Abstract
Objectives
This study aims to examine whether older workers aged 50–64 years with multimorbidity are at increased risk to transition from full-time paid employment to part-time employment, partial retirement, unemployment, disability, economic inactivity, full retirement or die than workers without a chronic health condition and workers with one chronic health condition, and whether socioeconomic position (SEP) modifies these transitions.
Method
Using data from the Health and Retirement Study (1992–2014; n = 10,719), sub-distribution hazard ratios with 95% confidence intervals were calculated with a time-varying Fine and Gray competing-risks survival regression model to examine exit from full-time paid employment. We investigated the modifying effect of SEP by examining its interaction with multimorbidity.
Results
Workers with multimorbidity had a higher risk of transitioning to partial retirement (1.45; 1.22, 1.72), disability (1.84; 1.21, 2.78) and full retirement (1.63; 1.47, 1.81), and they had a higher mortality risk (2.58; 1.71, 3.88) than workers without chronic disorders. Compared to workers with one chronic health condition, workers with multimorbidity had an increased risk for partial (1.19; 1.02, 1.40) and full retirement (1.29; 1.17, 1.42), and mortality (1.49; 1.09, 2.04). Only SEP measured as educational level modified the relationship between multimorbidity and mortality.
Discussion
Workers with multimorbidity seem more prone to leave full-time paid employment than workers without or with one a chronic health condition. Personalized work accommodations may be necessary to help workers with multimorbidity prolong their working life.
Keywords: Chronic health condition, Labor market participation, Socioeconomic position, Transition
Multimorbidity is becoming increasingly more common (Uijen & van de Lisdonk, 2008; Ward & Schiller, 2013), affecting both individuals and society (Murray et al., 2012; Wolff, Starfield, & Anderson, 2002). Multimorbidity is defined as the co-occurrence of two or more chronic health conditions (CHCs) where, in contrast to the concept of comorbidity, none of these are considered the primary condition (van den Akker, Buntinx, & Knottnerus, 1996; van den Akker, Buntinx, Metsemakers, Roos, & Knottnerus, 1998). Multimorbidity is a major burden in terms of disability-adjusted life years (Murray et al., 2012), and poses a major challenge to health care and welfare systems in terms of health care delivery and costs (Wolff et al., 2002). The risk for multimorbidity rises with increasing age (van den Akker et al., 1998), and it is estimated that about half of all people aged 65 years and older report more than one CHC (Barnett et al., 2012). This suggests that a substantial part of older workers (i.e., often defined as workers aged ≥50 years (Organisation for EconomicCo-operation and Development, 2014)) have multimorbidity. However, the degree to which multimorbidity affects older workers’ transition out of full-time paid employment, and how, remains largely unknown.
Multimorbidity may affect the labor market participation of older workers and how they transition out of full-time paid employment. Older workers may reduce their full-time paid employment by transitioning to part-time work or partial retirement, or they may leave full-time paid employment through disability, unemployment, economic inactivity, or full retirement. Also, workers with multimorbidity may die before reaching retirement. All these trajectories, including mortality, serve as potentially competing transitions in exits from full-time paid employment; for example, “early retirement” would impede an exit transition into “leaving work because of disability” (Reeuwijk, van Klaveren, van Rijn, Burdorf, & Robroek, 2017). There is ample evidence that CHCs negatively affect people’s labor market participation (de Boer et al., 2018; Bøje, 2014; Breton et al., 2013; Carlsen, Oksbjerg Dalton, Frederiksen, Diderichsen, & Johansen, 2008; Kjær et al., 2013; Kouwenhoven-Pasmooij, Burdorf, Roos-Hesselink, Hunink, & Robroek, 2016; Sin, Stafinski, Ng, Bell, & Jacobs, 2002; Smith et al., 2014; Ubalde-Lopez, Delclos, Benavides, Calvo-Bonacho, & Gimeno, 2016; Ubalde-Lopez et al., 2017). For example, common CHCs, such as type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD), and chronic obstructive pulmonary disease, have been related to absenteeism, unemployment, disability benefits, and early retirement (de Boer et al., 2018; Breton et al., 2013; Kouwenhoven-Pasmooij et al., 2016; Sin et al., 2002; Smith et al., 2014).
Multimorbidity may have a particularly strong impact on the ability to remain in full-time paid employment compared to having no or just one CHC. Studies have shown that multimorbidity increases the risk for sickness absence (Ubalde-Lopez et al., 2016, 2017) and early retirement (Bøje, 2014; Carlsen et al., 2008; Kjær et al., 2013) beyond the risk of having just one CHC. In addition, a study in Canadian adults found that combinations of chronic conditions were associated with a greater risk of not being able to work due to health reasons than the individual effects of each chronic condition by itself (Smith et al., 2014). In contrast, in a study in older European workers on early exit from paid work, interaction effects were observed neither between diabetes or CVD and comorbidity (Kouwenhoven-Pasmooij et al., 2016). Given these somewhat consistent findings, the role of multimorbidity on competing transitions out of full-time paid employment, compared to having no or one CHC, remains poorly understood. The current study will try to elucidate the effect of multimorbidity on competing transitions out of full-time paid employment. On the basis of the rather scarce literature summarized earlier, we hypothesize that workers with multmorbidity are at increased risk to leave full-time paid employment through disability, unemployment, economic inactivity, or full retirement instead of reducing paid employment through a transition to part-time work or partial retirement because the poor health status of these workers may not allow for a gradual transition out of full-time paid employment.
A potentially important factor in the context of multimorbidity and the transition out of full-time paid employment is socioeconomic position (SEP). SEP embodies a wide array of resources such as money, knowledge, and social connections (Link & Phelan, 1995). According to the fundamental causes of health inequalities theory (Link & Phelan, 1995), differences in the distribution of these factors across socioeconomic groups may explain the large health inequalities found across socioeconomic groups. It is already known that low SEP is related to the development of chronic disorders and multimorbidity (Barnett et al., 2012; Tucker-Seeley, Li, Sorensen, & Subramanian, 2011), and it has also been shown that low SEP affects transitions out of paid employment (Schuring, Robroek, Otten, Arts, & Burdorf, 2013). However, it is unclear whether SEP further modifies the relationship between multimorbidity and older workers’ transitions out of full-time paid employment. A better understanding of the role of SEP is necessary to tackle the large inequalities in work and health-related outcomes across socioeconomic groups.
SEP may modify the relationship between multimorbidity and the transition out of full-time paid employment because of several reasons. In general, people with a low SEP have more physically demanding work than people with a high SEP, they have an unhealthier lifestyle (Govil, Weidner, Merritt-Worden, & Ornish, 2009), they experience more difficulties in coping with CHCs (Sloan, Padrón, & Platt, 2009), they have lower adherence to prescribed medications (Wamala, Merlo, Bostrom, Hogstedt, & Agren, 2007), and have more difficulties in accessing health care (Vart, Gansevoort, Crews, Reijneveld, & Bültmann, 2015). All these factors may influence the ability and decision to stay in full-time paid employment in the context of multimorbidity. On the basis of extensive literature showing that individuals with a low SEP are generally worse off regarding many health- and work-related outcomes than their high SEP counterparts (Burgard & Lin, 2013; Mackenbach et al., 2008), we hypothesize that workers with a low SEP and multimorbidity are more likely to leave full-time paid employment than workers with a high SEP and multimorbidity.
It is important to gain a better understanding of the effect of multimorbidity on older workers’ transitions out of full-time paid employment because many industrialized countries are currently stimulating their citizens to prolong their working lives to keep health care and welfare systems sustainable in coming decades (Harper, 2014). Consequently, the share of older workers in the labor market is rising sharply in many countries (Harper, 2014), among many of whom have multimorbidity (Barnett et al., 2012). Better knowledge may provide guidance on how to accommodate workers with multimorbidity at the workplace through tailored prevention and interventions so that they may remain in work despite their health status. This is important not only for society to keep health care and welfare systems sustainable, but also for individuals because work offers them the possibility to earn an income, fulfil a social role, and give meaning to their lives (Bowling, 1995; McKee-Ryan, Song, Wanberg, & Kinicki, 2005).
The aims of this study were to examine (a) whether older workers aged 50–64 years with multimorbidity are at increased risk to reduce paid employment (i.e., part-time work and partial retirement combined) or leave full-time paid employment (i.e., disability, unemployment, economic inactivity, and full retirement combined) than workers without CHCs, (b) the effect of multimorbidity on the specific type of transition out of full-time paid employment (i.e., to part-time work, partial retirement, disability, unemployment, economic inactivity, full retirement, and mortality), and (c) to investigate whether SEP modifies the relationship between multimorbidity and the specific type of transition out of full-time paid employment. We hypothesize that full-time workers with multimorbidity are more prone to leave full-time paid employment than to reduce paid employment, compared to workers without CHCs. We further hypothesize that low SEP increases the risk for leaving full-time paid employment when having multimorbidity.
Method
Study Design and Sample
The study was conducted using data from the Health and Retirement Study (HRS) (Sonnega et al., 2014). The HRS is a longitudinal cohort study conducted in the United States that includes more than 37,000 individuals from more than 23,000 households. Index participants were aged more than 50 years. The HRS covers four major topics—income and wealth; health, cognition, and use of health care services; work and retirement; and family connections. The HRS was established to better understand aging and to examine national-level social and policy changes that may affect individuals. The initial HRS cohort was interviewed for the first time in 1992 and followed up at 2-year intervals. Between 1992 and 2010, five other cohorts were merged with the initial HRS cohort; Asset and Health Dynamics Among the Oldest Old (AHEAD; 1993), the Children of the Depression (CODA; 1998), the War Babies (1998), Early Baby Boomers (EBB; 2004), and Mid Baby Boomers (MBB; 2010) to become a nationally representative cohort study. More details on study design are described elsewhere (Sonnega et al., 2014). The HRS is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and is conducted by the University of Michigan. The HRS was approved by the institutional review board at the University of Michigan, and all participants have provided informed consent.
For this study, we used data from the RAND Contributed Files (v.P), which include data from 1992 to 2014 (Health and Retirement Study, 2016). We restricted the analyses to participants aged 50–64 years at baseline who worked full time at their first measurement wave. The age restriction was to prevent inclusion of a highly selective group, that is, the older-old still at work. The restriction to full-time paid workers was done because routes for leaving full-time and part-time employment are slightly different. Full-time workers may still have the option to transition to part-time employment whereas part-time workers do not have this option. This led to exclusion of 16,301 of the 37,495 participants due to age ineligibility and 9,455 participants due to not working full-time at baseline. We also excluded 605 participants with a person-level analysis weight of zero on their first measurement because these participants will be automatically omitted in the analysis. Finally, we excluded participants missing all follow-up measurements but not known to be deceased prior to their first follow-up interview (n = 415), resulting in a final sample size of 10,719 participants.
Measures and Procedure
Transitions from full-time paid employment to another employment status
Employment status and thus the type of transition out of full-time paid employment was assessed at every measurement wave (i.e., biennially) by asking participants the question: “What is your labor force status?” with answer categories “work full-time,” “work part-time,” “unemployed,” “partly retired,” “retired,” “disabled,” and “not in labor force”. The latter comprises people who are economically inactive; neither working nor looking for work. Workers transitioning from full-time paid employment to part-time paid employment or partial retirement were considered to reduce paid employment. Workers transitioning to unemployment, disability, economic inactivity, and full retirement were considered to leave full-time paid employment. In addition, mortality was registered during follow-up and was considered a competing event.
Multimorbidity
Multimorbidity was assessed at baseline and during all follow-up measurements by asking participants whether or not a doctor had ever told them that they had any of the following CHCs: (a) high blood pressure or hypertension; (b) diabetes or high blood sugar; (c) cancer or a malignant tumor of any kind except skin cancer; (d) chronic lung disease such as chronic bronchitis or emphysema except asthma; (e) heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems; (f) stroke or transient ischemic attack; (g) emotional, nervous, or psychiatric problems; and (h) arthritis or rheumatism. All CHCs, and the handling of disputes, are described in detail elsewhere (Bugliari et al., 2016). In short, with the exception of cases that dispute a report from a prior wave, each of these variables is set to “yes” if the respondent answered “yes” to the pertinent question in the current or any prior wave, and to “no” if the respondent responded “no” at the current and all prior waves. Therefore, respondents could only remain stable or increase regarding their number of CHCs. In line with previous work on the HRS (Tucker-Seeley et al., 2011), a categorical, time-varying variable based on the sum of the CHCs was created, indicating whether participants had no CHC, one CHC, or multimorbidity. With this approach, participants could have three observation periods (i.e., time without a CHC, time with one CHC, time with multimorbidity). Participants with no CHC were the reference category.
Socioeconomic position
SEP was assessed with two indicators; wealth and educational level, with wealth as the main indicator for SEP. Wealth was assessed at baseline as total wealth calculated as the sum of 10 assets components (i.e., value of primary residence, net value of vehicles, net value of real estate, net value of businesses, net value of Individual Retirement Accounts/Keogh accounts, net value of stocks, mutual funds, and investment trusts, value of checking, savings, or money market accounts, value of certificates of deposit, government saving bonds, and T-bills, net value of bonds and bond funds, net value of all other savings) minus all debt components (i.e., value of all mortgages/land contracts [primary residence], value of other home loans [primary residence], and value of other debts). All wealth components, and the imputation of missing wealth components, are described in detail elsewhere (Bugliari et al., 2016). Wealth was divided into quartiles (<US$30.000; US$30,000–<US$100,000; US$100,000–<US$246,500; ≥US$246,500) because of the skewed distribution. Educational level was assessed at baseline by asking participants their highest educational level achieved and was categorized into less than high school, high-school graduate (or General Education Development), some college, and college and above.
Covariates
Age, gender, race, and marital status were used as covariates in this study. Age was categorized into three groups, that is, 50–54, 55–59, and 60–64 years old. Race was categorized into non-Hispanic Whites, African Americans, and Other (e.g., American Indian or Alaskan Native, Asian or Pacific Islander). Marital status was categorized into married/partnered (i.e., married, married spouse absent, partnered) and not married/partnered (i.e., separated, divorced, separated/divorced, widowed, never married).
Statistical Analyses
First, we used frequencies to describe dichotomous and categorical variables, and means and standard deviations (SDs), or medians and interquartile ranges to describe continuous variables.
Second, we examined whether workers with multimorbidity were at increased risk to reduce full-time paid employment (i.e., to part-time work and partial retirement combined) or leave it (i.e., to disability, unemployment, economic inactivity, and full retirement combined) compared to workers without CHCs using a time-dependent Fine and Gray competing-risk survival regression model (Fine & Gray, 1999). We calculated sub-distribution hazard ratios (SHRs) with corresponding 95% confidence intervals (CIs). Competing-risk regression is an alternative to Cox regression for survival data in the presence of competing risks. The term competing risk refers to the chance that, for example, instead of the event of interest “reducing paid employment,” we will observe a competing event “leaving paid employment” or “mortality”. A competing event impedes the occurrence of the main event of interest. This is not to be confused with the usual right censoring found in survival data, such as censoring due to loss of follow-up. Therefore, competing events are distinct from standard censoring (StataCorp, 2017). These, and the following, analyses were adjusted for age, gender, race, marital status, educational level, wealth, and for the dependency of observations within participants.
Third, we examined the effect of multimorbidity on the specific type of transition out of full-time paid employment (i.e., transition to part-time work, partial retirement, disability, unemployment, economic inactivity, full retirement, or mortality) during follow-up, using a time-dependent Fine and Gray competing-risks survival regression model (Fine & Gray, 1999). We also examined the potential modifying role of age, gender, and marital status by adding interaction terms between these covariates and multimorbidity.
Fourth, to examine the modifying role of SEP we separately added an interaction term between wealth and multimorbidity and between educational level and multimorbidity to the competing-risks regression models.
In sensitivity analyses, we investigated possible effect modification of SEP on the relationship between multimorbidity and transitions out of full-time paid employment using current and longest held occupational class (blue vs white collar) as indicator for SEP. In a second sensitivity analysis, we added insurance status (i.e., health care insurance by employer or government [no/yes]) to our models to examine whether the relationship between multimorbidity and transitions out of full-time paid employment was attenuated.
We accounted for the stratified random sample design of the HRS by using person-level analysis weights as provided in the RAND HRS data set. These weights correspond to the number of individuals in the U.S. population by the March Current Population Survey for the year of data collection. Analyses were conducted using Stata 15 (Stata Corp, College Station, TX, USA).
Results
Baseline Characteristics
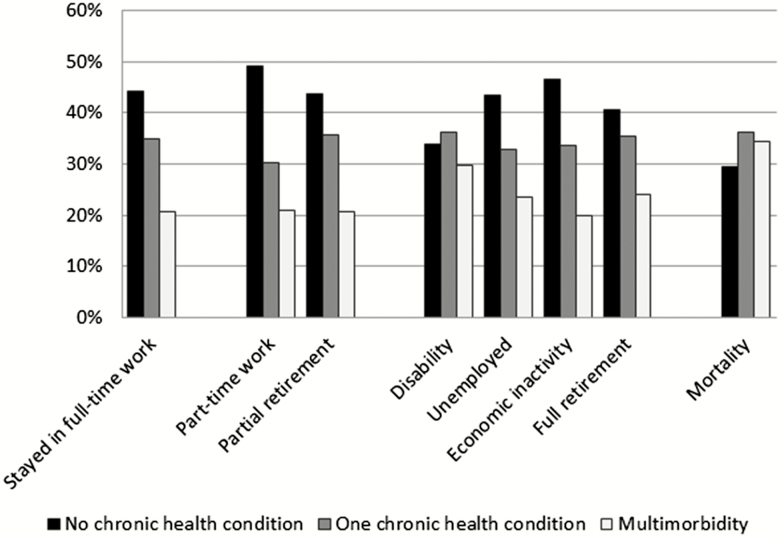
The study population consisted of 10,719 full-time workers at baseline, with a median follow-up time of 4.2 years (25th–75th percentile: 3.3–9.6) until any event or censoring. Mean age at baseline was 53.8 years (SD: 2.7) and the majority of participants was male (60.0%) (Table 1). The median follow-up time to a transition ranged from 3.8 years (disability and economic inactivity) to 7.5 years (full retirement) (Supplementary Table 1). In total, 68.8% of the study population left full-time paid employment during follow-up and transitioned to part-time work (12.9%), partial retirement (12.0%), disability (2.4%), unemployment (6.8%), economic inactivity (2.6%), or full retirement (32.1%). In addition, 2.8% of the participants died before they transitioned out of full-time paid employment. At baseline, 22.3% of the participants reported multimorbidity and 34.5% reported one CHC. The baseline prevalence of multimorbidity was highest among participants who left full-time paid employment into disability and among participants who died before otherwise leaving full-time paid employment (Figure 1). The baseline prevalence of most individual CHCs (e.g., diabetes, cancer, heart disease) was also highest among these workers (Supplementary Table 2). Participants missing all follow-up measurements but not known to be deceased prior to their first follow-up interview (n = 415) and participants with missing data on race (n = 23) or marital status (n = 5) did not differ regarding age, gender, multimorbidity, and wealth from participants with complete data, but had somewhat lower education (Supplementary Table 3).
Table 1.
Baseline Characteristics of the Study Sample (n = 10,719)
| Age (years), mean (SD) | 53.8 (2.7) |
| Age (years), (%) | |
| 50–54 | 65.2 |
| 55–59 | 29.9 |
| 60–64 | 4.9 |
| Time till event (years), median (IQR) | 4.2 (3.3, 9.6) |
| Gender (%) | |
| Male | 60.0 |
| Female | 40.0 |
| Race (%)a | |
| Non-Hispanic Whites | 83.1 |
| African American | 10.5 |
| Other | 6.4 |
| Marital status (%)b | |
| Married/partnered | 73.6 |
| Not married/partnered | 26.4 |
| Educational level (%) | |
| College and above | 32.0 |
| Some college | 26.6 |
| High-school graduate | 31.1 |
| Less than high school | 10.3 |
| Wealth (%) | |
| First quartile (high) | 31.1 |
| second quartile | 25.1 |
| Third quartile | 22.2 |
| Fourth quartile (low) | 21.5 |
| Multimorbidity (%) | |
| No CHC | 43.2 |
| One CHC | 34.5 |
| Multimorbidity | 22.3 |
Notes: SD = standard deviation; CHC = chronic health condition; IQR = interquartile range.
aWe had 23 missing values on race.
bWe had five missing values on marital status.
Figure 1.
The prevalence of chronic health conditions by the specific transitions out of full-time paid employment.
Multimorbidity and Reducing and Leaving Full-Time Paid Employment
We had a total of 13,325 observations on 10,691 participants with a total time at risk of 67,704 years. Multimorbidity did not affect the risk to reduce full-time paid employment, but workers with multimorbidity had a 45% higher risk (SHR: 1.45; 95% CI: 1.33, 1.59) of leaving full-time paid employment (Table 2). Workers with one CHC also had an increased risk of leaving full-time paid employment (SHR: 1.17; 95% CI: 1.06, 1.28). Several sociodemographic factors, such as age and marital status, were important regarding the transition out of full-time paid employment (Table 2).
Table 2.
Effect of Multimorbidity on Reducing Paid Employment and Leaving Full-Time Paid Employment
| Reduction of full-time paid employment | Leaving full-time paid employment | |
|---|---|---|
| SHR (95% CI) | SHR (95% CI) | |
| Multimorbidity | ||
| No CHC | Ref | Ref |
| One CHC | 0.99 (0.88, 1.11) | 1.17 (1.06, 1.28)** |
| Multimorbidity | 1.10 (0.98, 1.24) | 1.45 (1.33, 1.59)** |
| Age (years) | ||
| 50–54 | Ref | Ref |
| 55–59 | 1.27 (1.15, 1.40)** | 1.26 (1.16, 1.35)** |
| 60–64 | 1.54 (1.29, 1.83)** | 1.96 (1.70, 2.25)** |
| Gender | ||
| Male | Ref | Ref |
| Female | 1.33 (1.21, 1.47)** | 1.00 (0.92, 1.07) |
| Race | ||
| White | Ref | Ref |
| African American | 0.98 (0.86, 1.12) | 1.11 (1.01, 1.22)* |
| Other | 0.88 (0.70, 1.11) | 1.15 (0.98, 1.34) |
| Marital status | ||
| Married | Ref | Ref |
| Not married | 0.87 (0.77, 0.99)* | 1.12 (1.03, 1.23)* |
| Education | ||
| College | Ref | Ref |
| Some college | 0.84 (0.74, 0.95)** | 1.25 (1.13, 1.39)** |
| HS graduate | 0.84 (0.75, 1.95)** | 1.40 (1.27, 1.54)** |
| Less than HS | 0.89 (0.76, 1.04) | 1.60 (1.42, 1.80)** |
| Wealth | ||
| Q1 (high) | Ref | Ref |
| Q2 | 0.83 (0.73, 0.94)** | 1.20 (1.08, 1.32)** |
| Q3 | 0.80 (0.70, 0.91)** | 1.14 (1.03, 1.27)* |
| Q4 (low) | 0.90 (0.77, 1.04) | 1.02 (0.90, 1.14) |
Notes:CHC = chronic health condition; CI = confidence interval; HS = high school; Q = quartile; SHR = sub-distribution hazard ratio.
*p < .05. **p < .01..
Multimorbidity and the Specific Transitions Out of Full-Time Paid Employment
Regarding the specific transitions in reducing full-time paid employment (Table 3), the risk of transitioning to partial retirement was higher for workers with multimorbidity (SHR: 1.45; 95% CI: 1.22, 1.72) than for workers without a CHC. The same was observed for workers with one CHC. Multimorbidity did not affect the risk for transitioning to part-time work. Workers with one CHC were less likely to transition from full-time paid employment to part-time paid employment (SHR: 0.85; 95% CI: 0.72, 1.00) than workers without a CHC. Especially age was an important sociodemographic factor regarding the transition from full-time paid employment to partial retirement. After changing the reference group to those with one CHC, workers with multimorbidity still had an increased risk to partially retire (SHR: 1.19; 95% CI: 1.02, 1.40) (Supplementary Table 4). We found no effect modification for age, gender, and marital status (Supplementary Table 5).
Table 3.
Effect of Multimorbidity on the Specific Transitions Reducing Full-Time Paid Employment
| Part-time work | Partial retirement | |
|---|---|---|
| SHR (95% CI) | SHR (95% CI) | |
| Multimorbidity | ||
| No CHC | Ref | Ref |
| One CHC | 0.85 (0.72, 1.00)* | 1.22 (1.03, 1.44)* |
| Multimorbidity | 0.89 (0.75, 1.05) | 1.45 (1.22, 1.72)** |
| Age (years) | ||
| 50–54 | Ref | Ref |
| 55–59 | 1.04 (0.91, 1.21) | 1.49 (1.29, 1.72)** |
| 60–64 | 0.79 (0.58, 1.07) | 2.46 (1.99, 3.04)** |
| Gender | ||
| Male | Ref | Ref |
| Female | 1.95 (1.70, 2.24)** | 0.81 (0.70, 0.93)** |
| Race | ||
| White | Ref | Ref |
| African American | 1.24 (1.04, 1.47)* | 0.68 (0.55, 0.84)** |
| Other | 1.16 (0.88, 1.53) | 0.58 (0.39, 0.87)** |
| Marital status | ||
| Married | Ref | Ref |
| Not married | 0.84 (0.71, 0.98)* | 0.94 (0.78, 1.13) |
| Education | ||
| College | Ref | Ref |
| Some college | 0.88 (0.74, 1.06) | 0.81 (0.68, 0.97)* |
| HS graduate | 0.92 (0.77, 1.10) | 0.80 (0.67, 0.94)** |
| Less than HS | 1.13 (0.91, 1.39) | 0.67 (0.53, 0.85)** |
| Wealth | ||
| Q1 (high) | Ref | Ref |
| Q2 | 0.85 (0.71, 1.02) | 0.86 (0.72, 1.02) |
| Q3 | 0.83 (0.69, 1.01) | 0.81 (0.67, 0.98)* |
| Q4 (low) | 1.14 (0.93, 1.39) | 0.67 (0.53, 0.84)** |
Notes:CHC = chronic health condition; CI = confidence interval; HS = high school; Q = quartile; SHR = sub-distribution hazard ratio.
*p < .05. **p < .01.
When examining the specific types of transitions related to leaving full-time paid employment (Table 4), workers with multimorbidity had a higher risk of transitioning to disability (SHR: 1.84; 95% CI: 1.21, 2.78) and full retirement (SHR: 1.63; 95% CI: 1.47, 1.81). Workers with one CHC were also more likely to transition to full retirement than workers without a CHC (SHR: 1.26; 95% CI: 1.13, 1.41). Workers with multimorbidity had no increased risk for transitioning to unemployment or economic inactivity. Again, age was the most important sociodemographic factor regarding the transition out of full-time paid employment. After changing the reference group to those with one CHC, workers with multimorbidity had an increased risk to fully retire (SHR: 1.29; 95% CI: 1.17, 1.42) but there was no increased risk to transition to disability (Supplementary Table 4). We found no effect modification for gender and marital status, but we did find effect modification by age for disability and unemployment (Supplementary Table 5). Workers aged 60–64 years with one CHC were less likely to transition to disability (SHR: 0.05; 95% CI: 0.05, 0.49) and workers aged 60–64 years with multimorbidity were less likely to transition to unemployment (SHR: 0.12; 95% CI: 0.04, 0.37) (Supplementary Table 6). A sensitivity analysis showed that insurance status did not change our main results (Supplementary Table 7).
Table 4.
Effect of Multimorbidity on the Specific Transitions Leaving Full-Time Paid Employment
| Disability | Unemployed | Economic inactivity | Full retirement | |
|---|---|---|---|---|
| SHR (95% CI) | SHR (95% CI) | SHR (95% CI) | SHR (95% CI) | |
| Multimorbidity | ||||
| No CHC | Ref | Ref | Ref | Ref |
| One CHC | 1.50 (0.98, 2.30) | 1.04 (0.83, 1.29) | 0.75 (0.52, 1.08) | 1.26 (1.13, 1.41)** |
| Multimorbidity | 1.84 (1.21, 2.78)** | 1.18 (0.94, 1.48) | 0.90 (0.62, 1.31) | 1.63 (1.47, 1.81)** |
| Age (years) | ||||
| 50–54 | Ref | Ref | Ref | Ref |
| 55–59 | 0.91 (0.66, 1.26) | 0.75 (0.61, 0.92)** | 0.52 (0.37, 0.74)** | 1.56 (1.43, 1.70)** |
| 60–64 | 0.34 (0.14, 0.82)* | 0.75 (0.47, 1.22) | 0.33 (0.17, 0.63)** | 2.70 (2.33, 3.14)** |
| Gender | ||||
| Male | Ref | Ref | Ref | Ref |
| Female | 0.93 (0.67, 1.30) | 0.91 (0.75, 1.10) | 2.01 (1.40, 2.89)** | 0.94 (0.86, 1.03) |
| Race | ||||
| White | Ref | Ref | Ref | Ref |
| African American | 1.62 (1.13, 2.33)** | 0.88 (0.68, 1.12) | 1.10 (0.71, 1.70) | 1.10 (0.98, 1.23) |
| Other | 1.14 (0.55, 2.35) | 1.58 (1.16, 2.15)** | 1.33 (0.84, 2.11) | 0.90 (0.74 (1.11) |
| Marital status | ||||
| Married | Ref | Ref | Ref | Ref |
| Not married | 1.29 (0.89, 1.87) | 1.22 (0.99, 1.51) | 1.48 (1.01, 2.18)* | 1.01 (0.90, 1.12) |
| Education | ||||
| College | Ref | Ref | Ref | Ref |
| Some college | 2.74 (1.60, 4.72)** | 1.10 (0.86, 1.41) | 1.19 (0.73, 1.93) | 1.17 (1.04, 1.32)* |
| HS graduate | 2.23 (1.35, 3.70)** | 0.89 (0.69, 1.15) | 1.09 (0.67, 1.79) | 1.50 (1.34, 1.68)** |
| Less than HS | 2.85 (1.60, 5.08)** | 0.90 (0.66, 1.23) | 3.30 (2.00, 5.43)** | 1.50 (1.31, 1.72)** |
| Wealth | ||||
| Q1 (high) | Ref | Ref | Ref | Ref |
| Q2 | 0.89 (0.52, 1.53) | 1.08 (0.82, 1.43) | 1.06 (0.67, 1.68) | 1.24 (1.11, 1.40)** |
| Q3 | 1.03 (0.60, 1.78) | 1.40 (1.06, 1.84)* | 1.14 (0.72, 1.82) | 1.09 (0.97, 1.23) |
| Q4 (low) | 1.75 (1.03, 2.98)* | 1.59 (1.19, 2.12)** | 1.19 (0.73, 1.96) | 0.79 (0.69, 0.91)** |
Notes: CHC = chronic health condition; CI = confidence interval; HS = high school; Q = quartile; SHR = sub-distribution hazard ratio.
*p < .05. **p < .01.
Multimorbidity and Mortality
The risk of mortality was increased among workers with multimorbidity (SHR: 2.58; 95% CI: 1.71, 3.88) and among workers with one CHC (SHR: 1.73; 95% CI: 1.17, 2.55) (Supplementary Table 8). After changing the reference group to those with one CHC, workers with multimorbidity still had an increased mortality risk (SHR: 1.49; 95% CI: 1.09, 2.04) (Supplementary Table 4). We found no effect modification for age, gender, and marital status (Supplementary Table 5).
The Role of Socioeconomic Position
Main effects of wealth and educational level
Educational levels lower than college and wealth lower than the highest quartile were associated with a lower risk for reducing full-time paid employment and a higher risk for leaving full-time paid employment (Table 2). When examining the specific transitions regarding reducing full-time paid employment, educational levels lower than college and the two lowest wealth quartiles were associated with a decreased risk of partial retirement (Table 3). When examining the specific transitions regarding leaving full-time paid employment, educational levels lower than college were associated with an increased risk for disability and full retirement, whereas those with an educational level less than high school had an increased risk for economic inactivity (Table 4). Compared to the highest wealth quartile, workers in the lowest wealth quartile had an increased risk to transition to disability, those in the lowest two wealth quartiles to transition to unemployment, and those in the lowest and second wealth quartile to full retirement. In addition, workers in the lowest wealth quartile had an increased mortality risk compared to those in the highest wealth quartile (Supplementary Table 8).
Modifying effects of wealth and educational level
As an additional aim, we investigated the possible modifying effect of SEP on the relationship between multimorbidity and the transitions out of full-time paid employment. SEP measured by education only modified the relationship between multimorbidity and mortality (p value: .02) and SEP measured by wealth only modified the relationship between multimorbidity and economic inactivity (p value: .02) (Supplementary Table 5). Workers with both an educational level less than high school and with multimorbidity were less likely to die (SHR: 0.27; 95% CI: 0.09, 0.85) than workers with a college degree without a CHC (Supplementary Table 6). Although the p value for the contrast of marginal linear predictions for the interaction between wealth and multimorbidity was statistically significant, we found no statistically significant interaction between specific combinations of multimorbidity and wealth categories. Sensitivity analyses showed that none of the interaction terms between multimorbidity and occupational class as indicator for SEP were statistically significant (Supplementary Table 9).
Discussion
Full-time workers with multimorbidity in their late work life had an increased risk to transition to partial retirement, disability, and full retirement compared to workers without a CHC. In addition, workers with multimorbidity had an increased mortality risk. Workers with multimorbidity were just as likely to transition to part-time work, unemployment, and economic inactivity as workers without a CHC. Results were similar for workers with one CHC, except that they had no increased risk for the transition to disability and had a decreased risk to transition to part-time work. Importantly, compared to workers with one CHC, workers with multimorbidity had an increased risk to partially and fully retire and to die. We found no modifying effect of SEP on the relationship between multimorbidity and the transition from full-time paid employment to another employment status. However, we did find that SEP had a main effect on the transition out of full-time paid employment. Low SEP workers were generally more likely to transition to disability, unemployment, economic inactivity, or die.
Results from this study suggest that full-time workers with multimorbidity are more prone to transition from full-time paid employment to disability and partial and full retirement than their counterparts without a CHC. This is in line with European studies showing that poor self-rated health increases the likelihood of labor force exit into unemployment, disability pension, and early retirement (Reeuwijk et al., 2017; Robroek, Schuring, Croezen, Stattin, & Burdorf, 2013; Schuring et al., 2013). Studies focusing on workers with cancer show that comorbidities like CVD and T2DM were more important for exit from paid work than disease-related factors such as tumor site and tumor stage (Carlsen et al., 2008; Kjær et al., 2013). Workers with one CHC also had an increased risk to transition to partial and full retirement and to die than workers without a CHC but the magnitude of their risk was lower than the risk for those with multimorbidity. Compared to workers with multimorbidity, however, their risk was significantly lower. In addition, we found that the effect of multimorbidity on transitions out of full-time paid employment was homogeneous across age groups, gender, race, and marital status. This suggests that interventions to reduce the effect of multimorbidity on transitions out of paid employment may target working individuals regardless of these characteristics.
We found no strong evidence that the relationship between multimorbidity and the type of transition out of full-time paid employment was modified by SEP. Previous studies showed that low SEP workers often have more physically or mentally demanding jobs (Burgard & Lin, 2013), more difficulty coping with their CHCs (Sloan et al., 2009), a lower adherence to prescribed medication, (Wamala et al., 2007) an unhealthier lifestyle (Govil et al., 2009), and it may be more difficult for them to access health care than for workers with a high SEP (Vart et al., 2015). Yet, in our study, this did not lead to a modification of the risk for leaving full-time paid employment in the context of multimorbidity. SEP measured as wealth was in itself associated with an increased risk for the transition from full-time paid employment into disability, unemployment, and with a decreased risk to partly or fully retire. SEP measured as low educational level was also associated with a decreased risk to partly retire and an increased risk for the transition to disability but also with an increased risk for the transition to economic inactivity and full retirement. These findings are in line with studies showing that low SEP increases the likelihood to transition from paid employment to unemployment, disability pension, and economic inactivity (Schuring et al., 2013). Previous studies also suggest that low SEP is related to multimorbidity (Barnett et al., 2012, Tucker-Seeley et al., 2011). Thus, low SEP is an important factor for developing multimorbidity and for the transition out of full-time paid employment, but low SEP does not modify the association between multimorbidity and transitions out of full-time paid employment. Future studies should further examine the possible modifying role of SEP using additional modeling strategies like square terms, other polynomials, or three-way interactions.
In the current study, we focused on workers in full-time paid employment at baseline and investigated their transition out of this employment status. This could imply that our study sample is a selection of relatively healthy older workers. Those with the poorest health may already have transitioned to another employment status from full-time paid employment. This suggests that the observed associations between multimorbidity and transition out of full-time employment may represent an underestimate of the true effects. This potential bias can be addressed in future studies by following working-age adults from a much younger age, prior to the development of CHCs, to obtain a more accurate assessment of the effect of CHCs, and multimorbidity in particular, on labor market transitions. By including only full-time workers, we excluded part-time workers whom contribute valuably to the workforce. However, combining full-time and part-time workers at baseline could dilute the effect of multimorbidity on the transition from paid employment to another employment status because of differences in the routes for leaving full-time and part-time employment. Full-time workers may still have the option to transition into part-time employment whereas part-time workers do not have that option. In addition, only 10% of the participants excluded based on their work status were working part-time.
This study has a number of notable strengths. First, the HRS is a nationally representative cohort study for adults aged more than 50 years (Sonnega et al., 2014). Therefore, our results are likely to be generalizable to the U.S. population aged 50–64 years in full-time paid employment. Caution is still warranted as we might have included a relatively healthy group of older workers. Second, our analytic approach based on prospective data minimizes the possibility of reverse causation between multimorbidity and exits from full-time paid employment, though other studies suggest that exiting paid employment by itself may increase the risk for CHCs (Dupre, George, Liu, & Peterson, 2012). Third, the modifying role of SEP on the relationship between multimorbidity and the type of transition out of full-time paid employment was assessed using two different indicators for SEP (i.e., wealth and educational level). This approach showed that findings regarding SEP were robust. Fourth, the application of the Fine and Gray competing-risks survival regression model is relatively new in the field of work and health, while it is important to account for competing outcomes when examining transitions in employment status (Reeuwijk et al., 2017). Fifth, we took into account that workers could develop multimorbidity during follow-up. Finally, although it may be intuitive to assume that multimorbidity increases the risk to transition out of full-time paid employment, this is the first study that supports this assumption by evidence, and shows that SEP does not modify this risk.
This study also has some limitations. First, multimorbidity and the type of transition out of full-time paid employment were based on self-reports. Although previous research has shown that patient’s self-reports on CHCs compared to data from general practitioners are fairly accurate, some degree of information bias may be present due to over- or underreporting of CHCs and may thus have influenced our findings (Kriegsman, Penninx, van Eijk, Boeke, & Deeg, 1996). More objective measures regarding CHCs (e.g., blood markers for T2DM) and labor market transitions obtained from national registers could have strengthened our study. Second, we did not have information on specific work and employment characteristics, which could provide insight into barriers and facilitators for staying in full-time paid employment in the context of multimorbidity. Third, we could not take into account whether participants received proper treatment for their CHCs. Receiving proper treatment for CHCs may buffer the detrimental consequences of multimorbidity. However, a sensitivity analysis in which we adjusted our main analyses for insurance status as a crude indicator for receiving treatment did not change our results.
The findings of this study have some important implications for health care professionals and policy makers. Population aging is currently forcing countries to stimulate their citizens to extend their working lives (Harper, 2014; Organisation for Economic Co-operation and Development, 2015). Although prevention of multimorbidity could help to achieve the policy goal of extending working lives, the focus of health care professionals and policy makers should also be on retaining workers with one CHC or multimorbidity in the workforce. Individuals with multimorbidity may need special attention regarding personalized work accommodations to be retained in the workforce. Workers with a low SEP may deserve special attention because they are more likely to leave the workforce than their high-SEP counterparts. In addition, their general physical and mental health status tends to be lower than that of high SEP workers and their functional health status tends to decline at a faster rate before retirement (Chandola, Ferrie, Sacker, & Marmot, 2007; van Zon, Bultmann, Reijneveld, & de Leon, 2016).
Findings from this study also have important implications for researchers. First, future studies should investigate transitions over a longer work-life trajectory from full-time or part-time employment to full retirement, using sequence analyses, for example. Such studies may elucidate how multimorbidity affects the labor market participation of people that are not in full-time employment. In addition, future studies should take labor market developments and occupational type into account (Amick, McLeod, & Bültmann, 2016). It would also be valuable to identify which work characteristics are barriers and facilitators for workers with multimorbidity in staying in full-time paid employment to better understand the mechanisms behind the different transitions. Furthermore, contextual factors like the work role of a spouse could influence if, and how, workers with multimorbidity exit full-time paid employment. Future studies should further elucidate the role of such contextual factors. Future studies should also examine whether specific combinations of CHCs are more detrimental than others regarding the risk of leaving full-time paid employment, and whether some single CHCs (e.g., stroke) are comparably impactful as combinations of other CHCs (e.g., hypertension and diabetes). Examining the role of disease severity is an additional topic for further research.
We conclude that compared to having no CHC, multimorbidity increases the risk of transitioning from full-time paid employment to disability, partial and full retirement, and the risk of dying. Compared to having one CHC, multimorbidity increases the risk of transitioning from full-time paid employment to partial and full retirement and the risk of dying. To help workers with multimorbidity stay in full-time or part-time paid employment, personalized work accommodations seem necessary. Although low SEP in itself is an important factor for the transition out of full-time paid employment, we found no strong evidence that SEP modifies the relationship between multimorbidity and the type of transition from full-time paid employment to another employment status.
Supplementary Material
Funding
The Health and Retirement Study is sponsored by the National Institute on Aging (grant number NIA U01AG009740). This work did not receive specific funding; all authors were funded by their respective institutes.
Author Contributions
S. K. R. van Zon, S. A. Reijneveld, A. Galaurchi, J. Almansa, and U. Bültmann conceived and designed the study. S. K. R. van Zon and J. Almansa analyzed the data. S. K. R. van Zon, S. A. Reijneveld, C. F. Mendes de Leon, J. Almansa, and U. Bültmann were involved in interpreting the data. All authors critically revised the manuscript, read, and approved the final manuscript.
Conflict of Interest
None reported.
References
- van den Akker M., Buntinx F., & Knottnerus J. A (1996). Comorbidity or multimorbidity: What’s in a name? A review of literature. European Journal of General Practice, 2, 65–70. doi:10.3109/13814789609162146 [Google Scholar]
- van den Akker M., Buntinx F., Metsemakers J. F., Roos S., & Knottnerus J. A (1998). Multimorbidity in general practice: Prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. Journal of Clinical Epidemiology, 51, 367–375. doi:S0895-4356(97)00306-5 [DOI] [PubMed] [Google Scholar]
- Amick B. C., McLeod C. B., & Bültmann U (2016). Labor markets and health: An integrated life course perspective. Scandinavian Journal of Work, Environment & Health, 42, 346–353. doi:10.5271/sjweh.3567 [DOI] [PubMed] [Google Scholar]
- Barnett K., Mercer S. W., Norbury M., Watt G., Wyke S., & Guthrie B (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet (London, England), 380, 37–43. doi:10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- de Boer A. G. E. M., Geuskens G. A., Bültmann U., Boot C. R. L., Wind H., Koppes L. L. J., & Frings-Dresen M. H. W (2018). Employment status transitions in employees with and without chronic disease in the Netherlands. International Journal of Public Health, 63, 713–722. doi:10.1007/s00038-018-1120-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bøje C. R. (2014). Impact of comorbidity on treatment outcome in head and neck squamous cell carcinoma—A systematic review. Radiotherapy and Oncology, 110, 81–90. doi:10.1016/j.radonc.2013.07.005 [DOI] [PubMed] [Google Scholar]
- Bowling A. (1995). What things are important in people’s lives? A survey of the public’s judgements to inform scales of health related quality of life. Social science & medicine (1982), 41, 1447–1462. doi:10.1016/0277-9536(95)00113-L [DOI] [PubMed] [Google Scholar]
- Breton M. C., Guénette L., Amiche M. A., Kayibanda J. F., Grégoire J. P., & Moisan J (2013). Burden of diabetes on the ability to work: A systematic review. Diabetes Care, 36, 740–749. doi:10.2337/dc12-0354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugliari D., Campbell N., Chan C., Hayden O., Hurd M., Main R., . . . St.Clair P (2016). RAND HRS data documentation, version P. Santa Monica, CA: Labor & Population Program RAND Center for the Study of Aging. [Google Scholar]
- Burgard S. A., & Lin K. Y (2013). Bad jobs, bad health? How work and working conditions contribute to health disparities. American Behavioral Scientist, 57, 1105–1127. doi:10.1177/0002764213487347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlsen K., Oksbjerg Dalton S., Frederiksen K., Diderichsen F., & Johansen C (2008). Cancer and the risk for taking early retirement pension: A Danish cohort study. Scandinavian Journal of Public Health, 36, 117–125. doi:10.1177/1403494807085192 [DOI] [PubMed] [Google Scholar]
- Chandola T., Ferrie J., Sacker A., & Marmot M (2007). Social inequalities in self reported health in early old age: Follow-up of prospective cohort study. BMJ (Clinical Research Ed.), 334, 990. doi:bmj.39167.439792.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre M. E., George L. K., Liu G., & Peterson E. D (2012). The cumulative effect of unemployment on risks for acute myocardial infarction. Archives of Internal Medicine, 172, 1731–1737. doi:10.1001/2013.jamainternmed.447 [DOI] [PubMed] [Google Scholar]
- Fine J. P., & Gray R. J (1999). A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association. 94, 496–509. doi:10.2307/2670170 [Google Scholar]
- Govil S. R., Weidner G., Merritt-Worden T., & Ornish D (2009). Socioeconomic status and improvements in lifestyle, coronary risk factors, and quality of life: The Multisite Cardiac Lifestyle Intervention Program. American Journal of Public Health, 99, 1263–1270. doi:10.2105/AJPH.2007.132852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S. (2014). Economic and social implications of aging societies. Science (New York, N.Y.), 346, 587–591. doi:10.1126/science.1254405 [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. (2016). RAND Contributed Files (v.P) public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI: RAND Center for the Study of Aging. [Google Scholar]
- Kjær T., Bøje C. R., Olsen M. H., Overgaard J., Johansen J., Ibfelt E., . . . Dalton S. O (2013). Affiliation to the work market after curative treatment of head-and-neck cancer: A population-based study from the DAHANCA database. Acta oncologica (Stockholm, Sweden), 52, 430–439. doi:10.3109/0284186X.2012.746469 [DOI] [PubMed] [Google Scholar]
- Kouwenhoven-Pasmooij T. A., Burdorf A., Roos-Hesselink J. W., Hunink M. G., & Robroek S. J (2016). Cardiovascular disease, diabetes and early exit from paid employment in Europe; the impact of work-related factors. International Journal of Cardiology, 215, 332–337. doi:10.1016/j.ijcard.2016.04.090 [DOI] [PubMed] [Google Scholar]
- Kriegsman D. M., Penninx B. W., van Eijk J. T., Boeke A. J., & Deeg D. J (1996). Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. Journal of Clinical Epidemiology, 49, 1407–1417. doi:10.1016/S0895-4356(96)00274-0 [DOI] [PubMed] [Google Scholar]
- Link B. G., & Phelan J (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, Spec No. 80–94. Extra Issue: Forty Years of Medical Sociology: The State of the Art and Directions for the Future. doi:10.2307/2626958 [PubMed] [Google Scholar]
- Mackenbach J. P., Stirbu I., Roskam A. J., Schaap M. M., Menvielle G., Leinsalu M., . . . Kunst A. E.; European Union Working Group on Socioeconomic Inequalities in Health (2008). Socioeconomic inequalities in health in 22 European countries. New England Journal of Medicine, 358, 2468–2481. doi:10.1056/NEJMsa0707519 [DOI] [PubMed] [Google Scholar]
- McKee-Ryan F., Song Z., Wanberg C. R., & Kinicki A. J (2005). Psychological and physical well-being during unemployment: A meta-analytic study. Journal of Applied Psychology, 90, 53–76. doi:10.1037/0021-9010.90.1.53 [DOI] [PubMed] [Google Scholar]
- Murray C. J., Vos T., Lozano R., Naghavi M., Flaxman A. D., Michaud C., . . . Memish Z. A (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England), 380, 2197–2223. doi:10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development (2014). Ageing and employment policies: Netherlands 2014: Working better with age. Paris, France: OECD Publishing. Retrieved from http://dx.doi.org/10.1787/9789264208155-en. Accessed December 14, 2017. [Google Scholar]
- Organisation for Economic Co-operation and Development (2015). Pensions at a glance 2015: OECD and G20 indicators. Paris, France: OECD Publishing. Retrieved from http://dx.doi.org/10.1787/pension_glance-2015-en. Accessed March 30, 2017. [Google Scholar]
- Reeuwijk K. G., van Klaveren D., van Rijn R. M., Burdorf A., & Robroek S. J (2017). The influence of poor health on competing exit routes from paid employment among older workers in 11 European countries. Scandinavian Journal of Work, Environment & Health, 43, 24–33. doi:10.5271/sjweh.3601 [DOI] [PubMed] [Google Scholar]
- Robroek S. J., Schuring M., Croezen S., Stattin M., & Burdorf A (2013). Poor health, unhealthy behaviors, and unfavorable work characteristics influence pathways of exit from paid employment among older workers in Europe: A four year follow-up study. Scandinavian Journal of Work, Environment & Health, 39, 125–133. doi:10.5271/sjweh.3319 [DOI] [PubMed] [Google Scholar]
- Schuring M., Robroek S. J., Otten F. W., Arts C. H., & Burdorf A (2013). The effect of ill health and socioeconomic status on labor force exit and re-employment: A prospective study with ten years follow-up in the Netherlands. Scandinavian Journal of Work, Environment & Health, 39, 134–143. doi:10.5271/sjweh.3321 [DOI] [PubMed] [Google Scholar]
- Sin D. D., Stafinski T., Ng Y. C., Bell N. R., & Jacobs P (2002). The impact of chronic obstructive pulmonary disease on work loss in the United States. American Journal of Respiratory and Critical Care Medicine, 165, 704–707. doi:10.1164/ajrccm.165.5.2104055 [DOI] [PubMed] [Google Scholar]
- Sloan F. A., Padrón N. A., & Platt A. C (2009). Preferences, beliefs, and self-management of diabetes. Health Services Research, 44, 1068–1087. doi:10.1111/j.1475-6773.2009.00957.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P., Chen C., Mustard C., Bielecky A., Beaton D., & Ibrahim S. (2014). Examining the relationship between chronic conditions, multi-morbidity and labour market participation in canada: 2000–2005. Ageing & Society, 34, 1730–1748. doi:10.1017/S0144686X13000457 [Google Scholar]
- Sonnega A., Faul J. D., Ofstedal M. B., Langa K. M., Phillips J. W., & Weir D. R (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43, 576–585. doi:10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata survival analysis reference manual release 15. College Station, TX: Stata Press. [Google Scholar]
- Tucker-Seeley R. D., Li Y., Sorensen G., & Subramanian S. V (2011). Lifecourse socioeconomic circumstances and multimorbidity among older adults. BMC Public Health, 11, 313. doi:10.1186/1471-2458-11-313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ubalde-Lopez M., Arends I., Almansa J., Delclos G. L., Gimeno D., & Bültmann U (2017). Beyond return to work: The effect of multimorbidity on work functioning trajectories after sick leave due to common mental disorders. Journal of Occupational Rehabilitation, 27, 210–217. doi:10.1007/s10926-016-9647-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ubalde-Lopez M., Delclos G. L., Benavides F. G., Calvo-Bonacho E., & Gimeno D (2016). Measuring multimorbidity in a working population: The effect on incident sickness absence. International Archives of Occupational and Environmental Health, 89, 667–678. doi:10.1007/s00420-015-1104-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uijen A. A., & van de Lisdonk E. H (2008). Multimorbidity in primary care: Prevalence and trend over the last 20 years. European Journal of General Practice, 14(Suppl 1), 28–32. doi:10.1080/13814780802436093 [DOI] [PubMed] [Google Scholar]
- Vart P., Gansevoort R. T., Crews D. C., Reijneveld S. A., & Bültmann U (2015). Mediators of the association between low socioeconomic status and chronic kidney disease in the United States. American Journal of Epidemiology, 181, 385–396. doi:10.1093/aje/kwu316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wamala S., Merlo J., Bostrom G., Hogstedt C., & Agren G (2007). Socioeconomic disadvantage and primary non-adherence with medication in Sweden. International Journal for Quality in Health Care, 19, 134–140. doi:mzm011 [DOI] [PubMed] [Google Scholar]
- Ward B. W., & Schiller J. S (2013). Prevalence of multiple chronic conditions among US adults: Estimates from the National Health Interview Survey, 2010. Preventing Chronic Disease, 10, E65. doi:10.5888/pcd10.120203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff J. L., Starfield B., & Anderson G (2002). Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of Internal Medicine, 162, 2269–2276. doi:ioi20083 [DOI] [PubMed] [Google Scholar]
- van Zon S. K., Bultmann U., Reijneveld S. A., & de Leon C. F (2016). Functional health decline before and after retirement: A longitudinal analysis of the Health and Retirement Study. Social Science & Medicine, 170, 26–34. doi:S0277-9536(16)30561-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.