Abstract
Aims
Natural processes of change have been documented in treatment-seekers who begin to reduce their drinking in anticipation of treatment. The study examined whether non-treatment-seeking problem drinkers would engage in drinking reduction in anticipation of participating in a research study.
Methods
Non-treatment-seeking problem drinkers (n = 935) were culled from five behavioral pharmacology studies. Participants reported on their alcohol use during the past 30 days using the Timeline Followback. Cluster analysis identified distinct groups/clusters based on drinking patterns over the 30-day pre-visit period. The identified clusters were compared on demographic and clinical measures.
Results
Three distinct clusters were identified (a) heavy-decreasing drinking group (n = 255, 27.27%); (b) a moderate-stable drinking group (n = 353, 37.75%) and (c) low-stable drinking group (n = 327, 34.97%). The three clusters differed significantly on a host of measures including pre-visit drinking (age at first drink, drinking days, drinks per week, drinks per drinking day), alcohol use severity, alcohol craving, readiness for change, depression and anxiety levels. These differences were alcohol dose-dependent such that the heavier drinking group reported the highest levels on all constructs, followed by the moderate group, and the low drinking group last.
Conclusions
Baseline drinking patterns of non-treatment-seekers were generally stable and pre-visit reductions were only observed among the heavy drinking group. This generally stable pattern stands in contrast to previous reports for treatment-seeking samples. Nevertheless, the heavier drinking group, which is most similar to treatment-seekers, displayed pre-study drinking reduction. Overall, naturalistic processes of change may pose less of a threat to randomization and testing in this population.
Short Summary: The baseline drinking patterns of non-treatment-seeking problem drinkers (n = 935) were evaluated and clustered within a heavy-decreasing group (n = 255, 27.27%), a moderate-stable group (n = 353, 37.75%) and a low-stable group (n = 327, 34.97%). Baseline drinking patterns of non-treatment seekers were fairly stable, yet drinking reductions were observed in the heavy drinking group.
INTRODUCTION
Alcohol use disorder (AUD) is a highly prevalent, chronic relapsing condition (Grant et al., 2015; Koob and Volkow, 2016). AUD is characterized as a loss of control over alcohol intake, compulsive use and negative affect upon drinking cessation (Carvalho et al., 2019). Despite the prevalence of AUD and the benefits of treatment (Hasin et al., 2007), AUD is among the most undertreated health conditions (Grella and Stein, 2013; Carvalho et al., 2019). According to the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), only 7% of those with AUD receive treatment (Hasin et al., 2007). One reason for low treatment prevalence is fear of stigmatization (Carvalho et al., 2019). In addition, many individuals with AUD do not seek treatment until several years after onset of AUD (Blanco et al., 2015). Delay in treatment-seeking may be associated with greater severity, poorer health (Grella and Stein, 2013) and past history of treatment seeking (Hasin et al., 2007).
While treated individuals with AUD tend to make beneficial changes to their drinking (Grella and Stein, 2013; Meier et al., 2017), it has also been documented that a sizeable subset of individuals reduces their drinking without seeking treatment (Cutler and Fishbain, 2005; Witkiewitz et al., 2014). In fact, it is estimated that 77% of all people who resolved their alcohol-related problems did so without treatment (Sobell et al., 1996; Grella et al., 2009). Among those who do seek formal treatment, studies indicate that changes in drinking and substance use behavior may occur prior to the start of treatment (Ondersma et al., 2012; Stasiewicz et al., 2019). Perhaps as individuals become motivated to receive treatment, they also begin to alter their drinking in anticipation of the treatment process. Kaminer et al. (2008) found that 51.4% of adolescents with alcohol and other substance use disorders reported abstinence from alcohol between intake and first session. Studies with adult populations reveal similar findings (Orford et al., 2006; Kindsvatter et al., 2010; Stasiewicz et al., 2019).
Different patterns of pre-treatment change have been identified. For example, Stasiewicz et al. (2013) identified two types of changes during pre-treatment, rapid change and gradual change. Rapid change occurs during pre-treatment and is defined as a change that largely occurs between the initial phone screen and first in-person baseline assessment, which was then maintained during treatment. In contrast, gradual change involves minimal change during pre-treatment period and moderate change throughout treatment. Another study identified three classes of pre-treatment change trajectories: High Abstinence-Minimal Increase in number of days abstinent per week (HA-MI); Low Abstinence-Steady Increase in number of days abstinent per week (LA-SI) and Non-Abstinence-Accelerated Increase in number of days abstinent per week (NA-AI). The HA-MI class represents individuals who reported high levels of pre-treatment number of days abstinent (NDA) per week with a slight linear increase during 8-week pre-treatment intervals. LA-SI represents individuals who reported low pre-treatment NDA and substantial linear increase beginning 2 weeks prior to the phone screen and continuing to the first interview. The NA-AI represents individuals who reported low or no pretreatment NDA and an accelerated increase following the phone screen and leading to the first treatment session (Stasiewicz et al., 2019). Regardless of the pattern, it is clear that pre-treatment drinking changes are common.
Various mechanisms have been proposed to describe the occurrence of changes in drinking prior to treatment onset. One potential mechanism is assessment reactivity, in which participants curb drinking after completing initial alcohol-related assessments and interviews (Clifford and Davis, 2012). Assessment reactivity may occur due to the nature of the screening/intake processes of clinics and treatment studies alike, where individuals undergo assessments during the eligibility screening process and may become self-aware of their drinking level (Epstein et al., 2005; Kaminer et al., 2008). Thus, individuals may change their drinking behavior (i.e. reduce drinking) between baseline or their initial visit and their initial therapy session or research visit (Clifford and Davis, 2012; Ondersma et al., 2012). Another proposed mechanism for pre-treatment drinking reduction consists of the accumulation and worsening of external influences, such as harmful drinking consequences and family pressure to make a change (Orford et al., 2006). Similarly, pre-treatment changes due to the recognition of problem severity and need for support have been reported across therapies for other disorders, such as depression and anxiety (Kindsvatter et al., 2010). Pre-treatment change may be more common among heavy drinkers who have a ‘learning history’ related to seeking treatment (Orford et al., 2006). Individuals may have learned through past treatment that seeking treatment provides relief, which prompts them to initiate change. Additionally, pre-treatment change may be associated with lower perceived cost of alcohol use reduction, and individuals having greater confidence, commitment and motivation to abstaining (Stasiewicz et al., 2019). Altogether, these studies demonstrate that a sizeable number of individuals with AUD begin to reduce their drinking prior to treatment.
Pre-treatment drinking reduction has been associated with favorable outcomes, such as reduced drinking and increased abstinence (Orford et al., 2006; Morgenstern et al., 2007; Stasiewicz et al., 2013). Additionally, as participants who exhibit rapid change patterns experience better long-term outcomes (largely attributed to self-motivated pre-treatment change), it has also been suggested that treatment may be modified for rapid-changers in order to capitalize on these initial gains (Kindsvatter et al., 2010; Stasiewicz et al., 2013; Connors et al., 2016). A study evaluating drinking reduction prior to randomization in a pharmacotherapy clinical trial found that participants reduced drinking by 30% from intake to trial end (Penberthy et al., 2007). Pre-treatment drinking reduction was the largest contributor to reduced alcohol consumption at the completion of the trial, regardless of medication condition. Furthermore, Stasweitz and colleagues (2019) suggest that pre-treatment change should be used as part of the study and treatment design process, such that treatments can be adapted in response to pre-treatment change. Alternatively, they suggest that research studies include pre-treatment change in the randomization process for clinical trials.
As the literature on pre-treatment drinking reduction spans various treatment contexts, including pharmacotherapy trials, non-treatment-seeking individuals have also been studied. Morgenstern et al. (2007), compared treatment-seeking individuals with AUD to a group of non-help seeking (NHS) individuals comprised of eligible participants who declined treatment, but were followed (Morgenstern et al., 2007). In comparison to treatment-seeking groups, the NHS group exhibited significantly greater drinking reduction following the intake session. While both treatment-seekers and non-treatment seekers experience assessment reactivity, this study suggests that non-treatment seekers may be more reactive. It remains unknown whether non-treatment seekers reduce their drinking prior to the first assessment visit.
To advance the literature on mechanisms of behavior change in AUD, and in the context of clinical research participation, the current study examined pre-screening (i.e. pre-intake) drinking in a large sample of non-treatment seeking problem drinkers. Based on the literature, we investigated whether non-treatment seekers would engage in drinking reduction in anticipation of participation in a research study on alcohol. We examined daily drinking data for 30 days prior to first visit using a cluster analysis approach to identify drinking patterns. Once clusters were identified, we examined group differences in demographic and clinical measures, in order to elucidate the correlates of each group identified empirically for their drinking pattern. This approach examines the overall stability of drinking patterns pre-screening, with a focus on identifying pre-visit drinking reductions akin to what has been reported in the literature for treatment-seeking research participants. Characterizing such patterns is relevant to understanding behavior change and, more broadly, to clinical research in AUD.
MATERIALS AND METHODS
Participants
The current sample is culled from five separate psychopharmacology studies with similar inclusion criteria and recruitment methods, all conducted at the Addictions Laboratory at the University of California, Los Angeles. Specifically, this sample was drawn from human laboratory studies examining alcohol self-administration, acute subjective responses to alcohol, naltrexone and ibudilast as a pharmacotherapy for AUD. Although some studies involved pharmacological manipulations, all data were collected at a baseline assessment visit (i.e. prior to medication randomization or any experimental procedures). All studies recruited community samples of non-treatment-seeking problem drinkers from the greater Los Angeles area via media advertisements. These advertisements were crafted based on the specific aims of each study but generally called for individuals who drank alcohol and/or had thought about changing their drinking. It was specified that these were not treatment-related studies. All study procedures were approved by the University of California, Los Angeles Institutional Review Board, and all participants provided written informed consent upon receiving a full explanation of the study procedures.
Procedures
Interested individuals completed a phone interview for initial eligibility. Problem drinking was verified through at least one of the following methods: (a) greater than 48 drinks per month; (b) greater than 4 or 7 drinks per week for females and greater than 6 or 14 drinks per week for males; (c) an Alcohol Use Disorder Identification Test (AUDIT) score of 8 of higher (Saunders et al., 1993); (d) a score of 2 or higher on the Cutting down, Annoyance by criticism, Guilty feeling and Eye-opener questionnaire (Bush et al., 1987).
All studies had the following common exclusion criteria: (a) current involvement in treatment programs for alcohol use or have received treatment in the past 30 days; (b) use of non-prescription psychoactive drugs or use of prescription medications for recreational purposes; (c) self-reported history of bipolar disorder or psychotic disorders; (d) current use of antidepressants, mood stabilizers, sedatives, anti-anxiety medications, seizure medications or prescription painkillers; (e) self-reported history of chronic medical conditions (e.g. chronic liver disease, cardiac disease); (f) if female, pregnant (as verified by a urine sample), nursing or planning to get pregnant in the next 6 months or refusal to use a reliable method of birth control; (g) breath alcohol concentration (BrAC) of greater than 0.000 g/dl and (h) positive urine toxicology screen for any drug (other than cannabis).
Measures
Across all studies, participants deemed eligible after the telephone interview were invited to the laboratory to complete an in-person screening. The time in between the telephone screening and in-person screening varied for each participant based on individual scheduling but was no longer than 2 weeks. During the in-person screening, participants completed a phenotypic battery consisting of sociodemographic variables (i.e. age, sex) and an interview-based assessment of alcohol use over the previous 30 days, using the Timeline Followback (TLFB; Sobell and Sobell, 1992). Alcohol use measures included the AUDIT, which measures harmful and hazardous alcohol drinking (Saunders et al., 1993), the Alcohol Dependence Scale (ADS; Skinner and Horn, 1984), which evaluates AUD severity, the Obsessive Compulsive Drinking Scale (OCDS; Anton, 2000) and the Penn Alcohol Craving Scale (PACS; Flannery et al., 1999), which measure alcohol craving, the Family Tree Questionnaire, which assesses the family history of alcohol problems (FH+) (Mann et al., 1985), the Readiness to Change Ladder (RTC; Rollnick et al., 1992); and Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES; Miller and Tonigan, 1997), which evaluates motivation to reduce drinking. Additional questionnaires evaluated smoking status (Fagerström Test for Nicotine Dependence; Heatherton et al., 1991), anxiety (Beck Anxiety Inventory; BAI; Beck et al., 1988) and depressive symptomology (Beck Depression Inventory; BDI-II; Beck et al., 1996). The Structured Clinical Interview of DSM-IV or DSM-5 was administered by a master’s level clinician to determine age at first drink and assess for current AUD symptoms. To streamline the merging of data across multiple studies using both DSM-IV and DSM-5 criteria, participants who were diagnosed with alcohol dependence using DSM-IV terminology are considered to have an AUD.
Statistical analysis
Clustering methods
The goal of the cluster analysis was to identify groups based on their drinking patterns over the 30 days prior to the study visit. In order to smooth out the volatility that most subjects exhibit in their day-to-day drinking pattern, drink counts were recorded as mean drinks per day over ‘bins’ comprised of discrete 7-day periods. The 7-day period was selected because there was a significant difference in drinks per day between weekends and weekdays (Supplemental Fig. 1). This is in addition to the observed volatility in participants’ day-to-day drinking pattern. We account for both the weekend-effect, as well as the daily volatility in drinks, before clustering drinking patterns. To this end, drink counts are recorded as mean drinks per day over 7-day periods (‘bins’). It is worth noting that most participants completed the TLFB interview on different days of the week. However, by aggregating 7-day periods going back from the TLFB interview day, we have already accounted for any potential noise caused by which day of the week that the interview was conducted on. The weekend effect is also accounted for, since each 7-day period includes exactly 5 weekdays and a weekend, regardless of when the interview was conducted. We fitted a third-degree polynomial linear mixed model on mean 7-day drinks as a function of time-to-interview. The time variable ranges from 30 days prior to the interview, to a day before the interview. This linear mixed model serves as a growth curve model. The random effects from the polynomial linear mixed model seek to capture the drinking trend over time while accounting for variability among individuals. Furthermore, drink counts are evaluated on a log scale, which provides better separations among drinker groups. The justification for using a third-degree polynomial is that such a degree captures the underlying trends without including too much noise in the data. Then, we used these random effects to conduct an unsupervised K-means clustering. All analyses were conducted in R.
Group comparisons
Using the clusters identified by employing the procedures described above, Analyses of Covariance (ANCOVAs) were conducted as omnibus tests comparing the drinking groups/clusters on continuous demographic and clinical measures. Cochran–Mantel–Haenszel (CMH) tests were used to compare drinking groups/clusters on categorical measures. CMH tests are an extension of chi-square tests and allow for comparison of categorical variables while controlling for covariates. All analyses controlled for the effects of study source (i.e. the original study from which data were culled). P-value correction was implemented to reduce the risk of Type I error. Since demographic and clinical variables were the two categories in which the groups were compared, the P-value of 0.05 was divided by 2, resulting in a corrected critical P-value for the omnibus tests of P < 0.025. Tukey–Kramer t-tests were used to follow-up significant omnibus ANCOVAs. These post hoc tests are commonly used in psychological research as they allow for pairwise comparisons between group means while conservatively controlling the Type 1 experiment-wise error rate (Maxwell and Delaney, 2004). Specifically, Tukey tests compute a single value that determines the minimum difference between means that is necessary for significance. This value is called the honestly significant difference (HSD), and mean differences that exceed Tukey’s HSD are considered significantly different. Group comparison analyses were conducted in SAS 9.4 using PROC FREQ (CMH tests) or PROC GLM (ANCOVAs).
RESULTS
Drinking clusters
A total of 935 participants were included in the analyses since the TLFB interview data were complete for all participants. By extracting the random effects, and submitting them to a cluster analysis, we were able to identify three alcohol use trajectories prior to the screening visit. The resulting three clusters group subjects into three visually distinct drinking patterns. The first cluster was characterized by a heavy and decreasing drinking pattern (n = 255, 27.27% of total sample), the second cluster was defined by a moderate and stable drinking pattern (n = 353, 37.75% of total sample) and the third cluster showed a low and stable drinking pattern (n = 327, 34.97% of total sample). Figure 1A depicts all the individual observations across the time-bins with drinks per day on a 7-day period. Figure 1B displays the three clusters in times-bins with drinks per day on a 7-day period.
Fig. 1 .
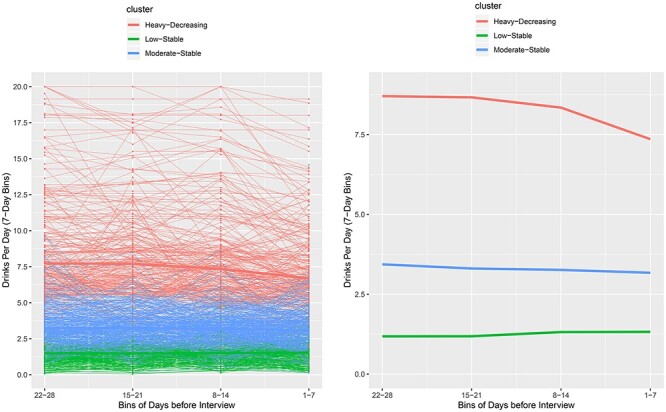
Drinking pattern clusters.
(A) All the individual observations across the time-bins with drinks per day on a 7-day period. (B) The three clusters in time-bins with drinks per day on a 7-day period.
To test the reliability of the clustering method, we used a robustness measure. To do so, we first varied the parameters of the model within a reasonable grid of numbers. For example, in the first step of the clustering, we fit both a quadratic form linear mixed regression and a regular linear mixed regression, and for each regression, we specified different number of neighborhoods used for k-means clustering, from 2 to 6 neighborhoods. We can then calculate a pairwise robustness, which is defined as the proportion of number of times that some pair of subjects is grouped in the same cluster, out of all 10 runs (Lu et al., 2019). We then evaluated an averaged robustness, given the drinking group assignments that we have specified for this study. For each of the 3 drinking groups that we have assigned, we calculated an average robustness among all pairs within that group (conditional robustness). In other words, we evaluated how often the subjects specified by our final assignments also get clustered in other models with different tuning parameters. We found that the robustness for cluster 1 high-decreasing was 0.742, robustness for cluster 2 moderate-stable was 0.637 and robustness for cluster 3 low-stable is 0.708. These robustness results are in the range of what is considered a ‘stable cluster’, when compared with other stable clustering algorithms (Lu et al., 2019). These steps support the clustering approach, which allowed us to identify three distinct alcohol use patterns prior to the screening visit.
Clinical characteristics distinguishing drinking clusters
To advance our understanding of the demographic and clinical characteristics that distinguish the observed three groups, we compared those using CMH tests for categorical variables and ANCOVAs for continuous variables (all analyses controlling for study source). These omnibus tests were followed by planned post hoc comparisons. As shown in Table 1, the groups differed significantly on a host of measures including pre-visit drinking (age at first drink, drinking days, drinks per week, drinks per drinking day), alcohol use severity (AUDIT and ADS scores), alcohol craving (PACS and OCDS scores), and depression (BDI) and anxiety (BAI) levels. In regard to the measures of motivation to change their drinking, the groups differed on SOCRATES, but not RTC.
Table 1.
Comparisons among drinking profiles on demographic and clinical characteristics while controlling for study source
| Means (SD) or N (%) | ||||||
|---|---|---|---|---|---|---|
| Heavy-decreasing (n = 255; 27.27%) | Moderate-stable (n = 353; 37.75%) | Low-stable (n = 327; 34.97%) | Statistic | P | Effect size | |
| Age | 34.35  9.80 9.80 |
33.26  9.88 9.88 |
30.00  9.29 9.29 |
F = 0.47 | 0.625 |
 = 0.001
= 0.001 |
| Sex (Male) a–c | 209 (81.96%) | 244 (69.12%) | 176 (53.82%) | CMH = 42.81 | <0.001 | - |
| Income | CMH = 11.71 | 0.798 | - | |||
| $0—$14 999 | 96 (38.10%) | 108 (31.03%) | 87 (26.69%) | |||
| $15 000—$29 999 | 64 (25.40%) | 92 (26.44%) | 74 (22.70%) | |||
| $30 000—$44 999 | 34 (13.49%) | 50 (14.37%) | 43 (13.19%) | |||
| $45 000—$59 999 | 25 (9.92%) | 31 (8.91%) | 32 (9.82%) | |||
| $60 000—$74 999 | 14 (5.56%) | 22 (6.32%) | 19 (5.83%) | |||
| $75 000—$89 999 | 5 (1.98%) | 12 (3.45%) | 23 (7.06%) | |||
| $90 000—$104 999 | 4 (1.59%) | 8 (2.30%) | 15 (4.60%) | |||
| $105 000—$119 999 | 2 (0.79%) | 9 (2.59%) | 8 (2.45%) | |||
| $120 000+ | 8 (3.17%) | 16 (4.60%) | 25 (7.67%) | |||
| Cigarette smoker a–c | 224 (88.89%) | 250 (71.84%) | 169 (51.68%) | CMH = 26.95 | <0.001 | - |
| BDI-II a–c |
13.15  10.76 10.76
|
9.53  8.39 8.39
|
7.46  7.32 7.32
|
F = 24.99 | <0.001 |
 = 0.05
= 0.05
|
| BAI a–c |
8.95  9.12; n = 238 9.12; n = 238
|
7.23  7.53; n = 313 7.53; n = 313
|
4.97  5.50; n = 177 5.50; n = 177
|
F = 12.48 | <0.001 |
 = 0.03
= 0.03
|
| FH+ a,b | 137 (60.62%) | 144 (45.43%) | 101 (41.06%) | CMH = 13.47 | 0.001 | - |
| Age at first drink b |
14.91  3.04; n = 78 3.04; n = 78
|
15.70  3.84; n = 158 3.84; n = 158
|
16.72  2.85; n = 229 2.85; n = 229
|
F = 6.56 | 0.002 |
 = 0.03
= 0.03
|
| AUD Diagnosis a–c | 47 (54.02%); n = 87 | 42 (23.86%); n = 176 | 15 (6.22%); n = 241 | CMH = 73.57 | <0.001 | - |
| Drinking days a–c |
25.57  4.71 4.71
|
19.33  6.66 6.66
|
10.81  5.39 5.39
|
F = 332.73 | <0.001 |
 = 0.42
= 0.42
|
| Drinks per week a–c |
57.37  23.46 23.46
|
22.55  5.92 5.92
|
8.58  3.46 3.46
|
F = 852.88 | <0.001 |
 = 0.65
= 0.65
|
| Drinks per drinking day a–c |
9.69  3.43 3.43
|
5.56  2.30 2.30
|
3.81  1.86 1.86
|
F = 339.69 | <0.001 |
 = 0.42
= 0.42
|
| ADS a – c |
16.83  7.72 7.72
|
12.95  6.81 6.81
|
9.49  5.28 5.28
|
F = 74.86 | <0.001 |
 = 0.14
= 0.14
|
| AUDIT a–c |
23.64  6.63; n = 78 6.63; n = 78
|
16.63  6.33; n = 159 6.33; n = 159
|
11.35  4.68; n = 230 4.68; n = 230
|
F = 113.83 | <0.001 |
 = 0.33
= 0.33
|
| OCDS a–c |
16.69  8.03; n = 186 8.03; n = 186
|
11.90  6.37; n = 223 6.37; n = 223
|
7.22  4.95; n = 243 4.95; n = 243
|
F = 71.09 | <0.001 |
 = 0.18
= 0.18
|
| PACS a–c |
15.48  7.18 7.18
|
11.38  6.22 6.22
|
6.91  4.60 4.60
|
F = 90.17 | <0.001 |
 = 0.16
= 0.16
|
| RTC ladder | 4.39  2.80; n = 87 2.80; n = 87 |
4.40  3.20; n = 171 3.20; n = 171 |
3.48  3.50; n = 237 3.50; n = 237 |
F = 1.38 | 0.254 |
 = 0.006
= 0.006 |
| SOCRATES-recognition a–c |
21.77  7.52; n = 70 7.52; n = 70
|
17.95  6.92; n = 111 6.92; n = 111
|
12.89  5.65; n = 188 5.65; n = 188
|
F = 23.61 | <0.001 |
 = 0.11
= 0.11
|
| SOCRATES-ambivalence b ,c |
13.17  4.20; n = 70 4.20; n = 70
|
11.90  3.76; n = 111 3.76; n = 111
|
9.05  3.72; n = 188 3.72; n = 188
|
F = 15.76 | <0.001 |
 = 0.08
= 0.08
|
| SOCRATES-taking steps | 20.71  7.24; n = 70 7.24; n = 70 |
21.98  7.46; n = 111 7.46; n = 111 |
19.14  7.74; n = 188 7.74; n = 188 |
F = 1.65 | 0.194 |
 = 0.009
= 0.009 |
aHeavy-Decreasing and Moderate-Stable groups differ, P < 0.05.
bHeavy-Decreasing and Low-Stable groups differ, P < 0.05.
cModerate-Stable and Low-Stable groups differ, P < 0.05.
Bold type indicates significant differences between clusters on omnibus test (P < 0.025). Sample sizes for individual measures for each group are provided in the row associated with that measure.
Tukey post hoc tests indicated that the heavy-decreasing group had greater depression (P’s < 0.001) and anxiety levels (P’s < 0.05), greater pre-visit drinking (P’s < 0.001), greater alcohol craving (P’s < 0.001) and higher SOCRATES recognition scores (P’s < 0.001) compared with the other groups. The heavy-decreasing group also had a younger age at first drink (P = 0.001) and higher SOCRATES ambivalence scores (P < 0.001) relative to the low-stable group. Compared with the moderate-stable group, the low-stable group had lower depression (P = 0.011) and anxiety levels (P = 0.006), lower pre-visit drinking (P’s < 0.001), lower alcohol use severity (P’s < 0.001), lower alcohol craving (P’s < 0.001), and lower SOCRATES recognition (P < 0.001) and ambivalence scores (P < 0.001).
DISCUSSION
This study examined whether a large sample of non-treatment-seeking problem drinkers would engage in drinking reduction in anticipation of participation in an alcohol research study, using daily drinking data for the 30-days prior to the screening visit. A cluster analysis identified three distinct drinking patterns, labeled (a) heavy-decreasing drinking, (b) moderate-stable drinking and (c) low-stable drinking. While a decrease in drinking prior to study participation was observed, this was only observed in the heavy-decreasing cluster (n = 255, 27.27%) with the majority of study participants classified as stable drinkers, either moderate-stable or low-stable.
Germane to the clustering procedures based on drinking data, and providing a proof-of-concept of the clustering itself, group differences in demographic and clinical measures revealed the three groups differed on measures of prior-to-visit drinking behavior, alcohol use severity and alcohol craving. The three clusters differed significantly on a host of measures including pre-visit drinking (age at first drink, drinking days, drinks per week, drinks per drinking day), alcohol use severity, alcohol craving, readiness for change, depression and anxiety levels. These differences were alcohol-dose dependent such that the heaviest-drinking group reported the highest levels on all constructs, followed by the moderate group, and the low-drinking group last. Inspection of the clusters and their relationship to the demographic, alcohol use, motivation for change and clinical measures suggest a linear effect of alcohol consumption and largely support the clustering approach. In other words, the three clusters were distinct in linear and dose–response fashion from each other based on the heaviness of drinking. Given these robust cluster-based findings, the fact that only the heaviest drinking group showed decreases in drinking prior to the visit provides unique insights into the nature of drinking reduction in this sample.
The identification of a cluster of individuals who display a drinking reduction prior to initial study visit align in part with past research on pre-treatment drinking reduction in treatment-seeking populations (Penberthy et al., 2007; Kaminer et al., 2008; Stasiewicz et al., 2013). However, the fact that majority of the sample were comprised of stable drinkers suggests that drinking patterns are less likely to change in anticipation of a research study visit among non-treatment seeking problem drinkers, as compared with what has been documented in treatment-seeking samples. Various state and trait factors might contribute to the differential stability drinking patterns among non-treatment and treatment-seeking populations. For instance, Orford et al. (2006) argued that pre-treatment changes in treatment seeking individuals are due to recognizing the accumulation and worsening of problems in multiple life aspects due to drinking. Penberthy et al. (2007) found that higher levels of readiness to change in heavy drinking individuals seeking treatment were a predictor of significant reductions to drinking prior to treatment. In support, the current study found that motivation to change, indexed by the SOCRATES, but not RTC, was sensitive to group differences with the heavy-decreasing group reporting greater problem recognition than the moderate-stable and low-stable groups. These motivational differences between treatment seeking and non-treatment seeking individuals may contribute to the stability in pre-treatment/pre-study drinking patterns. Specifically, only the heaviest drinking cluster in this non-treatment seeking sample showed some motivation for change that may approximate what is reported in treatment seeking samples.
A putative mechanism for pre-treatment changes in drinking is assessment reactivity (Epstein et al., 2005; Morgenstern et al., 2007; Kaminer et al., 2008). The notion maintains that the assessment process increases the awareness of one’s drinking, thus leading to self-initiated drinking reductions. In support of this idea, Morgenstern et al. (2007) found that an NHS group showed sharp drinking reductions which they attributed to assessment reactivity. Although our two moderate drinking clusters showed variability in drinking patterns prior to the initial visit, the majority of participants had a generally stable drinking pattern. This is consistent with the fact that no formal assessment took place to trigger reactivity, although the initial telephone interview is arguably a brief assessment. This is also consistent with Stasiewicz et al. (2013) who argued that assessment reactivity could not explain the entirety of drinking change observed in their study and that instead motivational and change processes may be at play. While the Morgenstern et al.’s (2007) sample was entirely comprised of individuals with AUD, in contrast to the present sample, we argue that alcohol use problems clearly manifest themselves in a continuum and that non-treatment seekers with and without AUD may be sensitive to assessment reactivity and underlying motivation to reduce their drinking. This is largely consistent with the longstanding literature on naturalistic recovery, with and without an AUD diagnosis (Tucker et al., 1994; Tucker et al., 2002a, 2002b).
Notably, this study has several strengths and limitation. Strengths include the large sample size of non-treatment seeking problem drinkers culled from a host of behavioral pharmacology studies. The use of advanced data modeling methods, such as cluster analysis, is represented as a strength. Study limitations include the relatively young age of study participants, the lack of precision about when participants completed the telephone interview, the potential impact of study advertisement language on drinking reductions, as well as the inherent individual-level volatility in day-to-day drinking pattern over the 30-day period. In addition, our approach to comparing the three clusters assumes that our classification of individuals into clusters was error-free, which is a limitation of this approach.
In sum, the present findings add to the literature on non-treatment seeking samples by suggesting that their drinking patterns may be more stable than what has been reported for treatment-seekers. However, drinking reductions were observed in the heavy drinking group. This is notable as the heavy drinking group most closely resembles a treatment-seeking sample. Previous studies have suggested that pre-treatment drinking reductions pose a risk to clinical research whereby one may misattribute drinking reduction to experimental treatments, rather than an underlying naturalistic process of change (Kaminer et al., 2008; Stasiewicz et al., 2013). The relative stability of drinking patterns in non-treatment seekers suggests that naturalistic processes of change and assessment reactivity may pose less of a threat to randomization and testing procedures than has been previously documented among treatment-seekers. Nevertheless, among the heaviest drinking subset of non-treatment seekers in this large sample, drinking reductions were in fact documented. This suggests that very heavy drinking patterns may be a common feature in pre-study drinking reductions across both treatment-seekers and non-treatment seekers for AUD.
Supplementary Material
ACKNOWLEDGEMENT
Support for data analysis and manuscript preparation provided by from the National Institute on Alcohol Abuse and Alcoholism K24AA025704, awarded to Lara Ray.
Contributor Information
Wave-Ananda Baskerville, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA.
Steven J Nieto, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA.
Diana Ho, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA.
Brandon Towns, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA.
Erica N Grodin, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA.
Caesar Li, Department of Biostatistics, University of California, Los Angeles, Los Angeles, CA, USA.
Elizabeth Burnette, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA; Brain Research Institute, University of California, Los Angeles, Los Angeles, CA, USA.
Suzanna Donato, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA.
Lara A Ray, Department of Psychology, University of California, Los Angeles, Los Angeles, CA, USA; Brain Research Institute, University of California, Los Angeles, Los Angeles, CA, USA; Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, Los Angeles, CA, USA.
DATA AVAILABILITY STATEMENT
The data underlying this article will be shared on reasonable request to the corresponding author.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
References
- Anton RF (2000) Obsessive–compulsive aspects of craving: development of the obsessive compulsive drinking scale. Addiction 95:211–7. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G et al. (1988) An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 56:893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK (1996) Manual for the Beck Depression Inventory-II, Vol. 1. San Antonio, TX: Psychological Corporation, 82. [Google Scholar]
- Blanco C, Iza M, Rodríguez-Fernández JM et al. (2015) Probability and predictors of treatment-seeking for substance use disorders in the US. Drug Alcohol Depend 149:136–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush B, Shaw S, Cleary P et al. (1987) Screening for alcohol abuse using the CAGE questionnaire. Am J Med 82:231–5. [DOI] [PubMed] [Google Scholar]
- Carvalho AF, Heilig M, Perez A et al. (2019) Alcohol use disorders. Lancet 394:781–92. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Davis CM (2012) Alcohol treatment research assessment exposure: a critical review of the literature. Psychol Addict Behav 26:773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connors GJ, Maisto SA, Schlauch RC et al. (2016) Therapeutic alliances predict session by session drinking behavior in the treatment of alcohol use disorders. J Consult Clin Psychol 84:972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler RB, Fishbain DA (2005) Are alcoholism treatments effective? The Project MATCH data BMC Public Health 5:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein EE, Drapkin ML, Yusko DA et al. (2005) Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol-dependent women. J Stud Alcohol 66:369–78. [DOI] [PubMed] [Google Scholar]
- Flannery B, Volpicelli J, Pettinati H (1999) Psychometric properties of the Penn alcohol craving scale. Alcohol Clin Exp Res 23:1289–95. [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD et al. (2015) Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on alcohol and related conditions III. JAMA Psychiat 72:757–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US et al. (2009) Perceptions of need and help received for substance dependence in a national probability survey. Psychiatr Serv 60:1068–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Stein JA (2013) Remission from substance dependence: differences between individuals in a general population longitudinal survey who do and do not seek help. Drug Alcohol Depend 133:146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E et al. (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiatry 64:830–42. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC et al. (1991) The Fagerström test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict 86:1119–27. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH (2008) Can assessment reactivity predict treatment outcome among adolescents with alcohol and other substance use disorders? Subst Abus 29:63–9. [DOI] [PubMed] [Google Scholar]
- Kindsvatter A, Osborn CJ, Bubenzer D et al. (2010) Client perceptions of pretreatment change. J Couns Dev 88:449–56. [Google Scholar]
- Koob GF, Volkow ND (2016) Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry 3:760–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, Y., Phillips, C. A., & Langston, M. A. (2019). A robustness metric for biological data clustering algorithms. BMC bioinformatics, 20(15), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann RE, Sobell LC, Sobell MB et al. (1985) Reliability of a family tree questionnaire for assessing family history of alcohol problems. Drug Alcohol Depend 15:61–7. [DOI] [PubMed] [Google Scholar]
- Maxwell, S. E., Delaney, H. D., & Kelley, K. (2018). Designing Experiments and Analyzing Data: A Model Comparison Perspective (3rd ed.). New York: Routledge. [Google Scholar]
- Meier E, Miller MB, Lombardi N et al. (2017) Assessment reactivity: a randomized controlled trial of alcohol-specific measures on alcohol-related behaviors. Addict Behav 67:44–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS (1997) Assessing drinkers' motivation for change: the Stages of Change Readiness and Treatment Eagerness Scale SOCRATES. American Psychological Association. [Google Scholar]
- Morgenstern J, Irwin TW, Wainberg ML et al. (2007) A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. J Consult Clin Psychol 75:72. [DOI] [PubMed] [Google Scholar]
- Ondersma SJ, Winhusen T, Lewis DF (2012) Pre-treatment change in a randomized trial with pregnant substance-abusing women in community-based outpatient treatment. Contemp Clin Trials 33:1074–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orford J, Kerr C, Copello A et al. (2006) Why people enter treatment for alcohol problems: findings from UK alcohol treatment trial pre-treatment interviews. J Subst Abus 11:161–76. [Google Scholar]
- Penberthy JK, Ait-Daoud N, Breton M et al. (2007) Evaluating readiness and treatment seeking effects in a pharmacotherapy trial for alcohol dependence. Alcohol Clin Exp Res 31:1538–44. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R et al. (1992) Development of a short ‘readiness to change’questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br J Addict 87:743–54. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF et al. (1993) Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 88:791–804. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Horn JL (1984) Alcohol dependence scale (ADS). In User's guide. Addiction Research Foundation. [Google Scholar]
- Sobell LC, Cunningham JA, Sobell MB (1996) Recovery from alcohol problems with and without treatment: Prevalence in two population surveys. Am J Public Health 86:966–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline follow-back. In Measuring Alcohol Consumption. Humana Press, Totowa, NJ., 41–72. [Google Scholar]
- Stasiewicz PR, Bradizza CM, Ruszczyk MU et al. (2019) The identification of pretreatment trajectories of alcohol use and their relationship to treatment outcome in men and women with alcohol use disorder. Alcohol Clin Exp Res 43:2637–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasiewicz PR, Schlauch RC, Bradizza CM et al. (2013) Pretreatment changes in drinking: Relationship to treatment outcomes. Psychol Addict Behav 27:1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Gladsjo JA (1994) Environmental events surrounding natural recovery from alcohol-related problems. Addictions Nursing 6:117–28. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Rippens PD (2002a) Environmental contexts surrounding resolution of drinking problems among problem drinkers with different help-seeking experiences. J Stud Alcohol 63:334–41. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Vuchinich RE, Rippens PD (2002b) Predicting natural resolution of alcohol-related problems: A prospective behavioral economic analysis. Exp Clin Psychopharmacol 10:248. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Dearing RL, Maisto SA (2014) Alcohol use trajectories among non–treatment-seeking heavy drinkers. J Stud Alcohol Drugs 75:415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


