Abstract
Introduction
The correlation between inflammation and vascular disease is widely accepted. High levels of C-reactive protein (CRP) have been shown to play a role in the process of endothelial dysfunction. Hypertension is described as an inflammatory vascular disease, and is 1 of the most commonly encountered diseases in the outpatient setting. We studied the association between the elevated high sensitivity-CRP (hs-CRP) level and hypertension, as well as other comorbid conditions.
Methods
Electronic medical records of 169 adult patients in our internal medicine office were reviewed for hs-CRP levels, and divided into 2 groups: elevated hs-CRP (≥2 mg/L; n = 110) and normal hs-CRP (<2 mg/L; n = 59). Independent T-Test was used to compare the means of continuous variables between the groups if they were normally distributed. Mann Whitney U-Test was used to compare the continuous variables that were non-parametric. Logistic regression was used to compare the dependent and independent variables.
Results
Among subjects with elevated hs-CRP, 58.2% had hypertension while 47.5% of subjects with normal hs-CRP levels had hypertension (P = .182). There were higher frequencies of association of coronary artery disease (CAD), cerebrovascular disease and hypothyroidism in elevated hs-CRP group but the differences were not statistically significant. Mean white blood cell count was statistically higher in elevated hs-CRP group (P < .05), while alcohol use was significantly higher (P < .05) and statin use was higher in the normal hs-CRP group. There was an inverse relationship between HDL-C and hs-CRP.
Conclusions
There was no statistically significant correlation between hs-CRP level and hypertension. Hs-CRP has statistically significant associations between alcohol use, dementia, white blood cell count, and HDL levels. Promising but not statistically significant correlations were observed between hs-CRP and statin therapy, hypothyroidism, coronary artery disease, and cerebrovascular disease.
Keywords: hypertension, high sensitivity C-reactive protein (hs-CRP), inflammation
Introduction
Hypertension is a prevalent and growing public health problem that is managed in the primary care setting on a regular basis. Forty-six percent of the U.S. adult population is affected by hypertension. Hypertension is a major risk factor for stroke, cardiovascular disease, and other vascular diseases. Despite current medical therapies, hypertension remains a prevalent cardiac, renal, and cerebrovascular risk factor.1
As per the current hypertension guidelines, hypertension is diagnosed as a measurement of systolic blood pressure of 130 mmHg, or greater, and/or diastolic pressure of 80 mmHg, or greater. The guidelines goal systolic blood pressure is below 120 mmHg and diastolic blood pressure is below 80 mmHg.2
Hypertension, smoking, diabetes, and hyperlipidemia, are all risk factors for development of cardiovascular diseases. There is ample evidence that reduction of these risk factors results in improved cardiovascular morbidity and mortality. However, these risk factors are not present in up to half of the patients with clinical manifestations of cardiovascular disease.3 Hence, identification of other modifiable cardiovascular risk factors in persons without an overt diagnosis of hypertension may allow for further interventions to prevent development of hypertension and cardiovascular events.
Hypertension is an inflammatory disease that is triggered by angiotensin II.4,5 Angiotensin II triggers an inflammatory response which increases vascular permeability, cause migration and adhesion of inflammatory markers, increases levels of VEG-F causing proliferation of vasculature, and increases levels of endothelin causing stiffening of vasculature.4 As it is an inflammatory process, studies postulate that measurement of high-sensitive C-reactive protein (hs-CRP) may be a marker for early development of hypertension. Remodeling of the vasculature causes arterial stiffness and leads to progression of hypertension.6-8 Inflammatory markers, specifically hs-CRP levels, have correlated with high systolic and diastolic pressures.1,5
The purpose of our retrospective study was to investigate the correlation between hs-CRP levels and hypertension in clinical practice. Based on the available studies it appears that early detection and initiation of anti-hypertensive agents at the onset of elevated hs-CRP in patients that have not yet met the clinical criteria for hypertension may help prevent the progression of the inflammatory response and prevent the development of further vascular complications.7-9 We hypothesized that elevated hs-CRP levels would be associated with hypertension.
Methodology
Study Sample
We reviewed electronic medical records of the patients 18 years and older who had hs-CRP levels completed between January 1, 2019 and December 31, 2019 at a single primary care practice ran by a sole provider. Given that the number of patients in our study who had hs-CRP tests, were not as high as expected, we conducted a population study in which we examined 420 patients as per the recommended sample size of the full population, and selected 169 patients who fit within the study inclusion criteria. The study was approved by the Institutional Review Board (IRB). As our study was a retrospective review of patients’ medical records, informed consent was not required by the IRB.
Data Collection
For each patient we gathered the following data: age (years), gender, race, (non-Hispanic Caucasian/ African American/Asian/Hispanic/other), social history (tobacco use, alcohol use, recreational drug use), family history of illness (dementia, mild cognitive impairment, cognitive impairment), associated medical conditions, such as hypertension, diabetes mellitus, hyperlipidemia, hypothyroidism, coronary artery disease, cerebrovascular accident, peripheral arterial disease, carotid artery stenosis, congestive heart failure, arthritis and other rheumatologic disorders, mental health disorder, chronic obstructive pulmonary disease, asthma, chronic kidney disease, liver disease, colorectal disorder, immunocompromised host, medication use (aspirin/non-steroidal anti-inflammatory drugs, statin, steroid, and immunosuppressive agents), and other parameters, such as systolic and diastolic blood pressures, hs-CRP (elevated hs-CRP ≥2 mg/L, or normal hs-CRP <2 mg/L), white blood cell count, erythrocyte sedimentation rate, antinuclear antibody, rheumatoid factor, total cholesterol, low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), and triglyceride levels.
Statistical Study
We entered all collected data into a Microsoft Excel (2019, Redmond, Washington, USA) spreadsheet. We performed statistical analysis by using SPSS (Statistical Package for the Social Sciences, version 20, IBM, Armonk, New York, USA). As our study was a population study we looked to obtain all patients during our set time period that met our inclusion criteria. There were 169 patients of 420 patients who had an hs-CRP test during the study period that met our inclusion criteria. The IRB accepted our sample size, and our study progressed as planned.
The tests that were used to determine the distribution of the data were the Shapiro Wilk test and the test of skewness. There was no power analysis completed as the full population of those who fit the inclusion criteria was used. Independent t-test compared the means of continuous variables between the study groups if they were normally distributed. The Mann-Whitney U-test was used to compare the continuous variables that were non-parametric. A discriminant function analysis was done which showed that the model is not significant in that the variables in the model, including systolic blood pressure, diastolic blood pressure, body mass index, total cholesterol, triglyceride, and white blood cell count, are not significant discriminators between normal and elevated hs-CRP. Logistic regression was also used which verified that none of the above mentioned variables were shown to be significant. The dependent variable was hypertension. The independent variable of interest was hs-CRP level, which was dichotomized to be labeled “high” versus “normal”. Other independent variables that were used in the model were age, body mass index, sex, race, history of recreational drug use, diabetes mellitus, chronic obstructive pulmonary disease, and asthma.
Results
A total of 169 patient medical records were included. Among them, 110 (65.0%) patients had elevated hs-CRP levels and 59 (34.9%) patients had normal hs-CRP levels. The age range of patients with hs-CRP levels in our study was 38 to 70 years. The majority of the patients with hs-CRP levels were in the 50 to 53 years of age range. The mean age of the patients with elevated hs-CRP levels was 57.9 + 16.1 years and the mean age of the patients with normal hs-CRP levels was 53.9 years + 16.8. There was no statistically significant difference in the mean ages between the 2 groups (Table 1). We found that for every increased year of age, there was 1.1 times greater odds of having hypertension (95% CI 1.02-1.09). Gender analysis revealed a higher frequency of female patients with elevated and normal hs-CRP levels compared to males but the difference was not statistically significant. There were 63.3% females with high hs-CRP levels compared to 36.4% of males and 54.2% females with normal hs-CRP levels compared to 45.8% of males (P = .234; Table 1). We found that men had 2.7 times greater odds of having hypertension (95% CI 1.2-6.2).
Table 1.
Population Characteristics.
| Variable | High hs-CRP (n = 110) | Normal hs-CRP (n = 59) | P-value |
|---|---|---|---|
| Age | |||
| Mean (SD) | 57.89 (16.07) | 53.97 (16.76) | .138* |
| Gender | |||
| Male (n, %) | 40 (36.4) | 27 (45.8) | .234** |
| Female (n, %) | 70 (63.3) | 32 (54.2) | |
| Race | |||
| Caucasian (n, %) | 66 (60.0) | 40 (67.8) | .557** |
| African American (n, %) | 28 (25.5) | 11 (18.6) | |
| Other (n, %) | 16 (14.5) | 8 (13.6) | |
| Social factors | |||
| Alcohol (n, %) | 31 (28.2) | 28 (47.5) | .012** |
| Cigarettes (n, %) | 46 (41.8) | 25 (42.4) | .944** |
| Illicit drug use (n, %) | 17 (15.5) | 9 (15.3) | .973** |
| Family Hx of illness | |||
| Dementia (n, %) | 0 (0.0) | 3 (5.1) | .041** |
| Mild cognitive impairment (n, %) | 1 (0.9) | 0 (0.0) | 1.000** |
| Cognitive impairment (n, %) | 0 (0.0) | 0 (0.0) | No incidence |
Abbreviation: SD, standard deviation.
Independent t-Test. **Chi-squared test.
The analysis of race showed that the majority of the patients in both groups were Caucasian (60% in High hs-CRP group, and 67.8% in normal hs-CRP group), followed by African American (25.5% in high hs-CRP group, 18.6% in normal hs-CRP group), and other races (14.5% in high hs-CRP group, 13.6% in normal hs-CRP group; Table 1). These differences were not statistically significant.
We found that 47.5% of patients with normal CRP levels used alcohol, and 28% of patients with high CRP levels used alcohol. The difference was statistically significant (P < .05). We also found that 42.4% of patients with normal hs-CRP levels smoked cigarettes, where as 41.8% of people with high hs-CRP smoked cigarettes. Illicit drug use was equally present in the high hs-CRP level group and normal hs-CRP group as 15%. Neither of these differences regarding smoking cigarettes or illicit drug use were statistically significant (Table 1). There was a higher association of dementia in patients with normal hs-CRP levels compared to the patients with high hs-CRP (5.5% vs. 0.0%). Likewise, there was a higher association seen with mild cognitive impairment and high hs-CRP levels but the number of patients was too small (Table 1).
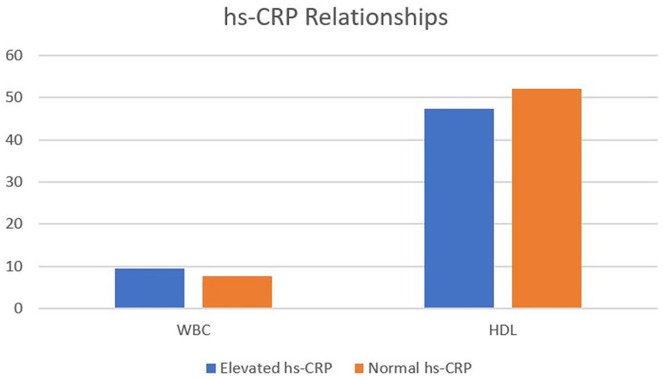
Analysis of vital parameters and diagnostic tests showed that the mean body mass index (BMI) of patients with high hs-CRP levels was lower at 26.9 kg/m2 compared to 27.9 kg/m2 in the normal hs-CRP group; however this was not statistically significant (Table 2). There was no statistical significant difference seen in systolic blood pressure or diastolic blood pressure between the 2 groups (Table 2). However, lipid analysis showed a higher mean level of HDL cholesterol level in the normal hs-CRP group (53.66 mg/dL) compared to the high hs-CRP group (47.56 mg/dL) (P = .050; Figure 1 and Table 2). There was no statistically significant difference in the mean levels of total cholesterol, LDL cholesterol, and triglycerides between the groups. We also discovered that the mean white blood cell count was higher in the high hs-CRP group compared to the normal hs-CRP group (8.9 × 109/L vs 7.6 × 109/L; P < .05; Figure 1 and Table 2).
Table 2.
Vitals and Diagnostic Tests.
| Variable | High hs-CRP (n = 110) | Normal hs-CRP (n = 59) | P-value* |
|---|---|---|---|
| Systolic blood pressure (mmHg) (mean, SD) | 131.65 (20.88) | 132.88 (17.04) | .679 |
| Diastolic blood pressure (mmHg) (mean, SD) | 74.46 (12.31) | 76.83 (12.95) | .244 |
| Body mass index (kg/m2) (mean, SD) | 26.99 (7.68) | 27.97 (5.41) | .384 |
| Total cholesterol (mg/dL) (mean, SD) | 162.06 (51.01) | 174.42 (41.65) | .160 |
| LDL cholesterol (mg/dL) (mean, SD) | 88.92 (38.70) | 95.06 (34.40) | .373 |
| HDL cholesterol (mg/dL) (mean, SD) | 47.56 (16.24) | 53.66 (17.36) | .050 |
| Triglyceride (mg/dL) (mean, SD) | 130.54 (89.45) | 124.06 (75.23) | .655 |
| White blood cell count (mean, SD) | 8.97 (4.42) | 7.60 (3.82) | .045 |
Abbreviations: LDL, low density lipoprotein; HDL, high density lipoprotein; SD, standard deviation.
Independent t-test.
Figure 1.
Relationship between hs-CRP levels and common diagnostic test parameters.
In regards to the medication use, we found no significant difference between the 2 groups in use of aspirin, non-steroidal anti-inflammatory drugs, steroids, or immunosuppressive agents. However, a higher percentage of statin users were seen in the normal hs-CRP group (35.6%) compared to 19.1% seen in the elevated hs-CRP group (P = .053; Table 3).
Table 3.
Medication Usage.
| Variable | High hs-CRP (n = 110) | Normal hs-CRP (n = 59) | P-value* |
|---|---|---|---|
| Aspirin (n, %) | 30 (27.3) | 14 (23.7) | .617 |
| Non-steroidal anti-inflammatory drugs (n, %) | 14 (12.7) | 9 (15.3) | .648 |
| Statin (n, %) | 21 (19.1) | 21 (35.6) | .053 |
| Steroid (n, %) | 12 (10.9) | 7 (11.9) | .851 |
| Immunosuppressive agents (n, %) | 5 (4.5) | 2 (3.4) | 1.000 |
Chi-squared test.
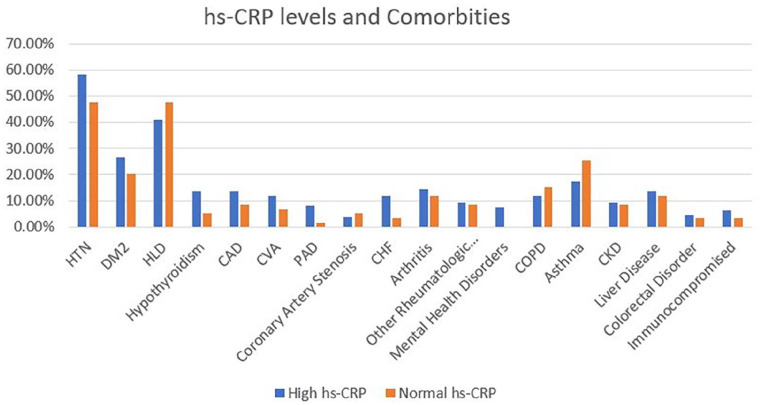
Analysis of comorbid medical conditions showed a higher association of hypertension in the subjects with elevated hs-CRP (58.2%) compared to 47.5% of subjects in the normal hs-CRP group, but the difference was not statistically significant (P = .182; Figure 2 and Table 4). Among patients with elevated hs-CRP levels 13.6% had coronary artery disease while only 8.5% of patients with normal hs-CRP levels had CAD (P = .322; Table 4). Similarly, 13.6% of people with elevated hs-CRP values had hypothyroidism whereas 5.1% of the patients with normal hs-CRP values had hypothyroidism. This finding was not statistically significant (P = .086; Table 4).
Figure 2.
Relationship between hs-CRP levels and common comorbid conditions.
Table 4.
Associated Medical Conditions.
| Variable | High hs-CRP (n = 110) | Normal hs-CRP (n = 59) | P-value* |
|---|---|---|---|
| Hypertension (n, %) | 64 (58.2) | 28 (47.5) | .182 |
| Diabetes mellitus (n, %) | 29 (26.4) | 12 (20.3) | .384 |
| Hyperlipidemia (n, %) | 45 (40.9) | 28 (47.5) | .413 |
| Hypothyroidism (n, %) | 15 (13.6) | 3 (5.1) | .086 |
| Coronary artery disease (n, %) | 15 (13.6) | 5 (8.5) | .322 |
| Cerebrovascular accident (n, %) | 13 (11.8) | 4 (6.8) | .299 |
| Peripheral arterial disease (n, %) | 9 (8.2) | 1 (1.7) | .088 |
| Carotid artery stenosis (n, %) | 4 (3.6) | 3 (5.1) | .696 |
| Congestive heart failure (n, %) | 13 (11.8) | 2 (3.4) | .066 |
| Arthritis (n, %) | 16 (14.5) | 7 (11.9) | .628 |
| Other rheumatologic disorders (n, %) | 10 (9.1) | 5 (8.5) | .089 |
| Mental health disorder (n, %) | 8 (7.3) | 0 (0.0) | .520 |
| Chronic obstructive pulmonary disease (n, %) | 13 (11.8) | 9 (15.3) | .527 |
| Asthma (n, %) | 19 (17.3) | 15 (25.4) | .208 |
| Chronic kidney disease (n, %) | 10 (9.1) | 5 (8.5) | .893 |
| Liver disease (n, %) | 15 (13.6) | 7 (11.9) | .744 |
| Colorectal disorder (n, %) | 5 (4.5) | 2 (3.4) | 1.000 |
| Immunocompromised host (n, %) | 7 (6.4) | 2 (3.4) | .498 |
Chi-squared test.
The association of cerebrovascular accident was higher (11.8%) in the patients with elevated hs-CRP levels compared to 6.8% patients with normal hs-CRP levels, the difference was not statistically significant (P = .299; Table 4). There was no statistically significant difference between the 2 groups in the association of other comorbid conditions, such as diabetes mellitus, hyperlipidemia, peripheral arterial disease, carotid artery stenosis, congestive heart failure, arthritis, other rheumatologic disorders, mental health disorder, chronic obstructive pulmonary disease, asthma, chronic kidney disease, liver disease, colorectal disorder, and immunocompromised host. We found that subjects with diabetes had 4.3 times greater odds of having hypertension (95% CI 1.6-11.6), while those with asthma had 6.3 times greater odds of having hypertension (95% CI 2.1-18.7).
Discussion
While we did not find a statistically significant correlation between hs-CRP and hypertension further studies may be necessary to truly evaluate the correlation between these 2 variables. Harrison et al4 supported a role of inflammation and immunity in hypertension and cardiovascular disease in their review of the relationship between inflammation, immunity, and hypertension. The proposed mechanism includes the role of T cells and inflammation in hypertension. This results in activation of the stimulants of hypertension, such as angiotensin II and sodium, resulting into modest elevation in the blood pressure which in turn leads to neo-antigen formation that promotes T cell activation which enters the kidney and blood vessels. Interleukin-17, a T cell derived signal, facilitates the recruitment of macrophages that release cytokines causing vasoconstriction, enhance sodium and water absorption, resulting into development of hypertension.4 Smith et al8 reported that hypertension caused an inflammatory response with elevated hs-CRP levels, hence elevated hs-CRP levels could have been a predictive marker for early hypertension. Other studies have either directly, or indirectly, shown similar associations.5-8 Promising but not statistically significant associations were observed between hs-CRP and statin therapy, hypothyroidism, coronary artery disease, and cerebrovascular disease. We believe that with a larger sample of subjects the difference in our study would have achieved statistical significance. Further research could be beneficial, as this would allow hs-CRP to be used as a screening tool for early detection of risk of development of hypertension. Ideally this may help physicians in the outpatient setting with managing and mitigating the risks of hypertension prior to disease onset.8
Several studies have reported that inflammation plays a role in the pathogenesis of vascular disease, coronary artery disease in particular. Habib and Al Masri9 concluded that hs-CRP could be used as a predictor for vascular changes and coronary events. Their study founds a positive correlation between hs-CRP and coronary artery disease (r = .423, P = .018).9 Another study examined the association between hs-CRP levels and severity of coronary disease, and found a strong association between the extent of disease of the coronary vessels and the level of hs-CRP.10
Statins are known to decrease low-density lipoprotein (LDL) levels, and they also have pleomorphic effects that help in the reduction of vascular disease. We found a higher association between statin therapy in subjects with normal hs-CRP levels compared to the subjects with elevated hs-CRP levels (P = .053). A study found that statin treatment was associated with lower levels of hs-CRP.11 Another study found that Simvastatin decreased hs-CRP levels significantly within 2 weeks (P = .011).12 The JUPITER study evaluated whether Rosuvastatin therapy was beneficial in patients with elevated levels of hs-CRP who did not meet routine criteria for initiation of a statin. Due to the pleomorphic effects of statins, they found that after a year of Rosuvastatin therapy, the median hs-CRP level decreased by 37%.13 We, once again, believe that with a larger sample of subjects this difference in association in our study could have achieved statistical significance.
While not statistically significant we found an association of cerebrovascular accident in subjects with elevated hs-CRP compared to subjects with normal hs-CRP levels. Liu et al14 found that elevated hs-CRP levels were associated with a higher risk of ischemic stroke. Another study demonstrated that elevated levels of hs-CRP in patients with small-artery occlusion, were a predictor of poor prognosis in patients under 75 years of age.15 In this study patients with hs-CRP levels over 2.77 mg/L were at increased risk of poor outcomes (P = .034) when compared to the patients who had normal hs-CRP levels.15 Another study found that not only elevated hs-CRP levels were significantly associated with a greater risk for stroke, but that men who were hypertensive, had elevated hs-CRP levels, and were more likely to have stroke than any other demographic group.16
Another non-statistically significant association was seen in patients with hypothyroidism and elevated hs-CRP levels. A study reported that subclinical hypothyroidism is associated with increased inflammatory markers, such as CRP, along with dyslipidemia compared to those without subclinical hypothyroidism.17 Hypothyroidism can be indirectly related to cardiovascular disease, and it has therefore been recommended that subclinical hypothyroidism be treated to reduce the risk of cardiovascular disease.17
We found a statistically significant correlation between elevated mean white blood cells in subjects with elevated hs-CRP levels compared to the subjects with normal hs-CRP levels. In concordance with our study, Ajala and Everett18 showed that vascular inflammation contributes to increased cardiovascular risk. Biomarkers such as hs-CRP have been seen to be associated with major cardiovascular events such as myocardial infarction and stroke despite having an appropriate lipid panel. With a rise in inflammatory markers comes a rise in white blood cell count as this is part of a significant inflammatory response, and thus reflects the association in our research.18
We also found an inverse relationship between high density lipoprotein cholesterol (HDL-C) and hs-CRP. Chrysohoou et al19 found that HDL-C was inversely correlated with hs-CRP (r = −.68, P = .018). Our findings suggest that HDL-C may play an anti-inflammatory role as supported by Chrysohoou et al findings.19
Interestingly, we found that subjects in the normal hs-CRP group had a significantly higher frequency of alcohol use compared to the subjects in the elevated hs-CRP group. Our findings contrast with the findings of Ojima et al20 in their study of association of risk factors for atherosclerosis, which included alcohol use as a risk factor for elevated hs-CRP and arterial disorder. Our correlation between alcohol use and normal hs-CRP represents an anti-inflammatory effect and is a unique finding, which should be further studied.
There were several limitations in our study. Being a retrospective review, the information obtained was through review of our electronic medical record, which fully depended on documentation by patient care teams. Many differences in associations were close to being statistically significant, which could have been achieved by recruiting a larger sample of subjects. One of the strengths of our study is that we further examined background factors, which may have played a role as confounding factor in the study. The other major strength of our study was the review of clinical data of our established patients in our primary care office who followed at scheduled intervals and were treated by the same care provider. This allowed us to analyze the provider specific management strategies, adherence and outcomes; as well as inclusion of a multitude of associated medical conditions that could have influenced the management outcomes.
Conclusion
Although a higher frequency of association of hypertension was observed in elevated hs-CRP group compared normal hs-CRP group, the difference in the frequencies was not statistically significant. Hs-CRP had statistically significant associations between alcohol use, white blood cell count, and HDL levels. Promising but not statistically significant associations were observed between hs-CRP and statin therapy, hypothyroidism, coronary artery disease, and cerebrovascular disease. Our study highlights the potential utilization benefits that hs-CRP levels may be able to provide physicians with when managing common medical conditions such as hypertension, coronary artery disease, cerebrovascular disease, and hypothyroidism. Hs-CRP has the potential to be used as not only a screening tool, but also as a measure of treatment efficiency. Hypertension is a significant risk factor for both cardiovascular and cerebrovascular disease. Further studies with a larger sample size would be beneficial in assessing whether hs-CRP can be used to manage hypertension as well as other critical vascular diseases.
Acknowledgments
The authors thank Christine Rickette, RN (study coordinator) for her contribution to this study.
Footnotes
Author Contributions: SB, VT, and SR made substantial contributions to the study design, drafting, data acquisition and analysis, and manuscript writing. KH analyzed the data. SR contributed in revising the manuscript critically for improved intellectual content, and final approval for the version to be published.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed Consent: Not applicable. Being a retrospective chart review study the Institutional Review Board waived the need for informed consent.
ORCID iD: Sharmila Bisaria  https://orcid.org/0000-0002-1698-0811
https://orcid.org/0000-0002-1698-0811
Data Availability: The authors declare that data supporting the findings of this study are available within the article.
References
- 1. Hage FG, Oparil S, Xing D, Chen YF, McCrory MA, Szalai AJ. C-reactive protein-mediated vascular injury requires complement. Arterioscler Thromb Vasc Biol. 2010;30:1189-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127-e248. [DOI] [PubMed] [Google Scholar]
- 3. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285:2486-2497. [DOI] [PubMed] [Google Scholar]
- 4. Harrison DG, Guzik TJ, Lob HE, et al. Inflammation, immunity, and hypertension. Hypertension. 2011;57:132-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang CH, Li SH, Weisel RD, et al. C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation. 2003;107:1783-1790. [DOI] [PubMed] [Google Scholar]
- 6. Boos C, Lip G. Elevated high-sensitive C-reactive protein, large arterial stiffness and atherosclerosis: a relationship between inflammation and hypertension? J Hum Hypertension. 2005;19:511-513. [DOI] [PubMed] [Google Scholar]
- 7. Kusche-Vihrog K, Urbanova K, Blanqué A, et al. C-reactive protein makes human endothelium stiff and tight. Hypertension. 2011;57:231-237. [DOI] [PubMed] [Google Scholar]
- 8. Smith GD, Lawlor DA, Harbord R, et al. Association of C-reactive protein with blood pressure and hypertension: life course confounding and mendelian randomization tests of causality. Arterioscler Thromb Vasc Biol. 2005;25:1051-1056. [DOI] [PubMed] [Google Scholar]
- 9. Habib SS, Al Masri AA. Relationship of high sensitivity C-reactive protein with presence and severity of coronary artery disease. Pak J Med Sci. 2013;29:1425-1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Al-Tu’maa F, Abd-Yasera Z, Al-Naffi K. Association between hs-CRP levels and the severity of coronary atherosclerosis. J Contemp Med Sci. 2016;2:42-44. [Google Scholar]
- 11. Chan AW, Bhatt DL, Chew DP, et al. Relation of inflammation and benefit of statins after percutaneous coronary interventions. Circulation. 2003;107:1750-1756. [DOI] [PubMed] [Google Scholar]
- 12. Plenge JK, Hernandez TL, Weil KM, et al. Simvastatin lowers C-reactive protein within 14 days: an effect independent of low-density lipoprotein cholesterol reduction. Circulation. 2002;106:1447-1452. [DOI] [PubMed] [Google Scholar]
- 13. Shishehbor MH, Hazen SL. Jupiter to earth: a statin helps people with normal LDL-C and high hs-CRP, but what does it mean? Cleve Clin J Med. 2009;76:37-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu Y, Wang J, Zhang L, et al. Relationship between C-reactive protein and stroke: a large prospective community based study. PLOS ONE. 2014;9:e107017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Qiu R, Gao Y, Hou D, et al. Association between hs-CRP levels and the outcomes of patients with small-artery occlusion. Front Aging Neurosci. 2016;8:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jiménez MC, Rexrode KM, Glynn RJ, Ridker PM, Gaziano JM, Sesso HD. Association between high-sensitivity C-reactive protein and total stroke by hypertensive status among men. J Am Heart Assoc. 2015;4:e002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gupta G, Sharma P, Kumar P, Itagappa M. Study on subclinical hypothyroidism and its association with various inflammatory markers. J Clin Diagn Res. 2015;9:BC04-BC06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ajala ON, Everett BM. Targeting inflammation to reduce residual cardiovascular risk. Curr Atheroscler Rep. 2020;22:66. [DOI] [PubMed] [Google Scholar]
- 19. Chrysohoou C, Pitsavos C, Skoumas J, et al. The emerging anti-inflammatory role of HDL-cholesterol, illustrated in cardiovascular disease free population; the ATTICA study. Int J Cardiol. 2007;122:29-33. [DOI] [PubMed] [Google Scholar]
- 20. Ojima S, Kubozono T, Kawasoe S, et al. Association of risk factors for atherosclerosis, including high-sensitivity C-reactive protein, with carotid intima-media thickness, plaque score, and pulse wave velocity in a male population. Hypertens Res. 2020;43:422-430. [DOI] [PubMed] [Google Scholar]