly reported here. The study protocol and amendments underwent ethics review at each site. The full list of all sites involved in the study and their respective institutional review boards and ethics committees can be found in the supplementary material (Table S1). The study was conducted in compliance with the Declaration of Helsinki and was consistent with Good Clinical Practice and applicable regulatory requirements. Written informed consent was obtained from all patients before enrollment.
Patients and Treatments
Adults aged 18–50 years with a diagnosis of schizophrenia (Diagnostic and Statistical Manual of Mental Disorders, 5th ed.23) were included in the study if they were adequately treated with PP1M for at least 4 months (with two identical doses before switching), had a PANSS total score less than 70 points, and were considered likely to benefit from treatment with PP3M according to the investigator, based on tolerability (lack of intolerable side effects) and clinical response (defined as PANSS total score <70 at screening) to pre-study treatment with PP1M. Following a 7-day screening period, patients were converted from PP1M to PP3M in line with the prescribing information24 and then entered a 52-week, flexible-dose treatment period.
Assessments
Goal Attainment Scaling (GAS)25 was used to evaluate the extent to which the patient’s individual goals were achieved during the course of the study. Before the first PP3M administration, each patient (together with the investigator and in some cases a carer) set up to three personal goals. Importantly, the GAS procedure includes “a priori” establishment of criteria for a “successful” outcome,26 which was also agreed with the patient at the start of this study. For the purpose of this analysis, patient goals were translated from their local language to English. Using Jose et al (2015),6 the authors reviewed and grouped the patient goals into four general categories: family (eg, relationships, responsibility, and social life), illness (eg, symptoms and functioning), self (eg, self-acceptance/control, soft skills, managing self, leading a meaningful life), and social (eg, connectedness, inclusion, communication, leadership role).
Each goal was rated at baseline for importance, difficulty of achieving, and baseline function. Goal attainment was evaluated until the goals were either achieved or the study finished (at Month 6, and if relevant, at Month 12 or early withdrawal). Each goal was scored on a 5-point scale, recording the degree of achievement for each goal area. The scale ranged from −2 (much less than expected) to +2 (much better than expected), with goals rated 0 if the patient achieved the expected level. At baseline, goals were typically scored as −1, unless patients were as bad as they could possibly be in that goal area, in which case they were scored −2.
Each goal was also weighted according to its importance and difficulty. All goals were then incorporated into a single GAS total score per patient, calculated using the published formula [Kiresuk and Sherman 1968],25 thus providing a standardized measure of goal attainment. Increases in GAS scores from baseline represent improvement in goal attainment.
Change in disability was assessed using the World Health Organization Disability Assessment Schedule (WHODAS), Version 2.0, a standardized measurement of health and disability across cultures.27 WHODAS captures the patient’s functioning in six domains of life: 1. cognition (understanding and communicating), 2. mobility (moving and getting around), 3. self-care (attending to one’s hygiene, dressing, eating, and staying alone), 4. getting along (interacting with other people), 5. life activities (domestic responsibilities, leisure, work, and school), and 6. participation (joining in community activities, participating in society).27 In this study, the full version of WHODAS, consisting of 36 questions across the six domains,27 was administered by an investigator at baseline and at Months 6 and 12, using a recall period of the previous 30 days. Decreases in WHODAS scores from baseline represent improvement.
Statistical Analysis
The modified intention-to-treat efficacy and safety analysis sets comprised all patients who provided written consent and received at least one dose of PP3M during the 52-week treatment period, and who had at least one post-baseline efficacy or safety assessment, respectively.
LOCF endpoint analysis was performed in addition to observed case analysis. No testing of predefined hypotheses was performed and there was no adjustment for multiplicity. Descriptive statistics are presented including 95% confidence intervals (CI) as estimates of effect or association for efficacy endpoints. Significant effects are suggested if, for instance, the 95% CI of a change from baseline does not include zero within the interval, or if the 95% CIs of the mean values in two groups do not overlap. Spearman’s rank correlation was used to investigate the relationship between GAS scores and variables relating to functioning, demographics, and clinical parameters. Explorative stepwise logistic regression analysis was performed to investigate the association of relevant factors with goal attainment.
Data from GAS and WHODAS 2.0 were analyzed for the total population and in subgroups of those who did and did not achieve symptomatic remission at LOCF endpoint.
Results
Baseline Characteristics
In total, 305 patients were enrolled and received PP3M, of whom 291 (95.4%) completed the 12-month study. Approximately two-thirds of patients (65.6%) were male; the mean (standard deviation [SD]) age was 36.5 (8.0) years and the mean (SD) time since first diagnosis of schizophrenia was 9.2 (7.3) years.22 Prior to treatment with PP3M, 77.4% of patients had been treated with PP1M for more than 6 months, 19.0% for 4–6 months, and 3.6% had an undefined PP1M duration of at least 4 months.
Goal Setting
Goal Setting at Baseline
GAS was obtained for 281 patients at baseline (92.1% of the total group [N=305]). Most patients (73.0%, n=205) set one goal, and equal proportions set two or three goals (13.5%, n=38 for each). Of the 281 patients with baseline GAS data, 160 achieved symptomatic remission according to the Andreasen criteria at LOCF endpoint. Similar proportions of patients who did and did not achieve symptomatic remission at LOCF endpoint set one (73.8% and 71.9%), two (12.5% and 14.9%), or three goals (13.8% and 13.2%).
The mean (SD) GAS score at baseline was 37.0 (4.2) in the total group (Table 1) with no difference between the subgroups who did or did not reach symptomatic remission at LOCF endpoint. Overall, for most goals (79.7%), there was some baseline functioning (score of −1); for a minority of the goals (20.3%), there was no functioning at baseline (score of −2).
Table 1.
Mean (SD) GAS Score at Baseline and LOCF Endpoint, Overall Mean Goal Importance Score, Mean Difficulty Score and Functioning at Baseline for the Total Population, and for Patients with and without Symptomatic Remission at LOCF Endpoint
| Total Group (N=303) | Symptomatic Remission at LOCF Endpoint | ||
|---|---|---|---|
| Yes (n=172) | No (n=131) | ||
| Baseline GAS score | |||
| N | 248 | 143 | 105 |
| Mean (SD) | 37.0 (4.2) | 37.2 (4.2) | 36.7 (4.3) |
| 95% CI | 36.4, 37.5 | 36.5, 37.8 | 35.9, 37.6 |
| LOCF endpoint | |||
| N | 248 | 143 | 105 |
| Mean (SD) | 53.8 (8.0) | 54.9 (8.0) | 52.2 (7.6) |
| 95% CI | 52.8, 54.8 | 53.6, 56.3 | 50.8, 53.7 |
| Change from baseline to LOCF endpoint | |||
| N | 248 | 143 | 105 |
| Mean (SD) | 16.8 (9.0) | 17.8 (8.4) | 15.5 (8.6) |
| 95% CI | 15.8, 17.9 | 16.4, 19.2 | 13.9, 17.2 |
| Overall mean goal importance score at baseline | |||
| N | 281 | 160 | 121 |
| Mean (SD) | 1.5 (0.6) | 1.5 (0.6) | 1.6 (0.6) |
| 95% CI | 1.5, 1.6 | 1.4, 1.6 | 1.5, 1.7 |
| Mean difficulty score at patient level, including goals with difficulty=0 | |||
| N | 281 | 160 | 121 |
| Mean (SD) | 1.5 (0.7) | 1.4 (0.7) | 1.53 (0.8) |
| 95% CI | 1.4, 1.6 | 1.3, 1.5 | 1.4, 1.7 |
| Patients with one or more goal with baseline=no function, n (%) | |||
| N | 202 (71.9) | 119 (74.4) | 83 (68.6) |
| Y | 79 (28.1) | 41 (25.6) | 38 (31.4) |
Notes: Each goal was rated for importance (1=important, 2=very important, 3=extremely important), difficulty of achieving (0=not difficult, 1=minor difficulty, 2=moderate difficulty, 3=extreme difficulty), and baseline function (−1=some function, −2=no function, “as bad as can be”). At Months 6 and 12, attainment Yes or No was recorded, and level of attainment was scored on an ordinal scale from +2 (much better than expected) to −2 (much worse than expected). A standardized overall GAS score was calculated by combining weighted (for importance and difficulty) goals with baseline function (for baseline GAS score) or with attainment level (for follow-up GAS scores).26 Goals were evaluated until they were either achieved or the study finished.
Abbreviations: CI, confidence interval; GAS, Goal Attainment Scaling; LOCF, last observation carried forward; SD, standard deviation.
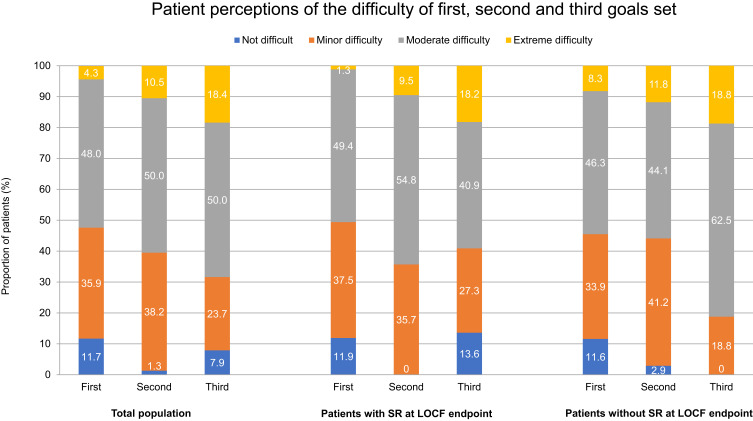
As each patient could set up to three goals, a comparison of the first, second and, third set goals was performed to assess any observable differences in the baseline functioning, difficulty, and importance of the goals by the order in which they were set. No difference was identified in the baseline functioning or the importance of the goals by order, while a trend was observed towards progressive difficulty from first to third goal (Figure 1). In order to limit a potential bias due to this trend and to ensure a sizable group for analysis, data are presented in the current manuscript on the first goal set, representing all patients who set at least one goal, unless indicated otherwise.
Figure 1.
Patient perceptions at baseline of the difficulty of their first, second, and third goals for the total population (N=281) and among patients with (n=160) and without (n=121) symptomatic remission at LOCF endpoint.
Abbreviation: LOCF, last observation carried forward; SR, symptomatic remission.
Baseline functioning for first goals was similar regardless of symptomatic remission at LOCF endpoint (81.2% of patients who achieved remission and 77.7% of patients who did not achieve remission had some functioning at baseline). Just under half of patients who set at least one goal ranked them as “very” or “extremely” important; this was consistent across patients who did and did not achieve symptomatic remission at LOCF endpoint. Likewise, 52.3% of patients ranked the goal as “moderately” or “extremely” difficult, with somewhat higher perceived difficulty in the subgroup without symptomatic remission at LOCF compared with those with symptomatic remission at LOCF endpoint (Figure 1).
Categories of Goals Set
Across all goals set, most were categorized by the authors as “self” related (68.7%); this was consistent across both sexes, although numerically slightly more goals categorized as “self” were set by men than women (73.8% vs 62.5%); 17.7% of goals were categorized as “social” and 10.3% as “family-related”. Notably, there was a low rate of “illness-related” goals (3.3%). More than twice as many “family goals” were set by women than men (16.3% vs 7.1%); however, small subgroups resulted in wide overlapping 95% CIs (8.9, 26.2 vs 3.7, 12.1). For the first goals set, those categorized as ’self’ goals were most frequently related to work (45.4%); others were related to diet and lifestyle (23.6%), other life skills (17.8%), and education (13.2%). Example goals are presented in Table S2.
Social and family goals were of greatest importance to patients, with each rated as “very” or “extremely” important by over half of respondents (Table S3). Family goals were most likely to be rated as “extremely important” (21.6%), compared with self (10.1%), illness (8.3%), and social goals (3.1%). Across all categories, slightly more than half of goals were considered moderately difficult; however, numerically, social goals were more likely to be considered extremely difficult than other categories (12.5% vs 0.0–6.5%, respectively).
Goal Attainment
Post-baseline GAS scores were obtained for 248 patients (143 who achieved symptomatic remission and 105 who did not), of whom the majority (67.7%) achieved at least one goal at LOCF endpoint.
A significantly higher proportion of patients with symptomatic remission (vs those without) at LOCF endpoint achieved at least one goal: 75.5% vs 57.1%, respectively, as suggested by non-overlapping 95% CIs (67.6, 82.3 vs 47.1, 66.8).
Of patients who achieved both symptomatic remission and functional remission (Personal and Social Performance scale total score >70) at LOCF endpoint, 80.8% achieved at least one goal, a significant difference compared with 62.3% of patients who did not achieve both symptomatic and functional remission at LOCF endpoint (95% CIs: 69.9, 89.1 vs 54.7, 69.5).
At LOCF endpoint, mean GAS (95% CI) score increased significantly by 16.8 points (15.8, 17.9) to 53.8 (52.8, 54.8; Table 1). In patients with and without symptomatic remission at LOCF endpoint, mean GAS scores were similar at baseline and LOCF endpoint (Table 1), and increased significantly from baseline in both subgroups.
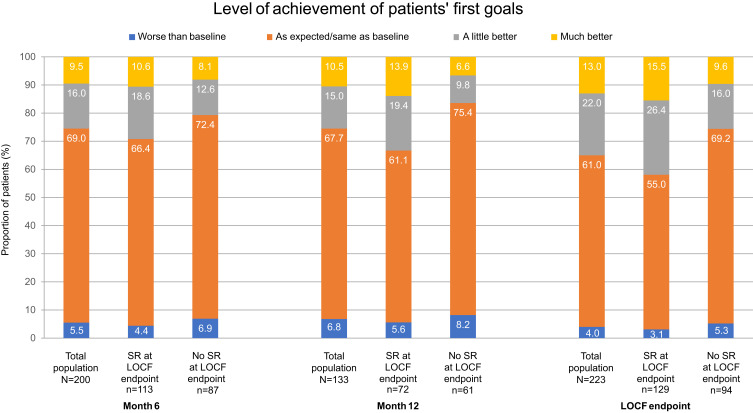
More than one-third of patients (35.0%) who achieved their first goal scored their level of achievement as “a little” or “much” better at LOCF endpoint, with the majority achieving as expected (61.0%); only 4.0% scored “worse” than planned (Figure 2).
Figure 2.
Level of goal achievement for first goals at Month 6, Month 12, and LOCF endpoint for the total population and among patients with and without symptomatic remission at LOCF endpoint.
Abbreviation: LOCF, last observation carried forward; SR, symptomatic remission.
Of all reported goals, achievement was highest for family goals: almost three-quarters of family goals set (72.2%) were achieved at LOCF endpoint, compared with around half of illness (54.6%), self (55.0%), and social goals (52.4%).
Among the first goals set in the self category, around half of those related to work, diet and lifestyle, education, and other life skills were achieved (53.1%, 53.7%, 52.2%, and 61.3%, respectively). In patients who did and did not achieve symptomatic remission at LOCF endpoint, comparable proportions of goals relating to work (56.0% and 48.2%, respectively) and other life skills (64.7% and 57.1%, respectively) were achieved. Conversely, patients who achieved symptomatic remission achieved higher proportions of goals relating to lifestyle and education (66.6% and 75.0%, respectively) compared with patients who did not achieve symptomatic remission (28.5% and 27.3%, respectively).
WHODAS
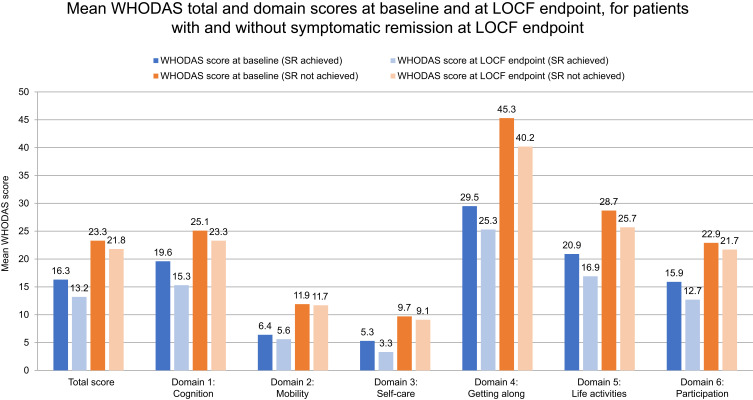
The mean (SD) WHODAS total score at baseline was 19.4 (14.7), reflecting an overall mild level of disability; at LOCF endpoint, it decreased by 2.4 (95% CI: −3.9, −0.9) points, indicating a significant reduction in disability with marginal clinical relevance. At baseline, the highest functioning (indicated by the lowest WHODAS scores) was seen for mobility (domain 2) and self-care (domain 3), and the lowest functioning was seen for getting along (domain 4). Mean changes from baseline at LOCF endpoint in cognition, getting along, life activities, and participation scores ranged from −2.3 to −3.9, representing improvements from baseline domain scores of around 11% to 15% at LOCF endpoint. Although mean changes from baseline at LOCF endpoint were lower for mobility and self-care scores (−0.5 and −1.4 points), due to the low baseline self-care score, this represented a 20% improvement in self-care from baseline at LOCF endpoint.
Patients who achieved symptomatic remission at LOCF endpoint had better mean WHODAS total and domain scores at both baseline and LOCF endpoint, and demonstrated larger numerical improvements in scores from baseline, compared with those who did not achieve symptomatic remission (Figure 3). In the total group, change in WHODAS score from baseline to LOCF endpoint was significant in the cognition, getting along, life activities, and participation domains. For patients who achieved symptomatic remission, change in WHODAS score from baseline to LOCF endpoint was significant in the cognition, self-care, getting along, life skills, and participation domains. Change in WHODAS score was not significant for any domain for patients who did not achieve symptomatic remission.
Figure 3.
Mean WHODAS scores at baseline and at LOCF endpoint for total score and each of the six WHODAS domains for patients with and without symptomatic remission at LOCF endpoint.
Notes: Each item was rated on a 5-point Likert scale (0=no difficulty, 1=mild difficulty, 2=moderate difficulty, 3=severe difficulty, 4=extreme difficulty, or cannot do). These results were used to generate scores across the six domains and to calculate an overall score, with scores ranging from 0 to 100 (higher scores indicating worse disability).
Abbreviations: LOCF, last observation carried forward; SR, symptomatic remission; WHODAS, World Health Organization Disability Assessment Schedule.
In line with the achievement of work-related self goals, in the total group, 11.3% of patients had an improvement in remunerated work status at LOCF endpoint (ie, from “no” at baseline to “yes” at LOCF endpoint), with the proportion of patients in the subgroup with symptomatic remission at LOCF endpoint more than twice as high as that in the subgroup without symptomatic remission at LOCF endpoint (15.2 vs 6.3%, respectively).
Relationship Between WHODAS Scores and Goal Achievement
Spearman correlation was used to examine correlations between goal achievement and WHODAS scores. Patients who had achieved at least one goal by Month 12 had significantly lower WHODAS total scores, and cognition and life activities domain scores at the respective time points, compared with patients who had not achieved at least one goal. WHODAS total and domain scores were numerically lower in patients who achieved at least one goal by Month 6, compared with those who did not. Conversely, for patients with data available, those who did not achieve a goal by Month 6 but who achieved at least one goal by Month 12 had significantly lower WHODAS total scores compared with patients who achieved no goals by Month 12 (mean [95% CI] 14.0 [10.8, 17.1] vs 21.9 [18.6, 25.3]). Similar significant differences were observed for patients who had achieved at least one goal at Month 12 vs those who had not for WHODAS cognition (14.5 [11.2, 17.8] vs 25.7 [21.7, 29.8]), and life activities domain scores (16.4 [11.8, 20.9] vs 28.6 [23.3, 33.9]).
For patients who achieved at least one goal, improvements from baseline were seen in WHODAS total score and all domains at both time points. These improvements were statistically significant for total score and all domains except mobility (at Months 6 and 12) and life activities (at Month 6). At Month 6, patients who had not achieved at least one goal demonstrated a significant improvement in the cognition domain only (mean [95% CI] −3.1 [−6.1, −0.2]). At Month 12, patients who had not achieved at least one goal showed no improvement in WHODAS total score, and non-significant improvements in the getting along and participation domains only.
Goal achievement and symptomatic remission were consistently associated with low WHODAS scores (Figure S1) in line with expectations. At Month 6, for the WHODAS total score, life activities, and participation domains, patients who had achieved symptomatic remission and at least one goal had significantly lower (better) WHODAS scores than patients who did not achieve symptomatic remission or any goals. For the participation domain, patients who had achieved symptomatic remission and at least one goal also had significantly lower scores than patients who did not achieve symptomatic remission but did achieve at least one goal. At both Month 12 and LOCF endpoint, patients who had achieved symptomatic remission and at least one goal had significantly lower total score and all domain scores than patients who did not achieve symptomatic remission or any goals, and had significantly lower scores for the life activities domain compared with patients who did achieve symptomatic remission but did not achieve any goals.
Explorative Multivariate Analysis of Goal Setting and Attainment
A stepwise logistic regression analysis was performed to investigate the effect of relevant factors on the achievement of at least one goal. Investigated factors were demographic and disease characteristics, clinical and functional effectiveness endpoints and their interactions.
Only two factors showed some effect. Higher PANSS general score at baseline had lower odds for achieving at least one goal at LOCF endpoint (odds ratio [OR]=0.897, [95% CI] 0.845, 0.952). In addition, patients with less improvement on PANSS general score from baseline to LOCF endpoint had lower odds of achieving at least one goal at LOCF endpoint (OR=0.878, [95% CI] 0.821, 0.940). Age, duration of disease, and duration of PP1M treatment did not appear to have an impact on goal setting or on goal attainment.
Discussion
This analysis assessed the impact of transitioning stable patients with schizophrenia from PP1M to PP3M on goal attainment and disability in a pragmatic clinical setting. Helping patients to set personal goals is an important strategy for improving patient engagement with treating and managing their schizophrenia.11,12 This may help patients to feel more involved in their treatment and more receptive to considering different treatment options.11,12,28 Initiating such discussions is particularly important given that many clinicians may overestimate patients’ concerns around LATs, anticipating resistance to the administration by injection.29,30 These preconceptions can impede shared decision-making, an approach with the potential to increase adherence31 and ultimately improve treatment outcomes.32,33
The large proportion of patients (281 patients; 92.1%) with GAS scoring available at baseline in this study demonstrates that patients are willing and able to set relevant goals as part of their treatment, thereby highlighting the importance of asking patients about their goals in routine clinical practice.
In the current study, the goals set by patients were reviewed and grouped by the authors into four broad categories – family, illness, self, and social – based on the categorization of themes derived from perception of recovery as an outcome by people with schizophrenia.6 Most goals set by both male and female patients related to the “self” category, of which almost half were work-related, which is consistent with previous studies showing that people with schizophrenia view self-management, improvement, and functioning as the most important aspects of recovery.6 Very few patients set illness goals, which might suggest that, in stable patients with mild or moderate symptomatology, the focus of the patients shifts towards goals beyond the illness.
Approximately half of all patients considered set goal(s) to be very or extremely important (45.6%) but acknowledged that these goals would be moderately or extremely difficult to achieve (52.3%). Social and family goals were considered most important (rated “very” or “extremely” important), and social goals were considered most difficult. As treatment goals can often differ between patients and physicians,34 it is important for healthcare professionals to ask the patient about their goals, particularly those relating to self-efficacy and family and societal performance, to clarify individual priorities within a person-centered approach.12
In the current study, most patients (67.7%) achieved at least one goal at LOCF endpoint, with GAS scores increasing. Numerically more patients with symptomatic remission at LOCF endpoint achieved at least one goal than those without symptomatic remission (not statistically evaluated); however, both groups achieved statistically significant changes in mean GAS scores from baseline. This was an unexpected outcome as a relationship between symptom severity and GAS was presumed. The fact that GAS scores improved for patients both with and without symptomatic remission suggests that these variables may evolve independently in patients with schizophrenia. Symptom remission and clinical stability are separate concepts. In our sample, patients with schizophrenia were clinically stable (ie, were not in an acute phase of the disease); however, not all patients had achieved symptomatic remission based on the two criteria by Andreasen et al by the end of the study. This suggests that the impact of PP3M on goal attainment occurs independently of symptom response to the treatment.
The achievement of goals that are considered important to the patient may have a considerable impact on patients’ quality of life, and working towards and achieving personal goals give patients autonomy, helps them to gain control of their lives, and provides a sense of meaning.11 Such improvements in life context and well-being have a reinforcing effect, further promoting additional progress.9 In addition, goal achievement may improve patient satisfaction with treatment and positively impact the likelihood of patients remaining on treatment, which, in turn, will help to further improve outcomes.12
Baseline WHODAS score (mean [SD], 19.4 [14.7]) indicated that patients had mild disability before transitioning from PP1M to PP3M. This reflects the stable status of patients receiving PP1M and may suggest that improvements in disability likely already occurred with PP1M treatment; however, measuring this was outside the scope of the current study. The overall improvement in WHODAS scores of 2.4 points at LOCF endpoint, although statistically significant, was of marginal clinical relevance. The low effect size, however, could also be attributed to the mild baseline disability.
Clinical trials with antipsychotic drugs in patients with acute schizophrenia have demonstrated a close relationship between functional improvement and symptom remission.35 A large proportion of the improvement tends to occur during the first weeks of treatment, followed by a slower rate of change. In our study, most patients had already been treated with the same active ingredient (PP1M) for several months prior to initiating PP3M (77.4% of patients received PP1M for more than 6 months prior to initiating PP3M). Furthermore, most patients were not participating in a structured psychiatric rehabilitation program, yet we found a small improvement in WHODAS, suggesting that long-term treatment with PP3M may improve functional outcomes. It is possible that a combination of psychiatric rehabilitation techniques and long-term treatment with PP3M may boost the impact on functionality. Patients who achieved symptomatic remission at LOCF endpoint not only had lower mean baseline WHODAS total and domain scores than patients who did not achieve symptomatic remission (indicating better baseline functioning) but also had greater numerical improvement in WHODAS from baseline to LOCF endpoint. Further, there was a notable positive relationship between goal attainment, better WHODAS scores, and achieving symptomatic remission. Following switching to PP3M, the greatest improvements were seen in the WHODAS cognition, getting along, and life activities domains. This indicates improvement in key skills that are necessary to achieve the types of goals frequently set by patients, including the ability to learn, concentrate, and communicate; and to complete household and work/school responsibilities. When combined with symptomatic remission, this may facilitate goal achievement.
In general, fewer than 20–30% of people with schizophrenia are employed.36–40 In the current study, most self goals were work-related, suggesting that this patient population are highly motivated to find and maintain employment. Around half of the work-related goals in this study were achieved; moreover, at LOCF endpoint, 11.3% of patients gained remunerated work, with more than double the number of patients with symptomatic remission than without symptomatic remission at LOCF endpoint achieving it. Gaining employment is a central concept to recovery from mental illness and is important for patients with schizophrenia.38,41–45 Work has been linked to modest clinical improvements in people with mental illness, including better social functioning, self-esteem, and quality of life, and reduced symptom severity.36,38 It also has a positive impact on leisure activities.41
This study demonstrated that stable patients experience multiple benefits following 1 year of treatment with PP3M after switching from PP1M. The 95.4% completion rate of this study is one of the highest observed for a 1-year real-world study in schizophrenia.22 Longer-term, continuous, uninterrupted treatment with LATs is associated with numerous patient benefits compared with oral antipsychotics, including reduced risk of relapse and hospitalization and improved overall survival.15,46,47 It may therefore be likely that the benefits of reduced frequency of LAT administration observed in the current study translate to longer-term benefits for patients. Further study is warranted to explore this.
Study Limitations
The primary limitation of this study was that it is a single treatment arm, uncontrolled, open-label study, so did not allow for a direct head-to-head comparison of changes in goal attainment for PP3M vs PP1M. The external validity of the study may be limited because patients were stabilized on PP1M before entering the study and thus had a relatively low level of disability. Furthermore, patients with major comorbid psychiatric and severe substance use disorders were excluded from the study. Given that these conditions can impact goal attainment, the study results may not be applicable to this patient group. Unfortunately, we could not assess sustained attainment or loss of attainment from Month 6 to Month 12 because goals that were achieved at Month 6 were not reassessed at Month 12 according to the protocol.
Assessing disability in patients with schizophrenia is fraught with difficulty.48 In the current study, we used the WHODAS 2.0 scale. When used in patients with schizophrenia, WHODAS 2.0 identifies disability compared with healthy populations, and results from WHODAS 2.0 have been consistent with those from other measures of disability or health status, or with clinician and proxy ratings.48–50 WHODAS 2.0 is, however, a tool that relies on the study participants to self-report on the severity of their disability. Cognitive deficits and limited insight often associated with schizophrenia may limit the reliability of self-reported data in this patient population.48 Moreover, WHODAS 2.0 has been found to be sensitive to the severity of depressive symptoms,48 which are commonly experienced by people with schizophrenia and are known to be associated with worse functioning and lower levels of well-being.51–53 Given this strong link between WHODAS 2.0 scores and the severity of depressive symptoms, it may not be entirely clear whether WHODAS 2.0 is a measure of disability or of depression.
Conclusions
In this secondary analysis assessing goal attainment in stable patients switched from PP1M to PP3M, two-thirds of patients achieved their goals at LOCF endpoint. Goals were most commonly related to self, with work as a key theme, and with an increased proportion of patients in work at the study end. Goal achievement was positively associated with achieving symptomatic remission, reduced disability and improved functioning. Transitioning patients to LATs that require less frequent administration may help patients to meet their goals and engage in desirable normal life activities.
Acknowledgments
Results from this study were previously presented in part at the European College of Neuropsychopharmacology congress 2018; however, this particular sub-analysis was not included. Results of the REMISSIO study have been published in Garcia-Portilla M et al Therapeutic Advances in Psychopharmacology 2020;10:1–20., but does not include this sub-analysis.
Editorial assistance in the development of this manuscript was provided by OPEN Health Medical Communications (UK) with financial support from Janssen (EMEA), which has marketing authorization for PP1M and PP3M in Europe. The authors retained full editorial control over the content of the manuscript and the decision to publish it.
Funding Statement
This research was sponsored by Janssen, which has marketing authorization for PP1M and PP3M in Europe.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the Yale University Open Data Access Initiative for undefined period at https://yoda.yale.edu/; reference number NCT02713282. Respective datasets will be made available on reasonable request, subject to possible IP, privacy, regulatory, and/or other constraints.
Disclosure
M Lambert reports personal fees from Janssen-Cilag during the conduct of the study; personal fees from AstraZeneca, Bristol-Myers Squibb, Lilly Deutschland GmbH, Janssen Cilag GmbH, Lundbeck GmbH, Otsuka Pharma GmbH, Roche Deutschland Holding GmbH, Sanofi Aventis and Trommsdorff GmbH & Co KG. P Bergmans, S Gopal, M Mathews, A Wooller, and K Pungor are full-time employees of Janssen and stockholders of Johnson & Johnson. P Sanchez reports personal fees from Janssen-Cilag during the conduct of the study; personal fees from Janssen, Lundbeck, Otsuka, Casen-Recordati, Angelini, Adamed, Exeltis, Osakidetza and Ferrer, and grants from Instituto de Salud Carlos III, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Bitter I, Czobor P, Borsi A, et al. Mortality and the relationship of somatic comorbidities to mortality in schizophrenia. A nationwide matched-cohort study. Eur Psychiatry. 2017;45:97–103. doi: 10.1016/j.eurpsy.2017.05.022 [DOI] [PubMed] [Google Scholar]
- 2.Gardner KN, Nasrallah HA. Managing first-episode psychosis: rationale and evidence for nonstandard first-line treatments for schizophrenia. Curr Psychiatr. 2015;14:33–e33. [Google Scholar]
- 3.Nordstroem A-L, Talbot D, Bernasconi C, Berardo CG, Lalonde J. Burden of illness of people with persistent symptoms of schizophrenia: A multinational cross-sectional study. Int J Soc Psychiatry. 2017;63(2):139–150. doi: 10.1177/0020764016688040 [DOI] [PubMed] [Google Scholar]
- 4.Tandon R, Nasrallah HA, Keshavan MS. Schizophrenia, “just the facts” 4. Clinical features and conceptualization. Schizophr Res. 2009;110(1–3): 1–23. [DOI] [PubMed] [Google Scholar]
- 5.Emsley R, Chiliza B, Asmal L, Lehloenya K. The concepts of remission and recovery in schizophrenia. Curr Opin Psychiatry. 2011;24(2):114–121. [DOI] [PubMed] [Google Scholar]
- 6.Jose D, Ramachandra LK, Gandhi S, Desai G. Nagarajaiah. Consumer perspectives on the concept of recovery in schizophrenia: A systematic review. Asian J Psychiatr. 2015;14:13–18. [DOI] [PubMed] [Google Scholar]
- 7.Lahera G, Galvez JL, Sanchez P, et al. Functional recovery in patients with schizophrenia: recommendations from a panel of experts. BMC Psychiatry. 2018;18(1):176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leucht S. Measurements of response, remission, and recovery in schizophrenia and examples for their clinical application. J Clin Psychiatry. 2014;75(Suppl 1):8–14. [DOI] [PubMed] [Google Scholar]
- 9.Lloyd H, Lloyd J, Fitzpatrick R, Peters M. The role of life context and self-defined well-being in the outcomes that matter to people with a diagnosis of schizophrenia. Health Expect. 2017;20(5):1061–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rose G, Smith L. Mental health recovery, goal setting and working alliance in an Australian community-managed organisation. Health Psychology Open. 2018;5(1):2055102918774674. doi: 10.1177/2055102918774674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanches SA, van Busschbach JT, Michon HWC, van Weeghel J, Swildens WE. The Role of Working Alliance in Attainment of Personal Goals and Improvement in Quality of Life During Psychiatric Rehabilitation. Psychiatr Serv. 2018;69(8):903–909. doi: 10.1176/appi.ps.201700438 [DOI] [PubMed] [Google Scholar]
- 12.Bridges JF, Beusterien K, Heres S, et al. Quantifying the treatment goals of people recently diagnosed with schizophrenia using best–worst scaling. Patient Prefer Adherence. 2018;12:63–70. doi: 10.2147/PPA.S152870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pietrini F, Albert U, Ballerini A, et al. <p>The modern perspective for long-acting injectables antipsychotics in the patient-centered care of schizophrenia. Neuropsychiatr Dis Treat. 2019;15:1045–1060. doi: 10.2147/NDT.S199048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stip E, Lachaine J. Real-world effectiveness of long-acting antipsychotic treatments in a nationwide cohort of 3957 patients with schizophrenia, schizoaffective disorder and other diagnoses in Quebec. Ther Adv Psychopharmacol. 2018;8(11):287–301. doi: 10.1177/2045125318782694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tiihonen J, Mittendorfer-Rutz E, Majak M, et al. Real-World Effectiveness of Antipsychotic Treatments in a Nationwide Cohort of 29 823 Patients With Schizophrenia. JAMA Psychiatry. 2017;74(7):686–693. doi: 10.1001/jamapsychiatry.2017.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mathews M, Gopal S, Nuamah I, et al. <p>Clinical relevance of paliperidone palmitate 3-monthly in treating schizophrenia. Neuropsychiatr Dis Treat. 2019;15:1365–1379. doi: 10.2147/NDT.S197225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berwaerts J, Liu Y, Gopal S, et al. Efficacy and Safety of the 3-Month Formulation of Paliperidone Palmitate vs Placebo for Relapse Prevention of Schizophrenia: A Randomized Clinical Trial. JAMA Psychiatry. 2015;72(8):830–839. doi: 10.1001/jamapsychiatry.2015.0241 [DOI] [PubMed] [Google Scholar]
- 18.Savitz AJ, Xu H, Gopal S, et al. Efficacy and Safety of Paliperidone Palmitate 3-Month Formulation for Patients with Schizophrenia: A Randomized, Multicenter, Double-Blind, Noninferiority Study. Int J Neuropsychopharmacol. 2016;19(7):pyw018. doi: 10.1093/ijnp/pyw018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lai JK, Margolese HC. A qualitative study of patient experience when switching from paliperidone palmitate once monthly (PP1M) to paliperidone palmitate three monthly (PP3M) long-acting injectable antipsychotic. Schizophr Res. 2019;204:443–444. doi: 10.1016/j.schres.2018.09.012 [DOI] [PubMed] [Google Scholar]
- 20.Pai N, Warden M. Early Australian experience in the maintenance of schizophrenia management with 3-monthly paliperidone palmitate. Australas Psychiatry. 2018;26(6):628–634. doi: 10.1177/1039856218789770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rise M, Stølan L, Erdner A, et al. Scandinavian user perspectives on three-monthly administrations of antipsychotic medication. 27th European Congress of Psychiatry; 2019; Warsaw, Poland. [Google Scholar]
- 22.Garcia-Portilla MP, Llorca P-M, Maina G, et al. Symptomatic and functional outcomes after treatment with paliperidone palmitate 3-month formulation for 52 weeks in patients with clinically stable schizophrenia. Ther Adv Psychopharmacol. 2020;10:2045125320926347. doi: 10.1177/2045125320926347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 24.TREVICTA®. Prolonged Release Suspension for Injection [Summary of Product Characteristics]. Beerse, Belgium:: Janssen-Cilag International NV; 2019. [Google Scholar]
- 25.Kiresuk TJ, Sherman RE. Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health J. 1968;4(6):443–453. doi: 10.1007/BF01530764 [DOI] [PubMed] [Google Scholar]
- 26.Turner-Stokes L. Goal Attainment scaling (GAS) in rehabilitation: a practical guide. Clinical Rehabilitation; 2019. http://www.kcl.ac.uk/lsm/research/divisions/cicelysaunders/attachments/Tools-GAS-Practical-Guide.pdf. Accessed August, 2019. [DOI] [PubMed]
- 27.Üstün T, Kostanjsek N, Chatterji S, Rehm J. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule (WHODAS 2.0). World Health Organization; 2010. http://apps.who.int/iris/bitstream/10665/43974/1/9789241547598_eng.pdf. [Google Scholar]
- 28.Potkin S, Bera R, Zubek D, Lau G. Patient and prescriber perspectives on long-acting injectable (LAI) antipsychotics and analysis of in-office discussion regarding LAI treatment for schizophrenia. BMC Psychiatry. 2013;13(1):261. doi: 10.1186/1471-244X-13-261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cahling L, Berntsson A, Broms G, Ohrmalm L. Perceptions and knowledge of antipsychotics among mental health professionals and patients. BJPsych Bulletin. 2017;41(5):254–259. doi: 10.1192/pb.bp.116.055483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiden PJ, Roma RS, Velligan DI, Alphs L, DiChiara M, Davidson B. The challenge of offering long-acting antipsychotic therapies: a preliminary discourse analysis of psychiatrist recommendations for injectable therapy to patients with schizophrenia. J Clin Psychiatry. 2015;76(6):684–690. doi: 10.4088/JCP.13m08946 [DOI] [PubMed] [Google Scholar]
- 31.Beitinger R, Kissling W, Hamann J. Trends and perspectives of shared decision-making in schizophrenia and related disorders. Curr Opinion Psychiatry. 2014;27(3):222–229. doi: 10.1097/YCO.0000000000000057 [DOI] [PubMed] [Google Scholar]
- 32.Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):98. doi: 10.1186/s13012-018-0784-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamann J, Langer B, Winkler V, et al. Shared decision making for in-patients with schizophrenia. Acta Psychiatr Scand. 2006;114(4):265–273. doi: 10.1111/j.1600-0447.2006.00798.x [DOI] [PubMed] [Google Scholar]
- 34.Kuhnigk O, Slawik L, Meyer J, Naber D, Reimer J. Valuation and attainment of treatment goals in schizophrenia: perspectives of patients, relatives, physicians, and payers. J Psychiatr Pract. 2012;18(5):321–328. doi: 10.1097/01.pra.0000419816.75752.65 [DOI] [PubMed] [Google Scholar]
- 35.Janicak PG. Paliperidone ER: a review of the clinical trial data. Neuropsychiatr Dis Treat. 2008;3(6):869–897. doi: 10.2147/NDT.S1365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marwaha S, Johnson S. Schizophrenia and employment - a review. Soc Psychiatry Psychiatr Epidemiol. 2004;39(5):337–349. doi: 10.1007/s00127-004-0762-4 [DOI] [PubMed] [Google Scholar]
- 37.Marwaha S, Johnson S, Bebbington P, et al. Rates and correlates of employment in people with schizophrenia in the UK, France and Germany. Br J Psychiatry. 2007;191(1):30–37. doi: 10.1192/bjp.bp.105.020982 [DOI] [PubMed] [Google Scholar]
- 38.McGurk SR, Mueser KT, DeRosa TJ, Wolfe R. Work, recovery, and comorbidity in schizophrenia: a randomized controlled trial of cognitive remediation. Schizophr Bull. 2009;35(2):319–335. doi: 10.1093/schbul/sbn182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenheck R, Leslie D, Keefe R, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163(3):411–417. doi: 10.1176/appi.ajp.163.3.411 [DOI] [PubMed] [Google Scholar]
- 40.Salkever DS, Karakus MC, Slade EP, et al. Measures and predictors of community-based employment and earnings of persons with schizophrenia in a multisite study. Psychiatr Serv. 2007;58(3):315–324. doi: 10.1176/ps.2007.58.3.315 [DOI] [PubMed] [Google Scholar]
- 41.Charzyńska K, Kucharska K, Mortimer A. Does employment promote the process of recovery from schizophrenia? A review of the existing evidence. Int J Occup Med Environ Health. 2015;28(3):407–418. doi: 10.13075/ijomeh.1896.00341 [DOI] [PubMed] [Google Scholar]
- 42.Krupa T. Employment, Recovery, and Schizophrenia: integrating health and disorder at work. Psychiatric Reha J. 2004;28(1):8–15. doi: 10.2975/28.2004.8.15 [DOI] [PubMed] [Google Scholar]
- 43.Provencher HL, Gregg R, Mead S, Mueser KT. The role of work in the recovery of persons with psychiatric disabilities. Psychiatric Rehab J. 2002;26(2):132–144. doi: 10.2975/26.2002.132.144 [DOI] [PubMed] [Google Scholar]
- 44.Resnick SG, Rosenheck RA, Lehman AF. An exploratory analysis of correlates of recovery. Psychiatr Serv. 2004;55(5):540–547. doi: 10.1176/appi.ps.55.5.540 [DOI] [PubMed] [Google Scholar]
- 45.Warner R. Recovery from schizophrenia and the recovery model. Curr Opinion Psychiatry. 2009;22(4):374–380. doi: 10.1097/YCO.0b013e32832c920b [DOI] [PubMed] [Google Scholar]
- 46.Schreiner A, Aadamsoo K, Altamura AC, et al. Paliperidone palmitate versus oral antipsychotics in recently diagnosed schizophrenia. Schizophr Res. 2015;169(1–3):393–399. doi: 10.1016/j.schres.2015.08.015 [DOI] [PubMed] [Google Scholar]
- 47.Taipale H, Mittendorfer-Rutz E, Alexanderson K, et al. Antipsychotics and mortality in a nationwide cohort of 29,823 patients with schizophrenia. Schizophr Res. 2018;197:274–280. doi: 10.1016/j.schres.2017.12.010 [DOI] [PubMed] [Google Scholar]
- 48.McKibbin C, Patterson TL, Jeste DV. Assessing disability in older patients with schizophrenia: results from the WHODAS-II. J Nerv Ment Dis. 2017;74(7):405–413. doi: 10.1097/01.nmd.0000130133.32276.83 [DOI] [PubMed] [Google Scholar]
- 49.Ertugrul A, Ulug B. The influence of neurocognitive deficits and symptoms on disability in schizophrenia. Acta Psychiatr Scand. 2002;105(3):196–201. [DOI] [PubMed] [Google Scholar]
- 50.Guilera G, Gomez-Benito J, Pino O, et al. Utility of the World Health Organization Disability Assessment Schedule II in schizophrenia. Schizophr Res. 2012;138(2–3):240–247. [DOI] [PubMed] [Google Scholar]
- 51.Conley RR, Ascher-Svanum H, Zhu B, Faries DE, Kinon BJ. The burden of depressive symptoms in the long-term treatment of patients with schizophrenia. Schizophr Res. 2007;90(1–3):186–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gaynes BN, Burns BJ, Tweed DL, Erickson P. Depression and health-related quality of life. J Nerv Ment Dis. 2002;190(12):799–806. [DOI] [PubMed] [Google Scholar]
- 53.Jin H, Zisook S, Palmer BW, Patterson TL, Heaton RK, Jeste DV. Association of depressive symptoms with worse functioning in schizophrenia: a study in older outpatients. J Clin Psychiatry. 2001;62(10):797–803. [DOI] [PubMed] [Google Scholar]