Abstract
Hip arthroscopy has been increasingly used to treat labral tears and cam and pincer lesions found in femoroacetabular impingement. Although the classic impingement with cam deformity at the proximal femoral anterolateral quadrant is most common, there has been evidence of cam impingement extension to the anteromedial and posterior quadrants of the proximal femur. Posterior cam decompression carries a theoretical risk of vascular insult and subsequent osteonecrosis, which have led investigators to approach these posterior lesions through an open surgical correction. Recent improvements have led to the development of pre-bent burs that allow for bonier resection flexibility. Here, we report on an arthroscopic posterior cam decompression using the traditional anterior portals and curved hip burs via a figure-of-four positioning technique.
Femoroacetabular impingement (FAI) is a common cause of hip pain and disability in younger adults and is linked to worsening cartilage and labral damage when left untreated.1 This chondrolabral damage is due to the mechanical impaction of the proximal femur with the rim of the acetabulum. Classifications include cam, pincer, or mixed type. Cam deformity is described as a bony offset prominence at the anterolateral portion of the femoral head–neck region. Radiologically, cam lesions are characterized by decreased femoral head–neck offset (<7 mm), head–neck offset ratio, femoral head asphericity, osseous bumps, pit herniations, triangular index,2 and wide alpha angles. A large alpha angle is a key radiologic finding in cam FAI, is often greater than 65°,3 leads to chondrolabral damage, and can be found in other conditions. Increased femoral head coverage, which is measured by lateral central edge angle, may protect against acetabular cartilage damage.3
Previous studies have shown that cam deformity can extend to the anteromedial and posterior femoral head regions.4,5 Osteoplasty at this particular region, otherwise known as the anteromedial “critical corner,” can improve internal rotation of the flexed hip. However, this comes at a risk of causing iatrogenic damage to the primary vascular supply to the femoral head, the retinacular vessels from the ascending branch of the medial femoral circumflex artery. A vascular safe zone has been studied and was found anterior to the mid-coronal plane of the superior femoral neck.4 During arthroscopy, the posterior-most aspect is the lateral synovial fold. Due to the risk of vascular insult, it has been suggested that patients with posterior cam lesions should be treated with an open surgical dislocation rather than a hip arthroscopy.5 This has proposed the advantages of direct visualization for a safe femoral osteoplasty to minimize femoral head osteonecrosis and fracture. Open surgical dislocation comes with a larger incision and potential complications from trochanteric nonunion, heterotopic ossification, neuropraxia, and residual abductor weakness. Other surgeons advocate the use of arthroscopic techniques. Among these techniques are additional portal placements, namely a posterolateral portal, which has increased risk for injury at the sciatic nerve, an approach that works from anterior to lateral to posterior, as described by Matsuda and Hanami,6 or use of a medial portal, as described by Polesello et al.7
We present a strategy that uses the traditional modified anterior and anterolateral portals, but with the addition of a pre-bent bur. This technique also allows for dynamic testing to test the resection and reduce the risk of persistent impingement. If the surgeon remains proximal to the posterolateral retinacular vessels, one can safely decompress the posterior cam lesion.
Technical Note
Indications and Patient Evaluation
At the time of the initial presentation, the patient was a 15-year old preprofessional female ballet dancer who started having bilateral hip pain for 15 months. She tried several months of physical therapy, along with cortisone injections, but the pain continued. On physical examination, the patient could touch her palms to the floor, but no other Beighton’s signs were noted. She had hip pain at 105° of flexion bilaterally. Her internal rotation was 5° right hip, and 10° left. Her external rotation was 80° right, and 85° left. She had internal snapping hip bilaterally. She had a positive impingement test on both hips.
Imaging
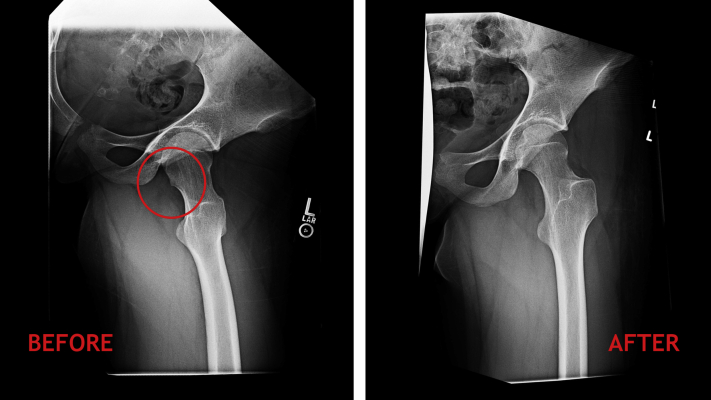
On radiographs, the patient had a cam impingement bilaterally, with alpha angle 56°. On both hips, there were also symmetric posterior cam lesions (Fig 1). On magnetic resonance imaging, the patient had typical bilateral anterior labral tears, and the posterior cam lesions are clearly visible on the axial obliques. After not responding to conservative treatment, she was indicated for hip arthroscopy, osteoplasty, and labral repair.
Fig 1.
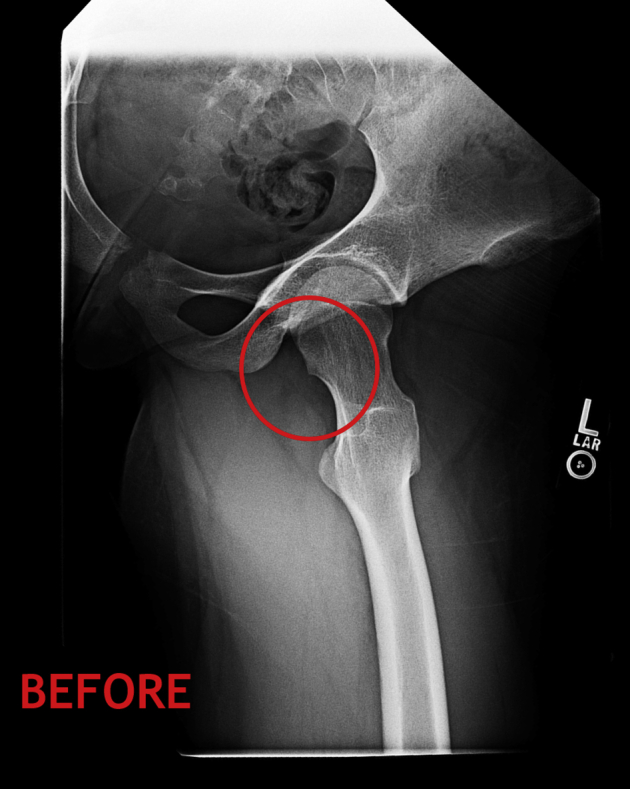
Detail of preoperative frog-leg lateral radiograph of a 16-year-old female patient with symptomatic femoroacetabular impingement. One should note the posterior cam deformity (red circle) that is causing posterior impingement.
Surgical Technique (With Video Illustration)
After induction of general anesthesia, the patient is positioned supine. All bony prominences are well padded, and a well-padded peroneal post is used (Fig 2). Standard anterolateral and mid-anterior portals are used with fluoroscopic guidance and hip distraction via a shaver and radiofrequency probe. A slotted cannula facilitates the switching of portals. An arthroscopic pump is used with pressures around 50 mm Hg with hypotensive general anesthesia. An interportal capsulotomy is performed via a shaver and radiofrequency probe. After central compartment hip arthroscopy, pincer resection and standard labral repair, the hip is taken out of traction and flexed to 40°. Traction sutures are placed in the inferior capsule through both the mid-anterior and anterolateral portals in the peripheral compartment, to facilitate exposure.8
Fig 2.
Surgical table set up for hip arthroscopy. If the nonoperative leg is abducted, the fluoroscopy machine can be positioned between the legs. This makes it easier to get oblique or lateral radiographs, without the other hip superimposed, if needed.
After standard pincer acetabuloplasty and anterolateral cam osteoplasty with a 5.5-mm burr, the posterior cam lesion is addressed (Figs 2 and 3, Table 1). The boot is released from the traction device. The patient’s operative leg is then placed in flexion and maximal external rotation (figure-of-4 position) (Fig 4), with the 70° arthroscope placed through the anterolateral portal and a pre-bent burr (Conmed, Largo, FL) through the midanterior portal (Fig 5). This extreme external rotation, along with the convexity of the pre-bent burr, allows exposure of the medial femoral neck and allows decompression of the cam lesion (Fig 6). The zona orbicularis is adjacent to the curved burr during this part of the procedure. The curved burr is essential for this portion of the procedure since it allows easier contact to the bone from the midanterior portal. As the posterior cam lesion decompression progresses, one is able to obtain progressive external rotation of the hip. Care is taken to avoid inadvertent damage to the posterolateral retinacular vessels. Fluoroscopic confirmation on anteroposterior view with neutral and external/internal hip rotation allows arthroscopic confirmation of posterior cam decompression. Video 1 and Table 2 highlight key principles and technical pearls of this technique for arthroscopic posterior cam decompression.
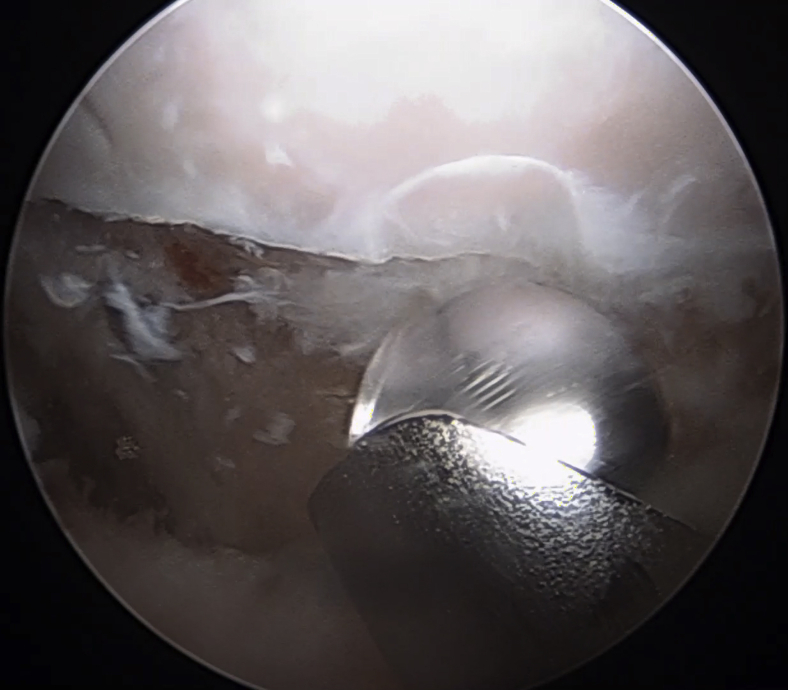
Fig 3.
Supine arthroscopic view with a 70° arthroscope of a patient’s left hip viewed from the midanterior portal detailing the anterior cam osteoplasty. The femoral head cartilage is noted at the top of the figure. At the bottom of the figure, a 5.5-mm burr through the anterolateral portal is used to perform the osteoplasty.
Table 1.
Keys to Arthroscopic Posterior Femoroplasty With Anteriorly Based Pre-bent Hip Burrs
| Step | Procedure | Rationale |
|---|---|---|
| 1 | Central compartment hip arthroscopy Perform acetabuloplasty and labral repair, if indicated |
|
| 2 | Release traction device, flex hip to ∼40° Peripheral compartment entered and traction sutures applied (anteriorly and laterally) Anterolateral cam resection |
|
| 3 | Place hip in flexion and maximal external rotation (figure-of-4 position) 70° arthroscope through anterolateral portal with pre-bent burr in mid anterior portal |
|
| 4 | Dynamic and fluoroscopic testing post-resection |
|
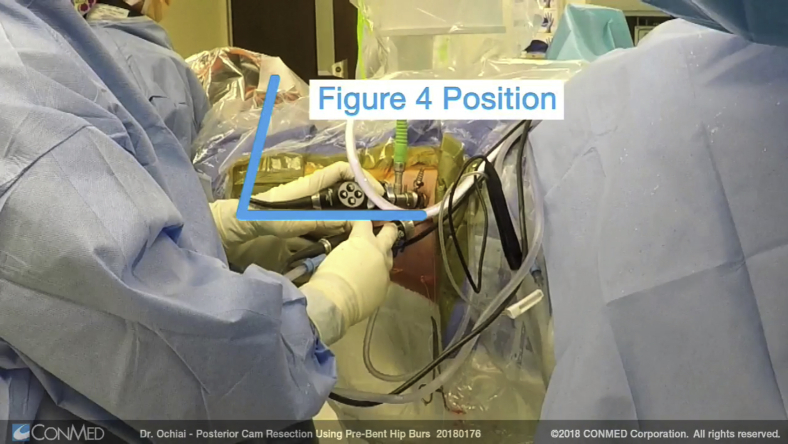
Fig 4.
Depiction of leg positioning using the figure 4 position to access the medial aspect of the femoral neck to subsequently gain exposure to the posterior cam lesion.
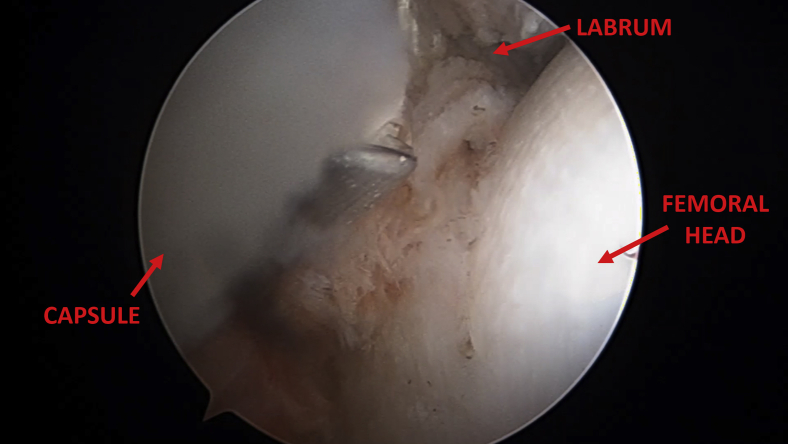
Fig 5.

Supine arthroscopic view with a 70° arthroscope of a patient’s left hip viewed from the anterolateral portal directed posteriorly. A curved hip bur is used from a mid-anterior portal to start the posterior cam osteoplasty. The adjacent zona orbicularis is shown for reference.
Fig 6.
Supine arthroscopic view with a 70° arthroscope of a patient’s central compartment left hip viewed from the anterolateral portal detailing the intra-articular capsulotomy. Capsule is labeled in the left side of the image and the femoral head is identified on the right half of the image. A generous interportal capsulotomy can allow the curved burr easier access.
Table 2.
Pearls and Pitfalls of Arthroscopic Posterior Femoroplasty With Anteriorly Based Pre-bent Hip Burrs
| Pearls | Pitfalls |
|---|---|
| Make a generous transverse capsulotomy, which can be closed at the end of the case | If on preoperative physical examination the patient cannot get at least 75° of external rotation in a FABER position, anticipate that this approach will be difficult, and probably require a larger capsulotomy. |
| Most traction devices allow some flexion and extension of the hip. Fine tune exposure by adjusting the hip flexion in the figure of four position | Avoid the temptation to do this as a radiographic only procedure. Since the femoral head is a 3-dimensional sphere, using 2-dimensional radiograph alone risks injury to femoral head articular cartilage. |
| If there is any disorientation, do not hesitate to use a single shot of fluoroscopy to help with orientation | If it is relatively easy to access the posterior aspect of the hip through this approach, be highly suspicious for capsular laxity. Even if you traditionally do not suture close or plicate the capsule, in this situation, strongly consider closing the capsule. |
FABER, flexion abduction external rotation.
Rehabilitation
The patient followed a standard postoperative rehabilitation, without alteration. The patient was weight bearing as tolerated immediately. Passive circumduction exercises were begun immediately. She was in a postoperative hip brace for one month after surgery. Postoperative radiographs show both normal femoral head–neck offset along with elimination of the posterior cam lesion (Fig 7). Formal physical therapy starts 2 weeks after surgery. Return to sport commences after 3 months if the hip is pain free and having normal strength and range of motion.
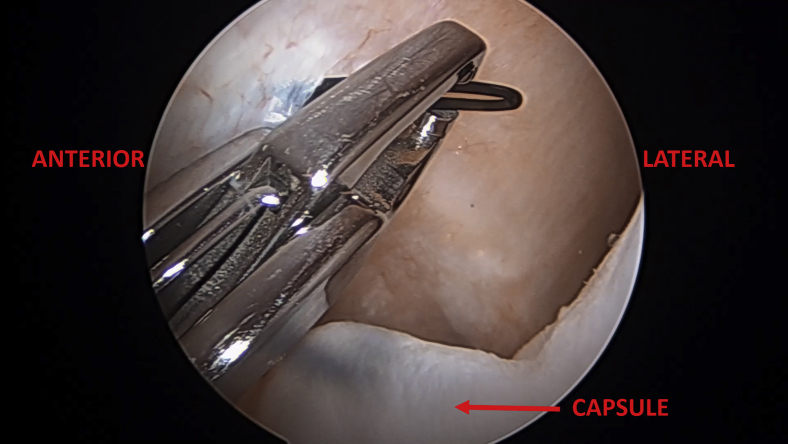
Fig 7.
Supine arthroscopic view with a 70° arthroscope of a patient’s left hip viewed from the anterolateral portal detailing the traction sutures placed around the inferior capsule. The anterior hip is labeled on the left side of the figure whereas the lateral part of the hip joint is labeled on the right side of the figure. The traction sutures allow the inferior capsule to be peeled away from the field, allowing better visualization for the anterior and posterior cam osteoplasty.
Discussion
Posterior cam FAI lesions provide a challenge to surgeons due to the proximity of vascular structures. Several approaches exist for the treatment of these posterior lesions. Arthroscopic techniques for osteoplasty of posterior cam lesions have the potential to efficiently and safely resect these posterosuperior bony lesions. To our knowledge, this is the first report in the literature describing the technique of an arthroscopic posterior cam resection using a pre-bent bur and the standard mid-anterior and anterolateral portals. This method allows the surgeon to use standard anterior hip arthroscopy portals while using a curved bur to resect previously difficult to reach areas. Due to the curvature of the bur, there is also improved visualization of the working field. Another advantage is that dynamic testing can be done intraoperatively and can aid in decreasing postoperative persistent impingement. Arthroscopic posterior cam resection is not a common procedure, so a true complication rate is not quantifiable. There have been no reported instances of osteonecrosis after such a procedure. Osteonecrosis after hip arthroscopy can be due to several factors related to hip joint surgery, including traction on the vessels, direct injury to the vessels, and raised intra-articular pressure. One limitation of our technique is that is requires the use of a specialized curved hip burr which is an added expense. Another limitation is that it is necessary to have an assistant diligently hold the leg in the figure-4 position during the posterior cam resection. Lastly, the use of this technique may require a larger capsulotomy than usual and may require a longer and more vigilant capsular closure.
Other current arthroscopic methods of posterior cam resection involve the posterolateral portal or the modified mid-anterior portal. The posterolateral portal is located on average 2.9 cm from the sciatic nerve at the level of the hip capsule and is 4.4 cm from the superior gluteal nerve. The portal is also located superior and anterior to the piriformis tendon, which is, on average, 5 mm average from the ascending cervical branch of the medial femoral circumflex artery, the main artery supplying the femoral head. A surgeon may choose to avoid the posterolateral portal for these reasons,9 but sometimes this portal is suggested when addressing posterior hip lesions such as posterior cam lesions.
Matsuda and Hanami6 described one strategy for posterior cam decompression, and it was performed without the posterolateral portal, using a modified mid-anterior portal. He described accessing a posterolateral cam lesion with extension and internal rotation, and the osteoplasty was performed proximal to the lateral retinacular vessels. Upon review of the images in this paper, the resection was more lateral than the lesion described in this paper. Essentially, the lesion was accessed laterally, while we describe accessing the lesion medially. Both methods can be useful, and in some instances, a combination of accessing a lesion around the lateral side and accessing around the medial side may be required.
A medial portal also can be used for posterior cam resection, as described by Polesello et al.7 While this may obviate the need for a curved burr, this portal is not a standard portal for hip arthroscopy, and it does come close to the obturator nerve and profunda femoris artery.
Previously, limitations of arthroscopy were due to difficulty in removing bony prominences on the femur that extend to the posterior neck. Hybrid techniques to surgery use arthroscopy but add an additional limited-open approach. They do not require dislocation; however, they do not address circumferential lesions and, notably, posterior lesions. The technique described in this report avoids the morbidity of an open surgical dislocation and uses standard anterior portals. We believe that direct arthroscopic visualization of the vessels with a controlled femoroplasty of the medial and even posterior femoral head–neck junction is a feasible and safe procedure using this method. This provides an alternative to open surgical dislocation, which carries the risk of trochanteric non-union, greater incidence of heterotopic ossification formation and neuropraxia, abductor weakness, and possible future removal of hardware. This also avoids potential trauma to the lateral retinacular vessels from a posterolateral portal and approach. This also avoids a medial portal, which can put the femoral artery and nerve at risk. Most cam lesions do not require any of the aforementioned techniques, but in the challenging posterior cam lesion, this arthroscopic anterior approach to the posterior femoral neck is feasible and should be considered (Figs 8 and 9, Table 3).
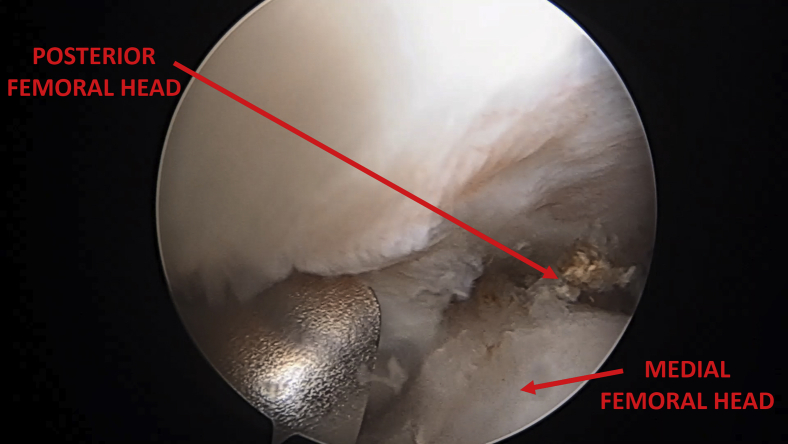
Fig 8.
Supine arthroscopic view with a 70° arthroscope of a patient’s left hip viewed from the anterolateral portal directed posteriorly. Another view of the posterior cam osteoplasty. The curved burr is medial, and with the increased external rotation of the figure-of-four position, the posterior femoral head is able to be accessed. The posterior femoral head and medial femoral head are labeled for reference.
Fig 9.
Preoperative and postoperative frog-leg lateral radiographs showing the osteoplasty of the posterior cam lesion. On the left, the posterior cam lesion (red circle) is delineated. On the right, the posterior cam lesion is adequately resected.
Table 3.
Advantages and Disadvantages of Arthroscopic Posterior Femoroplasty With Anteriorly Based Pre-bent Hip Burrs
| Advantages | Disadvantages |
|---|---|
| Uses traditional portals that are familiar to hip arthroscopy surgeons. | Requires a dedicated assistant to leg positioning during the figure of four portion of the procedure. |
| Can be done through 2 portals, which is more cosmetic. | Requires use of a curved burr. |
| Avoids a medial portal, which can put the femoral artery and nerve at more risk. | May require a larger capsulotomy than normally performed, which may require a longer closure time. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.O. reports consultant for Conmed. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Anterior arthroscopic approach for posterior cam lesion resection. Standard midanterior and anterolateral portals are used and the central compartment arthroscopy with pincer resection and labral repair are first addressed. The peripheral compartment is entered and traction sutures are placed in the inferior capsule to improve visualization. After anterolateral cam resection, the hip is flexed and maximally externally rotated (figure-of-four position) to allow for visualization of the posterior cam lesion with a 70° arthroscope. A curved bur is used to resect this posterior cam lesion, with care taken to note of the posterolateral retinacular vessels. As the resection progresses, one is able to progressively externally rotate to further resect the posterior cam lesion. Adequate osteoplasty is achieved.
References
- 1.Wang D, Marx R. Femoroacetabular impingement. J Bone Joint Surghttps://www.jbjs.org/summary.php?id=248.
- 2.Gosvig K.K., Jacobsen S., Palm H., Sonne-Holm S., Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89:1309–1316. doi: 10.1302/0301-620X.89B10.19405. [DOI] [PubMed] [Google Scholar]
- 3.Beaulé P.E., Hynes K., Parker G., Kemp K.A. Can the alpha angle assessment of cam impingement predict acetabular cartilage delamination? Clin Orthop Relat Res. 2012;470:3361–3367. doi: 10.1007/s11999-012-2601-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCormick F., Kleweno C.P., Jo Kim Y., Martin S.D. Vascular safe zones in hip arthroscopy. Am J Sports Med. 2011;39(suppl 1):64–71. doi: 10.1177/0363546511414016. [DOI] [PubMed] [Google Scholar]
- 5.Jäger M., Bittersohl B., Zilkens C. Surgical hip dislocation in symptomatic cam femoroacetabular impingement: What matters in early good results? Eur J Med Res. 2011;16:217–222. doi: 10.1186/2047-783X-16-5-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuda D.K., Hanami D. Hip arthroscopy for challenging deformities: Posterior cam decompression. Arthrosc Tech. 2013;2:e45–e49. doi: 10.1016/j.eats.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Polesello G.C., Omine Fernandes A.E., de Oliveira L.P., Tavares Linhares J.P., Queiroz M.C. Medial hip arthroscopy portals: An anatomic study. Arthroscopy. 2014;30:55–59. doi: 10.1016/j.arthro.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Thakral R., Ochiai D. Arthroscopic technique for treatment of combined pathology associated with femoroacetabular impingement syndrome using traction sutures and a minimal capsulotomy. Arthrosc Tech. 2014;3:e527–e532. doi: 10.1016/j.eats.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sussmann P.S., Zumstein M., Hahn F., Dora C. The risk of vascular injury to the femoral head when using the posterolateral arthroscopy portal: Cadaveric investigation. Arthroscopy. 2007;23:1112–1115. doi: 10.1016/j.arthro.2007.05.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anterior arthroscopic approach for posterior cam lesion resection. Standard midanterior and anterolateral portals are used and the central compartment arthroscopy with pincer resection and labral repair are first addressed. The peripheral compartment is entered and traction sutures are placed in the inferior capsule to improve visualization. After anterolateral cam resection, the hip is flexed and maximally externally rotated (figure-of-four position) to allow for visualization of the posterior cam lesion with a 70° arthroscope. A curved bur is used to resect this posterior cam lesion, with care taken to note of the posterolateral retinacular vessels. As the resection progresses, one is able to progressively externally rotate to further resect the posterior cam lesion. Adequate osteoplasty is achieved.