Abstract
Distal triceps ruptures are an uncommon injury, and currently, there is a lack of consensus on the optimal surgical technique for repair. The traditional transosseous cruciate repair has been shown to be nonanatomic and to have a higher failure rate and be biomechanically inferior to suture anchor repairs. The use of anchors significantly increases procedure cost and theoretically increases the risk of complications related to drill and anchor placement. The technique described in this article allows anatomic restoration of the triceps tendon while avoiding the increased cost and risk that may be associated with suture anchor placement.
Distal triceps ruptures are rare injuries that occur most frequently in middle-aged men.1,2 The mechanism of injury is typically an eccentric load to the triceps during a fall on an outstretched arm.1 These injuries can also occur from a direct blow or laceration to the elbow or during weightlifting or participation in contact sports.1,2 Most ruptures are located at the tendon-bone interface, and risk factors include systemic diseases, local corticosteroid injections, and use of anabolic steroids.1
Surgical treatment is the standard of care for triceps injuries in active individuals. Options for repair include transosseous,1, 2, 3, 4, 5, 6, 7 suture anchor (SA),1,2,4,8,9 and hybrid transosseous-SA techniques.3,5,6,10 The transosseous cruciate (TC) technique has been the historical standard for treatment of these injuries.11 However, recent studies have shown that the TC technique results in incomplete coverage of the triceps footprint on the olecranon4 and has inferior biomechanical properties to anatomic SA4 or hybrid5 techniques. Even so, anatomic SA techniques require the use of anchors on the tension side of the olecranon, which has the theoretical risk of ulnohumeral joint penetration and creates a stress riser on the olecranon. Use of anchors also increases the cost of surgery relative to using suture material alone.
In this article, we describe an all-suture repair technique that restores the anatomic footprint of the triceps without the use of anchors or drill holes on the tension side of the olecranon.
Surgical Technique
Setup and Surgical Approach
After general anesthesia and muscle relaxation, the patient is placed in the lateral decubitus position. The arm is placed in 90° of forward flexion, with the elbow draped over a padded lateral arm positioner. After routine preparation and draping, a sterile tourniquet is applied as high as possible on the arm and insufflated to 250 mm Hg after exsanguination of the extremity. A posterior approach to the elbow is performed with the incision placed off the lateral border of the olecranon process (Fig 1). The triceps rupture is identified, and blunt dissection is used to mobilize the tissue. The torn edge of the tendon is then debrided with a scalpel to stable healthy tissue (Table 1, Video 1).
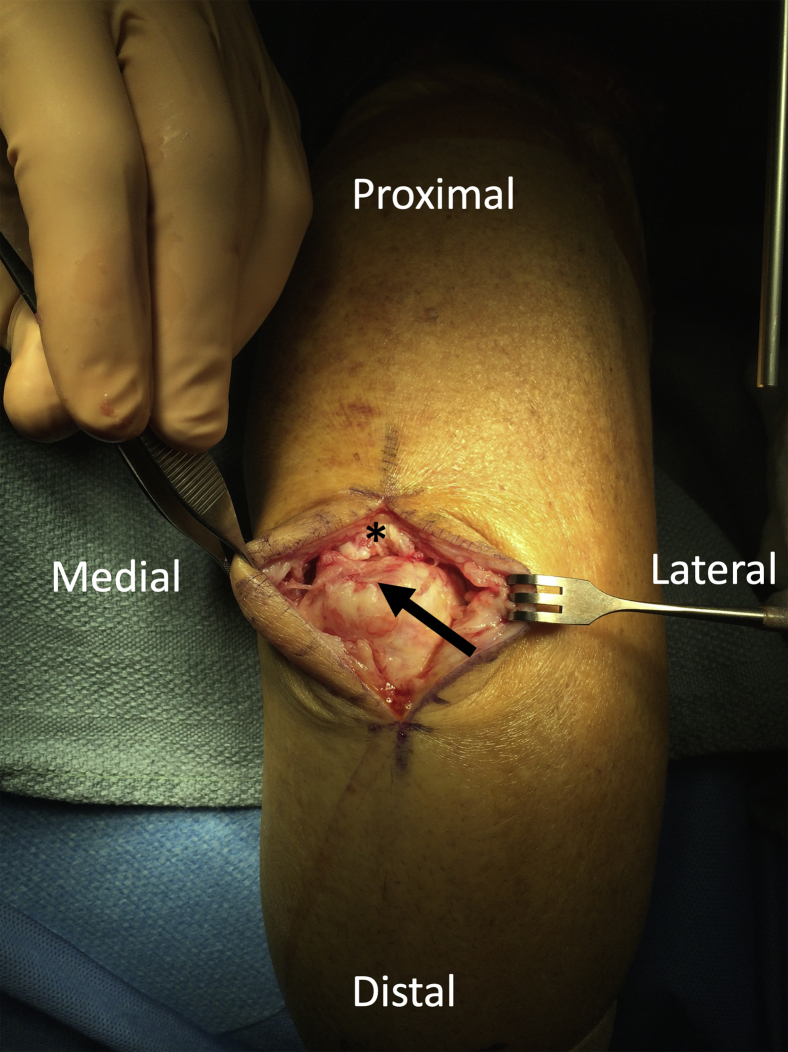
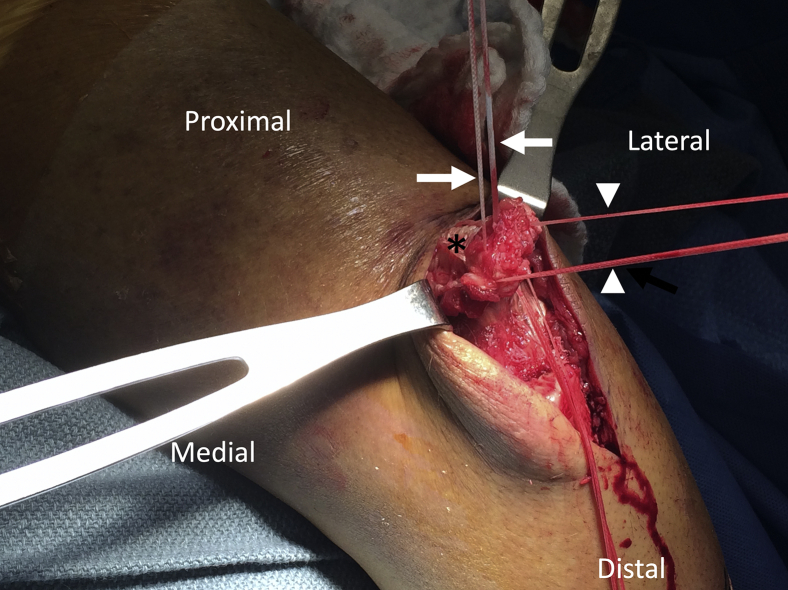
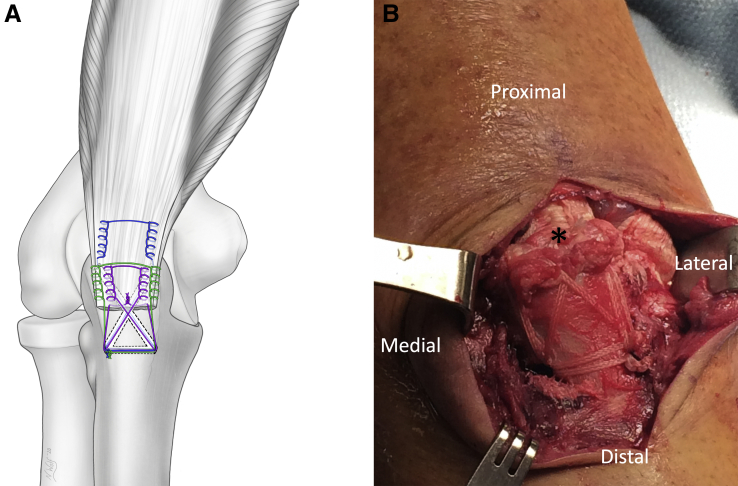
Fig 1.
Patient is in the lateral decubitus position. Posterior approach to triceps tendon. The residual triceps tendon stump (asterisk) and triceps footprint (arrow) are visualized.
Table 1.
Pearls and Pitfalls
| Pearls |
| Care should be taken to subperiosteally expose the olecranon sufficiently to allow protection of the ulnar nerve medially and placement of knots under the anconeus laterally. |
| Care should be taken to remove degenerative appearing tissue from the tendon edges. |
| A high-speed burr should be used to remove all soft tissue and lightly decorticate the footprint. |
| The cruciate drill tunnels should be placed on the most proximal medial and lateral aspects of the footprint to allow complete anatomic coverage of the footprint. |
| An Army-Navy retractor should be used to protect the ulnar nerve while drilling the transverse tunnel. |
| The arm should be placed in full extension and skeletal relaxation should be used while tying the sutures. |
| Pitfalls |
| Removing too much bone when preparing the footprint |
| Failure to aim the drill away from the joint surface during transosseous tunnel placement |
| Failure to protect the ulnar nerve while drilling the transverse drill tunnel |
| Not placing the knots under the anconeus to avoid knot irritation |
Bone Preparation and Tunnel Placement
A high-speed 4-mm oval burr is used to lightly decorticate the triceps footprint on the olecranon. The anconeus and flexor carpi ulnaris insertions are elevated off their respective sides of the olecranon to allow proper tunnel placement. After this, a 2-mm drill bit is used to create TC tunnels on the anteromedial and anterolateral aspects of the footprint, aiming 45° relative to the long axis of the olecranon (Fig 2A) and away from the ulnohumeral joint (Fig 2B). These tunnels are drilled from proximal to distal and exit 5 mm anterior to the dorsal ulnar ridge on the medial and lateral sides of the olecranon, approximately 2 cm distal to the triceps footprint. A transverse drill tunnel is made from lateral to medial at the points where the cruciate drill tunnels exit the olecranon.
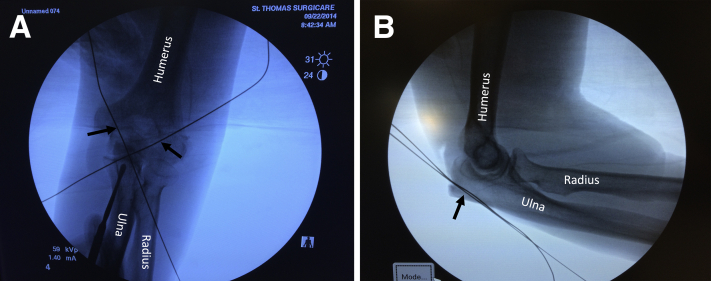
Fig 2.
Patient is in the lateral decubitus position. (A) Anteroposterior radiograph showing surgical steel wires (arrows) placed into transosseous cruciate drill tunnels. These tunnels are made 45° relative to the long axis of the olecranon. (B) Lateral radiograph with surgical steel wires (arrow) placed into tunnels, showing that the tunnel trajectory is away from the ulnohumeral joint.
Suture Placement and Tendon Repair
A LabralTape suture (Arthrex, Naples, FL) is placed using a locking Krackow technique, exiting the anterior aspect of the tendon, leaving enough tendon distal to where the sutures exit to completely cover the triceps footprint (Fig 3). The distance between the sutures where they exit the anterior tendon should be equal to the distance between the anteromedial and anterolateral transosseous drill tunnels. A second locking Krackow LabralTape suture is placed, exiting the posterior and distal aspect of the tendon on its peripheral medial and lateral margins (Fig 4). A third LabralTape suture is placed in a similar fashion to the second but in the central portion of the tendon and is marked with a surgical pen for later identification (Fig 5).
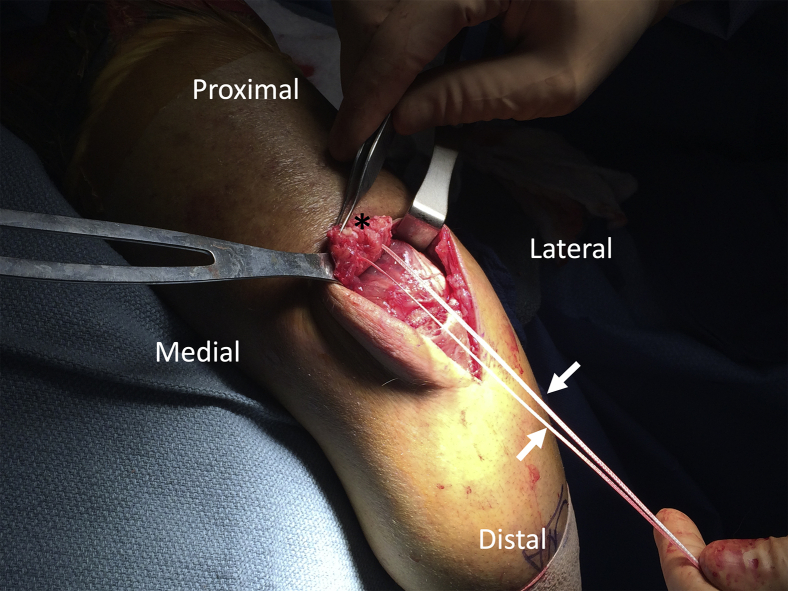
Fig 3.
Patient is in the lateral decubitus position. Posterior view of the elbow showing a LabralTape suture (arrows), placed in a locking Krackow fashion, with the suture limbs exiting the anterior aspect of the triceps tendon (asterisk).
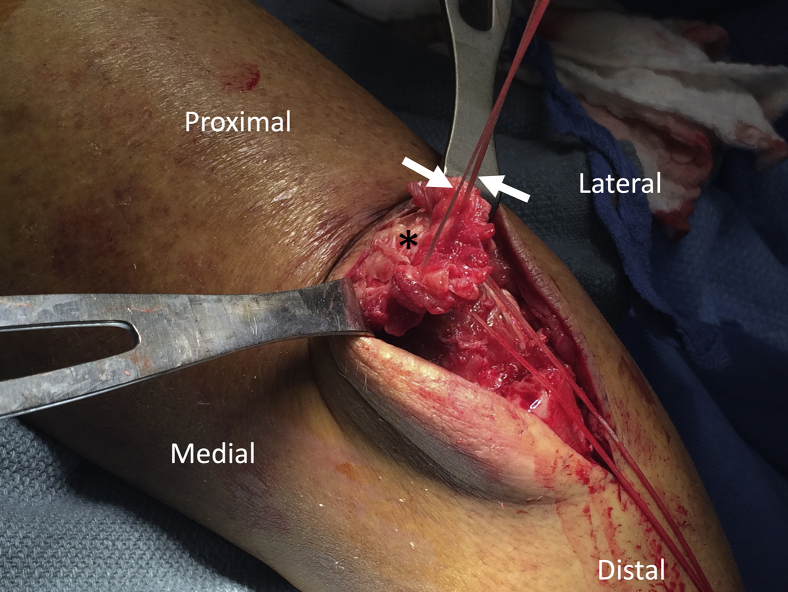
Fig 4.
Patient is in the lateral decubitus position. Posterior view of the elbow showing a second LabralTape suture (arrows), placed in a locking Krackow fashion, with the suture limbs exiting the posterior and distal aspect of the tendon (asterisk) on its peripheral medial and lateral margins.
Fig 5.
Patient is in the lateral decubitus position. Posterior view of the elbow showing a third LabralTape suture (arrows), placed in a locking Krackow fashion, with the suture limbs exiting the posterior and distal aspect of the tendon (asterisk). This suture is located centrally on the tendon between the tails of the second suture (arrowheads).
A Hewson suture passer (Smith & Nephew, Andover, MA) is used to pass the sutures exiting the anterior aspect of the tendon through their respective drill tunnels (Fig 6). The lateral limb of the centrally placed suture and the medial limb of the peripherally placed suture are shuttled through the transverse drill tunnel from medial to lateral (Fig 7). The medial limb of the centrally placed suture and the lateral limb of the peripherally placed suture are then shuttled from lateral to medial (Fig 8). Passing the sutures in this manner allows the centrally placed sutures to cross over each other, resulting in better coverage and compression of the tendon at the footprint. The suture exiting the anterior aspect of the tendon is tied first, with the elbow in full extension. The knot is placed on the lateral side of the olecranon deep to the anconeus muscle, which limits the possibility of knot irritation. After this, the peripheral posterior suture is tied in a similar fashion on the lateral side of the olecranon. The central posterior suture is then passed through the triceps tendon at the footprint and tied down to complete the repair (Fig 9). Tying the central posterior suture proximally increases compression at the footprint and decreases knot bulk distally.
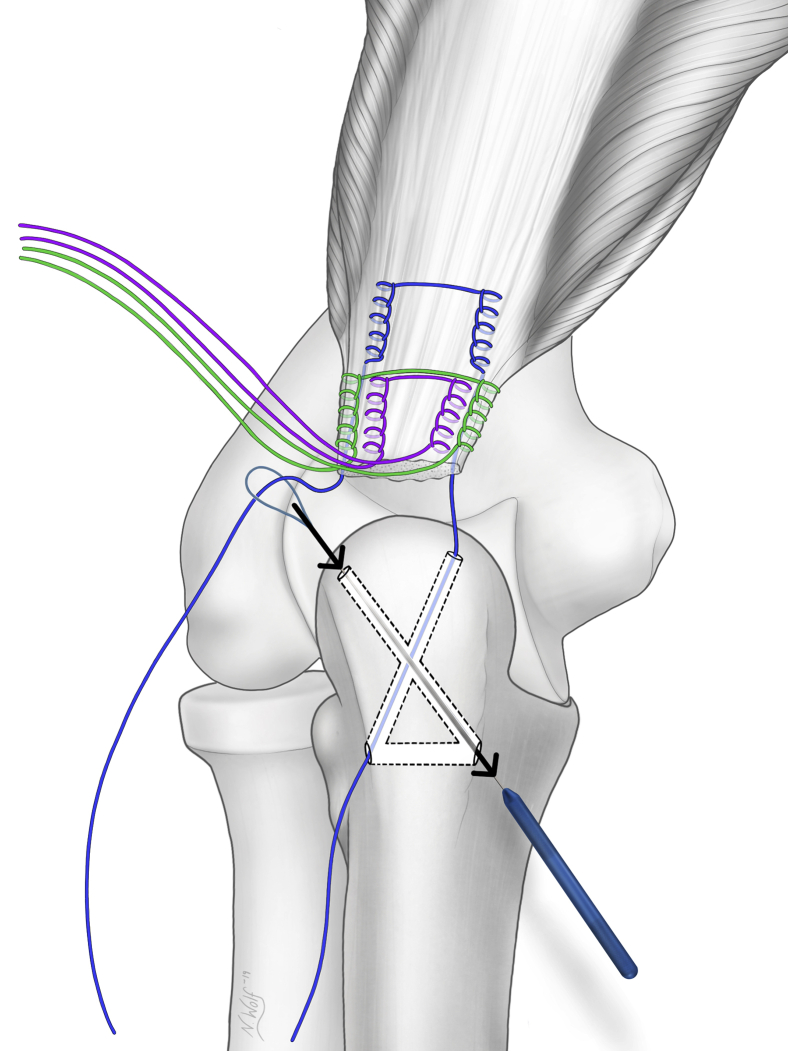
Fig 6.
Posterior view of the elbow showing passage of the sutures exiting the anterior aspect of the triceps tendon (blue) through their respective cruciate drill tunnels using a Hewson suture passer. (Illustration by Nicole Wolf, M.S., © 2019. Printed with permission.)
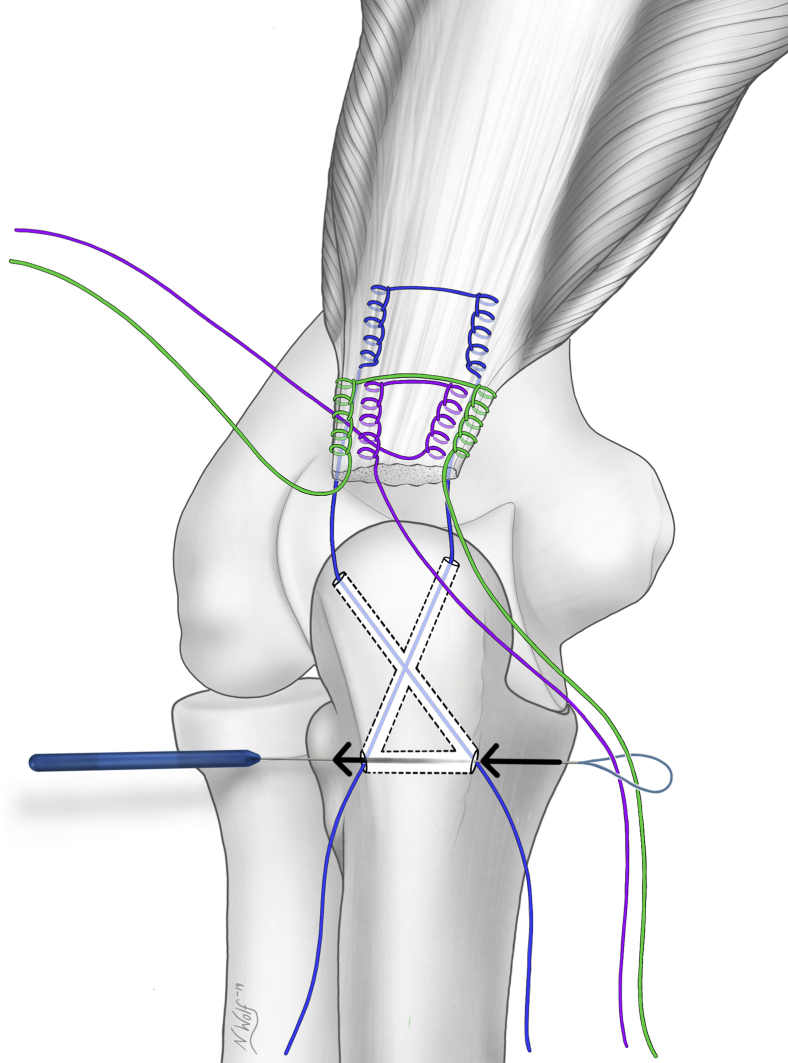
Fig 7.
Posterior view of the elbow showing passage of the lateral limb of the centrally placed suture (purple) and the medial limb of the peripherally placed suture (green) through the transverse drill tunnel from medial to lateral using a Hewson suture passer. (Illustration by Nicole Wolf, M.S., © 2019. Printed with permission.)
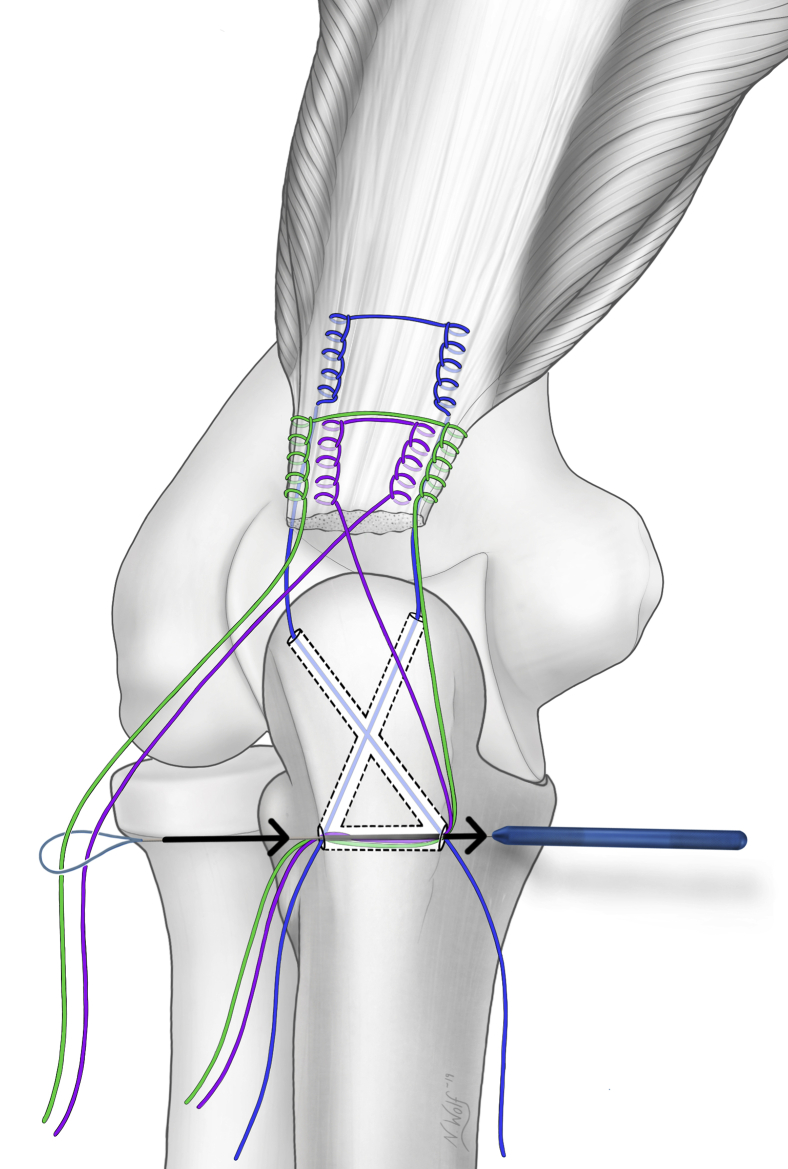
Fig 8.
Posterior view of the elbow showing passage of the medial limb of the centrally placed suture (purple) and the lateral limb of the peripherally placed suture (green) through the transverse drill tunnel from lateral to medial using a Hewson suture passer. (Illustration by Nicole Wolf, M.S., © 2019. Printed with permission.)
Fig 9.
Posterior view of the elbow showing the final repair construct. (A) With the arm in full extension, the suture limbs exiting the anterior aspect of the triceps (blue) are tied down laterally under the anconeus. Next, the posterior and peripheral suture (green) is tied down. Finally, the posterior and central suture (purple) is brought through the tendon with a free needle and tied down proximally to complete the repair. (Illustration by Nicole Wolf, M.S., © 2019. Printed with permission.) (B) Patient is in the lateral decubitus position. Surgical picture of the triceps tendon being compressed against the olecranon and covering the entire triceps footprint (asterisk).
Discussion
Distal triceps ruptures are a rare entity, with an overall incidence of 1.1 in 100,000.12 Given the uncommon nature of these injuries, there is a limited body of literature on the topic, consisting mostly of small level of evidence (LOE) IV studies.11 Currently, there are no LOE I or II comparative studies, and correspondingly, there is a lack of consensus on the ideal treatment of these tears. Even so, there appears to be more variability in the outcomes of TC repair compared with SA repair.1,2,6,11 In a recent systematic review (LOE IV), Dunn et al.11 reported that although 89% of patients returned to their preinjury level of activity, 5.9% (6 of 101) sustained a rerupture at a mean of 34.6 months, with all of these reruptures occurring after TC repair. Mirzayan et al.1 (LOE III) similarly found a higher retear rate (6.7% [n = 7] vs 0%), as well as a higher reoperation rate (9.7% vs 1.4%), with TC repair versus SA repair. Contradictory to these findings, Horneff et al.6 (LOE III) and Waterman et al.2 (LOE IV) found no differences in validated outcome measures or reruptures comparing TC repairs with SA repairs. Ultimately, the reason for the variable rerupture rate with TC repair is unclear, thus highlighting the need for well-controlled LOE I and II studies on this topic.
The variable retear rate with TC repair may be partly attributed to the inferior biomechanical properties of these nonanatomic repairs compared with techniques that restore the anatomy of the triceps footprint.4,5 In a controlled biomechanical study, Yeh et al.4 found that double-row SA repairs using 4 anchors showed significantly less displacement during cyclic loading than single-row SA and TC repairs. These double-row SA repairs were described as “anatomic” because they restored 86% of the triceps footprint compared with 31% and 48% for TC and single-row SA repairs, respectively.4 Clark et al.5 also found significantly less displacement during cyclic loading, as well as higher failure loads during ultimate failure testing, using an anatomic hybrid TC-SA technique compared with TC repair. This technique, described in more detail by Paci et al.,10 restored 74% of the footprint compared with only 21% with TC repair.5
Although these footprint-restoring SA and hybrid repairs have favorable anatomic and biomechanical properties, the use of anchors during tendon repair surgery has been shown to significantly increase surgical costs relative to the use of suture material alone.13 The hybrid repair technique is more cost-effective than anatomic double-row SA repair because it only requires the use of 1 anchor.5,10 Even so, both techniques require drilling and anchor placement toward the ulnohumeral joint, theoretically risking joint penetration and damage.4,5,10 Anchors are also placed on the tension side of the olecranon in both techniques, which can create a stress riser and theoretically weaken the bone.4,5,10 The technique described in this article has the advantage of providing an anatomic repair without the use of anchors, which improves cost-effectiveness. Furthermore, orienting the tunnels away from the joint surface and off the tension side of the olecranon improves the overall safety of the procedure relative to anatomic SA or hybrid techniques (Table 2).
Table 2.
Advantages and Disadvantages
| Advantages |
| Provides anatomic repair relative to conventional transosseous suture techniques |
| Decreases cost relative to use of anchors |
| Decreases theoretical risks that may be associated with use of anchors |
| Is less technically demanding relative to other anatomic all-suture repair techniques |
| Disadvantages |
| Has not been studied biomechanically |
| Has potential for knot irritation |
A biomechanical analysis of the described technique has yet to be performed; however, testing of other all-suture anatomic repair constructs has shown favorable biomechanical properties.3 Dorweiler et al.3 described an anatomic and anchorless technique that uses 4 transosseous tunnels drilled into the triceps footprint; biomechanical testing of this “double bi-cruciate” technique did not reveal a significant difference during cyclic or load-to-failure testing compared with the hybrid technique described by Paci et al.10 Even so, this technique is more technically demanding than our repair because it requires a total of 4 tunnels all placed within close proximity to each other on the triceps footprint.3 In our technique, only 3 tunnels are needed to create a mattress effect that applies compression evenly over the entire footprint. Whereas the clinical value of anatomic repair using a mattress technique is uncertain, we have found this to generally be a useful surgical principle.
Although this technique was designed to anatomically repair the distal triceps in a cost-effective manner that minimizes complications, there are some risks and limitations. There is a theoretical risk of joint penetration during transosseous tunnel drilling. However, because the tunnels are oriented away from the joint, there is a considerable distance between the tunnels and joint surface (Fig 2B), making this complication unlikely to occur. Drilling the transverse tunnel poses a theoretical risk of ulnar nerve injury. Therefore, we recommend judicious exposure, protecting the nerve with a retractor, and drilling from lateral to medial, which allows direct visualization of the drill tip. Finally, the suture knots could pose a risk of skin irritation (Table 2). Even so, these are strategically placed under the anconeus, and one is tied proximally to decrease knot bulk distally.
In conclusion, the current technique is a safe, cost-effective, and technically manageable procedure that fully restores the anatomic footprint of the distal triceps tendon. Further biomechanical and clinical studies are needed to determine how this procedure compares to other available techniques.
Footnotes
The author reports no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is positioned in the lateral decubitus position. A posterior approach to the distal triceps is made, exposing the ruptured tendon. The described technique allows anatomic repair of the triceps tendon in a safe and cost-effective manner without the use of anchors.
ICMJE author disclosure forms
References
- 1.Mirzayan R., Acevedo D.C., Sodl J.F. Operative management of acute triceps tendon ruptures: Review of 184 cases. Am J Sports Med. 2018;46:1451–1458. doi: 10.1177/0363546518757426. [DOI] [PubMed] [Google Scholar]
- 2.Waterman B.R., Dean R.S., Veera S. Surgical repair of distal triceps tendon injuries: Short-term to midterm clinical outcomes and risk factors for perioperative complications. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119839998. 2325967119839998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dorweiler M.A., Van Dyke R.O., Siska R.C., Boin M.A., DiPaola M.J. A comparative biomechanical analysis of 2 double-row, distal triceps tendon repairs. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117708308. 2325967117708308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yeh P.C., Stephens K.T., Solovyova O. The distal triceps tendon footprint and a biomechanical analysis of 3 repair techniques. Am J Sports Med. 2010;38:1025–1033. doi: 10.1177/0363546509358319. [DOI] [PubMed] [Google Scholar]
- 5.Clark J., Odopilwe E., Rizzi A. Distal triceps knotless anatomic footprint repair is superior to transosseous cruciate repair: A biomechanical comparison. Arthroscopy. 2014;30:1254–1260. doi: 10.1016/j.arthro.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Horneff J.G., III, Aleem A., Nicholson T. Functional outcomes of distal triceps tendon repair comparing transosseous bone tunnels with suture anchor constructs. J Shoulder Elbow Surg. 2017;26:2213–2219. doi: 10.1016/j.jse.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 7.Sarokhan A.K., Leung N.L. Acute triceps tendon repair: A technique utilizing 3 curved tunnels and proximal knots. Arthrosc Tech. 2019;8:e705–e712. doi: 10.1016/j.eats.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dimock R.A.C., Kontoghiorghe C., Consigliere P. Distal triceps rupture repair: The triceps pulley-pullover technique. Arthrosc Tech. 2019;8:e85–e91. doi: 10.1016/j.eats.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caldwell P.E., III, Evensen C.S., Vance N.G., Pearson S.E. Distal triceps speed bridge repair. Arthrosc Tech. 2018;7:e907–e913. doi: 10.1016/j.eats.2018.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paci J.M., Clark J., Rizzi A. Distal triceps knotless anatomic footprint repair: A new technique. Arthrosc Tech. 2014;3:e621–e626. doi: 10.1016/j.eats.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunn J.C., Kusnezov N., Fares A. Triceps tendon ruptures: A systematic review. Hand (N Y) 2016;12:431–438. doi: 10.1177/1558944716677338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balazs G.C., Brelin A.M., Dworak T.C. Outcomes and complications of triceps tendon repair following acute rupture in American military personnel. Injury. 2016;47:2247–2251. doi: 10.1016/j.injury.2016.07.061. [DOI] [PubMed] [Google Scholar]
- 13.Black E.M., Austin L.S., Narzikul A. Comparison of implant cost and surgical time in arthroscopic transosseous and transosseous equivalent rotator cuff repair. J Shoulder Elbow Surg. 2016;25:1449–1456. doi: 10.1016/j.jse.2016.01.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is positioned in the lateral decubitus position. A posterior approach to the distal triceps is made, exposing the ruptured tendon. The described technique allows anatomic repair of the triceps tendon in a safe and cost-effective manner without the use of anchors.
ICMJE author disclosure forms