Abstract
Improving antibiotic prescribing in outpatient settings is a public health priority. In the United States, urgent care (UC) encounters are increasing and have high rates of inappropriate antibiotic prescribing. Our objective was to characterize antibiotic prescribing practices during UC encounters, with a focus on respiratory tract conditions. This was a retrospective cohort study of UC encounters in the Intermountain Healthcare network. Among 1.16 million UC encounters, antibiotics were prescribed during 34% of UC encounters and respiratory conditions accounted for 61% of all antibiotics prescribed. Of respiratory encounters, 50% resulted in antibiotic prescriptions, yet the variability at the level of the provider ranged from 3% to 94%. Similar variability between providers was observed for respiratory conditions where antibiotics were not indicated and in first-line antibiotic selection for sinusitis, otitis media, and pharyngitis. These findings support the importance of developing antibiotic stewardship interventions specifically targeting UC settings.
Keywords: antibiotic stewardship, urgent care, telemedicine, pediatric urgent care
We describe antibiotic prescribing in a large network of urgent care (UC) clinics. The high volume of infectious diseases encounters and extreme provider variability in antibiotic prescribing frequency and quality highlight the importance of antibiotic stewardship interventions specifically targeting UCs.
Most human antibiotic use occurs in outpatient settings [1, 2]. At least 30% of these prescriptions are thought to be unnecessary [3], and contribute to avoidable harms and costs. These consequences include antibiotic-resistant infections, Clostridioides difficile infections [4], and adverse drug effects [5]. As such, improving antibiotic prescribing in outpatient settings is a public health priority, and a growing body of evidence exists about effective outpatient stewardship interventions [6–11].
The United States is experiencing a rapid change in health-care delivery, with a dramatic increase in outpatient encounters in nontraditional health-care settings, including urgent care (UC) clinics, retail clinics, and telemedicine [12, 13]. Compared to emergency departments, these settings may have certain advantages, including expanded hours, walk-in appointments, lower costs, and shortened wait times. These settings are well suited to care for patients with uncomplicated, low-acuity conditions (eg, acute respiratory conditions), to meet patient expectations for rapid and convenient care, and to lower the burden of acute care encounters in primary care clinics. Similar to national trends, UC and telemedicine encounters in the Intermountain Healthcare (IH) system have been increasing over the past 10 years [14].
Despite these secular trends, most stewardship interventions have focused on primary care settings and not UCs [6–11]. Compared to primary care settings, UCs have unique features, including high volumes with rapid patient turnarounds; limited communication with primary care providers; rotating UC providers, which limits the cohesiveness of a clinic team; and potentially different patient expectations. These factors may require adaptations from the design of stewardship interventions developed for primary care. A recent study indicated that across all health-care settings, in aggregate, UCs have both the highest percentage of visits resulting in antibiotic prescriptions and the highest rate of inappropriate prescribing for respiratory tract infections, making UCs a high-priority target for stewardship interventions [15].
Our objective was to characterize antibiotic prescribing practices during UC encounters within a large, integrated health-care system, with a focus on prescribing for respiratory tract infections overall and appropriate use across specific conditions. Secondary objectives were to characterize clinic and provider-level variations in prescribing practices and patient satisfaction. This work will provide insight into the appropriate targets and designs for stewardship interventions tailored for UC.
METHODS
Study Design and Setting
This was a retrospective, cohort study of UC encounters in the IH system from 1 August 2017 through 29 June 2019 (23 months). IH is a nonprofit, vertically integrated health-care delivery system that includes 24 hospitals, >185 outpatient clinics, >1500 clinicians, and a health insurance plan with over 850 000 covered lives throughout Utah and Idaho. IH operates 38 UC clinics, which include 32 clinics providing care for patients of all ages (InstaCare) and 6 providing care exclusively to children <18 years old (KidsCare). InstaCare and KidsCare clinics are predominantly staffed by physicians; KidsCare is exclusively staffed by pediatricians. In addition, IH operates a telemedicine UC clinic (Connect Care) where patients access clinicians for the treatment of low-acuity conditions via electronic devices, primarily staffed by advanced practice providers (APPs). IH’s institutional review board approved this retrospective study with a waiver of informed consent.
Data Collection
Medical training information (for physicians [MD or DO degree holders] or APPs) for all UC clinicians was obtained via IH’s human resources database. Patient demographics, obtained for each UC encounter, included age, sex, and race. Demographic data, diagnoses assigned, and antibiotic prescriptions were extracted electronically from the system-wide electronic health record.
Classification of Urgent Care Encounters
To characterize the distribution of diagnoses and antibiotic prescribing for UC encounters, all International Classification of Diseases, 10thRevision, Clinical Modification (ICD10) codes were obtained for each UC encounter. The top 1000 most commonly used ICD10 codes during UC encounters were then categorized into mutually exclusive clinical categories. An additional 401 related codes were also added for completeness. These related codes were part of relevant ICD10 code categories (eg, J01 Acute Sinusitis) but were not identified in the top 1000 ICD10 codes (eg, J01.40 acute unspecified pansinusitis). The clinical categories included skin and skin structure (skin); gastroenterology; genitourinary (GU); respiratory/inner ear (respiratory); and other. Each ICD10 code within each category was further subcategorized and assigned into tiered groups, based on whether antibiotics would be indicated, using a previously developed system: Tier 1 codes are those where antibiotics are almost always indicated (eg, pneumonia, urinary tract infection, group A streptococcal pharyngitis), Tier 2 codes are those where antibiotics may be indicated (eg, sinusitis, acute otitis media [AOM], cutaneous abscess), and Tier 3 codes are those where antibiotics are not indicated (eg, bronchitis, nausea) [3]. The 1401 ICD10 codes collectively account for over 97% of all ICD10 codes used in UC (Supplementary Appendix). When 2 or more ICD10 codes within the same clinical category were assigned for the same encounter, the diagnosis was based on the code with the lowest tier (eg, Tier 1). If multiple codes from the same tier were present, the diagnosis was based on the first listed ICD10 code. We excluded visits with ICD10 codes from 2 or more clinical categories (eg, respiratory and skin). In addition, we excluded encounters where the provider was unknown or encounters with those providers who had <25 encounters during the study period.
Antibiotic Prescriptions
Up to 2 antibiotic prescriptions generated or administered during UC encounters were captured as electronic orders. Our focus was on systemic (oral or parenteral) antibiotic prescriptions; therefore, topical and inhaled antibiotic formulations were excluded.
Patient Satisfaction
To assess patient satisfaction, we analyzed data from IH’s routinely collected patient satisfaction survey. Patient satisfaction scores were available through 31 December 2017. All IH UC patients received an automated patient satisfaction survey after their UC encounter. The Consumer Assessment of Healthcare Providers and Systems’ Clinician & Group Survey assesses patients’ experiences with health-care providers and staff in the UC office [16]. The survey includes a question asking the patient to rate their provider on a scale from 0 to 10 (with 0 being the “worst provider possible” and 10 being the “best provider possible”).
Outcomes
For all UC encounters, we determined the distribution by clinical categories, the distribution by tiers, and the percentages of encounters where antibiotics were prescribed overall and within each clinical category. The primary study outcomes were the percentages of respiratory encounters with an antibiotic prescription at the clinic and provider levels. Secondary outcomes included the percentage of encounters with a Tier 3 respiratory diagnosis with an antibiotic prescription (ideal percentage of 0%) and the frequency of use of first-line recommended antibiotics for selected respiratory conditions (higher is better) during encounters where an antibiotic was prescribed. The conditions of interest were AOM, sinusitis, and pharyngitis (streptococcal and unspecified). We defined first-line antibiotics as penicillin or amoxicillin for pharyngitis and amoxicillin or amoxicillin/clavulanate for acute sinusitis and AOM, based on local and national guidelines. For each outcome, we determined the aggregate percentage during the study period, as well as the variation by individual clinics and providers. For the analysis of patient satisfaction scores, we compared the mean scores for Tier 2 and Tier 3 respiratory encounters between those where antibiotics were and were not prescribed.
Statistical Analysis
Descriptive statistics reported central tendencies as medians and interquartile intervals (IQI) for metric variables and as proportions and sizes for categorical variables. Inferential analyses used multivariable regression analyses with outcome-appropriate distribution families and link functions. Variance decomposition was measured as the intraclass correlation coefficient (ICC) from a 3-level hierarchical logistic model that accounted for the encounter, provider, and clinic. Comparisons between settings were conducted as separate multivariate logistic regression analyses, using InstaCare as the reference category. Bootstrapped 95% confidence intervals (CIs) were derived for the comparison of mean patient satisfaction scores. Statistical analyses were conducted in R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Overall Urgent Care Encounters
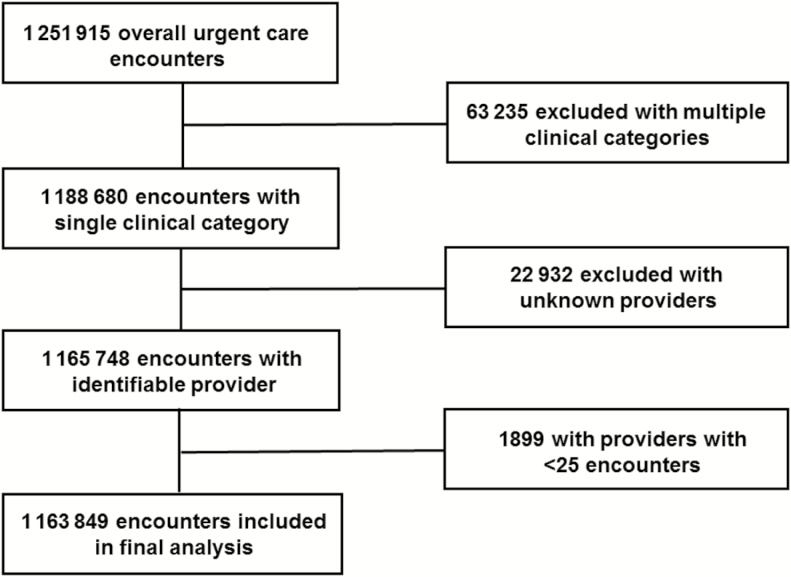
During the 23-month period, there were a total of 1 251 915 UC encounters. We excluded 63 235 (5.1%) encounters with diagnoses from multiple clinical categories, 22 932 (1.8%) with unknown providers, and 1899 (0.2%) with providers that had <25 encounters during the study period, yielding 1 163 849 UC encounters for the final analysis (Figure 1). Of these, 1 043 040 (89.6%) encounters were in InstaCare, 83 356 (7.2%) in KidsCare, and 37 453 (3.2%) in Connect Care. There were 888 providers identified during the study period, 396 of whom had at least 25 encounters. Of these, there were 292 physicians (73.7%), 66 APPs (16.7%), and 38 (9.6%) providers without medical training information available.
Figure 1.
Flow chart illustrating criteria used to exclude selected urgent care encounters to derive final study data set.
Patient Demographics
The median age of patients seeking care in UC was 30 years (IQI, 15–48) and ages varied by setting. The median age of KidsCare patients was 6 years (IQI, 2–11; Table 1). Most InstaCare and Connect Care encounters were for patients between the ages of 1 and 65 (accounting for 87.8% and 97.0% of encounters, respectively).
Table 1.
Patient Demographics and Clinical Distribution of Intermountain’s Urgent Care Encounters
| Total | InstaCare | Connect Care | KidsCare | |
|---|---|---|---|---|
| N = 1 163 849 | n = 1 043 040 | n = 37 453 | n = 83 356 | |
| Encounter-level patient demographics | ||||
| White | 83.6% (n = 973 289) | 84.3% (n = 878 835) | 83.4% (n = 31 221) | 75.9% (n = 63 233) |
| Female | 56.7% (n = 659 663) | 57% (n = 594 868) | 64.2% (n = 24 030) | 48.9% (n = 40 765) |
| Patient age, median | 30 (IQI 15-48)a | 32 (IQI 19-50) | 33 (IQI 19-43) | 6 (IQI 2-11) |
| Physician provider | 90% (n = 104 451)a | 92.5% (n = 961 057) | 0.5% (n = 205) | 100% (n = 83 189) |
| Advanced practice provider | 10% (n = 115 542)a | 7.5% (n = 78 294) | 99.5% (n = 37 248) | 0% (n = 0) |
| Encounter-level clinical categories | ||||
| Respiratory | 41.8% (n = 486 061) | 40.8% (n = 426 070) | 47% (n = 17 621) | 50.8% (n = 42 370) |
| Skin | 13.7% (n = 159 009) | 13.8% (n = 143 831) | 12.4% (n = 4635) | 12.6% (n = 10 543) |
| GU | 8.1% (n = 93 855) | 8.4% (n = 87 149) | 12.1% (n = 4541) | 2.6% (n = 2165) |
| GI | 6.3% (n = 73 823) | 6.4% (n = 66 665) | 5.7% (n = 2132) | 6% (n = 5026) |
| Other | 25.3% (n = 294 261) | 25.8% (n = 269 250) | 18.3% (n = 6862) | 21.8% (n = 18 149) |
| Unclassified | 4.9% (n = 56 840) | 4.8% (n = 50 075) | 4.4% (n = 1662) | 6.1% (n = 5103) |
| Tier 1 | 11.9% (n = 135 113) | 12.3% (n = 125 018) | 8.7% (n = 3229) | 8.6% (n = 6866) |
| Tier 2 | 30.1% (n = 341 050) | 29.7% (n = 302 337) | 33.1% (n = 12 271) | 33% (n = 26 442) |
| Tier 3 | 55.6% (n = 630 846) | 55.6% (n = 565 610) | 54.7% (n = 20 291) | 56.1% (n = 44 945) |
| Encounter-level antibiotic prescribing rate | ||||
| Total antibiotic prescribing rate | 34.1% (n = 396 825) | 34.9% (n = 364 097) | 32.6% (n = 12 208) | 24.6% (n = 20 520) |
In Tier 1, antibiotics were almost always indicated (eg, pneumonia); in Tier 2, antibiotics may have been indicated (eg, sinusitis); and in Tier 3, antibiotics were not indicated (eg, bronchitis). Abbreviations: GI, gastroenterology; GU, genitourinary; IQI, interquartile interval.
a4 encounters were missing patient age data and 3856 encounters were missing provider specialty data.
Urgent Care Visit Diagnoses and Overall Antibiotic Prescribing
The most common clinical category for UC encounters was respiratory encounters (41.8%), with skin and GU encounters representing 13.7% and 8.1%, respectively (Table 1). Across all clinical categories, 40.9% of UC visits included a Tier 1 or Tier 2 diagnosis, representing conditions where antibiotics are potentially warranted (42.0% in InstaCare, 41.8% in Connect Care, and 41.6% in KidsCare). Overall, 34.1% (n = 396 825) of UC visits included an antibiotic prescription order or an administered antibiotic (34.9% in InstaCare, 32.6% in Connect Care, and 24.6% in KidsCare; Table 1). The most commonly prescribed antibiotics were amoxicillin (27.9%), cephalexin (11.0%), and doxycycline (9.8%; Table S1 in Supplementary Appendix). Parenteral antibiotics were prescribed in 5.3% of encounters where an antibiotic was prescribed (83% ceftriaxone). Among UC visits where an antibiotic was prescribed, 61.1% (n = 242 651) were categorized as respiratory, 18.0% (n = 71 455) were GU, 13.9% (n = 55 079) were skin, 3.0% (n = 11 937) were other, 2.3% (n = 9312) were gastroenterology, and 1.6% (n = 6391) were unclassified encounters.
Antibiotic Prescribing in Respiratory Encounters
Among all respiratory encounters, 44 727 (9.2%) were Tier 1, 242 343 (49.9%) were Tier 2, and 189 991 (40.9%) were Tier 3 (Table 2). Antibiotics were prescribed for 96.6% of Tier 1, 64.8% of Tier 2, and 21.3% of Tier 3 encounters. Of all respiratory antibiotic prescriptions, 64.7% were for Tier 2 conditions and 17.5% were for Tier 3 conditions (Table 2). The most commonly prescribed antibiotics were amoxicillin (44.6%), doxycycline (14.0%), and azithromycin (12.7%; Table S2 in Supplementary Appendix).
Table 2.
Distribution of Respiratory Encounters and Antibiotic Prescribing Practices Among Intermountain’s Urgent Care Clinics
| Total, Respiratory | InstaCare, Respiratory | Connect Care, Respiratory | KidsCare, Respiratory | |
|---|---|---|---|---|
| N = 486 061 | 426 070 | 17 621 | 42 370 | |
| Distribution of respiratory encounter types | ||||
| Tier 1 | 9.2% (n = 44 727/486 061) | 9.4% (40 090/426 070) | 0.3% (47/17 621) | 10.8% (4590/42 370) |
| Tier 2 | 49.9% (n = 242 343/486 061) | 49.9% (212 432/426 070) | 53.8% (9484/17 621) | 48.2% (20 427/42 370) |
| Tier 3 | 40.9% (n = 198 991/486 061) | 40.7% (173 548/426 070) | 45.9% (8090/17 621) | 41% (17 353/42 370) |
| Respiratory encounter antibiotic prescribing rates | ||||
| Total respiratory prescribing rates | 49.9% (242 651/486 061) | 51.3% (218 445/426 070) | 44.4% (7829/17 621) | 38.7% (16 377/42 370) |
| Tier 1 | 96.6% (43 187/44 727) | 96.5% (38 686/40 090) | 31.9% (15/47) | 97.7% (4486/4590) |
| Tier 2 | 64.8% (157 078/242 343) | 65.4% (138 948/212 432) | 81.3% (7715/9484) | 51% (10 415/20 427) |
| Tier 3 | 21.3% (42 386/198 991) | 23.5% (40 811/173 548) | 1.2% (99/8090) | 8.5% (1476/17 353) |
| Respiratory tier distribution among respiratory encounters where an antibiotic was prescribed | ||||
| Tier 1 | 17.8% (43 187/242 651) | 17.7% (38 686/218 445) | 0.2% (15/7829) | 27.4% (4486/16 377) |
| Tier 2 | 64.7% (157 078/242 651) | 63.6% (138 948/218 445) | 98.5% (7715/7829) | 63.6% (10 415/16 377) |
| Tier 3 | 17.5% (42 386/242 651) | 18.7% (40 811/218 445) | 1.3% (99/7820) | 9% (1476/16 377) |
In Tier 1, antibiotics were almost always indicated (eg, pneumonia); in Tier 2, antibiotics may have been indicated (eg, sinusitis); and in Tier 3, antibiotics were not indicated (eg, bronchitis).
Antibiotic Prescribing Variability in Respiratory Encounters
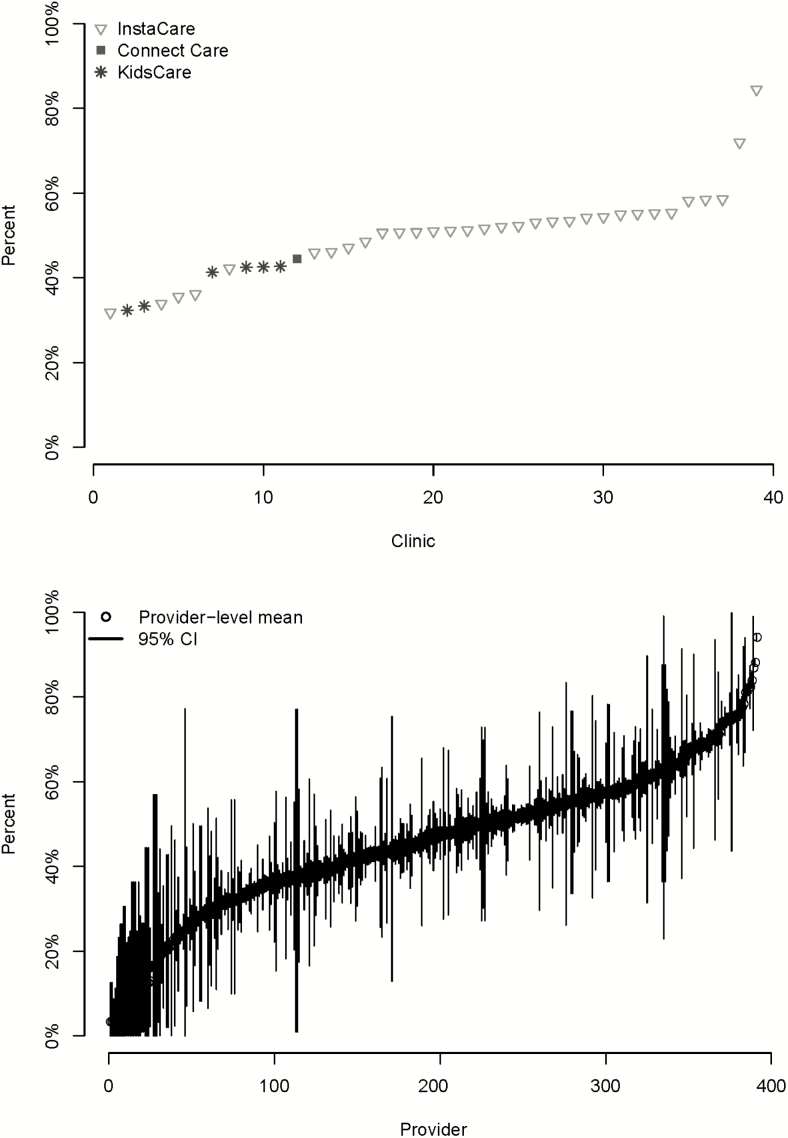
Overall, 49.9% of respiratory encounters resulted in the prescription of an antibiotic. The variability in respiratory antibiotic prescribing by clinic and provider is shown in Figure 2A and B, respectively. The median percent of all respiratory encounters with antibiotics prescribed was 51.0% (IQI, 42.6–54.3), with percentages ranging from 31.0% to 84.4% by clinic. Antibiotic prescribing for respiratory conditions was lower at KidsCare clinics (38.7% of encounters; P < .001) and Connect Care clinics (44.4%; P < .001), compared to InstaCare clinics (51.3%). A median of 47.2% (IQI, 36–56.8) of respiratory encounters resulted in the prescription of antibiotics, with percentages ranging from 3.3% to 94.1% by provider. The ICC for providers (0.105) was higher than for clinics (0.0026), indicating that a greater proportion of variation was explained by providers than clinics.
Figure 2.
The percentages of urgent care encounters for respiratory conditions with an antibiotic prescription, by (A) individual clinics and (B) individual providers. Data represent 39 total clinic sites (32 InstaCare [all ages], 6 KidsCare [<18 years], and 1 Connect Care [telemedicine]) and 396 providers. Respiratory conditions are defined in the Supplementary Appendix. The vertical lines represent 95% confidence intervals (CIs).
Antibiotic Prescribing Variability in Tier 3 Respiratory Encounters
Overall, 21.3% of Tier 3 respiratory encounters resulted in the prescription of an antibiotic. The variabilities in antibiotic prescribing for Tier 3 respiratory conditions by clinic and provider are shown in Figure S1A and B in the Supplementary Appendix. The median percent of Tier 3 respiratory encounters that had antibiotics prescribed was 21.7% (IQI, 12.9–25.0), with percentages ranging from 1.2% to 67.9% by clinic. The percentages of Tier 3 respiratory encounters that resulted in the prescription of antibiotics were lower at KidsCare clinics (8.5% of encounters; P < .001) and Connect Care clinics (1.2%; P < .001), compared to InstaCare clinics (23.5%). A median of 15.0% (IQI, 6.6–27.7) of Tier 3 respiratory encounters resulted in antibiotic prescriptions, with percentages ranging from 0.25% to 83.3% by provider. The ICC for providers (0.247) was higher than for clinics (0.0459), indicating that a greater proportion of variation was due to providers than clinics.
First-line Antibiotic Prescribing Variability
For encounters where patients were diagnosed with pharyngitis, sinusitis, or AOM and an antibiotic was prescribed, 69.2% of the prescriptions were for a first-line antibiotic. The variabilities in first-line antibiotic prescribing by clinic and provider are shown in Figure S2A and B in the Supplementary Appendix. A median of 70.6% (IQI, 65.9–73.8) of encounters for these conditions resulted in the prescription of a first-line antibiotic, with percentages ranging from 49.3% to 87.8% by clinic. The percentages of encounters for these conditions that resulted in the prescription of first-line antibiotics were higher at KidsCare clinics (85.5%; P < .001) and lower at Connect Care clinics (59.3%; P < .001), compared to InstaCare clinics (68.4%). A median of 75.0% (IQI, 66.8–81.9) of encounters for these conditions had first-line antibiotics prescribed, with percentages ranging from 14.4% to 96.7% by provider. The ICC for providers (0.0867) was higher than for clinics (0.0101).
Patient Satisfaction
During the 5-month period where patient satisfaction survey and antibiotic prescribing data were available, 10 179 surveys were completed for encounters for Tier 2 and Tier 3 respiratory conditions. Among these, antibiotics were prescribed in 5239 (51%) encounters. The mean satisfaction score for visits where an antibiotic was prescribed was slightly higher (8.68; 95% CI, 8.64–8.73), compared to visits where an antibiotic was not prescribed (8.33; 95% CI, 8.27–8.38).
DISCUSSION
In a large network of UCs, 34% of visits resulted in antibiotic prescriptions, and respiratory conditions accounted for the majority of these prescriptions (61%). For respiratory conditions specifically, antibiotics were prescribed half of the time, yet variability at the level of the provider ranged from prescribing antibiotics during as few as 3% to as many as 94% of encounters. Additionally, substantial variability existed among individual providers in appropriate prescribing of antibiotics, including antibiotic use for conditions that never warrant antibiotics and the use of first-line antibiotics. Collectively, these findings support the importance of integrating antibiotic stewardship principles into UC settings and developing interventions specifically targeting UC settings.
Many outpatient stewardship interventions have focused on reducing unnecessary antibiotic prescribing for conditions for which antibiotics are completely unnecessary [7, 8, 11]. However, our findings highlight the importance of Tier 2 respiratory conditions, including pharyngitis, sinusitis, and AOM. Collectively, these accounted for more than half of all antibiotic prescriptions; by comparison, Tier 3 respiratory conditions accounted for fewer than 1 in 5. Stewardship interventions that target Tier 2 respiratory conditions have the potential for substantial impacts through ensuring appropriate diagnoses to reduce unnecessary antibiotic use, utilizing delayed prescriptions for sinusitis and AOM, and promoting appropriate antibiotic selection.
Overall, antibiotic prescribing in the IH UC setting was similar to results from a national study (34% of visits for IH UC versus 39% nationally) [17]. However, we observed tremendous variability in all respiratory antibiotic prescribing metrics at the level of the individual prescriber, such that the highest-prescribing clinicians prescribed antibiotics nearly 5 times as often as the lowest-prescribing clinicians. The substantial between-clinician variability in appropriateness metrics, such as prescribing for Tier 3 respiratory conditions (ideally very low) and the use of first-line antibiotics (ideally very high), demonstrates that variability in appropriate prescribing also exists. These findings suggest that peer-comparison stewardship interventions, used successfully in primary care, could be used in UC and may need to be more intensively targeted towards selected clinicians with poor performance.
Patient satisfaction is important in all health-care settings. In our data, the mean satisfaction scores were slightly higher during those visits where antibiotics were prescribed compared those to where antibiotics were not prescribed, which is a trend seen in other outpatient settings [18–21]. These differences were so small that they can be used to reassure providers in our system that improving prescribing is unlikely to meaningfully impact patient satisfaction.
In respiratory encounters, we found that overall antibiotic prescribing was lower and measures of appropriateness were higher in KidsCare clinics, compared to InstaCare clinics. Additionally, overall and Tier 3 respiratory prescribing were also lower in Connect Care clinics than InstaCare clinics. Differences in overall antibiotic prescribing between settings could be explained by differences in case mixes and comorbidity profiles among InstaCare, KidsCare, and Connect Care clinics. Prior studies are consistent with our findings and have indicated that pediatricians prescribe antibiotics less often than other specialties [22, 23]. On the other hand, the relatively lower prescribing rates during telemedicine visits for Tier 3 respiratory conditions differs from rates reported from recent studies [24, 25]. A potential explanation is that our study focused on care within an integrated care delivery network, where incentives to prescribe antibiotics may be different than in other telemedicine settings [26]. Additionally, even though the IH UC network has not participated in a dedicated, system-wide antibiotic stewardship intervention, IH has a strong culture of antibiotic stewardship [27–30], which may partly explain differences in antibiotic prescribing practices compared to national studies.
Our study has limitations that may limit generalizability. Compared to national averages, antibiotic prescribing rates have been relatively low both in this geographic region [31] and in the IH system, which could have led to an underestimation of the extent to which inappropriate antibiotic prescribing occurs in UC settings. IH is an integrated care delivery system, which may lead to different practice patterns than in other types of UCs, due to differences such as physician compensation models and patient access to care. Our unit of analysis for antibiotic prescribing was the electronic prescription; this did not enable a distinction between immediate and delayed prescriptions, nor did this capture actual antibiotic fills. Thus, we may have overestimated actual antibiotic consumption. In addition, we did not assess the concordance of billed ICD10 codes and clinical diagnoses or accounts for laboratory confirmations of group A Streptococcus, which limited our ability to assess whether antibiotics were truly justified. For the analysis of first-line antibiotic prescribing, we did not account for recent antibiotic use or allergies, which affect antibiotic selection and may have led to an underestimation of appropriateness.
In conclusion, we found that in a large network of UC clinics, most encounters were for infectious disease conditions and substantial variability in antibiotic prescribing practices and appropriateness existed at the level of individual providers. These findings will require additional study to identify those predictors of antibiotic prescribing variability that would be amenable to stewardship interventions. Several UC organizations, such as the Urgent Care Association, have made commitments to improve antibiotic use [30]. The engagement of these industry partners will be critical to the success of stewardship initiatives in UC. Because UC encounters are rapidly growing nationwide, the design and implementation of stewardship strategies that are specifically tailored to UC settings through partnerships between UCs and stewardship communities is an urgent priority.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support. This work was supported by the Centers for Disease Control and Prevention Safety and Healthcare Epidemiology Prevention Research Development (contract number 200-2016-91799).
Potential conflicts of interest. K. D. B. has received grants from the American Medical Association and Centers for Disease Control and Prevention, outside the submitted work. R. S. is the physician founder of Innovation in Pediatric Education-Pediatric Research in Inpatient Settings Accelerating Safe Sign-outs Patient Safety Institute, with equities owned by Intermountain Healthcare; is an executive council member of Pediatric Research in Inpatient Settings; and reports grants from the Agency for Healthcare Research and Quality, the Patient-Centered Outcomes Research Institute, and the National Institutes of Health, outside the submitted work. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Frost HM, Knepper BC, Shihadeh KC, Jenkins TC. A novel approach to evaluate antibiotic utilization across the spectrum of inpatient and ambulatory care and implications for prioritization of antibiotic stewardship efforts. Clin Infect Dis 2019. PMID: 31162539. [DOI] [PubMed] [Google Scholar]
- 2. Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Matusiak LM, Schumock GT. Antibiotic expenditures by medication, class, and healthcare setting in the United States, 2010-2015. Clin Infect Dis 2018; 66:185–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA 2016; 315:1864–73. [DOI] [PubMed] [Google Scholar]
- 4. Lessa FC, Winston LG, McDonald LC; Emerging Infections Program Clostridium difficile Surveillance Team. Burden of Clostridium difficile infection in the United States. N Engl J Med 2015; 372:2369–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Geller AI, Lovegrove MC, Shehab N, Hicks LA, Sapiano MRP, Budnitz DS. National estimates of emergency department visits for antibiotic adverse events among adults-United States, 2011-2015. J Gen Intern Med 2018; 33:1060–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Meeker D, Knight TK, Friedberg MW, et al. Nudging guideline-concordant antibiotic prescribing: a randomized clinical trial. JAMA Intern Med 2014; 174:425–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA 2016; 315:562–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gonzales R, Anderer T, McCulloch CE, et al. A cluster randomized trial of decision support strategies for reducing antibiotic use in acute bronchitis. JAMA Intern Med 2013; 173:267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gerber JS, Prasad PA, Fiks AG, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians: a randomized trial. JAMA 2013; 309:2345–52. [DOI] [PubMed] [Google Scholar]
- 10. Yadav K, Meeker D, Mistry RD, et al. A multifaceted intervention improves prescribing for acute respiratory infection for adults and children in emergency department and urgent care settings. Acad Emerg Med 2019; 26:719–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hicks LA, King LM, Fleming-Dutra KE. Improving outpatient antibiotic prescribing. BMJ 2019; 364:l289. [DOI] [PubMed] [Google Scholar]
- 12. Ashwood JS, Reid RO, Setodji CM, Weber E, Gaynor M, Mehrotra A. Trends in retail clinic use among the commercially insured. Am J Manag Care 2011; 17:e443–448. [PMC free article] [PubMed] [Google Scholar]
- 13. Poon SJ, Schuur JD, Mehrotra A. Trends in visits to acute care venues for treatment of low-acuity conditions in the United States from 2008 to 2015. JAMA Intern Med 2018; 178:1342–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hart J, Woodruff M, Joy E, et al. Association of age, systolic blood pressure, and heart rate with adult morbidity and mortality after urgent care visits. West J Emerg Med 2016; 17:591–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Palms DL, Hicks LA, Bartoces M, et al. Comparison of antibiotic prescribing in retail clinics, urgent care centers, emergency departments, and traditional ambulatory care settings in the United States. JAMA Intern Med 2018; 178:1267–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. About CAHPS. Rockville, MD: Agency for Healthcare Research and Quality, 2019. Available at: https://www.ahrq.gov/cahps/about-cahps/index.html Accessed 19 July 2019. [Google Scholar]
- 17. Palms DL, Hicks LA, Bartoces M, et al. Comparison of antibiotic prescribing in retail clinics, urgent care centers, emergency departments, and traditional ambulatory care settings in the United States. JAMA Intern Med 2018; 178:1267–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jerant A, Fenton JJ, Kravitz RL, et al. Association of clinician denial of patient requests with patient satisfaction. JAMA Intern Med 2018; 178:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martinez KA, Rood M, Jhangiani N, Kou L, Boissy A, Rothberg MB. Association between antibiotic prescribing for respiratory tract infections and patient satisfaction in direct-to-consumer telemedicine. JAMA Intern Med 2018; 178:1558–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ashworth M, White P, Jongsma H, Schofield P, Armstrong D. Antibiotic prescribing and patient satisfaction in primary care in England: cross-sectional analysis of national patient survey data and prescribing data. Br J Gen Pract 2016; 66:e40–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cals JW, Boumans D, Lardinois RJ, et al. Public beliefs on antibiotics and respiratory tract infections: an internet-based questionnaire study. Br J Gen Pract 2007; 57:942–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hersh AL, Fleming-Dutra KE, Shapiro DJ, Hyun DY, Hicks LA; Outpatient Antibiotic Use Target-Setting Workgroup Frequency of first-line antibiotic selection among US ambulatory care visits for otitis media, sinusitis, and pharyngitis. JAMA Intern Med 2016; 176:1870–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. King LM, Bartoces M, Fleming-Dutra KE, Roberts RM, Hicks LA. Changes in US outpatient antibiotic prescriptions from 2011-2016. Clin Infect Dis 2019. PMID: 30882145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ray KN, Shi Z, Gidengil CA, Poon SJ, Uscher-Pines L, Mehrotra A. Antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics 2019; 143:e20182491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Antibiotic prescribing for acute respiratory infections in direct-to-consumer telemedicine visits. JAMA Intern Med 2015; 175:1234–5. [DOI] [PubMed] [Google Scholar]
- 26. Hersh AL, Stenehjem E, Daines W. RE: antibiotic prescribing during pediatric direct-to-consumer telemedicine visits. Pediatrics 2019; 144:e20190533. [DOI] [PubMed] [Google Scholar]
- 27. Dean NC, Jones BE, Jones JP, et al. Impact of an electronic clinical decision support tool for emergency department patients with pneumonia. Ann Emerg Med 2015; 66:511–20. [DOI] [PubMed] [Google Scholar]
- 28. Stenehjem E, Hersh AL, Buckel WR, et al. Impact of implementing antibiotic stewardship programs in 15 small hospitals: a cluster-randomized intervention. Clin Infect Dis 2018; 67:525–32. [DOI] [PubMed] [Google Scholar]
- 29. Pestotnik SL, Classen DC, Evans RS, Burke JP. Implementing antibiotic practice guidelines through computer-assisted decision support: clinical and financial outcomes. Ann Intern Med 1996; 124:884–90. [DOI] [PubMed] [Google Scholar]
- 30. Centers for Diesease Control and Prevention. The AMR challenge. Available at: https://www.cdc.gov/drugresistance/intl-activities/amr-challenge.html. Accessed 22 July 2019. [Google Scholar]
- 31. Hicks LA, Bartoces MG, Roberts RM, et al. US outpatient antibiotic prescribing variation according to geography, patient population, and provider specialty in 2011. Clin Infect Dis 2015; 60:1308–16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.