Abstract
Physical examination in the presence of a multiligament knee injury can be complex and challenging. Hence, stress radiography is a useful and inexpensive tool that is widely used in the assessment of this type of injury. It guarantees an objective analysis of the magnitude of knee instability, which may reduce the observer's interpretation bias in relation to the physical examination. However, for the radiographic analysis to be reproducible, it is necessary to standardize the technique to evaluate each of the main knee ligaments. This article aims to describe in detail how to perform stress radiography to assess the sufficiency of the posterior cruciate ligament and collateral ligaments in the context of a multiligament injury.
In the presence of a multiligament lesion, physical examination is sometimes inaccurate and barely reproducible. The examiner's experience, the patient's pain tolerance, and the concomitance of other lesions are factors that alter the reliability and reproducibility of the physical examination.1, 2, 3
Stress radiography is a very useful and inexpensive complementary examination, capable of showing the magnitude of knee instability in an objective and quantifiable way, and can assist in preoperative decision making; it is also of great value in the postoperative follow-up of multiligament injuries.4, 5, 6, 7, 8 Even magnetic resonance imaging (MRI), which is capable of diagnosing acute and chronic ligament injuries, may be interpreted inaccurately and may be unable to indicate the degree of ligament instability. Thus, stress radiography remains important, even in the face of more modern technologies.9
Ideally, the interpretation of stress radiography should always be based on the contralateral knee, as long as it does not also present multiligament injury.10,11 Despite being a widely used tool for the evaluation of knee ligament injuries,12,13 the radiologic protocol for posterior, varus, and valgus displacement assessment lacks standardization in relation to limb positioning and stress application.
Several studies have debated what method is best to objectively measure the degree of instability, which instruments could be used to perform stress (manual or computerized arthrometers, hydraulic or spring devices, and even manual force), and which parameters should be used to interpret the results (degree of openness and degree of translation, as well as from which points).4,6,8,14, 15, 16, 17, 18, 19 In the face of a multiligament injury, accurate diagnosis is a difficult task for the surgeon, who must seek all the tools available for this purpose.9 This work aims to describe in detail how to perform stress radiography to assess the sufficiency of the cruciate and collateral ligaments in the context of a multiligament injury and, in this way, to make the performance and interpretation of the examination reproducible and reliable.
Technique
Varus and Valgus Stress at 20°
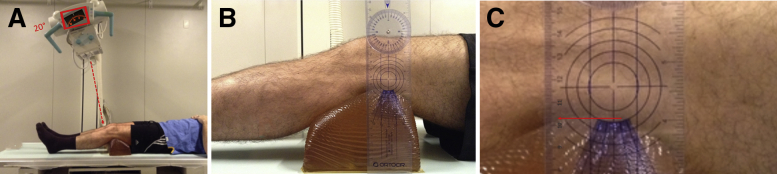
The patient must be dressed in shorts with the distal third of the thigh fully exposed. First, we position the patient at the end of the radiographic table to facilitate stress maneuvers of the knee. Then, we tilt the x-ray ampule 20° cephalic (Fig 1A), which is the same angle at which the knee should be flexed.17,18
Fig 1.
(A) The patient is placed in the supine position with the x-ray ampule angled at about 20° cephalic. Red rectangle shows a zoom of the degree of the angulation of the x-ray ampule. Red arrow simulates the direction of the x-ray. (B) The knee is flexed at 20°. To obtain this flexion, we place a radiotransparent cushion posterior to the knee. (C) The cushion should be approximately 10 cm height (red line).
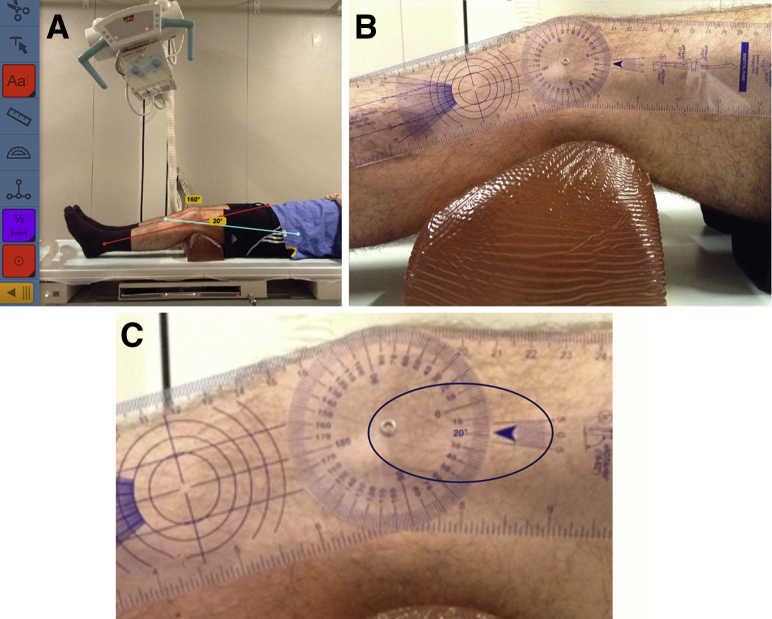
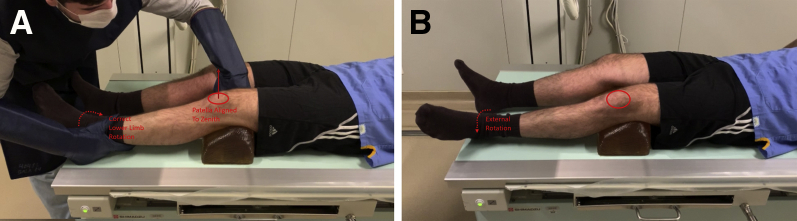
To obtain this flexion angle, we place a radiotransparent cushion posteriorly to the knee. This cushion should be approximately 10 cm high (Fig 1 B and C) in patients of medium stature (around 1.70 m). The knee flexion angle should be assessed to determine whether the desired angle is correct. For this verification, we recommend taking a lateral picture of the knee and measuring the knee angle with the Bone Ninja application (Sinai Hospital of Baltimore) (Fig 2A) or using a traditional goniometer (Fig 2 B and C) applied directly to the knee. Another precaution involves the control of lower limb rotation, which can be obtained by controlling the alignment of the patella to be directly vertical (Fig 3A). In this way, any external or internal rotation must be corrected before the varus and valgus stress maneuvers (Fig 3B). After the aforementioned steps are verified, we identify the joint line.
Fig 2.
The patient is lying in the supine position. The knee flexion angle is assessed by evaluating whether the desired angle is correct. For this verification, we recommend taking a lateral photograph of the knee and measuring the knee angle with the Bone Ninja application (A), or a traditional goniometer can be used (B, C). In panel A, the blue line represents the center of the long axis of the femur viewed in lateral view. The red line represents the center of the long axis of the tibia viewed in lateral view. In panel C, the blue oval represents a zoom of the numerical representation of the measured angle.
Fig 3.
The patient is lying in the supine position. (A) The lower limb must be in neutral rotation, so we must observe whether the patella is aligned directly vertical. (B) Any external or internal rotation must be corrected before the varus and valgus stress maneuvers are performed. Red oval represents the patella.
To obtain images under varus stress, the examiner applies pressure with his or her ipsilateral fist over the medial epicondyle of the distal femur, at the knee joint, while placing his or her other hand on the distal extremity of the limb, at ankle level, and a maximum varus stress maneuver is performed, aiming to increase the lateral femorotibial space of the examined knee. A radiographic image is obtained and evaluated.
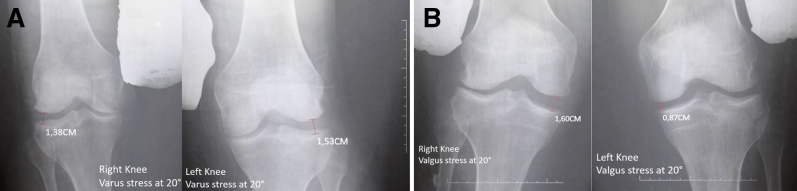
Then, the valgus stress maneuver is performed by pressing the contralateral hand on the lateral epicondyle of the distal femur, at the knee, while the other hand is positioned on the distal extremity of the limb, at the ankle, aiming to achieve maximum stress to obtain opening of the medial femorotibial space. A radiographic image is obtained and analyzed. Image quality must be analyzed after each radiograph is taken (Fig 4).
Fig 4.
(A) Radiographs with varus stress with the knee flexed at 20°, showing lateral femorotibial opening measurements of 1.38 cm on the right side and 1.53 cm on the left side. (B) Radiographs with valgus stress with the knee flexed at 20°, showing a 1.60-cm medial femorotibial opening in the right knee and 0.87-cm medial femorotibial opening in the left knee.
Varus and Valgus Stress at 0°
The posterior cushion is removed; the x-ray ampule is positioned at 0°, and the joint line is identified. The examiner applies pressure with his or her ipsilateral fist over the medial epicondyle of the distal femur, at the knee, while placing his or her other hand on the distal extremity of the limb, at the ankle, using maximum stress force, aiming to increase the lateral femorotibial space of the examined knee. Radiographic imaging is performed and analyzed. Then, the valgus stress maneuver is performed by supporting the contralateral hand on the lateral epicondyle of the distal femur, at the knee, while the other hand is on the distal extremity of the limb, at the ankle, aiming to achieve maximum stress by opening the medial femorotibial space (Fig 5).
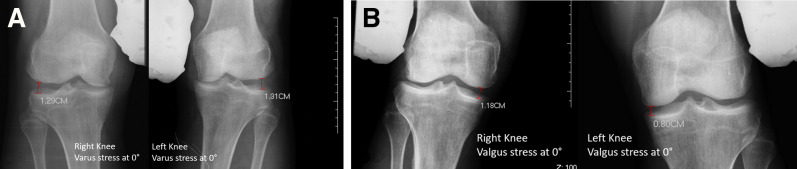
Fig 5.
(A) Radiographs with varus stress with the knee at 0°, showing lateral femorotibial opening measurements of 1.29 cm in the right knee and 1.31 cm in the left knee. (B) Radiographs with valgus stress with the knee at 0°, showing a 1.18-cm medial femorotibial opening in the right knee and 0.80-cm medial femorotibial opening in the left knee.
Image Evaluation After Stress Maneuvers
The images are uploaded into the software mDicomViewer (Microdata Tecnologia), and the degree of femorotibial space opening is measured and compared. The opening measurements for both the varus and valgus stress tests are obtained at the most distal point of the femur and its corresponding point in the tibial plateau (Figs 4 and 5).17,18
Assessment of Ligamentous Sufficiency of Lateral Collateral Ligament
With the knee flexed at 20°, an increase in lateral joint space greater than 2.7 mm in relation to the contralateral knee indicates an isolated lesion of the lateral collateral ligament. When the opening is larger than 4.0 mm, an associated posterolateral corner lesion should be suspected.17
Assessment of Ligamentous Sufficiency of Medial Collateral Ligament
Valgus stress is applied with maximum stress by the examiner with the knee fully extended, at 0°, and flexed at 20°. An opening of the medial joint space greater than 1.7 mm at 0°, as compared with the contralateral side, indicates a posterior capsular lesion, whereas an opening greater than 3.2 mm at 20° indicates a lesion of the medial collateral ligament,18 as shown in Fig 4B.
Kneeling-View Method
The patient is kept in the same kind of clothing previously mentioned. To carry out the kneeling-view method, we require a thick, soft cushion; a 2- to 3-step mobile ladder; and a straight support surface (100 × 550 cm) that can be fixed in the desired location, serving as an anterior support (Fig 6A). These items are positioned in front of the x-ray film. The x-ray light bulb is positioned angled perpendicular to the film. The knee to be evaluated must be as close as possible to the film and flexed 90°, with the thigh fully supported by the aforementioned straight support surface. The contralateral limb must be inclined posteriorly with partial proprioceptive load on the ground, aiming to leave the entire body weight on the knee to be examined (Fig 6B).20
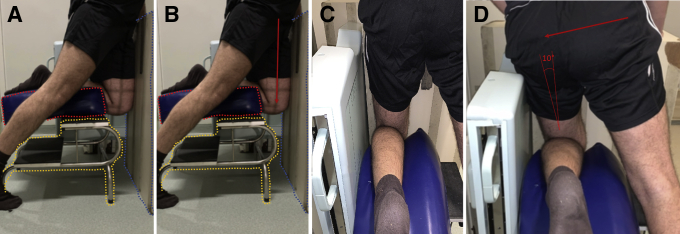
Fig 6.
The patient is kneeling on the affected knee. (A) A thick, soft cushion is required (dotted red line), in addition to a 2- to 3-step mobile ladder (dotted yellow line) and a straight support surface (dotted blue line) that can be fixed in the desired location, serving as an anterior support; this structure must be approximately 1 m high and 50 cm wide. These items are positioned in front of the x-ray film. The x-ray light bulb is positioned angled perpendicular to the film. (B) The knee to be evaluated must be the one closest to the film, being flexed at 90°, with the thigh fully supported by the aforementioned straight support surface. The contralateral limb must be inclined posteriorly with partial proprioceptive load on the ground, aiming to leave the entire body weight on the knee to be examined. Red arrow indicates that the patient must let the body weight fall on the flexed member. (C, D) The patient must lean his or her body 10° toward the examined side, with the aim of the condyles being superimposed in the image examination. In panel D, the red arrow shows that the patient must lean sideways by about 10° to the affected side.
The patient must rotate his or her body 10° toward the examined side, with the aim of the condyles being superimposed in the image examination (Fig 6 C and D). After verification of these steps, the radiograph is obtained (Video 1). The procedure is repeated for the contralateral knee, only inverting the ladder and the local support surface.
Image Evaluation After Kneeling-View Method
For the correct evaluation of the images, the femoral condyles must be completely overlapped. The images are uploaded in the software mDicomViewer, and the degree of posterior tibial translation is measured and compared.
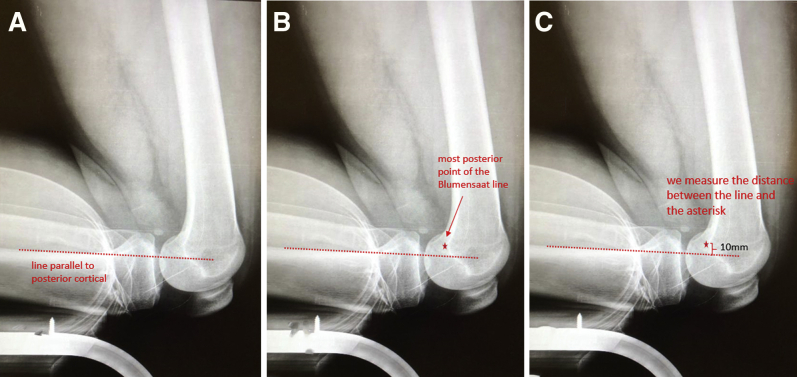
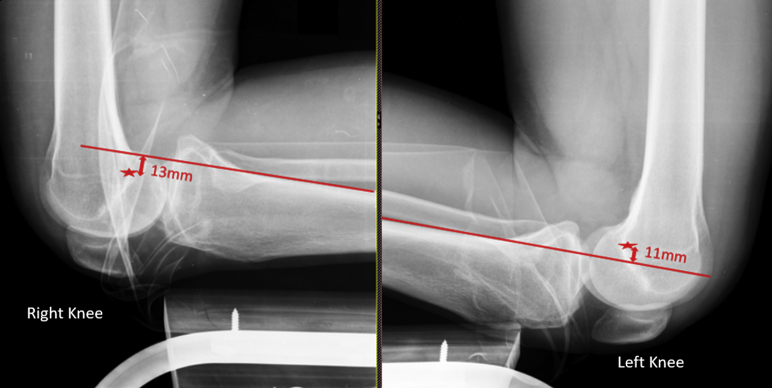
A line is drawn parallel to the posterior tibial cortex (Fig 7A), identifying the most posterior point on the Blumensaat line (Fig 7B), and the distance between this line and this point is assessed (Fig 7C). Comparisons are performed side to side. A difference in posterior tibial translation of greater than 7 mm between the knees indicates a complete lesion of the posterior cruciate ligament,15,20, 21, 22 as observed in Fig 8.
Fig 7.
We draw a line parallel to the posterior tibial cortex (red dotted line) (A) and identify the most posterior point on the Blumensaat line (star) (B). (C) We then assess the distance between this line and this point (red bracket).
Fig 8.
Side-by-side comparison is performed. A clear difference is observed between the knees, with posteriorization of the tibia on the right side compared with the left side. In panel A, the red line is parallel to posterior cortical. In panel B, the red star shows the most posterior point of the Blumensaat line. The distance between the line and red star was measured.
Discussion
Multiligament injury is a rare and complex pathology, with varied trauma mechanisms and different presentations, that represents a diagnostic challenge for the knee surgeon. This type of injury presents with several characteristics that must be diagnosed preoperatively. Although clinical protocols are available for treating this lesion, treatment must be individualized. We believe that the contralateral knee is of paramount importance for both surgical planning and evaluation of the final postoperative results. During the clinical and radiographic evaluation of the contralateral knee, we investigate previous ligament laxity and the degree of recurvatum, as well as tibial plateau tilt. These are important parameters that can compromise postoperative assessment. Therefore, we corroborate the statement of Rios et al.,11 who recommend requesting stress radiographs of both knees postoperatively. According to these authors, images obtained under stress help to provide evidence of whether the multiligament reconstruction has restored the normal knee ligament laxity.11
Gwathmey et al.10 (2,012) showed that stress radiographs are useful in defining the treatment of patients with posterolateral corner injury in conjunction with MRI. MRI is a complementary examination with high sensitivity for the diagnosis of ligament injuries; however, it is a static examination that does not show the functional consequences of these injuries.9 In contrast, stress radiography is a dynamic examination showing this functional laxity resulting from ligament deficiency.9 In multiligament injuries, stress radiographs complement the MRI study. Our experience supports these claims. We believe that these 2 incidence examinations facilitate a better understanding of the lesion and, consequently, surgical planning.
Sekiya et al.23 performed stress radiography in 10 pairs of knees of human cadavers sequentially, drying the posterior cruciate ligament and posterolateral corner, and showed that tibial translation over 10 mm corresponds to the presence of combined injury of these 2 structures. LaPrade et al.17 observed that varus stress radiography associated with the history and physical examination findings can differentiate an isolated lesion of the fibular collateral ligament from a posterolateral corner injury. They claimed that this complementary study is useful in the diagnosis, treatment, and postoperative clinical follow-up.17 We agree with that statement; as a result, we standardized the mandatory stress radiographs in patients with central pivot injuries associated with peripheral structures.
Another study by LaPrade et al.18 concluded that injuries to the medial compartment of the knee can be quantified through radiography performed under valgus stress. In addition, it was found that a medial opening with the knee extended evidences an isolated lesion of the medial collateral ligament. Therefore, we believe that stress radiographs represent a low-cost complementary examination, providing valuable information that will facilitate our surgical time. Exposure to ionizing radiation is a negative point; however, the benefits are greater than the harm.18 Among the various forms of assessment for posterior stress radiographs, the kneeling-view method was shown to be a reliable technique for assessing posterior cruciate injury by Garofalo et al.12,22
MRI is an inaccurate test to analyze a chronic posterior cruciate ligament injury.20 In our opinion, MRI may show healing of the posterior cruciate ligament but with a nonfunctional status. Thus, radiography with knee stress is a greater tool for analyzing the injury. The positioning of the patient, the radiographic technique, and the anatomic landmarks can alter radiographs obtained under stress.20
Beukes et al.24 performed a cadaveric study evaluating a new device to perform stress radiography without the need for a doctor or radiology technician to apply manual stress. They found results that were similar to those of manual stress, but adjustments would still be necessary to improve the method. In the same line of thought, trying to avoid exposure to radiation by doctors and technicians in radiology, Ellera Gomes et al.25 published a technique to perform radiography with stress in external rotation to assess whether rotational instability is present in posterolateral corner injuries. Although several researchers are looking for new alternatives to radiography with traditional manual stress, it remains as easily accessible and inexpensive method for the correct diagnosis of multiligament knee injuries.
Burrus et al.9 performed a literature review with critical analysis on the topic of multiligament injuries. They concluded that stress radiographs are more accurate than MRI in functional assessment, although this statement has a low level of evidence.9 We believe that the multiligament lesion is an extremely complex lesion. Therefore, we should associate the maximum of complementary imaging exams, optimizing our surgical procedure.
We present advantages, disadvantages, risks, and limitations of the stress radiography technique in Table 1 and tips and pitfalls in Table 2. Detailing the technique for performing stress radiography will allow this tool to assist in decision making in the face of complex ligament injuries, becoming a more reproducible technique.
Table 1.
Advantages, Disadvantages, Risks, and Limitations Associated With Using Stress Radiography
| Advantages | Disadvantages | Risks | Limitations |
|---|---|---|---|
| The technique has a low cost. | Radiation is emitted to the patient and the examiner who performs the examination. | Radiation | Only 1 knee can have a ligament injury. |
| The technique is simple to perform. | The examiner must know how to perform the technique, paying attention to the correct degree of knee flexion, as well as the rotation of the limb. | Pain when performing examination | Digital radiography is recommended. |
| The technique requires simple items found in clinics and hospitals that perform radiography (e.g., thick, soft cushion and 2- to 3-step ladder). | Eventually, radiography should be repeated if the technique has not been applied correctly. | Lead cloaks and lead gloves must be available to protect the examiner. | |
| The cushion used can hinder image interpretation. In our study, the cushion decreased the radiotransparency but without affecting the interpretation of the examination. | In acute injuries, stress radiography may not be possible because of edema and pain in the affected knee. |
Table 2.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| The examiner should ensure that a position of 20° of knee flexion is maintained during varus and valgus maneuvers with the knee flexed, aiming to standardize evaluations and comparisons. | Flexing the knee more than the recommended 20° can yield unreliable results. |
| When obtaining kneeling radiographs of the affected knee, the examiner should make sure that the thigh of the examined knee is tilted 10° toward the x-ray film so that the femoral condyles are superimposed, facilitating the interpretation of the examination findings. It is important that the knee being examined is the one closest to the x-ray film. | If the femoral condyles are not superimposed on the kneeling radiograph, it is impossible to precisely measure the posteriorization of the tibia in relation to the femur. |
| The examiner must simulate the positioning of the kneeling radiograph, showing the patient how he or she should position himself or herself; this will facilitate the patient’s understanding of the examination and speed up the procedure. | The examiner should make sure that the cushion used to obtain the kneeling radiograph is comfortable for the patient, preventing him or her from feeling pain during the examination and not staying in the desired position. |
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the supine position with the x-ray ampule angled at about 20° cephalic—the same angle to which the knee should be flexed. We use the Bone Ninja application to evaluate whether the patient has achieved 20° of flexion. A traditional goniometer can also be used to assess this 20° measurement. To achieve the desired flexion, we use a cushion approximately 10 cm posterior to the knee in individuals of medium height. The height of the cushion may vary according to the patient’s height. We position the patient at the end of the table to facilitate radiography with stress on the knees. We must pay special attention to the rotation of the lower limb, correcting such rotation, as in the presented case, which showed increased external rotation. We identify the joint line and position one hand on the distal end of the femur and the other hand on the distal end of the leg, again observing the rotation keeping the patella directly vertical. We then perform the varus stress maneuver. A 1.53-cm opening, measured using the digital x-ray software, is observed. Next, we perform the valgus stress maneuver with the knee flexed at 20°, identify the joint line, position the hands in the aforementioned places, and apply maximum strength. Radiography shows a 0.87-cm medial opening. The same steps are performed on the contralateral knee to compare the opening of the medial and lateral spaces and define the correct diagnosis of possible ligament injuries. We correct the rotation, identify the joint line, and perform the varus stress maneuver, observing a 1.38-cm opening. Then, we perform the stress maneuver in valgus with 20° of flexion, observing an opening of 1.60 cm. We remove the cushion, position the ampule at 0°, identify the joint line, and perform the varus stress maneuver, with a 1.31-cm lateral opening; the valgus stress maneuver is also performed on the same member, with a 0.8-cm opening. We perform the same steps on the contralateral knee, with varus stress at 0°, observing a 1.29-cm lateral opening, and when performing the valgus stress maneuver, we observe a 1.18-cm opening. To obtain a kneeling radiograph to assess the posteriorization of the tibia in lesions of the posterior cruciate ligament, we need a thick, soft cushion; a ladder; and an anterior support. The patient’s entire weight must be resting on the kneeling limb. Care must be taken to ensure that the patient is leaning to the side by about 10° while being examined, with the aim of the condyles being superimposed on the image. On stress radiography, we draw a line parallel to the posterior tibial cortex, identifying the most posterior point on the Blumensaat line, and we assess the distance between this line and this point.
References
- 1.Beldame J., Bertiaux S., Roussignol X. Laxity measurements using stress radiography to assess anterior cruciate ligament tears. Orthop Traumatol Surg Res. 2011;97:34–43. doi: 10.1016/j.otsr.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Katz J.W., Fingeroth R.J. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am J Sports Med. 1986;14:88–91. doi: 10.1177/036354658601400115. [DOI] [PubMed] [Google Scholar]
- 3.Peeler J., Leiter J., MacDonald P. Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sports Med. 2010;20:80–85. doi: 10.1097/JSM.0b013e3181ceca45. [DOI] [PubMed] [Google Scholar]
- 4.Sawant M., Narasimha Murty A., Ireland J. Valgus knee injuries: Evaluation and documentation using a simple technique of stress radiography. Knee. 2004;11:25–28. doi: 10.1016/S0968-0160(03)00009-7. [DOI] [PubMed] [Google Scholar]
- 5.Craft J.A., Kurzweil P.R. Physical examination and imaging of medial collateral ligament and posteromedial corner of the knee. Sports Med Arthrosc Rev. 2015;23:e1–e6. doi: 10.1097/JSA.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 6.Beldame J., Mouchel S., Bertiaux S. Anterior knee laxity measurement: Comparison of passive stress radiographs Telos(®) and "Lerat", and GNRB(®) arthrometer. Orthop Traumatol Surg Res. 2012;98:744–750. doi: 10.1016/j.otsr.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 7.Franklin J.L., Rosenberg T.D., Paulos L.E., France E.P. Radiographic assessment of instability of the knee due to rupture of the anterior cruciate ligament. A quadriceps-contraction technique. J Bone Joint Surg Am. 1991;73:365–372. [PubMed] [Google Scholar]
- 8.Schulz M.S., Steenlage E.S., Russe K., Strobel M.J. Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Joint Surg Am. 2007;89:332–338. doi: 10.2106/JBJS.C.00834. [DOI] [PubMed] [Google Scholar]
- 9.Burrus M.T., Werner B.C., Griffin J.W., Gwathmey F.W., Miller M.D. Diagnostic and management strategies for multiligament knee injuries: A critical analysis review. JBJS Rev. 2016;4 doi: 10.2106/JBJS.RVW.O.00020. [DOI] [PubMed] [Google Scholar]
- 10.Gwathmey F.W., Jr., Tompkins M.A., Gaskin C.M., Miller M.D. Can stress radiography of the knee help characterize posterolateral corner injury? Clin Orthop Relat Res. 2012;470:768–773. doi: 10.1007/s11999-011-2008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rios C.G., Leger R.R., Cote M.P., Yang C., Arciero R.A. Posterolateral corner reconstruction of the knee: Evaluation of a technique with clinical outcomes and stress radiography. Am J Sports Med. 2010;38:1564–1574. doi: 10.1177/0363546510363462. [DOI] [PubMed] [Google Scholar]
- 12.James E.W., Williams B.T., LaPrade R.F. Stress radiography for the diagnosis of knee ligament injuries: A systematic review. Clin Orthop Relat Res. 2014;472:2644–2657. doi: 10.1007/s11999-014-3470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verhulst F.V., MacDonald P. Diagnosing PCL injuries: History, physical examination, imaging studies, arthroscopic evaluation. Sports Med Arthrosc Rev. 2020;28:2–7. doi: 10.1097/JSA.0000000000000251. [DOI] [PubMed] [Google Scholar]
- 14.McDonald L.S., Waltz R.A., Carney J.R. Validation of varus stress radiographs for anterior cruciate ligament and posterolateral corner knee injuries: A biomechanical study. Knee. 2016;23:1064–1068. doi: 10.1016/j.knee.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Lee Y.S., Han S.H., Jo J., Kwak K.S., Nha K.W., Kim J.H. Comparison of 5 different methods for measuring stress radiographs to improve reproducibility during the evaluation of knee instability. Am J Sports Med. 2011;39:1275–1281. doi: 10.1177/0363546510396182. [DOI] [PubMed] [Google Scholar]
- 16.Kane P.W., Cinque M.E., Moatshe G. Fibular collateral ligament: Varus stress radiographic analysis using 3 different clinical techniques. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118770170. 2325967118770170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LaPrade R.F., Heikes C., Bakker A.J., Jakobsen R.B. The reproducibility and repeatability of varus stress radiographs in the assessment of isolated fibular collateral ligament and grade-III posterolateral knee injuries. An in vitro biomechanical study. J Bone Joint Surg Am. 2008;90:2069–2076. doi: 10.2106/JBJS.G.00979. [DOI] [PubMed] [Google Scholar]
- 18.Laprade R.F., Bernhardson A.S., Griffith C.J., Macalena J.A., Wijdicks C.A. Correlation of valgus stress radiographs with medial knee ligament injuries: An in vitro biomechanical study. Am J Sports Med. 2010;38:330–338. doi: 10.1177/0363546509349347. [DOI] [PubMed] [Google Scholar]
- 19.Kobayashi S., Terayama K. Quantitative stress radiography for diagnosis of anterior cruciate ligament deficiency. Comparison between manual and instrumental techniques and between methods with knee flexed at 20 degrees and at 90 degrees. Arch Orthop Trauma Surg. 1993;112:109–112. doi: 10.1007/BF00449983. [DOI] [PubMed] [Google Scholar]
- 20.Jackman T., LaPrade R.F., Pontinen T., Lender P.A. Intraobserver and interobserver reliability of the kneeling technique of stress radiography for the evaluation of posterior knee laxity. Am J Sports Med. 2008;36:1571–1576. doi: 10.1177/0363546508315897. [DOI] [PubMed] [Google Scholar]
- 21.Jung T.M., Reinhardt C., Scheffler S.U., Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: A comparison of five different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:1116–1121. doi: 10.1007/s00167-006-0137-3. [DOI] [PubMed] [Google Scholar]
- 22.Garofalo R., Fanelli G.C., Cikes A. Stress radiography and posterior pathological laxity of knee: Comparison between two different techniques. Knee. 2009;16:251–255. doi: 10.1016/j.knee.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Sekiya J.K., Whiddon D.R., Zehms C.T., Miller M.D. A clinically relevant assessment of posterior cruciate ligament and posterolateral corner injuries. Evaluation of isolated and combined deficiency. J Bone Joint Surg Am. 2008;90:1621–1627. doi: 10.2106/JBJS.G.01365. [DOI] [PubMed] [Google Scholar]
- 24.Beukes GL, Patnaik S, Sivarasu S. In vitro functional verification of a novel laxity measurement stress radiography device. In: Proceedings of the 2018 Design of Medical Devices Conference (DMD2018). New York: American Society of Medical Engineers, 2018.
- 25.Ellera Gomes J.L., de Aguiar M.R., Horta Barbosa L.B., Kennedy N.I., Ferrari M.B. The external rotation radiographic technique for posterolateral injury. Arthrosc Tech. 2017;6:e2183–e2186. doi: 10.1016/j.eats.2017.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position with the x-ray ampule angled at about 20° cephalic—the same angle to which the knee should be flexed. We use the Bone Ninja application to evaluate whether the patient has achieved 20° of flexion. A traditional goniometer can also be used to assess this 20° measurement. To achieve the desired flexion, we use a cushion approximately 10 cm posterior to the knee in individuals of medium height. The height of the cushion may vary according to the patient’s height. We position the patient at the end of the table to facilitate radiography with stress on the knees. We must pay special attention to the rotation of the lower limb, correcting such rotation, as in the presented case, which showed increased external rotation. We identify the joint line and position one hand on the distal end of the femur and the other hand on the distal end of the leg, again observing the rotation keeping the patella directly vertical. We then perform the varus stress maneuver. A 1.53-cm opening, measured using the digital x-ray software, is observed. Next, we perform the valgus stress maneuver with the knee flexed at 20°, identify the joint line, position the hands in the aforementioned places, and apply maximum strength. Radiography shows a 0.87-cm medial opening. The same steps are performed on the contralateral knee to compare the opening of the medial and lateral spaces and define the correct diagnosis of possible ligament injuries. We correct the rotation, identify the joint line, and perform the varus stress maneuver, observing a 1.38-cm opening. Then, we perform the stress maneuver in valgus with 20° of flexion, observing an opening of 1.60 cm. We remove the cushion, position the ampule at 0°, identify the joint line, and perform the varus stress maneuver, with a 1.31-cm lateral opening; the valgus stress maneuver is also performed on the same member, with a 0.8-cm opening. We perform the same steps on the contralateral knee, with varus stress at 0°, observing a 1.29-cm lateral opening, and when performing the valgus stress maneuver, we observe a 1.18-cm opening. To obtain a kneeling radiograph to assess the posteriorization of the tibia in lesions of the posterior cruciate ligament, we need a thick, soft cushion; a ladder; and an anterior support. The patient’s entire weight must be resting on the kneeling limb. Care must be taken to ensure that the patient is leaning to the side by about 10° while being examined, with the aim of the condyles being superimposed on the image. On stress radiography, we draw a line parallel to the posterior tibial cortex, identifying the most posterior point on the Blumensaat line, and we assess the distance between this line and this point.