Abstract
Posterolateral corner injuries are complex injuries, and their therapeutic management varies from one individual to another. Biomechanical studies demonstrate that anatomic posterolateral corner reconstruction restores knee kinematics better than nonanatomic reconstruction. The purpose of this report is to describe an all-arthroscopic procedure for anatomic posterolateral corner reconstruction.
Multiple techniques on posterolateral corner (PLC) reconstruction of the knee have been published. Anatomic reconstruction of the fibular collateral ligament (FCL), popliteofibular ligament (PFL), and patellar tendon (PT) restores their anatomic relations, origins, and insertions.1 Techniques vary between surgeons, but most use fibular head and transtibial tunnels to reconstruct all 3 stabilizers.1 Biomechanical studies demonstrate that anatomic PLC reconstruction restores knee kinematics better than nonanatomic reconstruction.2
All of the previously described anatomic reconstructive techniques use an open approach, with a large lateral incision, extensive exploration of the posterolateral structures, identification of the peroneal nerve, and a capsulotomy.3,4 Some authors have described arthroscopic reconstruction of isolated or combined structures such as the PT,5,6 the PFL, or the FCL.7,8 To our knowledge, there are no reports of arthroscopic reconstruction for all 3 PLC components in the same technique.
This report describes an all-arthroscopic procedure for anatomic reconstructions of the PT, PFL, and FCL.
Surgical Technique
This Technical Note is a cadaveric study conducted in the following 6 steps, also represented in the Video 1. Advantages, disadvantages, pearls, and pitfalls are presented in the .Table 1
Table 1.
Advantages, pearls, disadvantages, and pitfalls
| Advantages and Pearls | Disadvantages and Pitfalls |
|---|---|
| All-arthroscopic posterolateral corner anatomic reconstruction is a minimally invasive version of the well-established anatomic technique. | The learning curve is steeper than that of the open procedure. |
| Direct visualization of the common peroneal nerve prevents potential lesions, and direct visualization of the popliteus tendon groove avoids misplacement. | Suboptimal visualization of the footprints can lead to tunnel misplacement or mismatch. |
| During fibular tunnel drilling, use a finger to check your Kirschner wire (K-wire) placement at the level of the junction between the neck and the head of the fibula. | Iatrogenic neurovascular bundle injury with the reamer or the K-wire is a potential complication; always use a protective curette when reaming the tunnels. |
| Femoral socket reaming should be done last to maintain the arthroscopy water pressure. | Low-pressure arthroscopy can decrease visualization quality. Use plugs in the tunnels after reaming to avoid outflow that decreases the field of view. |
| Starting the procedure with lateral gutter dissection helps to decrease posterior soft tissue swelling and fluid infiltration. | |
| Passing the suture between the tibial and fibular tunnel can be difficult. Bring a probe into the loop to bring the loop in front of the fibular tunnel and pull it out. |
Step 1: Arthroscopic Portals and Identification and Exposure of the Posterolateral Structures
Five arthroscopic portals are necessary for the transseptal approach: anterolateral (AL), anteromedial (AM), posteromedial (PM), posterolateral (PL), and lateral parapatellar (LP). Detailed arthroscopic portals and identification and exposure of the posterolateral structures are described in Part 1.
Popliteus Tendon and Sulcus
Introduce the 30° arthroscope in the posteromedial portal and pass through the transseptal portal into the posterolateral compartment. The popliteus tendon, PFL, lateral femoral condyle, lateral meniscus, posterior capsule, fibular head, FCL, biceps femoris, and peroneal nerve are all well defined. Insert a radiofrequency device through the posterolateral portal and separate the posterolateral capsule from the lateral meniscus posterior horn by 2 cm to visualize the popliteal sulcus. Identify the lateral meniscus, the popliteus, and the posterior capsule. The posterior capsule and gastrocnemius muscle fibers are seen distally, and the space between popliteus and gastrocnemius is opened. Remove the synovium with the shaver jaws facing anteriorly until the popliteus musculotendinous junction is identified.
Fibular Head, Biceps Femoral, and FCL
Identification of the fibular head is paramount to identify the remaining PLC structures. After separating the posterolateral capsule from the posterior horn of the lateral meniscus, use the shaver to dissect lateral and slightly posterior to the popliteus until the fibular head comes into view. Palpate with any blunt instrument. Expose the posterosuperior part of the fibula head using the radiofrequency probe. Identify the biceps femoris by resecting the synovium from the posterior fibular head until the lateral border of the biceps femoris comes into the view. Identify the biceps bursa proximal to the fibular head and carefully penetrate to expose the FCL. The FCL can also be found by following the biceps anteriorly to its attachment on the fibular head with the knee at 90° flexion. The FCL runs perpendicular to the biceps and lateral to the popliteus tendon.
Peroneal Nerve
The landmarks to identify the peroneal nerve are the inferior border of the biceps femoris and the posterolateral fibular neck. Find the fatty tissue at this corner and carefully dissect with a blunt instrument instead of the shaver or radiofrequency device to prevent iatrogenic injury. The peroneal nerve is located just behind this fatty tissue.
Step 2: Graft Preparation
Semitendinosus and peroneus longus tendons are used for PT and combination FCL-PFL reconstruction, respectively. Tendon length of ≥22 cm is necessary for the grafts to exit the anterolateral tibial tunnel with sufficient length to allow for distal fixation.1 The grafts must be prepared to pass through a 7-mm tunnel and the tendon ends tubularized.
Step 3: Tunnel Drilling
Tibia Tunnel Drilling
Locate the muscle–tendon junction on the posterior aspect of the tibia and identify the insertion sites of the PFL on the tibia and fibula. Stay medial to the posterior tibiofibular joint and distal to the posterior tibial articular surface (Fig 1). Insert the ACL femoral drill guide (Arthrex, Naples, FL) through the posterolateral portal.
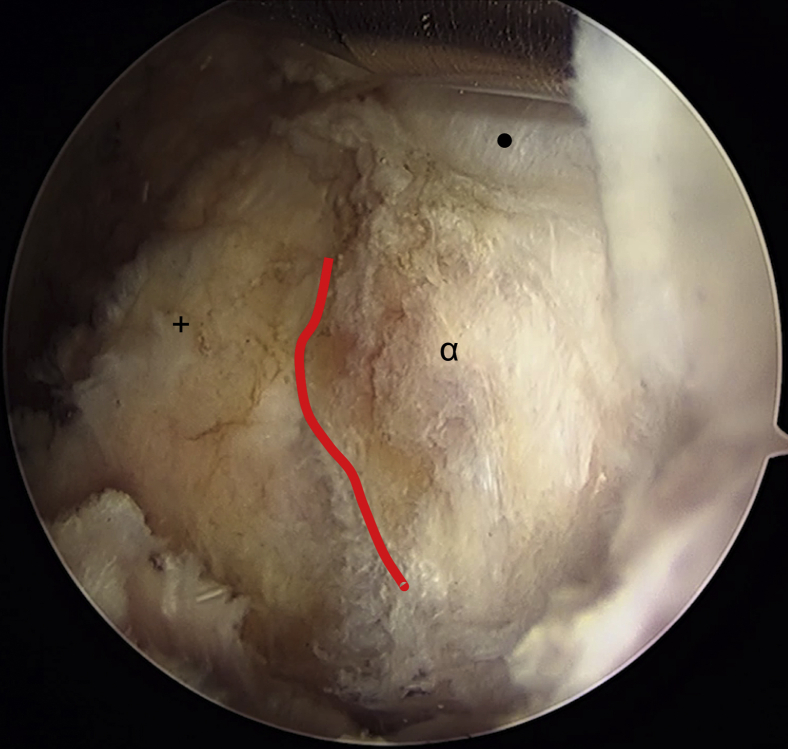
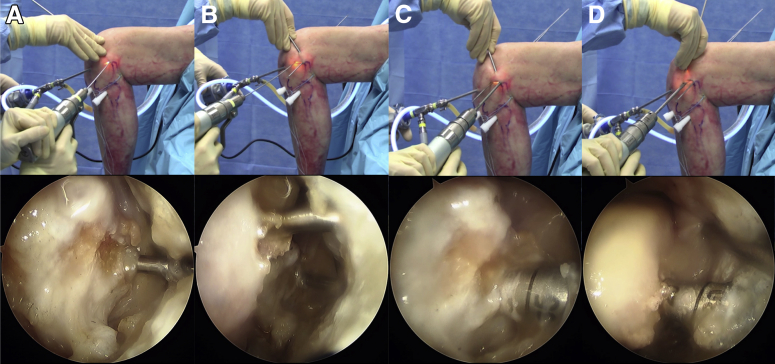
Fig 1.
Left knee in 90 degrees of flexion. Arthroscopic view of posterior tibial popliteal sulcus. Symbols: +, fibular head; α, tibia; •, cartilage; red line, tibiofibular joint line.
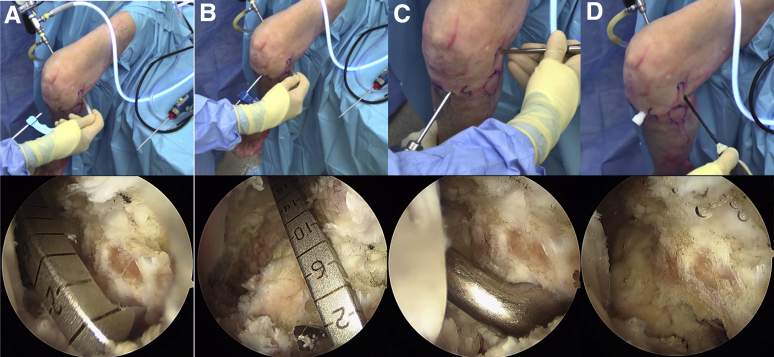
Place the tip of the guide in the middle of the PFL insertion site on the tibia at the level of the tip of the fibula6 (Fig 2A). Position the anterior start point of the drill guide between the lateral edge of the tibial tuberosity and the medial edge of Gerdy’s tubercle. Drill a Kirschner wire (K-wire) in an anteroposterior direction through the guide (Fig 2B). Ream a 10-mm tunnel over the K-wire, and place a curette over the tip for protection (Fig 2C). Clean the entry and exit sites of both tunnels with the shaver (Fig 2D).
Fig 2.
Left knee in 90 degrees of flexion. Tibia tunnel drilling. (A) Guide placed in the middle of the popliteofibular ligament insertion site on the tibia at the level of the tip of the fibula. (B) Drill guide between the lateral edge of the tibial tuberosity and the medial edge of Gerdy's tubercle. (C) 10-mm tunnel over the Kirschner wire (curette over the tip for protection). (D) Shaving entry and exit sites of both tunnels.
Fibula Tunnel Drilling
Make a small vertical incision (1 to 1.5 cm long) on the anterolateral aspect of the fibula head through the anterior arm of the long head of the biceps femoris. Incise the biceps bursa to locate and tag the FCL with a suture. Identify the attachment site of the FCL on the lateral aspect of the fibular head. Insert the ACL femoral guide through the posterolateral portal and target the fibular insertion of the popliteofibular ligament on the posteromedial aspect of the fibular head (Fig 3A). Drill a K-wire through the fibular head from the attachment site of the fibular collateral ligament on the anterolateral aspect of the fibular head to the attachment site of the popliteofibular ligament on the posteromedial fibular styloid (Fig 3A). Ream 6.5-mm tunnel over the K-wire using a protective curette on the tip (Fig 3B). Debride the entry and exit sites of both tunnels with a shaver (Fig 3C).
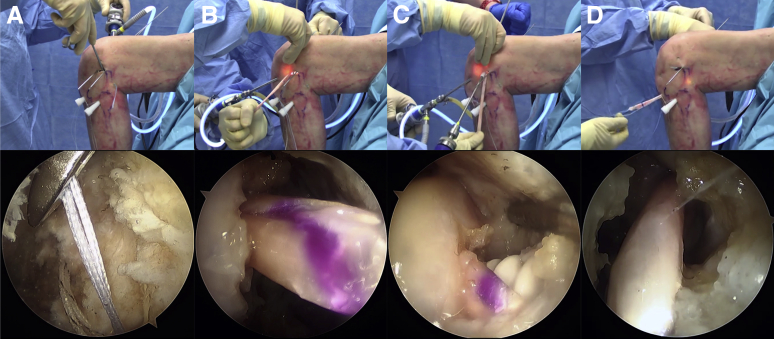
Fig 3.
Left knee in 90 degrees of flexion. Fibular tunnel drilling. (A) Guide position on the fibular insertion of the popliteofibular ligament on the posteromedial aspect of the fibular head and Kirschner wire drilled through the fibular head. (B) Fibula head, 6.5-mm reaming. (C) Tunnel extremities debridement with a shaver.
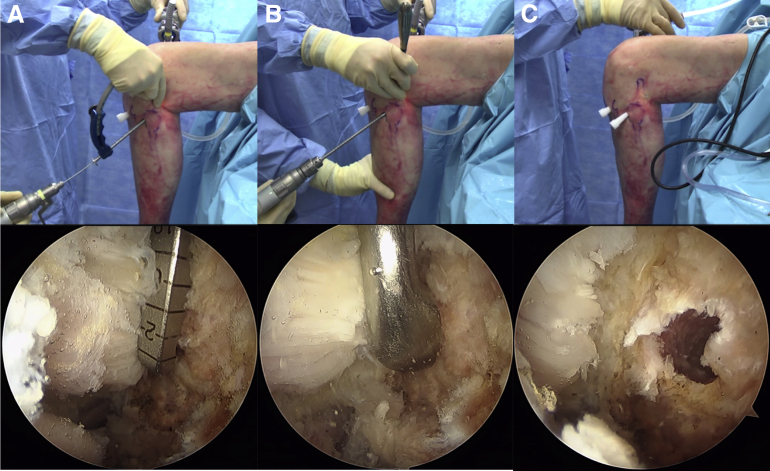
Step 4: Suture Passage
Loop a passing suture through the tibial tunnel from anterior to posterior (Fig 4A). Insert an arthroscopic grasper into the posterolateral compartment through the PL portal to grab the loop toward the fibular tunnel aperture. Place the grasper through the fibular tunnel from anterior to posterior to pull out the passing suture loop (white for FCL-PFL) (Fig 4C, D). Insert another passing suture through the tibial tunnel and retrieve it through the PL portal (blue for PT) (Fig 4B).
Fig 4.
Left knee in 90 degrees of flexion. Passing suture. (A) Passing suture through the tibial tunnel from anterior to posterior. (B) A second passing suture through the tibial tunnel pulled through the posterolateral portal. (C and D) Passing suture loop pulled out.
Step 5: Femoral Socket Reaming
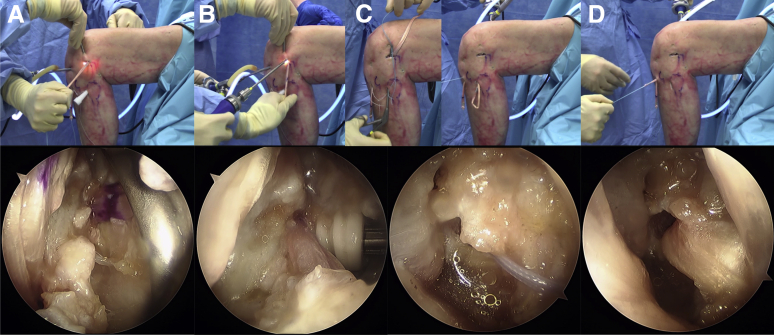
Introduce the 30° arthroscope from the AL portal into the lateral gutter. Make a vertical (1- to 1.5-cm) skin incision under arthroscopic vision between the PT and FCL footprints. Place K-wires in the middle of the femoral footprint of the PT and in the femoral footprint of the FCL (Fig 5A, B). The measured distance between the K-wires is ∼18.5 mm. Drill the femoral sockets with a 7-mm reamer to a depth of 25 mm for the PT and 30 mm for the FCL (Fig 5C, D). Load the Beath pin with suture and pass it out the medial side of the knee. Use a trocar through the superolateral (SL) portal as a retractor.
Fig 5.
Left knee in 90 degrees of flexion. Femoral socket reaming. (A and B) 30 arthroscope introduced from the anterolateral portal into the lateral gutter. Kirschner wire placement on patellar tendon and fibular collateral ligament footprints. (C and D) 7-mm reaming.
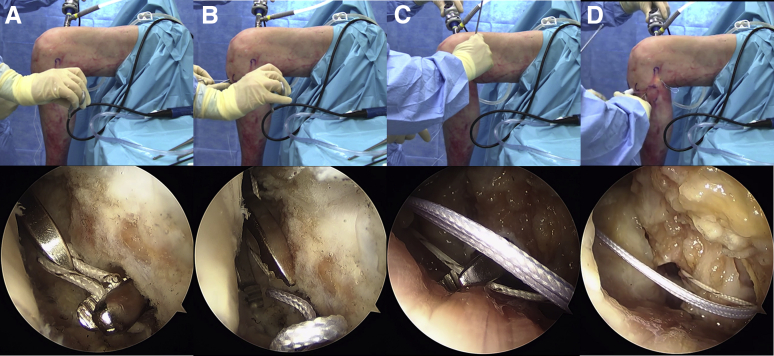
Step 6: Graft Passage and Fixation
Popliteus Graft
Insert the arthroscopic grasper into the SL incision to reach the posterolateral compartment through the popliteus hiatus along the native direction of the popliteus tendon (Fig 6A). Retrieve the previous passing suture (blue) to advance the PT graft along the trajectory of the native tendon.
Fig 6.
Left knee in 90 degrees of flexion. Popliteus graft passage. (A) Arthroscopic grasper through the popliteus hiatus along the native direction of the popliteus tendon. (B) Patellar tendon (PT) graft femoral passage. (C) PT graft fixation. (D) PT graft passage through the tibial tunnel.
Introduce the PT graft into the previously created femoral socket with the suture loop through the use of the eyelet guide pin (Fig 6B). Fix the popliteus femoral sided graft with an 8- by 23-mm cannulated bioabsorbable interference screw (Fig 6C). Bring the previously docked blue suture out the PL portal into the SL incision using a grasper. Pass the PT graft deep to the native PT into the PL compartment and then into the tibial tunnel in a posterior to anterior direction (Fig 6D).
FCL and Popliteofibular Graft
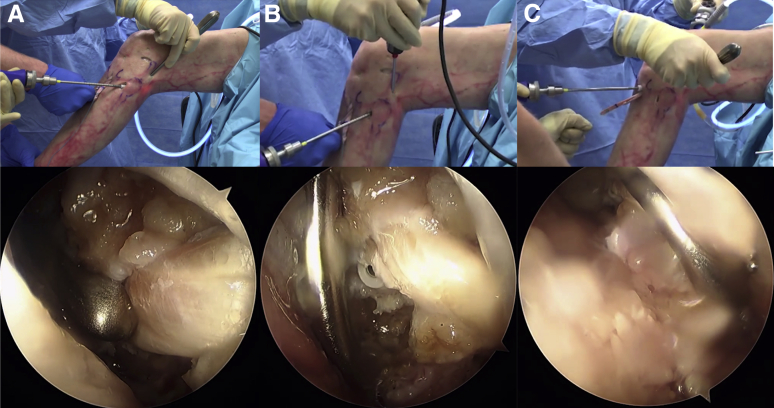
Pass the FCL graft through the femoral socket as described above for the popliteus graft (Fig 7A). Fix the FCL femoral graft side with an 8- by 28-mm cannulated bioabsorbable interference screw (Fig 7B).
Fig 7.
Left knee in 90 degrees of flexion. FCL-PFL passage. (A) FCL graft through the femoral tunnel. (B) FCL graft fixation. (C) FCL graft passage through the fibular tunnel in an anterior to posterior direction. (D) FCL graft passage through the tibial tunnel in a posterior to anterior direction. Abbreviations: FCL, fibular collateral ligament; PFL, popliteofibular ligament.
Develop the interval deep to the superficial layer of the iliotibial band by blunt dissection using a curved hemostat. Insert a grasper into this interval through the anterior fibular drilling incision, following the course of the FCL. Pass the FCL graft through the fibular tunnel in an anterior to posterior direction, and then into the tibial tunnel from posterior to anterior (Fig 7C, D).
Final Graft Fixation
With the knee at 30° flexion and neutral rotation, tension and fix the FCL graft in the fibular tunnel with a 7- by 23-mm cannulated bioabsorbable interference screw (Fig 8A, B). Simultaneously tension both grafts on the tibia by applying an anterior load to the grafts at 60° flexion and neutral rotation of the leg position. Fix the grafts with a 10- by 28-mm cannulated interference screw in the tibial tunnel (Fig 8C).
Fig 8.
Left knee in 60 degrees of flexion. Final fixation. (A and B) fibular collateral ligament (FCL) graft fixation in the fibular tunnel. (C) FCL graft fixation in the tibial tunnel.
Discussion
The study demonstrates that anatomic reconstruction of the fibular collateral ligament, popliteofibular ligament, and popliteus tendon can be performed with an all-arthroscopic technique. This operative procedure is reproducible and safe, since the peroneal nerve is directly visualized. An advantage of this technique is that a large lateral incision is not required, nor is extensive dissection of the posterolateral structures.
Numerous open posterolateral reconstruction techniques have been described to restore posterolateral stability. These techniques are classified as anatomic and nonanatomic. Biomechanical studies show that anatomic PLC reconstruction restores knee kinematics better than nonanatomic procedures.9 The PFL is an important structure that requires reconstruction.9 Two different techniques are generally used, tibiofibular1 and femorofibular.4 Yoon et al.4 found no significant differences in clinical outcomes or varus stability between these 2 techniques in patients with posterolateral corner injuries. We chose to replicate the LaPrade/Engebretsen technique,1 awhich has both biomechanical validity and successful clinical outcomes.10
A minimally invasive approach places the neurovascular structures at risk during anatomic fibular tunnel placement. Therefore, most anatomic techniques described in the literature are performed open. with exposure of the peroneal nerve. Frosch et al.6 concluded that the fibular head could not be arthroscopically visualized; therefore, an all-arthroscopic PFL reconstruction was not technically possible. However, Song et al.11 described an anatomic PFL reconstruction under arthroscopy with fibular head and native popliteofibular visualization, but without peroneal nerve exposure. In our study, we achieved anatomic placement of the fibular tunnel with a safe trajectory while directly visualizing the peroneal nerve. The safe zone is supported by the fact that the peroneal nerve crosses the posterior border of the fibula 21.9 mm from the tip of the styloid with the knee in 90° flexion.12
We enhanced the technique of Frosch et al.6 by creating an anatomic posterior tibial tunnel and precisely visualizing the fibular head, PFL, and proximal tibiofibular joint. Identification of the fibular head is an important cornerstone to accurately perform this surgical procedure. The anatomic tibial tunnel position is located directly at the crossing of a horizontal line at the tip with a vertical line at the medial edge of the fibula.6 Visualization of the sulcus is difficult with the open procedure; it is usually found indirectly by palpation.
Potential complications of this technique should be highlighted. There is risk of vascular injury to the popliteal and lateral inferior genicular arteries when exposing the posterior septum and the musculotendinous junction of the popliteus. To avoid vascular injury, the shaver jaws should always face anteriorly when removing synovial tissue until the popliteus musculotendinous junction is clearly identified. Also, common peroneal nerve injury, deep vein thrombosis, and tunnel mismatch are potential complications. In addition, posterolateral capsule detachment with extravasation of irrigation fluid could risk acompartment syndrome. Iatrogenic PLC instability is a concern, but the biomechanical study by Domnick et al.13 showed that resection of the popliteomeniscal fibers resected during the arthroscopic approach does not significantly affect stability.
In conclusion, this study describes an all-arthroscopic, anatomic PLC reconstruction technique for the PT, PFL, and FCL. This procedure retains the advantages of minimally invasive arthroscopic procedures while replicating the well-established Laprade/Engebresten anatomic technique. Biomechanical and clinical studies are needed to validate this method.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.S.-C. reports personal fees, Arthrex. A.J.K. reports personal fees, Arthrex, Vericel, Aesculap/B, Braun, Arthritis Foundation, Ceterix, Histogenics. M.J.S. reports personal fees, Arthrex, Stryker. B.A.L. reports personal fees, Arthrex, Smith & Nephew, Stryker, Biomet. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This cadaveric study presents a reproducible all-arthroscopic procedure for anatomic posterolateral corner reconstruction conducted in the following 5 steps: graft preparation, tunnel drilling, suture passage, femoral socket reaming, and graft passage and fixation. Arthroscopic portals and identification and exposure of the posterolateral structures are described in Part 1.
References
- 1.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomic posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 2.Miyatake S., Kondo E., Tsai T.-Y. Biomechanical comparisons between 4-strand and modified Larson 2-strand procedures for reconstruction of the posterolateral corner of the knee. Am J Sports Med. 2011;39:1462–1469. doi: 10.1177/0363546511404135. [DOI] [PubMed] [Google Scholar]
- 3.Blackman A.J., Engasser W.M., Krych A.J., Stuart M.J., Levy B.A. Fibular head and tibial-based (2-Tailed) posterolateral corner reconstruction. Sports Med Arthrosc Rev. 2015;23:44–50. doi: 10.1097/JSA.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 4.Yoon K.H., Lee S.H., Park S.Y., Park S.E., Tak D.H. Comparison of anatomic posterolateral knee reconstruction using 2 different popliteofibular ligament techniques. Am J Sports Med. 2016;44:916–921. doi: 10.1177/0363546515623966. [DOI] [PubMed] [Google Scholar]
- 5.Frosch K.-H., Akoto R., Drenck T., Heitmann M., Pahl C., Preiss A. Arthroscopic popliteus bypass graft for posterolateral instabilities of the knee: A new surgical technique. Oper Orthop Traumatol. 2016;28:193–203. doi: 10.1007/s00064-015-0432-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frosch K.-H., Akoto R., Heitmann M., Enderle E., Giannakos A., Preiss A. Arthroscopic reconstruction of the popliteus complex: Accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc. 2015;23:3114–3120. doi: 10.1007/s00167-014-3000-y. [DOI] [PubMed] [Google Scholar]
- 7.Frings J., Kolb J.P., Drenck T.C. Anatomic reconstruction of the posterolateral corner: An all-arthroscopic technique. Arthrosc Tech. 2019;8:e153–e161. doi: 10.1016/j.eats.2018.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu P., Wang J., Zhao F., Xu Y., Ao Y. Anatomic, arthroscopically assisted, mini-open fibular collateral ligament reconstruction: An in vitro biomechanical study. Am J Sports Med. 2014;42:373–381. doi: 10.1177/0363546513508536. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy M., Camarda L., Wijdicks C.A., Johansen S., Engebretsen L., Laprade R.F. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med. 2010;38:1674–1681. doi: 10.1177/0363546510361220. [DOI] [PubMed] [Google Scholar]
- 10.Woodmass J.M., Johnson N.R., Mohan R., Krych A.J., Levy B.A., Stuart M.J. Poly-traumatic multi-ligament knee injuries: Is the knee the limiting factor? Knee Surg Sports Traumatol Arthrosc. 2018;26:2865–2871. doi: 10.1007/s00167-017-4784-3. [DOI] [PubMed] [Google Scholar]
- 11.Song G.-Y., Zhang H., Zhang J., Li Y., Feng H. Anatomic popliteofibular ligament reconstruction of the knee joints: An all-arthroscopic technique. Knee Surg Sports Traumatol Arthrosc. 2015;23:2925–2929. doi: 10.1007/s00167-015-3531-x. [DOI] [PubMed] [Google Scholar]
- 12.Hildebrand G., Tompkins M., Macalena J. Fibular head as a landmark for identification of the common peroneal nerve: A cadaveric study. Arthroscopy. 2015;31:99–103. doi: 10.1016/j.arthro.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Domnick C., Frosch K.-H., Raschke M.J. Kinematics of different components of the posterolateral corner of the knee in the lateral collateral ligament-intact state: A human cadaveric study. Arthroscopy. 2017;33:1821–1830.e1. doi: 10.1016/j.arthro.2017.03.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This cadaveric study presents a reproducible all-arthroscopic procedure for anatomic posterolateral corner reconstruction conducted in the following 5 steps: graft preparation, tunnel drilling, suture passage, femoral socket reaming, and graft passage and fixation. Arthroscopic portals and identification and exposure of the posterolateral structures are described in Part 1.