Abstract
The number of anterior cruciate ligament (ACL) reconstructions in skeletally immature patients has been gradually increasing in recent years owing to the poor outcomes of conservative treatment. However, ACL reconstruction in children is a challenging procedure and may lead to severe complications, such as growth disturbance. Although double-bundle (DB) ACL reconstructions are preferable because of their superior clinical outcomes, there are few reports of DB ACL reconstruction in children with open epiphyses. In this Technical Note, an all-epiphyseal sparing DB ACL reconstruction technique, which is considered to help avoid growth disturbance, is described. This procedure does not create a thick tunnel and may facilitate subsequent revision surgery.
Anterior cruciate ligament (ACL) injuries in skeletally immature patients are increasing owing to early sports participation and specialization of young athletes, year-round training, and longer practice times.1 Conservative treatments are not effective in preventing instability or further meniscal and cartilage damage.1 Therefore, multiple studies have recommended surgical intervention. However, ACL reconstruction in patients with open physes may result in severe complications, including leg-length discrepancy and valgus or recurvatum angular deformities. Furthermore, the optimal reconstruction procedure for patients with open physes remains unknown.
Several techniques deemed “physeal-respecting” techniques have been reported to avoid growth disturbance.2 They include use of soft-tissue graft material, small-diameter drilling (≤8 mm), vertical bone tunneling, and fixation, as well as avoidance of a laterally placed tunnel. Additionally, various physeal-sparing techniques with a variety of tunneling methods have been reported. The “over-the-top” technique is one of the reliable approaches to prevent physeal injury.3 Anderson4 first reported an “all-epiphyseal” technique to minimize the risk of physeal injury in a more anatomic fashion. In this technique, all bone tunnels drilled are contained completely within the epiphyses in the skeletally immature knee, which attains proper graft position. Koizumi et al.5 reported on physeal-sparing double-bundle (DB) ACL reconstruction, in which the posterolateral bundle (PLB) was reconstructed by an all-epiphyseal technique and the anteromedial bundle (AMB) was reconstructed by an over-the-top technique. Therefore, the AMB was reconstructed in an extra-articular fashion. Since 2005, we have performed DB ACL reconstruction with all-epiphyseal tunnels and fixation within the epiphyses to reproduce a more anatomic ACL.6 The purpose of this Technical Note was to describe our procedure using hamstring tendon.
Surgical Technique
Surgical Indication
Our surgical technique is shown in Video 1. In principle, skeletally immature patients with wide open physes are indicated for conservative treatment to prevent the risk of growth disturbance. However, if a patient with growth remaining complains of knee instability during activity or has a secondary meniscal injury develop, physeal-sparing ACL reconstruction is considered.
Patient Positioning and Diagnostic Arthroscopy
Under general anesthesia, the patient is placed supine on the operating table at 90° of knee flexion with the use of supporting plates. Diagnostic arthroscopy with a 30° arthroscope is performed through standard anterolateral and anteromedial portals. If necessary, intra-articular lesions, such as meniscal tears, are treated (Fig 1). Although the anterolateral portal is used as a scoping portal, the anteromedial portal is essential to identify the femoral attachment and determine the precise femoral tunnel position (Fig 2). We prefer to use a radiofrequency device for removing soft tissue to preserve the bony landmark (resident ridge).
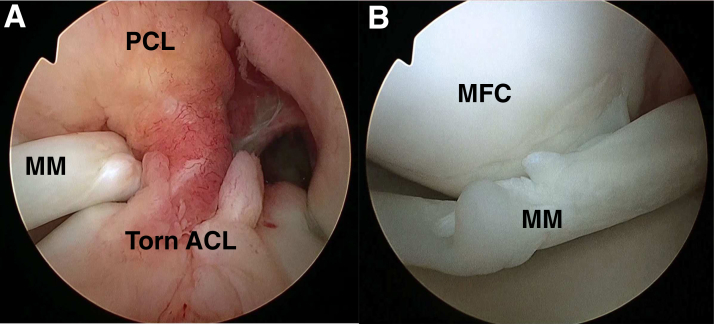
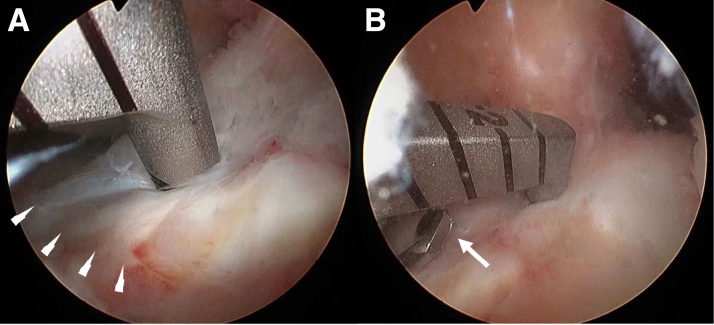
Fig 1.
Arthroscopic view of the intercondylar notch in a left knee from the anterolateral portal. (A) The anterior cruciate ligament (ACL) is completely torn. (B) Bucket-handle tear of medial meniscus (MM). The MM was reduced and then repaired using the inside-out technique. (MFC, medial femoral condyle; PCL, posterior cruciate ligament.)
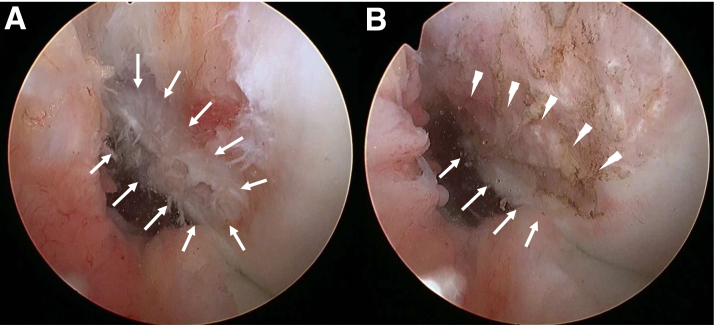
Fig 2.
Identification of the anterior cruciate ligament femoral footprint (left knee, viewed through anteromedial portal). (A) Anterior cruciate ligament femoral footprint (arrows). (B) The resident ridge (arrowheads) and articular cartilage margin of the posterior femoral condyle (arrows) should be identified.
Graft Harvest and Preparation
The semitendinosus tendon (ST) is first harvested using standard techniques through a 2-cm vertical skin incision. Because all bone tunnels are contained within the epiphyses and each tunnel is not particularly long, the ST alone is usually enough for all-epiphyseal DB ACL reconstruction. The harvested ST is cut in half, with the distal half used for the AMB and the proximal half used for the PLB. A No. 2 FiberWire (Arthrex, Naples, FL) is placed at the ends of the tendons with a whipstitch, and the tendon is looped over a No. 2 FiberWire or cortical suspensory device (TightRope [Arthrex] or EndoButton [Smith & Nephew, Andover, MA]). The doubled tendons are then placed under tension using a Graftmaster device (Smith & Nephew).
Guide Pin Placement
First, a small longitudinal skin incision is made above the lateral epicondyle of the femur (Fig 3A); then, the iliotibial band is incised along the fiber direction. While visualizing the femoral ACL footprint through the anteromedial portal, the tip of an outside-in Small Angle Footprint Femoral ACL Guide (AR-1510FRS; Arthrex) is set at the center of the AMB femoral footprint through the anterolateral portal (Fig 3B). If this specific guide is not available, an outside-in PCL femoral guide is useful for inserting the guide pin while avoiding epiphyseal injury. A 2.4-mm guide pin is inserted into the AMB footprint through a 2.4-mm Guide Pin Sleeve (AR-1204F-24I; Arthrex) with a Stepped Ratchet Drill Sleeve (AR-1510FS-7; Arthrex) (Fig 4A). Next, the tip of the femoral guide is set at the center of the PLB footprint, and a second guide pin for the PLB is inserted in the same manner (Fig 4B).
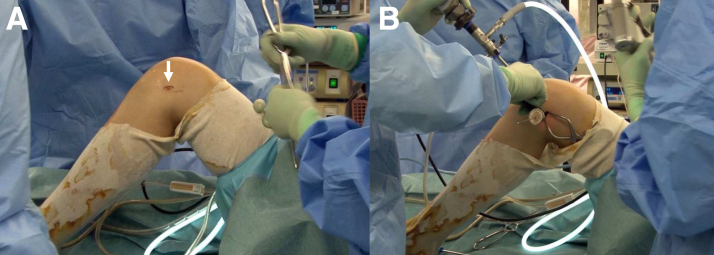
Fig 3.
Lateral skin incision for femoral tunnel drilling (left knee, lateral view). (A) The patient is placed in the supine position, and the knee is maintained at 90° of flexion. A small longitudinal skin incision (arrow) is made above the lateral femoral epicondyle. (B) An outside-in guide is set on the lateral femoral condyle.
Fig 4.
Insertion of femoral guide pins (left knee, viewed through anteromedial portal). (A) The tip of an outside-in guide is set at the center of the anteromedial bundle femoral footprint through the anterolateral portal. (B) The tip of the guide is set at the center of the posterolateral bundle femoral footprint (asterisk). The arrow shows the guide pin tip of the anteromedial bundle.
Subsequently, tibial guide pins are inserted into the ACL tibial footprint using a tibial guide (Small-Angle Pin Tip Tibial Marking Hook ACL Guide [AR-1510GTS]; Arthrex). The tip of the tibial guide is set at the center of the AMB tibial footprint through the anteromedial portal. This point is just behind the Parsons knob (Fig 5A). The first tibial guide pin is inserted through the skin incision for graft harvest. The second tibial guide pin is inserted into the PLB tibial footprint more medial to the tibia than the first (Fig 5B). The location of the pins is confirmed by radiographs (Fig 6).
Fig 5.
Insertion of tibial guide pins (left knee, viewed through anterolateral portal). (A) The tip of a tibial guide is set just behind the Parsons knob (arrowheads). (B) The tip of the guide is set at the center of the posterolateral bundle tibial footprint. The arrow shows the guide pin tip of the anteromedial bundle.
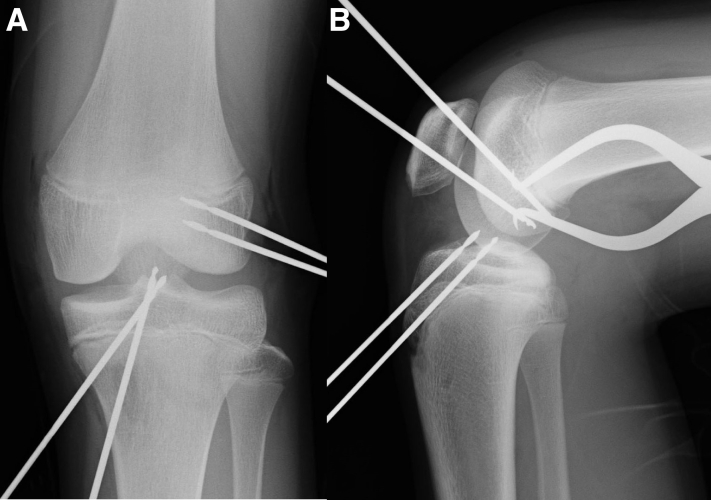
Fig 6.
Confirmation of guide pin position (left knee). (A) Anteroposterior view. (B) Lateral view.
Femoral Socket Drilling
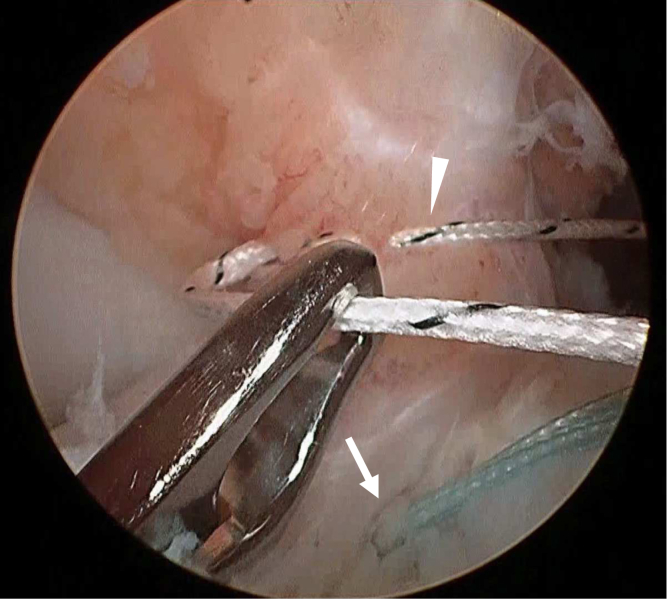
If the pin positions are appropriate, the femoral sockets are created before tibial tunnel creation. The guide pin sleeve and stepped drill sleeve are set over the PLB femoral guide pin, and the stepped drill sleeve is hammered and fixed at the femoral cortex. The guide pin and the guide pin sleeve are changed for the appropriately sized retrograde reamer (Short FlipCutter II [AR-1204AS]; Arthrex), which is drilled into the joint through the stepped drill sleeve (Fig 7). After the blade is flipped and locked in the cutting position, retrograde drilling of the femoral socket of the PLB is performed at about 20 mm of depth. The reamer is advanced into the joint, and the blade is flipped and removed. A FiberStick (Arthrex) is advanced through the stepped drill sleeve, delivered out through the anterolateral portal, and tagged for later graft passage (Fig 8A). The femoral socket for the AMB is created in the same manner. The femoral socket for the PLB should be created first. Otherwise, the FiberWire for the AMB may be damaged by drilling for the PLB femoral socket (Fig 8B).
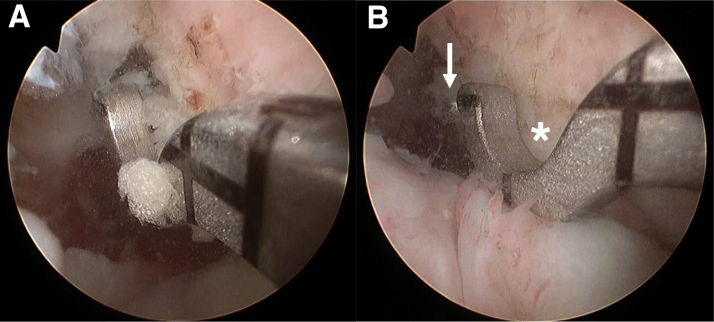
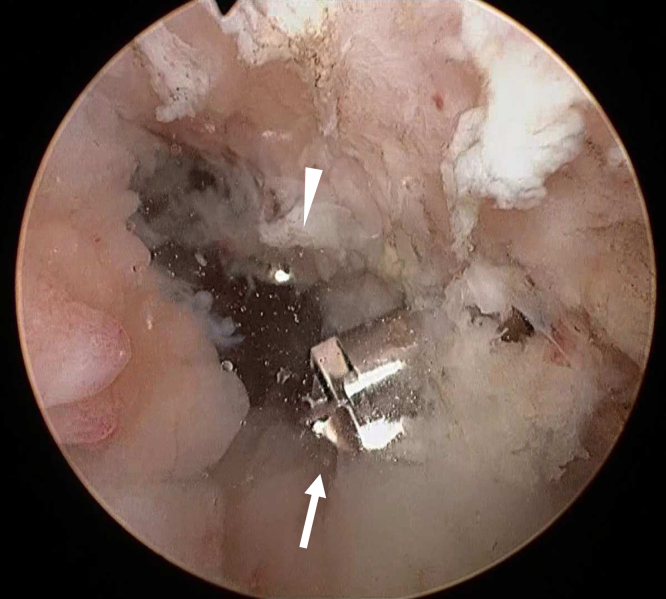
Fig 7.
Femoral socket creation (left knee, viewed through anterolateral portal). The femoral socket for the posterolateral bundle should be created first by a retrograde reamer (Arthrex FlipCutter, arrow). The arrowhead shows the tip of the anteromedial bundle femoral guide pin.
Fig 8.
Passage of pullout sutures (left knee, viewed through anterolateral portal). (A) A FiberStick (Arthrex) is advanced through the femoral socket of the posterolateral bundle (PLB). (A) FiberSticks are delivered out through the anterolateral portal and tagged for later graft passage.
Tibial Tunnel Drilling
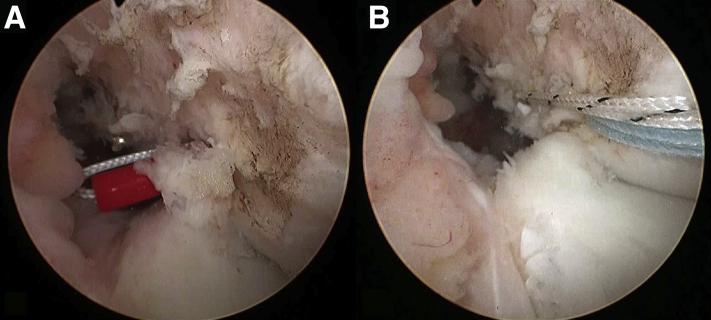
The previously inserted guide pins are over-drilled from the tibial side using an appropriately sized standard cannulated reamer. By use of an open suture retriever, each end of the previously passed FiberStick is pulled out through each tibial tunnel (Fig 9).
Fig 9.
FiberSticks are pulled out through each tibial tunnel (left knee, viewed through anterolateral portal). The blue suture (arrow) is for the posterolateral bundle, and the white suture (arrowhead) is for the anteromedial bundle.
Graft Passage and Fixation
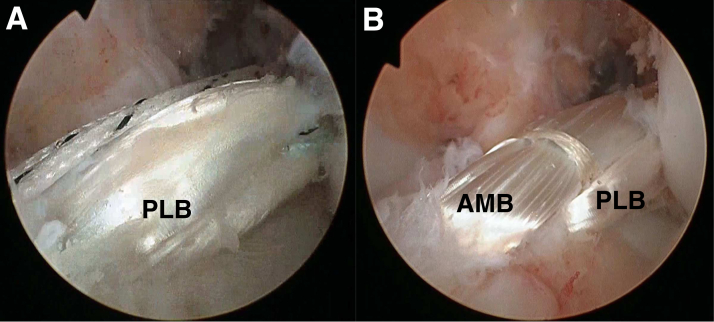
A No. 2 FiberWire or the pullout suture of the cortical suspensory device connected to the graft is pulled out from the tibial tunnel to the femoral socket. The PLB graft is then introduced into the joint, followed by the AMB graft (Fig 10). If a secure bone bridge between the AMB and PLB sockets is obtained, cortical suspensory devices may not be needed. The FiberWire of each graft is pulled up until the proximal graft end is in contact with the bottom of the socket. The AMB and PLB FiberWires are then tied together on the femoral cortex. If cortical suspensory devices are used, the buttons are flipped on the femoral cortex.
Fig 10.
Graft passage (left knee, viewed through anterolateral portal). (A) The posterolateral bundle (PLB) graft is introduced first. (B) After double-bundle anterior cruciate ligament reconstruction. (AMB, anteromedial bundle.)
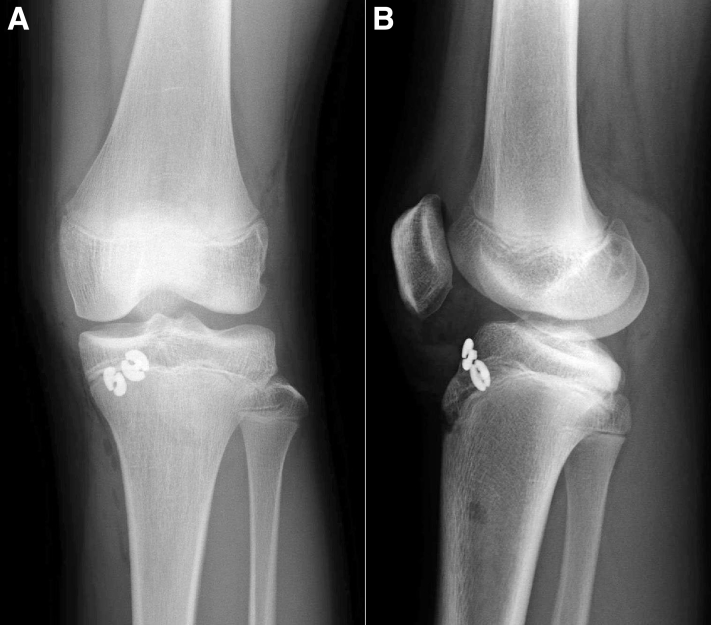
For final graft fixation, the knee is maintained at 20° of flexion. The PLB graft is first fixed by tying the FiberWire over a tibial disk, which is positioned proximal to the tibial physis. The AMB graft is subsequently fixed in the same manner (Figs 11 and 12). Although we have never experienced grafts extending through the tibial tunnel, they can be fixed to a tibial screw on the anterior aspect of the tibia.4 The skin incisions are closed according to the standard protocol.
Fig 11.
Postoperative radiographs (left knee). (A) Anteroposterior view. (B) Lateral view.
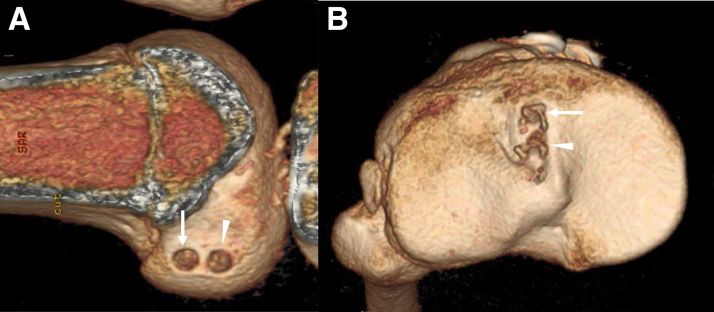
Fig 12.
Postoperative 3-dimensional computed tomography (left knee). (A) Medial view of femoral tunnels (lateral femoral condyle). (B) Upper view of tibial tunnels. The arrows show the anteromedial bundle tunnels, whereas the arrowheads show the posterolateral bundle tunnels.
Postoperative Rehabilitation
The knee is kept in extension using a brace after surgery. Range of motion and muscle control exercises, such as patellar setting and straight-leg raising, are started the day after surgery. Patients are allowed to jog at 3 months postoperatively and recommended to return to sports at 9 to 12 months. The advantages and disadvantages as well as pearls and pitfalls of this procedure are summarized in Tables 1 and 2.
Table 1.
Advantages and Disadvantages of All-Epiphyseal Double-Bundle ACL Reconstruction for Skeletally Immature Patients
| Advantages |
| Physeal injury is avoided. |
| Harvesting of only the semitendinosus tendon is required. |
| A small-diameter tunnel is used. |
| The native ACL footprints (femoral and tibial) are restored. |
| Revision surgery is simplified. |
| Disadvantages |
| The procedure is technically demanding. |
| An extra lateral incision is required for the outside-in technique. |
| Cortical suspensory devices are placed within the joint. |
| No evidence of clinical advantages has been observed in skeletally immature patients. |
ACL, anterior cruciate ligament.
Table 2.
Pearls and Pitfalls of All-Epiphyseal Double-Bundle ACL Reconstruction for Skeletally Immature Patients
| Pearls |
| A small-angle outside-in guide is necessary create the femoral tunnel. |
| Intraoperative radiographs should be obtained to confirm optimal guide pin positioning. |
| Pitfalls |
| The femoral socket for the posterolateral bundle should be created first to prevent damage to the FiberStick. |
| Placement of a guide pin is important to prevent tunnel coalition in small joints. |
ACL, anterior cruciate ligament.
Discussion
The most significant feature of this technique is that DB ACL grafts can be placed in the anatomic position while sparing both the femoral and tibial physes. Our clinical results were almost satisfactory without any significant growth disturbance.6 Several authors have reported on all-epiphyseal ACL reconstruction techniques.3,4,7,8 On the basis of a recent systematic review of 17 articles (N = 545), all-epiphyseal ACL reconstruction was very safe and had excellent postoperative functional results.8 Only 8 of 545 patients (1.5%) showed growth disturbances. Of course, there are potential risks to all-epiphyseal ACL reconstruction, such as graft rerupture, limb overgrowth, limb-length discrepancies, arthrofibrosis, knee stiffness, soft-tissue infection,8 and EndoButton migration within the joint.6
Several meta-analyses have shown that DB reconstruction decreases the postoperative positive pivot-shift ratio significantly more than single-bundle (SB) reconstruction.9 However, no studies have compared the clinical results of SB and DB ACL reconstructions in skeletally immature patients. Koizumi et al.5 evaluated the clinical outcomes of their physeal-sparing DB ACL reconstruction and compared these with those of adults. They concluded that their physeal-sparing technique in adolescents with open physes resulted in good clinical outcomes similar to those of anatomic DB ACL reconstruction in adults without growth abnormalities.
We cannot conclude that DB is superior to SB reconstruction in skeletally immature patients. However, there are some possible advantages. Although all-epiphyseal techniques minimize the risk of growth disturbance, damage to the growth plate may still occur during epiphyseal drilling. DB techniques increase the safety margin by decreasing the tunnel diameter.7 ACL reconstruction in pediatric patients is associated with relatively high reinjury rates, and surgical revision may be required.9 Whereas large tunnels made for thicker SB grafts may compromise subsequent revisions, small double tunnels will not. Furthermore, double femoral tunnels do not require cortical suspensory devices because the connecting sutures of the AMB and PLB grafts are on the femoral cortex. Because femoral cortical suspensory devices are placed within the joint, migration is possible. In fact, we have experienced a case in which the EndoButton migrated into the popliteal fossa as the patient grew.6 Therefore, we do not use cortical suspensory devices for femoral fixation if a secure bone bridge between the AMB and PLB sockets is obtained.
We acknowledge some limitations to our procedure. The most significant limitation is that we cannot prove the superiority of the DB procedure because the limited number of skeletally immature patients does not allow for randomized study. However, this procedure is not particularly challenging for surgeons who are familiar with DB ACL reconstruction using the outside-in technique. We believe that the all-epiphyseal DB technique is a promising alternative for ACL reconstruction in skeletally immature patients.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video shows all-epiphyseal double-bundle anterior cruciate ligament (ACL) reconstruction for skeletally immature patients. This patient was 12-year-old female basketball player with open physis. Despite conservative treatment for ACL injury of the left knee, she suffered medial meniscus injury. Therefore, we decided to perform physeal sparing ACL reconstruction. Under general anesthesia, the patient is placed supine on the operation table. Diagnostic arthroscopy is performed. The bucket handle tear of the medial meniscus is reduced and then repaired using inside-out technique. The femoral soft tissue is removed by punch and shaver, and the ACL femoral attachment identified through the anteromedial portal. We prefer to use a radiofrequency device for removing soft tissue to preserve the bony landmark. The resident's ridge and posterior cartilage margin are also identified. A small longitudinal skin incision is made above the lateral femoral epicondyle, and then the iliotibial band incised. The guide pin of the AM bundle is inserted into the AM bundle footprint using a small angle femoral ACL guide. Then the second guide pin for PL bundle is also inserted in the same manner. Subsequently, tibial guide pins are inserted into the ACL tibial footprint using a small angle tibial guide. The AM bundle guide pin is inserted first, and then the PL bundle guide pin is inserted. Location of these guide pins is confirmed by X-ray. If the pin positions are appropriate, the femoral sockets are created before tibial tunnel creation. The femoral socket for PL bundle is created by a FlipCutter at about 20 mm of depth. A FiberStick is advanced through the drill sleeve and delivered out through the anterolateral portal. The femoral socket for AM bundle is also created in the same manner. The previously inserted tibial guide pins are over-drilled using a standard cannulated reamer. And then we check the position. Using a suture retriever, each end of FiberStick is pulled out through each tibial tunnel. The pull-out suture connected to the graft is pulled out from the tibial tunnel to the femoral socket. The PL bundle graft is introduced into the joint, followed by the AM bundle graft. Proximal sutures of the AM and PL bundle are tied together on the femoral cortex, and distal sutures are fixed at suture buttons. 3D-CT shows anatomically placed femoral and tibial tunnels.
References
- 1.Pierce T.P., Issa K., Festa A., Scillia A.J., McInerney V.K. Pediatric anterior cruciate ligament reconstruction: A systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45:488–494. doi: 10.1177/0363546516638079. [DOI] [PubMed] [Google Scholar]
- 2.Cruz A.I., Jr., Fabricant P.D., McGraw M., Rozell J.C., Ganley T.J., Wells L. All-epiphyseal ACL reconstruction in children: Review of safety and early complications. J Pediatr Orthop. 2017;37:204–209. doi: 10.1097/BPO.0000000000000606. [DOI] [PubMed] [Google Scholar]
- 3.Roberti di Sarsina T., Macchiarola L., Signorelli C. Anterior cruciate ligament reconstruction with an all-epiphyseal "over-the-top" technique is safe and shows low rate of failure in skeletally immature athletes. Knee Surg Sports Traumatol Arthrosc. 2019;27:498–506. doi: 10.1007/s00167-018-5132-y. [DOI] [PubMed] [Google Scholar]
- 4.Anderson A.F. Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients. A preliminary report. J Bone Joint Surg Am. 2003;85:1255–1263. doi: 10.2106/00004623-200307000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Koizumi H., Kimura M., Kamimura T., Hagiwara K., Takagishi K. The outcomes after anterior cruciate ligament reconstruction in adolescents with open physes. Knee Surg Sports Traumatol Arthrosc. 2013;21:950–956. doi: 10.1007/s00167-012-2051-1. [DOI] [PubMed] [Google Scholar]
- 6.Kimura Y., Ishibashi Y. Pitfalls of Tight Rope or EndoButton fixation in ACL reconstruction using hamstring tendon. OS NEXUS. 2018;15:2–15. [in Japanese] [Google Scholar]
- 7.Espejo-Reina A., Espejo-Reina M.J., Rosa-Nogales J.D., Ruiz-Del Pino J., Espejo-Baena A. Physeal sparing anterior cruciate ligament reconstruction in skeletally immature patients bridging the tibial physis with two divergent tunnels. Arthrosc Tech. 2020;9:e747–e754. doi: 10.1016/j.eats.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta A., Tejpal T., Shanmugaraj A., Horner N.S., Gohal C., Khan M. All-epiphyseal anterior cruciate ligament reconstruction produces good functional outcomes and low complication rates in pediatric patients: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2020;28:2444–2452. doi: 10.1007/s00167-020-06085-3. [DOI] [PubMed] [Google Scholar]
- 9.Ishibashi Y., Adachi N., Koga H. Japanese Orthopaedic Association (JOA) clinical practice guidelines on the management of anterior cruciate ligament injury—secondary publication. J Orthop Sci. 2020;25:6–45. doi: 10.1016/j.jos.2019.10.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video shows all-epiphyseal double-bundle anterior cruciate ligament (ACL) reconstruction for skeletally immature patients. This patient was 12-year-old female basketball player with open physis. Despite conservative treatment for ACL injury of the left knee, she suffered medial meniscus injury. Therefore, we decided to perform physeal sparing ACL reconstruction. Under general anesthesia, the patient is placed supine on the operation table. Diagnostic arthroscopy is performed. The bucket handle tear of the medial meniscus is reduced and then repaired using inside-out technique. The femoral soft tissue is removed by punch and shaver, and the ACL femoral attachment identified through the anteromedial portal. We prefer to use a radiofrequency device for removing soft tissue to preserve the bony landmark. The resident's ridge and posterior cartilage margin are also identified. A small longitudinal skin incision is made above the lateral femoral epicondyle, and then the iliotibial band incised. The guide pin of the AM bundle is inserted into the AM bundle footprint using a small angle femoral ACL guide. Then the second guide pin for PL bundle is also inserted in the same manner. Subsequently, tibial guide pins are inserted into the ACL tibial footprint using a small angle tibial guide. The AM bundle guide pin is inserted first, and then the PL bundle guide pin is inserted. Location of these guide pins is confirmed by X-ray. If the pin positions are appropriate, the femoral sockets are created before tibial tunnel creation. The femoral socket for PL bundle is created by a FlipCutter at about 20 mm of depth. A FiberStick is advanced through the drill sleeve and delivered out through the anterolateral portal. The femoral socket for AM bundle is also created in the same manner. The previously inserted tibial guide pins are over-drilled using a standard cannulated reamer. And then we check the position. Using a suture retriever, each end of FiberStick is pulled out through each tibial tunnel. The pull-out suture connected to the graft is pulled out from the tibial tunnel to the femoral socket. The PL bundle graft is introduced into the joint, followed by the AM bundle graft. Proximal sutures of the AM and PL bundle are tied together on the femoral cortex, and distal sutures are fixed at suture buttons. 3D-CT shows anatomically placed femoral and tibial tunnels.