Abstract
Objective
To determine the implant orientation, especially the combined anteversion measurements in total hip arthroplasty (THA) using lateral approach, and to compare with implant orientation using posterior‐lateral (P‐L) approach. The secondary goal was to identify the factors associated with implant orientation.
Methods
Five hundred and one patients (545 hips) who underwent primary THA with the modified Hardinge approach between January 2016 and November 2019 by one senior surgeon in our department in a retrospective study were followed up. A survey to inquire about the history of dislocation of the hip after THA was designed and responses were gathered by telephone, WeChat software, and outpatient follow‐up. The mean age of the patients was 61.97 ± 11.72 years, and there were 254 males and 247 females. The average follow‐up time was 25.2 ± 13.7 months (range, 3.2–49.7 months). Among the patients who were followed up, 97 patients (104 hips) underwent computed tomography (CT) scans from L4 to the tuberosity of the tibia. The implant orientation, including the anteversion and inclination of the cup, anteversion of the stem, combined anteversion, and pelvic tilt were measured based on CT scans of these patients. The results were compared with the implant orientation reported in previous reports measured by CT. Factors that may be associated with implant orientation were investigated, including the patient's age, sex, body mass index (BMI), and diagnosis; size of the cup; diameter of the femoral head component; and pelvic tilt. Data and statistical analyses were performed using SPSS 20.0.
Results
No cases of dislocation were found in the 501 patients (545 hips) who underwent primary THA during this period. The mean inclination and anteversion of the cups were 38.83° ± 5.04° (24.5°–53.1°) and 9.26° ± 11.19° (−15°–48°), respectively. The mean anteversion of the stem was 13.83° ± 10.7° (−10.2°–42.3°). The combined anteversion was 23.1° ± 13.4° (−7.4°–54.6°). Compared with the reported combined anteversion and anteversion of the cup, the mean anteversion of the cup and combined anteversion using the lateral approach were much lower than the reported values in the literature using the P‐L approach. Pelvic tilt was found to be the only independent factor for cup anteversion. Factors including age, sex, BMI, diagnosis, cup size, and diameter of the femoral head component were not associated with implant orientation.
Conclusion
THA using the lateral approach yields smaller cup anteversion and combined anteversion values than using the P‐L approach. Pelvic tilt is the only predictor for cup anteversion.
Keywords: Joint Dislocations; Arthroplasty, Replacement, hip; Prostheses and Implants
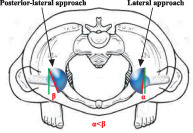
This study investigated the implant orientations in total hip arthroplasty using lateral approach and found the anteversion of cup and combined anteversion were lower than the value using posterior‐lateral approach. In the abstract graph, the green line represents sagittal plane while the red one shows the line connecting the lateral anterior and posterior margins of the cup. The angle “α” is the anteversion of cup using lateral approach while “β” represents the anteversion angle of cup using posterior‐lateral approach.
Introduction
Total hip arthroplasty (THA) is the most important treatment for the late stage of hip osteoarthritis, femoral head necrosis, as well as many hip diseases and achieves great success 1 . Dislocation commonly occurs after THA and this is believed to be the main cause leading to revision within the first 2 years after operation 2 . There are numerous factors associated with dislocation. Among them, the implant orientation, as an important evaluation of implant factors, plays a particularly critical role in the stability of prostheses 3 . The implant orientation mainly includes the anteversion and inclination of the cup and the anteversion of the femoral head component. In the 1970s, Lewinnek first defined the safe zone of the cup as an anteversion of 15° ± 10° and an inclination of 40° ± 10°, and showed that the rate of dislocation in the safe zone was much lower than that outside of the safe zone 4 . Since then, many studies have focused on the effect of implant orientation on dislocations and reported different conclusions regarding the ideal implant orientation 5 , 6 , 7 , 8 . For example, a study concluded that the dislocation risk was 1.9 times higher if cup anteversion was not between 10° and 30°, which is different from the Lewinneck safe zone 9 . Moreover, many studies have also focused on the factors influencing implant orientation 5 , 10 . For instance, after analyzing numerous factors related to dislocation, Callanan found that surgical approach, surgeon volume, and obesity (body mass index, BMI > 30 kg/m2) were independent factors related to mal‐positioned cups 5 . Migliorini also reported the effect of surgical approach on implant orientation 11 . Therefore, surgical approach is an important determinant of implant orientation. Although numerous reports have shown that, compared with the posterior‐lateral (P‐L) and anterior approaches, the lateral approach has the lowest rate of dislocation, only a few reports on implant orientation with this approach have been published 12 , 13 , 14 .
Combined anteversion, which is defined as the sum of the anteversion of the cup and that of the femoral component, is used to further illustrate the ideal orientation for the stability of prostheses. Many studies have summarized the angle of combined anteversion in clinic practice 6 , 8 , 15 . However, the range of combined anteversion varies in different reports. Dorr concluded that the combined anteversion was 37.6° ± 7° (range, 19°–50°) 6 . Kubota reported that combined anteversion is 41.2° ± 8.9° with navigation and 33.6° ± 20.5° without navigation 15 . Although the ideal combined anteversion still needs to be investigated, numerous studies have used the combined anteversion technique to guide their operations and achieve good results 16 , 17 , 18 , 19 . For example, Zhang found that the use of combined anteversion in THA could achieve stable and functioning joints for patients with developmental dysplasia of the hip (DDH) 18 . Another study reported that the use of combined anteversion in revision THA obtained favorable dislocation results 20 . Therefore, THA with the concept of combined anteversion decreases the dislocation rate and is widely used in clinical practice 19 . However, although the range of combined anteversion varies across reports 6 , 15 , no studies have investigated combined anteversion using the lateral approach. Moreover, because different approaches may require different implant orientations for hip stability, whether the required combined anteversion is similar to the angle used in the P‐L approach remains unknown. If it is not the same, the combined anteversion angle used with the P‐L approach may lead to an improper implant position in procedures performed with the lateral approach. Therefore, it is necessary to identify the combined anteversion angle using the lateral approach and compare it with the P‐L approach.
Several studies of the factors affecting the implant orientation have been conducted, but most of them have been based on the P‐L approach. These factors can be classified as patient‐dependent factors and patient‐independent factors. For example, patient‐dependent factors such as BMI were found to be important factors associated with cup malposition 5 . Zhu et al. showed that pelvic tilt contributes to cup anteversion and that each degree of tilt changes the cup anteversion by 0.8°, while another study concluded that cup anteversion is not correlated with the native acetabular anteversion 21 , 22 . Patient‐independent factors such as the surgical approach and size of the femoral head component were found to be important factors associated with cup anteversion 5 , 11 . However, the factors affecting implant orientation with the lateral approach have not been identified.
Therefore: (i) the primary goal of this study was to determine the implant orientation in patients who underwent THA using the lateral approach, especially the combined anteversion angles; (ii) the secondary goal was to compare these values with implant orientation using the P‐L approach; (iii) the third goal was to identify the factors associated with implant orientation. The elucidation of the above goals is not only useful for further understanding the implant orientation using the lateral approach, but also for guiding THA operations using the lateral approach during clinical practice.
Materials and Methods
Ethics Statement
Ethics approval was obtained from our institutional review board. Informed consent was obtained from all patients.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (i) patients with late stage of hip diseases who underwent primary THA in our department between January 2016 and November 2019; (ii) underwent the lateral approach and cementless prosthesis; (iii) the major comparison variables included dislocation of hip after THA, inclination of cup and anteversion of cup and stem measured on computed tomography (CT) scans as well as the combined anteversion; (iv) the main outcome was whether patients had a dislocation history after THA and implant orientation in these THAs; and (v) a retrospective study. The exclusion criteria were as follows: (i) revision cases; and (ii) periprosthetic fracture during the follow‐up time.
Surgical Procedures
All of the patients underwent THA with the modified Hardinge approach (Fig. 1). (i) Anesthesia and position: patients under general or spinal anaesthesia were positioned in a lateral position. (ii) Approach and exposure: a lateral incision above the greater trochanter was made (Fig. 1A). After the anterior 1/3 of the gluteus medius and vastus lateralis was detached (Fig. 1B and C), the gluteus minimus was split vertically and the capsule and labrum were partly removed. Then, the femoral head was exposed, and the joint was dislocated from the anterior direction (Fig. 1D and E). (iii) Preparation and fixation of prosthesis: we prepared the proximal femur first to determine the degree of anteversion and create more operative space for the acetabulum (Fig. 1F). Then, after the acetabulum was reamed, the cup was implanted into the acetabulum (Fig. 1G), and the femoral component was implanted (Fig. 1H). During the operation, we used the transverse acetabular ligament or the native acetabular rim or patient position as the guide for cup orientation. (iv) Prosthesis evaluation: after the joint was reduced, the joint stability and range of motion were assessed and confirmed that no dislocation occurred during flexion/extension, abduction/adduction, or external/internal rotation (Fig. 1I). (v) Wound closure and rehabilitation: the incision was closed without drainage after suture of the gluteus medius onto greater trochanter. After the operation, a standard protocol was used for rehabilitation. The cups used in our department were press fit and hemispherical shells, and the models used included the Pinnacle (DePuy, Warsaw, USA), Trabecular Metal (Zimmer, Warsaw, USA), and Trident (Stryker, Mahwah, USA) models. The femoral components used were Trilock (DePuy, Warsaw, USA), Trabecular Metal (Zimmer, Warsaw, USA), and Accolade (Stryker, Mahwah, USA).
Fig. 1.
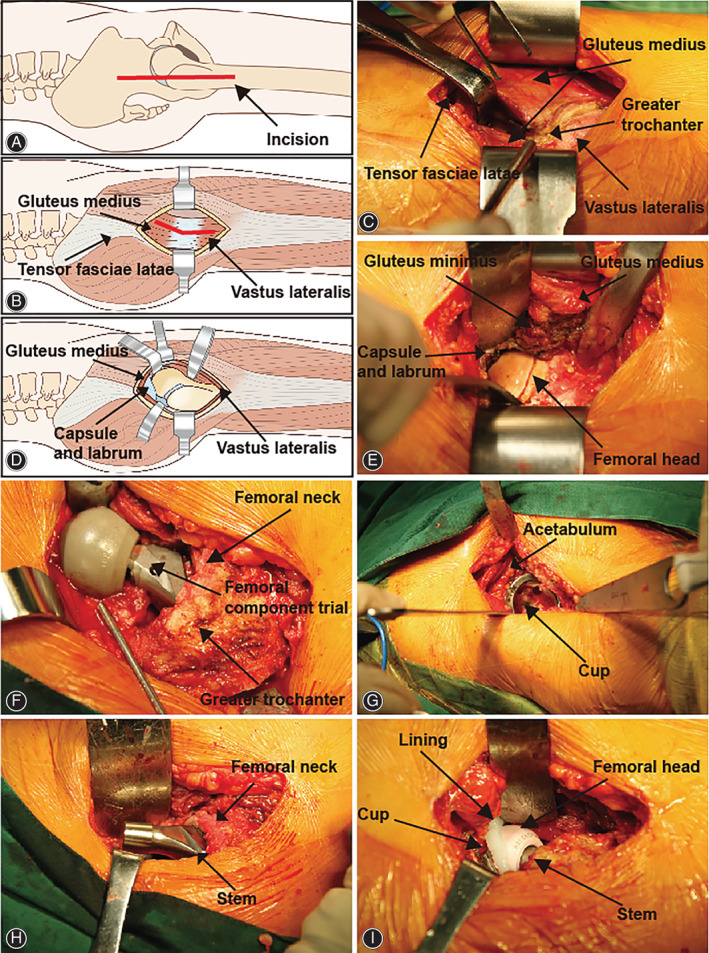
THA using the modified Hardinge approach. (A) The incision was started 3–5 cm proximal to the apex of the greater trochanter and extended distally about 5–7 cm in line with the femur. (B) and (C) The tendon and muscle fibers of the gluteus medius were visualized and split in a one‐third anterior/two‐thirds posterior fashion. (D) and (E) After the gluteus minimus was split, a capsulectomy and labrumectomy was performed to facilitate exposure and dislocation of the hip. (F) The proximal femur was prepared first to determine the anteversion of the stem. (G) The acetabulum was prepared, and the press‐fit cup was fixed on the acetabulum. (H) The proximal femur was further prepared, and the stem was fixed in the proximal femur. (I) The hip was reduced after all of the procedures, and the stability was assessed.
Data Collection
A survey was designed and administered by telephone, WeChat software (Tencent Tech Co., Ltd., Shenzhen, China), and outpatient follow‐up. This survey collected two categories of information: demographics and dislocation information.
Demographics
During this period, 564 patients (613 hips) who underwent THA in our department by a senior surgeon (ZY) using the modified Hardinge approach were identified. Among these patients, 54 were lost to follow‐up, and nine died. Therefore, a total of 501 patients (545 hips) completed the survey in this study. The mean age of the patients was 61.97 ± 11.72 years, and there were 254 males and 247 females. The average follow‐up time was 25.2 ± 13.7 months (range, 3.2–49.7 months). The diagnoses of the patients included femoral head necrosis (n = 247, 45.3%), femoral neck fracture (n = 63, 11.6%), hip osteoarthritis (n = 193, 35.4%), developmental hip dysplasia (DDH) (n = 36, 6.6%), and other conditions (n = 6, 1.1%).
Among the patients who were followed up, 97 patients (104 hips) underwent CT scans from L4 to the tuberosity of the tibia after THA. The mean age of the patients was 59.6 ± 12.5 years (range, 24–82 years), and there were 49 males and 48 females. The average follow‐up time was 20.4 ± 10.2 months (range, 3.3–38.9 months) and the mean BMI was 23.81 ± 3.58 kg/m2 (range, 16.80–34.37 kg/m2). The diagnoses of the patients included femoral head necrosis (n = 47), femoral neck fracture (n = 11), hip osteoarthritis (n = 34), DDH (n = 9), and other conditions (n = 3). The femoral head sizes used in these THAs were 28 mm (n = 16), 32 mm (n = 63) and 36 mm (n = 25), and the cup size varied from 44 mm–60 mm: 44 mm (n = 7), 46 mm (n = 10), 48 mm (n = 35), 50 mm (n = 13), 52 mm (n = 24), 54 mm (n = 8), 56 mm (n = 4), 58 mm (n = 2), and 60 mm (n = 1).
Dislocation Information
Dislocation after THA means the femoral head component comes out from the implanted cup. The patients will lose the ability to walk and limbs will not be equal in length if the dislocation occurrs after THA. Dislocation was confirmed by an X‐ray screen of hip. The survey inquired as to whether the patient had a history of dislocation after THA operation during the follow‐up. This was a binary variable that included “dislocation” and “no dislocation.” The variable reflects one of the most important complications leading to revision.
Radiographic Measurements
CT scans from L4 to tibial tuberosity were obtained after surgery. The CT information was stored and transferred in standard Digital Imaging and Communications in Medicine (DICOM) format to MIMICS 10.01 measurement software (Materialize Medical Co, Belgium). A single investigator (PF) performed all measurements to minimize interobserver variability.
Inclination and Anteversion of the Cup
The inclination of the cup defined the orientation of the cup in the coronal plane and sagittal plane, respectively. The value was measured based on CT images as described in previous reports 7 , 8 , 9 . Briefly, the inclination of the cup was calculated with respect to a horizontal line through the bottom edge of the ischial tuberosity while the anteversion of the cup was measured as the angle between a line connecting the lateral anterior and posterior margins of the cup and a perpendicular line connecting two identical points on either side of the pelvis. Typical images are shown in Figs 2A and B. According to the safe zone by Lewinnek, the inclination of the cup should be within 40° ± 10° and the anteversion of the cup should range from 5°–25°. Increasing or decreasing the inclination or anteversion of the cup reduced the stability of hip and probably led to dislocation.
Fig. 2.
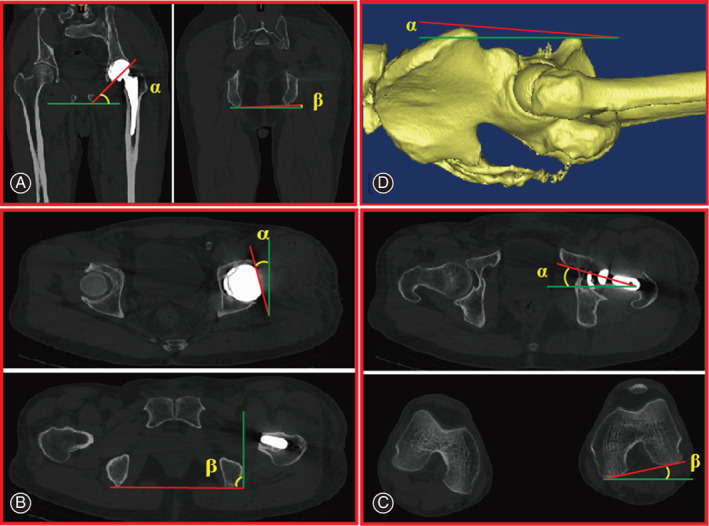
Methods used to measure implant orientation and pelvic tilt using CT. The red line is the measured line, while the green line is the reference line. The green lines refer to the horizontal plane in (A), sagittal plane in (B) and (D), and coronal plane in (C) and (D). To minimize the effect of rotation of the pelvis, the angle “β” is used as a reference angle. (A) The inclination of the cup is calculated as (α‐β). (B) The anteversion of the acetabular component is calculated as (α + 90‐β). (C) The anteversion of the stem is calculated as (α + β). (D) Pelvic tilt is calculated as the angle (α) between the line at “the top of the symphysis pubis in the same vertical plane as the anterior superior spine” and the sagittal plane in a 3‐D model.
Anteversion of the Stem
The anteversion of the stem reflects the angle between the condylar axis and stem neck and was measured based on CT images and analyzed as described in previous reports 7 , 8 , 9 . This angle was calculated as the angle between a line connecting the posterior aspect of the medial and lateral femoral condyles and a line from the center of the femoral head to the center of the neck of femoral component. Typical images are shown in Fig. 2C. The standard of this angle usually varies and largely depends on the proximal geometry of the femur. Increasing the anteversion of stem usually leads to anterior dislocation and vice versa.
Combined Anteversion
Combined anteversion was defined as the sum of the anteversion of the cup and that of the femoral component. It was calculated by the sum of the stem and cup anteversion angles. Dorr concluded that the combined anteversion was 37.6° ± 7° (range, 19°–50°) 6 . This value was used to assess the appropriateness of overall prosthetic alignment. Too large or too small combined anteversion may lead to anterior or posterior dislocation.
Pelvic Tilt
Pelvic tilt was the orientation of the pelvis in respect to the vertical plane of body. The angle of pelvic tilt was measured from “the top of the symphysis pubis in the same vertical plane as the anterior superior spine” in a three‐dimensional (3D) model (Fig. 2D) 22 , 23 . This virtual 3D model of the patient's pelvis was reconstructed using the DICOM files and MIMICS software. The pelvic tilt measurements were negative if the anterior superior iliac spines were posterior to the pubic symphysis and vice versa. The pelvic tilt was considered as an important factor contributing to the implant orientation.
Statistical Analysis
Data and statistical analyses were performed using SPSS 20.0 (IBM Corp., Armonk, NY, USA). Normally distributed data are described as the mean and standard deviation. Non‐normally distributed data are reported as the mean and 95% confidence interval (CI). Correlation coefficients were determined by the Spearman rank correlation test using two‐tailed P values. A correlation plot was generated using the R package (Version R 3.5.3, R Core Team, Vienna, Austria). Multivariate regression analysis using the stepwise method and seven variables (age, sex, BMI, diagnosis, cup size, diameter of femoral head component, and pelvic tilt) was performed to examine predictors of implant orientation. P < 0.05 corresponded to a significant difference.
Results
General Result
To investigate the prevalence of dislocation, we investigated whether the patients experienced dislocation. Fortunately, none of the THAs (0/545) experienced a history of dislocation during hospitalization as well as during the whole follow‐up period.
The Orientation of the Cup and Stem and the Combined Anteversion
Inclination and Anteversion of the Cup
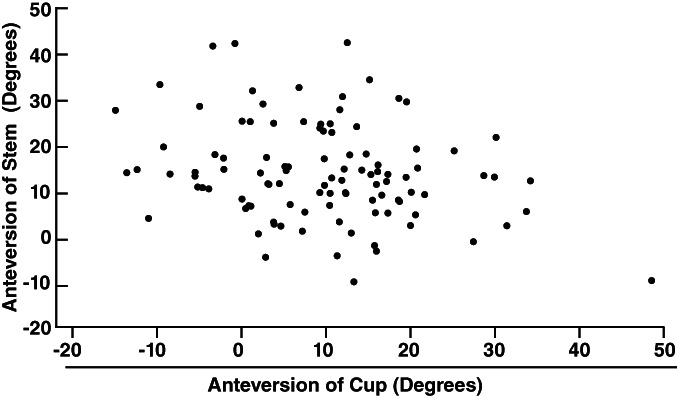
The mean inclination and anteversion of the cups were 38.83° ± 5.04° (24.5°–53.1°) and 9.26° ± 11.19° (−15°–48°), respectively. Among these measurements, 96.2% (100/104) of the inclination angles and 55.8% (58/104) of the anteversion angles of the cups were in the safe range according to Lewinnek's criteria. In addition, 52.9% of the cases were within the safe range for both anteversion and inclination (Fig. 3).
Fig. 3.
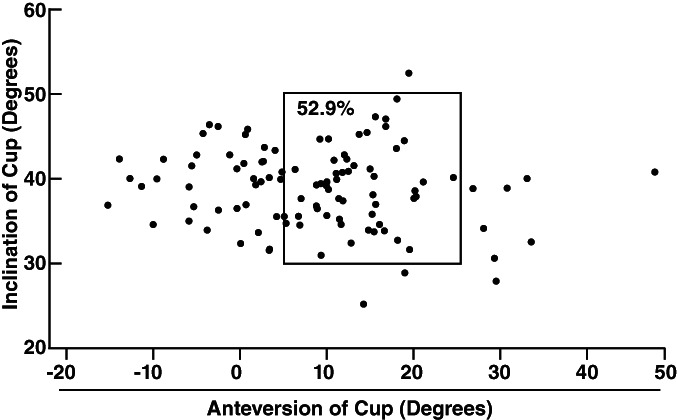
Scatter plots depicting the anteversion and inclination of the cup. The rectangle shows the hips that were within the Lewinnek safe zones.
Anteversion of the Stem
The mean anteversion of the stem was 13.83° ± 10.7° (−10.2°–42.3°). The anteversion angles of the cup and stem for all cases are shown in Fig. 4.
Fig. 4.
Scatter plots depicting the anteversion angles of the cup and stem.
Combined Anteversion
The combined anteversion in these patients who underwent THA was 23.1° ± 13.4° (−7.4°–54.6°). The combined anteversion and inclination angles of the cup for all cases are shown in Fig. 5. However, only 44.2% (46/104) of the hips had measurements within the combined anteversion zone (25°–50°) suggested by Dorr et al. 6 .
Fig. 5.
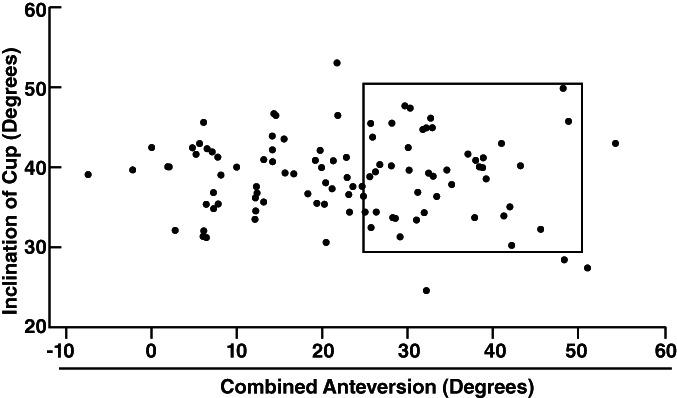
Scatter plots depicting the inclination of the cup and the combined anteversion. The rectangle shows the hips with an inclination of 40° ± 10° and a combined anteversion angle from 25° to 50°.
Taking into consideration the Lewinnek safe zone and Dorr's suggestion for combined anteversion, we found 73 outliers (70.2%). Meanwhile, we summarized the implant orientations measured using CT that were reported in previous studies and listed the information of dislocation and implant orientations in Table 1. We found the anteversion of the cup and the combined anteversion were lower than those reported in previous studies using the P‐L approach measured through CT, while the inclination of the cup and anteversion of the stem were similar to those reported in previous studies.
Table 1.
Studies in which implant orientation was measured by CT
| Study | Measurement method | Inclination of cup | Anteversion of cup | Anteversion of stem | Combined anteversion | Dislocation | Approach |
|---|---|---|---|---|---|---|---|
| Wines et al. (2006) 24 | CT | NA | 22.0° ± 14.0° (−12° to 52°) | 16.8° ± 11.1° (−15° to 45°) | NA | NA | Hardinge (n = 31) and P‐L (n = 80) |
| Dorr et al. (2009) 6 | CT | NA | 27° ± 4.6° (8.8° to 38.7°) | 10.6° ± 8° (−8.6° to 27.1 °) | 37.6° ± 7° (19° to 50°) | NA | P‐L(n = 47) |
| Wassilew et al. (2010) 25 | CT | NA | 19.5° ± 3.7° (11° to 27°) | NA | 34.4° ± 9.3° (16.3° to 57.3°) | None (0/46) | Anterolateral approach (n = 46) |
| Fujishiro et al. (2014) 7 | CT | 41.0° ± 6.2° | 24.7° ± 11.3° (−22.7° to 56.6°) | 40.3° ± 11.3° (−13.4° to 80°) | 65.0° ± 15.7° (12.9° to 112°) | NA | P‐L (n = 1411) |
| Tsai et al. (2014) 26 | CT | 40° ± 6.7° (34° to 56.8°) | 37.3° ± 21° (−10.1° to 58.7°) | NA | NA | 0/14 | NA (n = 14) |
| Fujishiro et al. (2016) 9 | CT | 40.9° ± 6.05° | 24.5° ± 11.4° | 39.9° ± 11.6° | NA | 50/1555 | P‐L (n = 1555) |
| Murphy et al. (2018) 8 | CT | 37° ± 7° (18° to 68°) | 34° ± 12° (−2° to 59°) | 24° ± 14° (−27° to 61°) | 57° ± 19° (−12° to 110°) | 0/175 | NA (n = 175) |
| Our Study | CT | 38.83 ± 5.04° (24.5° to 53.1°) | 9.26° ± 11.19° (−15° to 48°) | 13.83 ± 10.7° (−10.2° to 42.3°) | 23.1° ± 13.4° (−7.4° to 54.6°) | 0/104 | Hardinge (n = 104) |
NA, not applicable; P‐L, Posterior‐lateral approach.
Pelvic Tilt Associated with the Implant Orientation
Until now, the factors associated with implant orientation in THA with the lateral approach have not been identified. To identify the implant orientation‐related factors, seven variables were analyzed for correlations with implant orientation using a multivariate regression analysis including age, sex, BMI, diagnosis, size of the cup, diameter of the femoral head, and pelvic tilt. In this study, the mean pelvic tilt was 3.1° ± 7.8° (range, −32°–17°). This result was similar to those in previous reports 8 . The correlation between implant orientation and factors is shown in Fig. 6. After multivariate regression analysis was performed, we found that pelvic tilt was the only independent factor contributing to the anteversion of the cup (R 2 = 0.098, P = 0.008) but not associated with the inclination of the cup, the anteversion of the stem, or the combined anteversion angle. One degree of pelvic tilt was associated with −0.338° of cup anteversion. However, factors including age, sex, BMI, cup size, and diameter of the femoral head component were not associated with the implant orientation (Table 2).
Fig. 6.
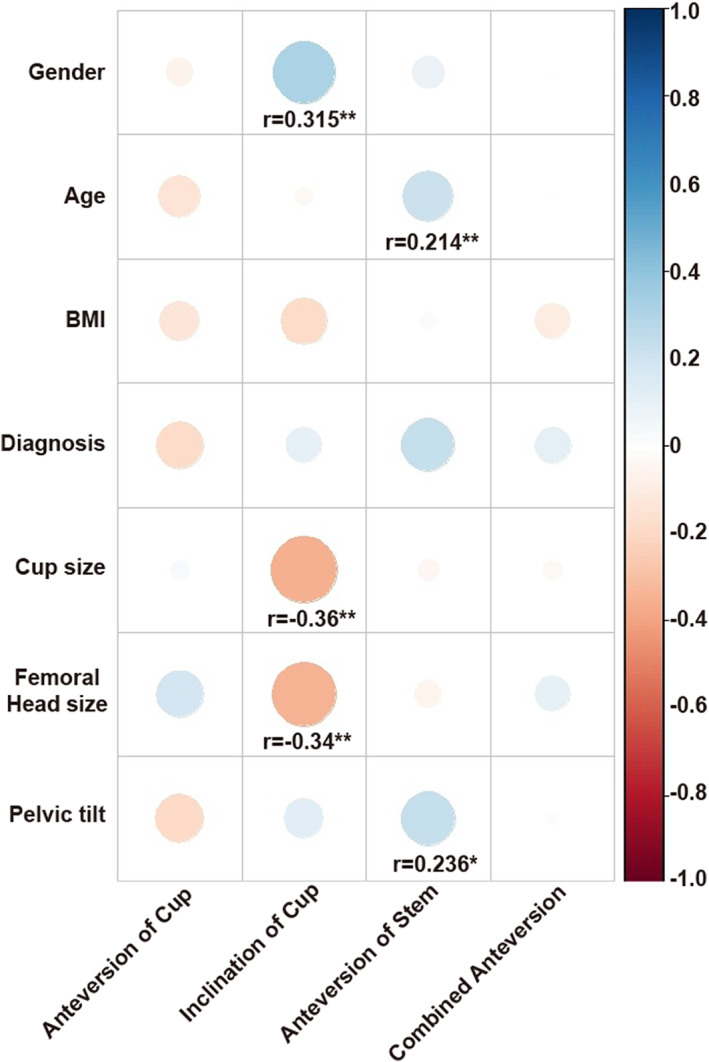
Correlations between implant orientation and seven other factors. The correlation coefficients were calculated by the Spearman rank correlation test using two‐tailed P values and are shown in the plot. The different colors and sizes of the circles represent the correlation coefficients between factors. Blue circles represent positive correlations, while red circles represent negative correlations. *P < 0.05, **P < 0.01.
Table 2.
Multivariate analysis with implant orientation and seven factors (P value)
| Factors | Anteversion of cup | Inclination of cup | Anteversion of stem | Combined anteversion |
|---|---|---|---|---|
| Gender | 0.780 | 0.586 | 0.986 | 0.924 |
| Age | 0.396 | 0.747 | 0.063 | 0.109 |
| BMI | 0.235 | 0.198 | 0.688 | 0.404 |
| Diagnosis | 0.403 | 0.099 | 0.331 | 0.586 |
| Femoral Head size | 0.860 | 0.435 | 0.489 | 0.489 |
| Cup diameter | 0.512 | 0.496 | 0.900 | 0.882 |
| Pelvic tilt | 0.008 | 0.102 | 0.296 | 0.509 |
BMI, body mass index.
Discussion
Different approaches may require different implant orientations to prevent dislocation after THA because different parts of soft tissues are disturbed in various approaches. Combined anteversion was found to be one of the most important implant orientation measures in THA. However, combined anteversion in procedures performed using the lateral approach has not been investigated previously. Therefore, this information on the implant orientation for this approach is not only useful to know but could also guide operations performed by surgeons using this approach.
Variation in the Dislocation Rates in THA Using Different Approaches and Its Possible Reasons
It is well known that different approaches lead to different rates of dislocation. Among them, the lateral approach has the lowest rate of dislocation. A review by Petis et al. compared the dislocation rates of different approaches and showed that the anterior approach has a dislocation rate of 0.61%–1.5% and the lateral approach has a dislocation rate of 0.4%–0.55%, whereas the P‐L approach has a dislocation rate of 1%–5% 14 . Masonis reported that the lowest rate of dislocation after THA occurred with the direct lateral approach (0.55%) compared with the transtrochanteric approach (1.27%), P‐L approach (3.23%), and anterolateral approach (2.18%) 27 . Moreover, Goyal found only one case of dislocation in 1010 patients (0.09%) who underwent THA using the modified Hardinge approach 28 . In our study, we used the modified Hardinge approach and obtained satisfactory results regarding dislocation. We hypothesize that the disturbed soft tissue in different approaches acts as a “door” for the femoral component head, and that different approaches may lead to different positions of “doors” (Fig. 7). Good suturing of these tissues will strengthen the door, while poor suturing of these soft tissues may weaken the door. A good example of a strong door was shown by Kwon et al., who found an eight times greater relative risk of dislocation when posterior soft tissue was not repaired with the P‐L approach, which indicates the importance of complete posterior soft tissue 29 . Because the door for the lateral approach is in the anterior‐lateral position, the actions required to open the door include adduction and external rotation. By contrast, the door for the P‐L approach is located on the posterior lateral side, and the actions required to open the door include flexion and internal rotation of the femur, which can be achieved by sitting or squatting and is commonly performed in daily activities. Therefore, it is reasonable that the lateral approach has a very low rate of dislocation.
Fig. 7.
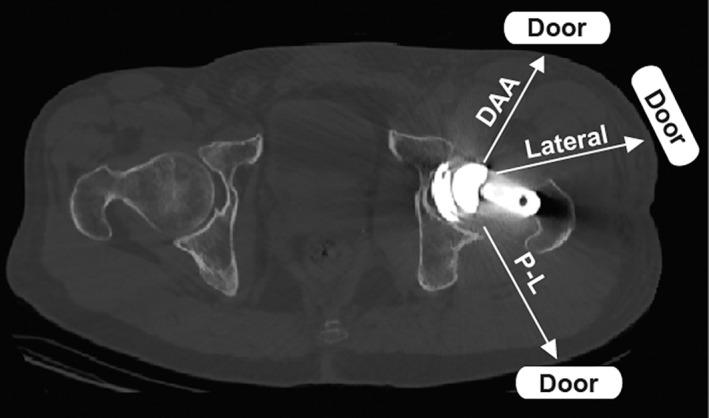
Schematic showing different “doors” with different approaches. DAA, direct anterior approach; P‐L, posterior‐lateral approach.
Different Approaches Exhibit Distinct Implant Orientations
One of most important factors influencing the stability of the hip is implant orientation. However, because the femur tends to dislocate from different “doors” after THA is performed using different approaches, different implant orientations may be required for the different approaches to prevent dislocation through weakened soft tissue. Therefore, it is worth investigating whether the implant orientation varies across various approaches. Anteversion angles in X‐rays taken in the standing position and supine position may differ due to changes in pelvic tilt; therefore, to minimize the effect of pelvic tilt, we compared our results with those from CT images taken in the supine position in previous studies (Table 1). Compared with previous reports, our study showed similar inclinations of the cup and anteversion angles of the stem, while the anteversion of the cup (9.26° ± 11.19°) and the combined anteversion (23.1° ± 13.4°) in our study were obviously smaller.
We also retrieved implant orientation from two studies in which the lateral approach was used, as illustrated in Table 3. Our measurements are similar but slightly smaller than the previously reported measurements. We think this discrepancy may be related to differences in the methods used to measure implant orientation and the surgeons' experience. Moreover, neither study investigated combined anteversion, which was shown in our study. However, we believe our implant orientation measurement is reasonable for THA using a lateral approach. Because highly anteverted cups and large angles of combined anteversion lead to an increased risk of anterior dislocation during THA and vice versa 8 , 9 , it is necessary to properly decrease the anteversion of the cup to prevent anterior dislocation. As mentioned above, decreased anteversion or combined anteversion angles will decrease the incidence of dislocation from the lateral “door.”
Table 3.
Implant orientation reported in two studies using the lateral approach
| Study | Measurement method | Inclination of cup | Anteversion of cup | Anteversion of stem | Combined anteversion | Dislocation | Approach |
|---|---|---|---|---|---|---|---|
| Wines et al. (2006) 24 | CT | NA | 16.2° (95% CI, 11.2°‐21.2°) | 12.9° (95% CI, 9.8°‐16.1°) | NA | NA | Hardinge (n = 31) |
| Goyal et al. (2016) 28 | Anteroposterior and lateral radiographs | 44.32° ± 7.0° | 21.8° ± 11.8° | NA | NA | 1/1010 | Hardinge (n = 1010) |
| Our study | CT | 38.83° ± 5.04° (24.5° to 53.1°) | 9.26° ± 11.19° (−15° to 48°) | 13.83° ± 10.7° (−10.2° to 42.3°) | 23.1° ± 13.4° (−7.4° to 54.6°) | 0/104 | Hardinge (n = 104) |
NA, not applicable.
Classic Safe Zone and Combined Anteversion May Not Be Suitable for THA Using the Lateral Approach
Interestingly, many studies have noted that THAs using the lateral approach may lead to a lower rate of implants being positioned properly in the Lewinnek safe zone than THAs using the P‐L approach, but THAs using the lateral approach lead to fewer dislocations 5 , 28 . We also found that only 52.9% of patients had measurements within the Lewinnek safe zone. In addition, we found that 44.2% of the hips had combined anteversion angles within the suggested zone (25°–50°) and there were no dislocations. However, we believe that these results further demonstrate that different approaches require different so‐called safe zones for joint stability; therefore, surgeons place implants with different orientations to stabilize the hip. In other words, surgeons performing THAs using the lateral approach place implants with a decreased cup anteversion on purpose. Therefore, on the basis of our results and those of previous reports, we conclude that the lateral approach may require smaller cup anteversion and combined anteversion angles to guide the operation.
Pelvic Tilt is the Only Contributor to Cup Anteversion
Pelvic tilt is the most important factor affecting cup anteversion. Several studies have reported that the degree of acetabular anteversion is related to pelvic tilt 10 , 21 , 30 , 31 . Lembeck reported that 1° of change in the pelvic tilt can lead to a change in the cup anteversion by approximately 0.7° 31 . Zhu et al. showed that each degree of change in pelvic tilt leads to a change in the cup anteversion by 0.8° 21 . However, their esults are based on changes in the same person. In our study, we found that pelvic tilt is the only contributor to cup anteversion. Moreover, our study investigated the effect of pelvic tilt on implant orientation in different persons and showed a 0.338° decrease in cup anteversion with each degree of change in pelvic tilt. This finding is important, especially for some patients with fixed pelvic tilt, such as those with late‐stage ankylosing spondylitis. Cases of fixed pelvic tilt require more accurate implant orientations. However, we found that pelvic tilt was not a contributor to the combined anteversion angle. In addition, age, sex, BMI, the size of the cup, and size of the femoral head did not affect the implant orientation. These results are also similar to those reported in previous studies 32 , 33 . Therefore, to place the cup accurately, it is essential to identify the pelvic tilt before THA is performed using a lateral approach or other approaches. On the basis of the above results, we recommend paying more attention to pelvic tilt during the operation to accurately place the implant and prevent dislocations.
Limitations
This study had a number of limitations. First, dislocation cases were not included because we did not observe any dislocation cases using this approach during the follow‐up period. Therefore, we cannot compare the implant orientations between patients with and without dislocation. Second, this was a retrospective study, which limits our ability to explore other factors that may affect implant orientation. Third, we did not have data from patients undergoing THA using the P‐L approach and could not compare the P‐L approach with the lateral approach in this study. However, combined anteversion has been investigated in several studies. The results comparing our data with previous reports using the P‐L approach should be sufficient to answer this question. Fourth, we did not have CT data from all of the followed patients for various reasons. Therefore, the range of implant orientation we reported cannot be concluded as a safe range because of the small sample size. However, we believe that the information on implant orientation from the 104 hips can mostly represent the group of 545 hips because there were no cases of dislocation and the same operative technique was used for all patients.
Conclusion
To the best of our knowledge, this is the first report of combined anteversion angles in THAs performed using the lateral approach. We found that the combined anteversion angle with the lateral approach may be smaller than that with the P‐L approach. In addition, pelvic tilt is an independent factor for cup anteversion. In the future, randomized controlled trials with large sample sizes using different approaches should be performed to elucidate the differences in implant orientations used with varied approaches.
Grant Sources: This work was supported by National Natural Science Foundation of China (81702660); Zhejiang Provincial Natural Science Foundation (LQ17C120002); Zhejiang Provincial Medical Health Science and Technology Plan Project (2017KY469) and Wenzhou Municipal Science and Technology Bureau funding (Y20180029, Y20170149).
Disclosures: All authors declare that they have no conflicts of interest.
References
- 1. Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet, 2007, 370: 1508–1519. [DOI] [PubMed] [Google Scholar]
- 2. Gwam CU, Mistry JB, Mohamed NS, et al Current epidemiology of revision total hip arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J Arthroplasty, 2017, 32: 2088–2092. [DOI] [PubMed] [Google Scholar]
- 3. Rowan FE, Benjamin B, Pietrak JR, Haddad FS. Prevention of dislocation after total hip arthroplasty. J Arthroplasty, 2018, 33: 1316–1324. [DOI] [PubMed] [Google Scholar]
- 4. Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip‐replacement arthroplasties. J Bone Joint Surg Am, 1978, 60: 217–220. [PubMed] [Google Scholar]
- 5. Callanan MC, Jarrett B, Bragdon CR, et al The John Charnley award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res, 2011, 469: 319–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res, 2009, 467: 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fujishiro T, Hayashi S, Kanzaki N, et al Computed tomographic measurement of acetabular and femoral component version in total hip arthroplasty. Int Orthop, 2014, 38: 941–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Murphy WS, Yun HH, Hayden B, Kowal JH, Murphy SB. The safe zone range for cup anteversion is narrower than for inclination in THA. Clin Orthop Relat Res, 2018, 476: 325–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fujishiro T, Hiranaka T, Hashimoto S, et al The effect of acetabular and femoral component version on dislocation in primary total hip arthroplasty. Int Orthop, 2016, 40: 697–702. [DOI] [PubMed] [Google Scholar]
- 10. Yang G, Li Y, Zhang H. The influence of pelvic tilt on the anteversion angle of the acetabular prosthesis. Orthop Surg, 2019, 11: 762–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Migliorini F, Eschweiler J, Trivellas A, et al Implant positioning among the surgical approaches for total hip arthroplasty: a Bayesian network meta‐analysis. Arch Orthop Trauma Surg, 2020, 140: 1115–1124. 10.1007/s00402-020-03448-w. [DOI] [PubMed] [Google Scholar]
- 12. Fleischman AN, Tarabichi M, Magner Z, Parvizi J, Rothman RH. Mechanical complications following total hip arthroplasty based on surgical approach: a large, single‐institution cohort study. J Arthroplasty, 2019, 34: 1255–1260. [DOI] [PubMed] [Google Scholar]
- 13. Demos HA, Rorabeck CH, Bourne RB, MacDonald SJ, McCalden RW. Instability in primary total hip arthroplasty with the direct lateral approach. Clin Orthop Relat Res, 2001, 393: 168–180. [DOI] [PubMed] [Google Scholar]
- 14. Petis S, Howard JL, Lanting BL, Vasarhelyi EM. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg, 2015, 58: 128–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kubota Y, Kaku N, Tabata T, Tagomori H, Tsumura H. Efficacy of computed tomography‐based navigation for cup placement in revision total hip arthroplasty. Clin Orthop Surg, 2019, 11: 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhu B, Su C, He Y, et al Combined anteversion technique in total hip arthroplasty for Crowe IV developmental dysplasia of the hip. Hip Int, 2017, 27: 589–594. [DOI] [PubMed] [Google Scholar]
- 17. Yoshimine F. The safe‐zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech, 2006, 39: 1315–1323. [DOI] [PubMed] [Google Scholar]
- 18. Zhang J, Wang L, Mao Y, Li H, Ding H, Zhu Z. The use of combined anteversion in total hip arthroplasty for patients with developmental dysplasia of the hip. J Arthroplasty, 2014, 29: 621–625. [DOI] [PubMed] [Google Scholar]
- 19. Nakashima Y, Hirata M, Akiyama M, et al Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop, 2014, 38: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chang JD, Kim IS, Prabhakar S, Mansukhani SA, Lee SS, Yoo JH. Revision total hip arthroplasty using imageless navigation with the concept of combined anteversion. J Arthroplasty, 2017, 32: 1576–1580. [DOI] [PubMed] [Google Scholar]
- 21. Zhu J, Wan Z, Dorr LD. Quantification of pelvic tilt in total hip arthroplasty. Clin Orthop Relat Res, 2010, 468: 571–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bargar WL, Jamali AA, Nejad AH. Femoral anteversion in THA and its lack of correlation with native acetabular anteversion. Clin Orthop Relat Res, 2010, 46: 527–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br, 1970, 52: 148–159. [PubMed] [Google Scholar]
- 24. Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty, 2006, 21: 696–701. [DOI] [PubMed] [Google Scholar]
- 25. Wassilew GI, Perka C, Koenig C, Janz V, Asbach P, Hasart O. 3D CT analysis of combined cup and stem anteversion in cases of cup navigation in hip arthroplasty. Orthopedics, 2010, 33: 48–51. [DOI] [PubMed] [Google Scholar]
- 26. Tsai TY, Dimitriou D, Li G, Kwon YM. Does total hip arthroplasty restore native hip anatomy? Three‐dimensional reconstruction analysis. Int Orthop, 2014, 38: 1577–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res, 2002, 405: 46–53. [DOI] [PubMed] [Google Scholar]
- 28. Goyal P, Lau A, McCalden R, Teeter MG, Howard JL, Lanting BA. Accuracy of the modified Hardinge approach in acetabular positioning. Can J Surg, 2016, 59: 247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. Does surgical approach affect total hip arthroplasty dislocation rates?. Clin Orthop Relat Res, 2006, 447: 34–38. [DOI] [PubMed] [Google Scholar]
- 30. McCarthy TF, Nevelos J, Elmallah RK, et al The effect of pelvic tilt and femoral head size on hip range‐of‐motion to impingement. J Arthroplasty, 2017, 32: 3544–3549. [DOI] [PubMed] [Google Scholar]
- 31. Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop, 2005, 76: 517–523. [DOI] [PubMed] [Google Scholar]
- 32. Bosker BH, Verheyen CC, Horstmann WG, Tulp NJ. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg, 2007, 127: 375–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Todkar M. Obesity does not necessarily affect the accuracy of acetabular cup implantation in total hip replacement. Acta Orthop Belg, 2008, 74: 206–209. [PubMed] [Google Scholar]


