Abstract
This review aims to summarize the latest knowledge on factors, diagnosis, and treatment of pancreatic cancer, and aims to promote further research on this under-studied malignant tumor. At present, we urgently need to identify high-risk patients with precancerous diseases through screening approaches, so that medical professionals and the general public may better understand prevention strategies or early detection measures. Pancreatic cancer is a highly invasive malignant tumor with a fatal risk, mainly seen in men and older adults (60-85 years old). Pancreatic cancer is now increasingly observed in young patients. Because the disease has no early symptoms and can quickly invade surrounding tissues and organs, it is one of the deadliest cancers. With a view to identify the important factors for the development of pancreatic cancer, previous studies have found that smoking, alcohol, and chronic pancreatitis are considered high-risk factors. Recent studies have shown that abnormal metabolism of human microorganisms, blood type, and glucose and lipid levels are also important factors in the development of pancreatic cancer. Identifying early diagnosis options is an important way to improve detection and survival rates of pancreatic cancer. None of the many tumor markers associated with pancreatic cancer are highly specific, which also indicates further research is required to improve the early detection rate. Future directions in terms of treatment evaluating the relationship between the microbiology-free system and immunotherapy will bring a major breakthrough and is expected to bring exciting clinical applications in improving the life-cycle of pancreatic cancer patients.
Keywords: human microorganisms, immunotherapy, treatment, risk factors, pancreatic cancer
Introduction
Over the past few years, the incidence of the pancreatic cancer (PC) has increased. It accounts for about 2% of all cancers and is associated with 5% of cancer-related deaths.1 Most patients have no obvious symptoms during disease development and progression to advanced metastasis pancreatic, whereby tumor cells are highly invasive. Early diagnosis is difficult,2 and it has become one of the most deadly malignant tumors. Most patients eventually relapse, even after a potential radical treatment, the patient’s 5-year survival rate is only 2%-9%.3 Pancreatic ductal adenocarcinoma (PDAC) is the most common among patients with PC.1 There are some risk factors for PC, including family history, pancreatitis, and diabetes. However, at present, there are no standard programs in the world to screen patients with high risk of PC. To improve the prognosis of PC patients, we reviewed recent advances in risk factors, diagnosis and treatment of PC.
Risk Factors
Risk factors for PC are classified as non-modifiable (age, sex, area, blood group, family history and genetic susceptibility, diabetes) and modifiable (intestinal microflora, smoking, alcohol, chronic pancreatitis [CP], obesity, dietary factors, infection).
Non-Modifiable Risk Factors
Age
PC usually occurs in older adults, and it is extremely rare for young people under the age of 30 to develop the disease. Approximately 90% of newly diagnosed patients are over 55 years old, most of them between 70-80 years old.4
Sex
The incidence of PC is lower in women than in men globally. In developed countries, this gap is even more pronounced.3 It may be because the steroid levels are higher in women than in men, which may have a protective effect against PC.5 Sadr-Azodi et al. confirmed through a paired cohort study that compared with women who were not administered menopausal hormone therapy (MHT), the prevalence of pancreatic cancer could be reduced by 23% in women who were administered MHT. Further, compared with MHT administration for <1 year, MHT administration for 1-2 years can reduce the prevalence by 35%, and MHT administration for more than 3 years can reduce the prevalence by 60%.6
Area
PC incidence varies in different parts of the world. In the United States, the incidence in African Americans is higher than that of Caucasians, while Asian Americans and Pacific Islanders have the lowest incidence.7 In China, the health burden of cancer is increasing and the rate of growth in recent years is parallel to that of the world. Possibly due to differences in socioeconomic environment and lifestyle, urban morbidity and mortality in urban areas are higher than those in rural areas.8 By 2018, among the people with PC in the world, the highest incidence rate of ASR is in Europe (7.7/10 million) and North America (7.6/10 million, Oceania [6.4/10 million]). The incidence rate in Africa is the lowest, with an estimated incidence rate (2.2 per 100,000 people).9
Blood Group
The ABO blood group antigen is present on the entire surface of red blood cells. Recent studies have shown that blood group antigens affect the risk of PC.10 Among people with diabetes, people with type A, AB, or B blood group have a higher risk of developing PC than those with type O.7,11 There is some evidence indicating that type A blood group and diabetes will jointly lead to the development of PC.11,12
The mechanism may involve the regulation of the host inflammatory process related to the ABO blood group, which may be related to the promotion of cancer progression and metastasis. The gene encoding the ABO antigen may be associated with various plasma components, such as soluble intercellular adhesion molecule-1 (sICAM- 1) and tumor necrosis factor (TNF). These proteins are adhesion molecules required for immune cell recruitment, and thus mediate systemic inflammation. These studies indicate that the gene encoding the ABO blood group plays a direct role in tumorigenesis and malignancy, and is involved in tumor cell immune surveillance, cell adhesion, tumor apoptosis, and angiogenesis.11
Genetic Factors
In recent years, studies have found that PC has a clear family basis, and family history of PC greatly increases the risk of disease.13,14 Mainly caused by genetic and acquired gene mutations, over than 80% of PC are due to sporadic mutations, and a small number of cases are caused by specific genetic mutations. The risk of familial PC increases exponentially with the increase in the number of first-degree relatives15,16 Currently, chromosomal aberrations at loci13q22.1, 15q14,17,18 6p25.3, 12p11.21, 7q36.2,19 21q21.3, 5p13.1, 21q22.3, 22q13.32 and 10q26.120 have been discovered by scientists from Japan and China. In the largest genome-wide collection in Europe, 7p12, 1p36.33, 8q21.11, 17q12, and 18q21.32 were identified as new PC susceptibility chromosomal target deletions.21 Point mutations3,7 in K-RAS, CDKN2A (P16), TP53, SMAD4,22,23 BRCA2, BRCA1, STK11, PRSS1 and MMR24,25 are the most frequently involved in PC.
In PC stem cells, there are obvious epigenetic changes, mainly manifested in the process of mutations in chromatin regulatory proteins and the control of epithelial-mesenchymal transition (EMT), but these changes do not involve changes in genetic sequence. Only DNA and chromatin structure/chemical changes are involved; thus, these changes ultimately affect the overall phenotypic state of the cell. Based on these ideas, some researchers have begun to investigate whether inhibiting the process of epigenetic regulation contributes to the development of new PC therapies.26
Diabetes
Modern epidemiology has confirmed a significant increase in the risk of developing PC in people with diabetes.27 In type 1 diabetes, the risk of PC increases by 5-10 times in patients with a disease duration of more than 10 years. People with diabetes who have been diagnosed with the disease for more than 20 years are at higher risk of PC.28 Recently, a study identified 2002 cases of PC during the follow-up of 7.5 million people. Compared with patients without diabetes, patients newly diagnosed with diabetes have an almost 7-fold increased risk of PC. In these patients with PC, blood glucose and glycated hemoglobin (HbA1c) levels increased significantly 1 month before the diagnosis of diabetes. Therefore, HbA1c is expected to be a potential biomarker for predicting PC.29
Modifiable Risk Factors
Human Microflora
The human microbiota is composed of a variety of organisms, including bacteria, viruses, fungi, and protozoa.30 They play a vital role in human health and disease states. Studies have shown that the occurrence, development and prognosis of PC are closely related to the human microbiota.31,32 Specific oral, gastrointestinal and pancreatic microbes, as well as some hepatitis viruses and bile, may have potential etiological effects in the development of PC.33 The microbiota is involved in the development of cancer mainly in the following ways.
Immunomodulatory activity:. The gut microbiota triggers many natural and adaptive immune responses involved in the process of tumor formation.33-36 The innate immune system regulates microbial composition by recognizing flagellin, lipopolysaccharide (LPS), peptidoglycan, Toll-like receptor (TLR), and Nodlike receptor (NLR).37 Microbiota in the pancreas promotes pancreatic tumor cellogenesis by inducing innate immune suppression and adaptive immunosuppression.38
Microbial metabolites.: Microbial products secondary bile acids, lipoteichoic acid (LTA), and short-chain fatty acids (SCFAs) play important roles in cancer cell growth.39 Among them, LTA and secondary bile acids promote malignant transformation. LTA mainly binds to specific differentiation clusters, resulting in excessive secretion of pro-inflammatory factors.40,41 Secondary bile acids promote abnormal cell proliferation42 and cellular DNA damage43 by activating G-protein coupled receptor 1 (GPBAR1). In terms of anti-inflammatory and anti-cancer effects, SCFA can exhibit the opposite effect of LTA and secondary bile acids by promoting Treg-mediated immune regulation.44-46 Metabolites produced by intestinal microbes cause PDAC by traveling and acting on pancreatic cells. The specific mechanism has not been elucidated.47
Microbiota dysbiosis.: Dysregulation of the human microbial system leads to reduced microbial diversity in the intestine and other organs in the body. Its occurrence is related to host gene mutations and ultimately affects the normal immune system in the body.30,48 The normal microbial system in the body can be affected by factors such as diet, infectious diseases, sex, genetics hormones, and bile acids.49,50 Recent studies have shown that mediators secreted by the pancreatic acinus shape the gut microbiota and intestinal immunity.51 After continuous intake of antibiotics, researchers induced microbial disorders in mice and found that the incidence of various extraintestinal tumors including PC was found to be significantly elevated.52 A growing body of evidence suggests that microbial dysbiosis is associated with susceptibility, occurrence and prognosis of PDAC.
Association of microbial toxins and virulence.: Certain bacterial toxins can cause chronic inflammation, and can also destroy cellular DNA and cause cancerogenesis through autotoxins.30 For example, cytotoxins such as aflatoxin, mycotoxins, and colicin are involved in carcinogenesis and damage host cell DNA.30,53
Compared with a healthy control group, patients with PDAC have microflora changes in different parts of the body, divided into the oral, gastrointestinal tract and pancreatic tissue.54
Oral microbes and oral diseases.: How oral microbes spread through translocation or spread to the pancreas has been confirmed by microbiologists.55 Xiaozhou et al. found in a case-control study that oral pathogens are associated with high risk of PC.56 Currently, key microorganisms associated with PC are Fusobacterium, Streptococcus mitis (S. mitis), Porphyromonas gingivalis (P. gingivalis), and Neisseria elongata (N. elongata).34 Periodontitis is directly linked to colorectal cancer,57 PC,58,59 and extraintestinal tumors.60-62 Corynebacterium and lectins are associated with a high risk of PDAC.56
Gastrointestinal microbiota.: The gut microbiota is a complex ecosystem consisting of the largest microbial community in the human body.63 The microbes in the microbiota interact to protect the body from infection, which in turn allow the gastrointestinal tract to function normally. The hydrolase secreted by the pancreas requires intestinal bacteria to break down; and the pancreatic juice has antibacterial activity, protects the pancreas from retrograde infection, and helps maintain the normal function of the intestinal flora. In recent years, studies have revealed the potential pathogenic role of intestinal microbes in PC. Intestinal microorganisms can be linked to the pancreas through the circulatory system or the bile duct (transduction).34,64,65 The main microorganisms are Helicobacter pylori (H. pylori), Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV). The role of H. pylori in PC has been controversial.66-69 Researchers have drawn different or even opposite conclusions through epidemiological methods such as cohort studies,70,71 case-control studies,72,73 and meta-analyses,72,74 suggesting that H. pylori may not directly interact with PC, but rather is related to its occurrence and indirect association with PC through inflammation and immune evasion.75
Intrapancreatic microbial system.: It has long been believed that most microorganisms cannot survive in the pancreas because the pancreas secretes a large amount of strongly alkaline pancreatic juice and proteases.76 However, some researchers have found that the number of microorganisms in the pancreas of PDAC patients is 1000 times that of the normal control group by RNA probe and PCR technology.65,77 A comparative study showed a significant increase in the number of Bifidobacteria, γ-Proteus, H. pylori, and Clostridium bacteria in the pancreas of patients with PDAC. Proteus γ may be related to the drug resistance of the anticancer drug gemcitabine.78 Clinical studies have shown that H. pylori activates pathways that control the growth and progression of pancreatic PDAC, which may be related to the malignancy of PC.79 In the prognostic assessment of PC, the presence of Fusobacterium can significantly shorten the survival of patients with PC.56,80(Figure 1)
Figure 1.
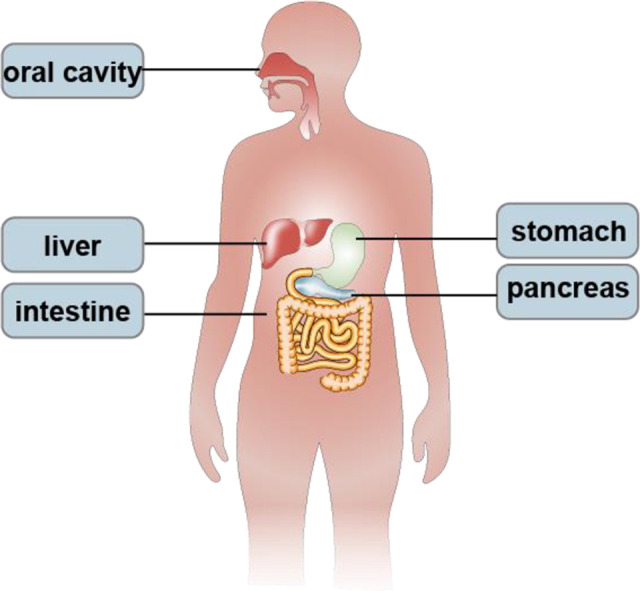
Microbial system associated with pancreatic cancer.
Smoking
Among the factors associated with PC, smoking is the most important modifiable factor. A case-control study demonstrated that smokers had a 74% increased risk of PC.81,82 The expression of stem cell markers in PDAC cells exposed to CSE and NNN/NNK (Nicotine and Nicotine-derived carcinogens) is significantly enhanced. Studies showed that cigarette smoke and its ingredients could increase the stem cell characteristics of pancreatic cells. The stem cell characteristics enable cancer cells to self-renew and differentiate into other cell types. The specific mechanism may involve CHRNA7 mediates the signal transmission and activates Fosl1 expression through the ERK1/2 pathway, thereby enabling the activation of the promoters of both Fosl1 and PAF1.83
In recent years, e-cigarettes have been proposed as long-term alternatives to traditional smoking or as a means of quitting smoking by heating nicotine; however, there is very little data on their effectiveness and safety. Thus, the relationship between e-cigarettes and pancreatic diseases remains to be elucidated.
Alcohol
A cohort study of 2187 patients with PC found that the risk of illness was significantly higher in people who drank more than 30 g per day (RR: 1.22, 95% confidence interval (CI): 1.03–1.45).84 There was also a meta-analysis that found that low- and moderate-drinking alcohol was not associated with PC risk, and there was a dose-response relationship between alcohol consumption and risk in high-drinking populations.85
Chronic Pancreatitis
There is growing evidence that CP is an independent risk factor for PC.86 CP is a progressive inflammatory state of the pancreas that causes pancreatic fibrosis and loss of islet cells.87 Frequent seizures of CP can lead to disease progression, as well as pancreatic exocrine and/or endocrine insufficiency, eventually leading to abnormal pancreatic enzymes. CP may also disrupt the endoplasmic reticulum, mitochondria, and lysosomal autophagy systems of pancreatic cells and can lead to cellular DNA damage, chromosomal mutations, and oncogene activation. A large cohort study and case-control study found that the combined relative risk of PC in CP patients was estimated to be 13.3.87
Obesity
For rapidly proliferating cancer cells, lipid oxidation and biosynthesis are essential for cell survival. Compared with non-tumor tissue, fat can make cancer cells more viable.88
Epidemiological evidence suggests that obesity is an important risk factor for PC. The KRAS mutation, a ring network between the YAP gene and obesity, contributes to the formation of PC.47 It was confirmed by the genetically engineered mouse disease model that the KRAS mutation is the initial event of PC. However, the oncogenic KRAS mutation needs to interact with environmental, nutrient, and metabolic stressors (inflammation and obesity), which together lead to the downstream effector gene activated of pancreas tumor cells.89 At the same time, changes in Type 2 diabetes mellitus (T2DM), insulin resistance, inflammation, intestinal microflora90 and gastrointestinal peptides91 can enhance/adjust downstream signals. There is evidence that fat distribution can also affect cancer risk. It is recommended to use the waist-to-hip ratio or waist circumference to measure the development of certain cancers together with the body mass index (BMI).47,92 Cancer cells have been shown to have the flexibility to use alternative and easily available carbon sources for biosynthesis processes.88
Diagnostic Investigations
Histological Examination
Histopathology analysis and/or cytology are the “gold standard” for the diagnosis of PC. Except for patients undergoing surgical resection, the remaining patients should strive for a clear pathological diagnosis before formulating a treatment plan. Current methods for obtaining histopathology or cytology specimens include: (1) Endoscopic ultrasonography (EUS) or computed tomography (CT) guided biopsy: (2) ascites cytology; or (3) exploratory biopsy under laparoscopy or open surgery diagnosis.
Tumor Biomarkers
In recent years, our knowledge of PDAC molecular changes has grown significantly and has helped identify new serum tumor markers. Currently, there are 6 common tumor biomarkers (CA19-9, CA242, carcinoembryonic antigen [CEA], CA125, microRNAs and K-RAS gene mutations) in PC.93 The combination of tumor markers and imaging methods may be the first choice for early screening for PC.94 According to reports in the literature, the combination of CA19-9 and CA125 increased sensitivity compared to CA19-9 alone, and the combination of serum CA19-9 and CEA increased specificity by 84%.95 Other researchers have shown through meta-analysis that the CA19-9 and CA242 combination, or CA19-9 and K-RAS gene mutation or endoscopic retrograde cholangiopancreatography and EUS may be more diagnostic than separate detection.96-99 There is also evidence that the combination of microRNAs and CA19-9 is more accurate.100,101 In recent years, advances in cytology and genomics have been used in conjunction with serum tumor markers for early diagnosis of PC. In the early stages of PC, tumor-associated macrophages (TAM) have been reported to be associated with a decrease in neutrophils and T cells.102 Among genes related to PC, including KRAS, TP53, CDKN2A, Smad4, PDAC1 and BRCA2.103,104 CA19-9 is the most commonly used indicator for postoperative detection in PC recurrence and prognosis.102,105 B7-H4, IL-6, IL-8, and IL-10 are indicators for assessing poor prognosis in PC.106,107
In recent years, circulating cell-free DNA (CfDNA) and mutation-specific circulating cell-free tumor DNA (CftDNA) have been identified as new potential biomarkers. The current studies show that there is a statistically significant correlation between changes in cfDNA and cftDNA concentrations and treatment response. Therefore, cfDNA and cftDNA may become new biomarkers for evaluating the efficacy of cancer after treatment, and because of their correlation with the tumor volume of metastases, they can also be used as tools to estimate tumor volume.108
Computed Tomography/Positron Emission Tomography
In the diagnosis of suspected pancreatic lesions, assessment of resectability of PC, assessment of vascular invasion and diagnosis of metastatic disease, multidetector computed tomography (MDCT) is now a routine examination.
MDCT can display not only small branch vessels and peripancreatic vessels, but also vascular anatomical variations, which can better understand the details of the lesions and the spatial anatomical relationship, show the changes in tumor morphology and changes in the density of various tissues, which is conducive to reflecting the stage of PC, which is related to whether surgical resection is performed. At the same time, the degree of invasion of surrounding organs and blood vessels can be determined, and the characteristics of metastatic foci can be observed. Furthermore, the influence of respiratory movement can be avoided, thereby reducing the potential for missed diagnosis of small lesions.109
The diagnostic criteria for staging refer to the PC staging established by the Japanese Pancreatic Case Association Criteria: Stage I, tumor diameter is less than or equal to 2 cm, no vascular invasion and metastasis; Stage II, tumor diameter is greater than 2 cm and less than 4 cm, enveloped cancer cell infiltration, no vascular invasion, metastasis; Stage III, tumor diameter is greater than 4 cm, with existence of nearby lymphatic metastasis; and Stage IV, tumor diameter is greater than 4 cm, with evidence of distant lymph node metastasis.
Positron emission tomography (PET) can reveal molecular information such as fine tissue function and metabolism in the body. PET-CT can diagnose tumors and other diseases early. Due to the active metabolism of tumor cells, the ability to take up imaging agents is 2-10 times that of normal cells, forming an obvious “light spot” on the image. Therefore, before the tumor has produced anatomical changes, hidden microscopic lesions (greater than 5 mm), to achieve the purpose of early detection and diagnosis of PC.110
Endoscopic Ultrasonography
Several reports in the literature have indicated that is superior to MDCT for the diagnosis of PC. In a retrospective study, the sensitivity of EUS and MDCT for the diagnosis of PC was 98% and 86%, respectively.95 In clinical studies, EUS-guided tissue specimens (EUS-TS) and endoscopic retrograde cholangiography-guided tissue specimens (ERCP-TS) are 2 common methods. In a prospective study of 125 patients, EUS-TS was superior to ERCP-TS in assessing biliary stricture caused by pancreatic disease, especially PC.111
Magnetic Resonance Imaging
In recent years, due to the development of magnetic resonance imaging (MRI) technology, MRI findings, accurate staging, and surgical resectability of PC have been receiving much attention. MRI can also dynamically reflect the movement and chemical shift of water molecules in the lesion, and can effectively combine function and morphology.112 There was no significant difference in the frequency of MRI staging and pathological staging (P > 0.05). This result indicates that MRI staging is completely consistent with the surgical staging. The MRI results of I/II or III/IV staging of PC showed an MRI sensitivity of 1.00 and a specificity of 0.67.113 Differential diffusion-weighted imaging (DWI) is a specific MRI technique, and 2 studies have shown that DWI plays a large role in distinguishing PC from mass formation,95,112 because MRI-DWI allows accurate depiction of pancreatic lesions without radiation exposure. In the preoperative staging and resectability assessment of PC, MRI-DWI may be more clinically meaningful than MDCT.
Endoscopic Retrograde Cholangiopancreatography
Endoscopic retrograde cholangiopancreatography (ERCP) is used to diagnose pancreatic head cancer and allows for cytopathological examination at the trans-nipple bile duct stent. It is more diagnostic in the case of exogenous bile duct stricture. It allows biopsy from the ampulla of a pancreatic tumor, and if there is cholestasis in the head of the pancreas, the stent needs to be placed in the bile duct. It allows more operability. Some researchers believe that the combination of brushing cytology and aspiration cytology during ERCP can improve the diagnostic accuracy.114 In addition, probe-based confocal laser endoscopes exhibit high sensitivity in detecting malignant tumors in pancreaticobiliary stenosis.115
Treatment
Traditional PC treatment includes surgery, chemotherapy, radiotherapy, and palliative care. In recent years, research on targeted therapy, immunotherapy, and microbial therapy has become more and more in-depth, and may be combined with traditional methods for the treatment of PC in the future. Similarly, the stage of PC determines its treatment.
Surgery
Surgical Resection Indication
Surgical treatment is considered the only way to cure PC. It can significantly prolong survival. Surgical resection can be divided into resectable PC, handover resectable PC, unresectable PC (local progression), or combined with distant metastasis95
Cooperation With Neoadjuvant Therapy
To achieve better local tumor control and ultimately improve patient survival and quality of life, it has been demonstrated in many clinical trials in the United States, Europe, and Japan that surgical resection is more likely if full-dose chemotherapy is given prior to surgery. Patient survival and quality of life increased significantly. Preoperative chemotherapy/radiation may eliminate potential metastatic lesions, and preoperative treatment may be more effective than postoperative treatment, possibly due to poor drug delivery and low sensitivity after tumor removal.116 Neoadjuvant chemotherapy should be applied to make local tumors easier to surgically remove.
In general, arterial-affected PC is considered unsuitable for resection. In a study of patients with unresectable PC, 76 of the 125 patients (61%) were able to undergo tumor resection after neoadjuvant chemotherapy, with a significant increase in the median survival period.117
Surgical Techniques
PC resection includes total pancreatectomy, distal pancreatectomy plus splenectomy and pancreaticoduodenectomy. However, only 10% of patients are diagnosed with early-onset PC, and standard excision methods can be used. About 60% of patients have metastatic disease or poor performance.
There is evidence that the prognosis is worse in patients with para-aortic lymph node (PALN) metastases, but PALN is insufficient evidence of a grade I contraindication for surgery.118
Laparoscopic surgery has now been performed in large hospitals for the treatment of PC. A retrospective cohort study has shown that laparoscopic PC resection allows patients to return to their diet earlier and reduce hospital stays with less trauma. But this technology is more demanding for doctors.119
In the past few decades, PC surgery has become quite safe and the risk of postoperative mortality has dropped to 3%. However, the risk of postoperative prevalence remains high, and the high invasiveness and metastasis of PC should be an important area of ongoing research. With the development of modern technology, surgical indications have expanded from resectable PC (stages I and II) to locally advanced disease (stage III). Surgical resection will still be the basic means of treatment for patients with PC. For stage IV patients, PC patients with distant metastases are not recommended for tumor reduction surgery, and some patients with distant isolated metastases can undergo surgical evaluation after tumor shrinkage after long-term chemotherapy.120
Chemotherapy
Chemotherapy is an important part of the comprehensive treatment of PC. Studies have shown that after radical resection, adjuvant chemotherapy can significantly improve disease-free survival and overall survival of patients with PC. After radical resection, modified leucovorin, 5-fluorouracil, irinotecan, and oxaliplatin (MFOLFIRINOX) are often used for 6 months of adjuvant chemotherapy, or 6 months of gemcitabine and capecitabine. In patients with metastatic PC, the preferred option is the FOLFIRINOX regimen, gemcitabine and NAB-paclitaxel in combination with chemotherapy. If the patient is not suitable for combination chemotherapy, gemcitabine is the first choice. For patients with locally advanced PC, combination therapy with chemotherapy and radiation therapy is the first choice for this type of patient, with gemcitabine (with or without erlotinib) combined with 54 Gy. Currently, researchers are investigating other forms of topical therapy such as radiofrequency ablation, high-intensity focused ultrasound, microwave ablation, irreversible electroporation, and topical anti-KRAS therapy (using siG12D-Loder). In patients with locally advanced unresectable cancer, neoadjuvant therapy combined with chemotherapy and surgical treatment is the only opportunity for secondary surgery in such patients.121 In the future, specific treatments based on the molecular characteristics of patient organs will become a reality and have considerable prospects.122
Radiotherapy
Radiation therapy uses X-rays to destroy or damage cancer cells, making them unable to proliferate. Radiotherapy is mainly used in patients with locally advanced PC. Multiple studies have shown that in patients with advanced PC, receiving chemotherapy was no better than continuing chemotherapy is better and does not improve patient survival.123,124 In clinical use, there are 4 main forms of radiotherapy:
External beam radiation therapy, which uses external radiation therapy sources that emit X-rays, gamma rays, electrons or heavy particles. However, the surrounding tissue is greatly damaged, and this treatment requires multiple courses of treatment;
Brachytherapy, which is mainly used for internal radiotherapy by surgery or laparoscopy in the pancreas or adjacent to the pancreas. It can be administered in the form of single or multiple scores and in combination with external radiation therapy.125
Targeted Therapy
Targeted therapy is very successful in many types of cancer. For example, EGFR or VEGF-directed antibodies in colorectal cancer, trastuzumab in HER-2 positive breast cancer, or tyrosine inhibitors in non-small cell lung cancer subpopulations, such as crizotinib. Although the Food and Drug Administration (FDA) has recently approved pembrolizumab as a targeted treatment for PC, to date, all other targeted drugs have failed in PC patients, including affrecept, cetuximab, sorafenib, bevacizumab, and axitinib. The available evidence preliminarily indicates that the efficacy in PDAC patients with HA-high expression depends on PEGPH20 when PARP inhibitors are used in combination with NAB-paclitaxel/gemcitabine.126
Recently, 19 patients with metastatic PC were clinically studied. They underwent a molecularly tailored treatment regimen. These patients received dual treatment with gemcitabine and oxaliplatin. The results showed that 55% of patients had tumor markers reduced by >50%. Partially relieved and stable patients were 28% and 50%, respectively. However, 7 (88%) patients still died within 3 months after treatment, and the rest received second-line treatment.127 New targets for targeted therapy for PC have recently been identified, such as PEGPH20 and CKAP4.128
Because PC tumor cells carry unique genetically driven mutations, this poses a huge challenge for molecular targeted therapy.
Immunotherapy
Immune checkpoint blockade (ICB) therapy is now approved for various types of cancer, such as melanoma, lung cancer, renal cell carcinoma, and head and neck squamous cell carcinoma.129 However, PC is considered to be a less immunogenic cancer. The microenvironment of PC tumors is thought to create an immunosuppressive environment. Therefore, there is currently no immunotherapy approved for patients with PC. Monotherapy of CTLA-4 or PD1 inhibitors is essentially ineffective in PC, and many clinical studies have tested immunotherapy in combination with chemotherapy, chemoradiotherapy, vaccines, and cytokine antagonism.130 In theory, clinically relevant drug chemotherapy should reduce the immune response, but clinical studies have shown that the patient’s immune status does not change.131,132 Radiation therapy can cause tumor macrophages to obtain an immunosuppressive phenotype and to disable T cell-mediated anti-tumor responses, thereby inhibiting cellular immune function. Nonetheless, the FDA approved the use of pembrolizumab in the treatment of microsatellite unstable cancers unrelated to the type of cancer, which is contrary to the conclusion that radiotherapy reduces cellular immune function. This milestone study is ongoing.133
However, certain tumors develop resistance and relapse during ICB treatment. Some intrinsic factors of immune cells and tumor cells may affect the patient’s response to ICB, including T cell infiltration; T cell and innate immune cells activate differentiation and antigen presentation to MHC-1 molecule.134 Recently, a study from the United States made a breakthrough in immunotherapy, and the results showed that interferon (IFNs) is a double-edged sword in the tumor immune response. IFNs activate dendritic cells at the initial stage to promote cross-activation of tumor-specific CD8+ T cells, but sustained IFNs can produce negative feedback, causing T cell failure to produce immunosuppression.135 Another study on enhancing the efficacy of tumor immunotherapy has made breakthroughs. It has shown that inhibiting IFNG signaling pathway in tumor cells can enhance the body’s ability to adapt to tumor cells or innate immune killing, and improve the efficacy of immunotherapy.136
Microbial Therapy
There is now strong evidence that the human microbiota plays a key role in regulating cancer development and response to cancer treatment. It affects the response of intestinal and parenteral tissues to cancer treatment.30 In one study, the researchers transplanted intestinal bacterial extracts from PC hosts into a mouse model and found that macrophages in the bacterial extract of patients prevented the activation of CD4+ and CD8+ T cells. Decreased ability to present antigenic macrophage antigens induces higher activation of different pattern recognition receptors (PRRs) in tumor macrophages. In contrast, PCs that grow in antibiotic ablation hosts show significantly opposite results.137
To date, the results of intestinal microflora forming systemic immunity and tumor-specific immunity in PC have been confirmed, but the mechanism remains to be studied. For example, it is unclear whether gut microbes only regulate tumors affecting immune cells in distant intestinal/intestinal-associated lymphoid tissue barriers or whether microbes need to affect local antigen presentation in tumor and tumor-draining lymph nodes.138 In addition, differential effects of microbial-derived metabolites have been reported to regulate PDAC immunity. This poses a challenge for clinically targeted tumor-targeted synthetic bacteria and probiotics. At the same time, the role of microbial-derived metabolites and microbial-matrix interactions in metastatic disease remains unclear.139 Several studies have shown that human microbes and gut bacteria are important components of the PC tumor microenvironment, and microbial conditioning such as fecal transplantation is a strong candidate for future clinical trials.140
In the future, how microflora contributes to the establishment and maintenance of immune tolerance is the focus of research in the attempt to find novel treatment strategies. A detailed analysis of the PC-associated microflora can be used to identify specific communities that play a positive or negative role in the development and progression of PC, thereby allowing more selective methods to modulate responses.
Palliative Care
Because PC patients need palliative care at some point, palliative care is as important as other treatments. Percutaneous bile duct drainage, surgical gastrojejunostomy, and endoscopic duodenal stents are the 3 main approaches form management of patients with gastric outlet obstruction.95
Future Treatment Directions for Pancreas Cancer
The limitations of current PC treatment strategies have led to the need for new therapeutic approaches, clinical studies of oncolytic virus therapy, combination of microbial and chemotherapy, immunotherapy, and gene editing techniques are considered to be promising.3
Conclusions
At present, we still know very little about the etiology of PC, and researchers need further large-scale prospective research to better understand the risk factors, new methods of diagnosis and treatment related to PC.
PC is clearly familial, and screening for high-risk individuals, including the familial PC family, will identify more patients with early-stage PC, which will increase the life-span of PC patients. However, for potential targets, the best screening age, the time interval at which screening should be performed, or optimal imaging techniques have not yet been determined. Previous studies have shown that the occurrence and metastasis of PC are associated with microorganisms. The human microbial system may be related to the formation of markers, which can potentially regulate the sensitivity of tumors to therapeutic drugs, which is very beneficial for improving the therapeutic effect of PC. Microbial systems can be combined with chemotherapy and immunotherapy, which may bring great hope to patients with PC. However, there is still much controversy in this field. The human microbial system may be related to many factors such as smoking, obesity, dietary intake, etc. These factors are also important factors leading to the development of PC cells. Therefore, it is helpful to understand the microbial system as another variable in PC involved in stimulating the medium and bridge of cancer occurrence and development, or the triggering of a series of reactions by itself.
To find an application for the microbial system in the future, we can improve the effectiveness of treatment by monitoring changes in the microbiome superiority during the progression of PC and developing methods to improve the cancer-associated microbial system. The emergence of immunogenomics and gut microgenomics in the life sciences will bring about a huge breakthrough in the relationship between microbial systems and immunotherapy, and may lead to exciting clinical applications in improving the lifespan of patients with PC.
Immunotherapy for PC has encountered difficulties at this stage, as most immunotherapeutics that have been shown to be effective against other malignancies have not been successful against pancreatic tumor cells to date, possibly related to the immune tolerance mechanism of PC.
At present, we know very little about the etiology of PC, and researchers need to engage in further large-scale research to better understand the risk factors associated with PC and find new diagnostic and treatment methods for PC, which will prolong the survival of PC patients.
Acknowledgments
I would like to thank everyone who helped me during the writing of this paper.
Abbreviations
- BMI
body mass index
- CEA
carcinoembryonic antigen
- CHRNA7
Cholinergic receptor nicotinic alpha 7 subunit
- CP
Chronic pancreatitis
- CT
Computed tomography
- CSE
Cigarette smoke extract
- DWI
Diffusion-weighted imaging
- EMT
Epithelial-mesenchymal transition
- ERCP
Endoscopic retrograde cholangiopancreatography
- EUS
Endoscopic ultrasonography
- FOSL1
AP-1 transcription factor subunit
- GPBAR1
G-protein coupled receptor 1
- HbA1c
glycated hemoglobin
- IFN
Interferon
- ICB
Immune checkpoint blockade
- LPS
Lipopolysaccharide
- LTA
Lipoteichoic acid
- MHT
Menopausal hormone therapy
- MDCT
Multidetector computed tomography
- MRI
Magnetic resonance imaging
- NLR
Nodlike receptor
- NNN /NNK
Nicotine and nicotine-derived carcinogens
- PALN
Para-aortic lymph node
- PAF1
RNA polymerase II-associated factor
- PC
Pancreatic cancer
- PDAC
Pancreatic ductal adenocarcinoma
- PET
Positron emission tomography
- RR
Risk ratio
- SCFA
Sshort-chain fatty acids
- sICAM- 1
Soluble intercellular adhesion molecule-1
- T2DM
Type 2 diabetes mellitus
- TAM
Tumor-associated macrophages
- TLR
Toll-like receptor
- TNF
Tumor necrosis factor
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research on teaching reform of clinical teaching base in guangdong province((2017JD098);)
ORCID iD: ZhiYu Zhao  https://orcid.org/0000-0001-5789-9852
https://orcid.org/0000-0001-5789-9852
References
- 1. Goral V. Pancreatic cancer: pathogenesis and diagnosis. Asian Pac J Cancer Prev APJCP. 2015;16(4):5619–5624. doi:10.7314/apjcp.2015.16.14.5619 [DOI] [PubMed] [Google Scholar]
- 2. Gillen S, Schuster T, Meyer Zum Buschenfelde C, Friess H, Kleeff J. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Medicine. 2010;7(4):e1000267 doi:10.1371/journal.pmed.1000267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24(43):4846–4861. doi:10.3748/wjg.v24.i43.4846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McMenamin UC, McCain S, Kunzmann AT. Do smoking and alcohol behaviours influence GI cancer survival? Best Pract Res Clin Gastroenterol. 2017;31(5):569–577.doi:10.1016/j.bpg.2017.09.015 [DOI] [PubMed] [Google Scholar]
- 5. Masoudi S, Momayez Sanat Z, Mahmud Saleh A, Nozari N, Ghamarzad N, Ghamarzad N. Menstrual and reproductive factors and risk of pancreatic cancer in women. Middle East J Dig Dis. 2017;9(3):146–149. doi:10.15171/mejdd.2017.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sadr-Azodi O, Konings P, Brusselaers N. Menopausal hormone therapy and pancreatic cancer risk in women: a population-based matched cohort study. United European Gastroenterol J. 2017;5:1123–1128. doi:10.1177/2050640617702060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Midha S, Chawla S, Garg PK. Modifiable and non-modifiable risk factors for pancreatic cancer: a review. Cancer Lett. 2016;381(1):269–277. doi:10.1016/j.canlet.2016.07.022 [DOI] [PubMed] [Google Scholar]
- 8. Li BQ, Wang L, Li J, et al. Surgeons’ knowledge regarding the diagnosis and management of pancreatic cancer in china: a cross-sectional study. BMC Health Serv Res. 2017;17(1):395 doi:10.1186/s12913-017-2345-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019;10(1):10–27. doi:10.14740/wjon1166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Risch HA, Lu L, Wang J, et al. ABO blood group and risk of pancreatic cancer: a study in shanghai and meta-analysis. Am J Epidemiol .2013;177(12):1326–1337, doi:10.1093/aje/kws458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li X, Xu H, Gao P. ABO blood group and diabetes mellitus influence the risk for pancreatic cancer in a population from china. Med Sci Monit. 2018;24:9392–9398. doi:10.12659/msm.913769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ciccone MM, Aquilino A, Cortese F, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6(1):297–305. doi:10.2147/vhrm.s9252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hruban RH, Canto MI, Goggins M, Schulick R, Klein AP. Update on familial pancreatic cancer. Adv Surg. 2010;44(1):293–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wood LD, Hruban RH. Pathology and molecular genetics of pancreatic neoplasms. Cancer J. 2012;18(6):492–501. doi:10.1097/PPO.0b013e31827459b6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Becker AE, Hernandez YG, Frucht H, Lucas AL. Pancreatic ductal adenocarcinoma: risk factors, screening, and early detection. World J Gastroenterol. 2014;20(32):11182–11198. doi:10.3748/wjg.v20.i32.11182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yeo TP. Demographics, epidemiology, and inheritance of pancreatic ductal adenocarcinoma. Seminars in Oncology. 2015;42(1):8–18. doi:10.1053/j.seminoncol.2014.12.002 [DOI] [PubMed] [Google Scholar]
- 17. Wolpin BM, Kraft P, Gross M, et al. Pancreatic cancer risk and ABO blood group alleles: results from the pancreatic cancer cohort consortium. Cancer Res. 2010;70(3):1015–1023. doi:10.1158/0008-5472.Can-09-2993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Petersen GM, Amundadottir L, Fuchs CS, et al. A genome-wide association study identifies pancreatic cancer susceptibility loci on chromosomes 13q22.1, 1q32.1 and 5p15.33. Nat Genet. 2010;42(3):224–228. doi:10.1038/ng.522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Low SK, Kuchiba A, Zembutsu H, et al. Genome-wide association study of pancreatic cancer in Japanese population. PloS One. 2010;5(7):e11824 doi:10.1371/journal.pone.0011824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wu C, Miao X, Huang L, et al. Genome-wide association study identifies five loci associated with susceptibility to pancreatic cancer in Chinese populations. Nat Genet. 2011;44(1):62–66. doi:10.1038/ng.1020 [DOI] [PubMed] [Google Scholar]
- 21. Klein AP, Wolpin BM, Risch HA, et al. Genome-wide meta-analysis identifies five new susceptibility loci for pancreatic cancer. Nat Commun. 2018;9(1):556 doi:10.1038/s41467-018-02942-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Landi S. Genetic predisposition and environmental risk factors to pancreatic cancer: a review of the literature. Mutat Res. 2009;681(2-3):299–307. doi:10.1016/j.mrrev.2008.12.001 [DOI] [PubMed] [Google Scholar]
- 23. Raimondi S, Maisonneuve P, Lowenfels AB. Epidemiology of pancreatic cancer: an overview. Nat Rev Gastroenterol Hepatol. 2009;6(12):699–708. doi:10.1038/nrgastro.2009.177 [DOI] [PubMed] [Google Scholar]
- 24. Del Chiaro M, Segersvard R, Lohr M, Verbeke C. Early detection and prevention of pancreatic cancer: is it really possible today? World J Gastroenterol. 2014;20(34):12118–12131. doi:10.3748/wjg.v20.i34.12118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen F, Roberts NJ, Klein AP. . Inherited pancreatic cancer. Chin Clin Oncol. 2017;6(6):58 doi:10.21037/cco.2017.12.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lanfranca PM, Thompson JK, Bednar F, et al. Metabolism and epigenetics of pancreatic cancer stem cells. Semin Cancer Biol. 2019;57:19–26. doi:10.1016/j.semcancer.2018.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gardner TB, Hessami N, Smith KD, et al. The effect of neoadjuvant chemoradiation on pancreatic cancer-associated diabetes mellitus. Pancreas. 2014;43(7):1018–1021. doi:10.1097/mpa.0000000000000162 [DOI] [PubMed] [Google Scholar]
- 28. Bosetti C, Rosato V, Silverman D, et al. Diabetes, antidiabetic medications, and pancreatic cancer risk: an analysis from the international pancreatic cancer case-control consortium. Ann Oncol. 2014;l25(10):2065–2072. doi:10.1093/annonc/mdu276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Huang BZ, Pandol SJ, Jeon CY, et al. New-onset diabetes, longitudinal trends in metabolic markers, and risk of pancreatic cancer in a heterogeneous population. Clin Gastroenterol Hepatol. 2019;18(8):1812–1821.e7. doi:10.1016/j.cgh.2019.11.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Raza MH, Raza MH, Arshad A, et al. Microbiota in cancer development and treatment. J Cancer Res Clin Oncol. 2019;145(1):49–63. doi:10.1007/s00432-018-2816-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Garrett WS. Cancer and the microbiota. Science. 2015;348(6230):80–86. doi:10.1126/science.aaa4972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hamm AK, Weir TL. Editorial on “cancer and the microbiota” published in science. Ann Transl Med. 2015;3(13):175 doi:10.3978/j.issn.2305-5839.2015.07.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Meng C, Bai C, Brown TD, Hood LE, Tian Q. Human gut microbiota and gastrointestinal cancer. Genomics, Proteomics Bioinformatics. 2018; 16(1):33–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wei MY, Shi S, Liang C, et al. The microbiota and microbiome in pancreatic cancer: more influential than expected. Mol Cancer. 2019;18(1):97 doi:10.1186/s12943-019-1008-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gensollen T, Iyer SS, Kasper DL, Blumberg RS. How colonization by microbiota in early life shapes the immune system. Science. 2016;352(6285):539–544. doi:10.1126/science.aad9378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Palm NW, de Zoete MR, Flavell RA. Immune-microbiota interactions in health and disease. Clin Immunol. 2015;159(2):122–127. doi:10.1016/j.clim.2015.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vijay-Kumar M, Gewirtz AT. Flagellin: key target of mucosal innate immunity. Mucosal Immunol. 2009;2(3):197–205. doi:10.1038/mi.2009.9 [DOI] [PubMed] [Google Scholar]
- 38. Pushalkar S, Hundeyin M, Daley D, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discovery. 2018;8(4):403–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Brown DG, Rao S, Weir TL, et al. Metabolomics and metabolic pathway networks from human colorectal cancers, adjacent mucosa, and stool. Cancer Metab. 2016;4:11 doi:10.1186/s40170-016-0151-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ginsburg I. Role of lipoteichoic acid in infection and inflammation. Lancet. Infect Dis. 2002;2(3):171–179. [DOI] [PubMed] [Google Scholar]
- 41. Hermann C, Spreitzer I, Schröder NW, et al. Cytokine induction by purified lipoteichoic acids from various bacterial species—role of LBP, sCD14, CD14 and failure to induce IL-12 and subsequent IFN-gamma release. Eur J Immunol. 2002;32(2):541–551, doi:10.1002/1521-4141(200202)32:2<541: Aid-immu541>3.0.Co;2-p [DOI] [PubMed] [Google Scholar]
- 42. Carino A, Graziosi L, D’Amore C, et al. The bile acid receptor GPBAR1 (TGR5) is expressed in human gastric cancers and promotes epithelial-mesenchymal transition in gastric cancer cell lines. Oncotarget. 2016;7(38):61021–61035. doi:10.18632/oncotarget.10477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol. 2014;12(10):661–672. doi:10.1038/nrmicro3344 [DOI] [PubMed] [Google Scholar]
- 44. Smith PM, Howitt MR, Panikov N, et al. The microbial metabolites, short-chain fatty acids, regulate colonic treg cell homeostasis. Science. 2013;341(6145):569–573. doi:10.1126/science.1241165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504(7480):446–450. doi:10.1038/nature12721 [DOI] [PubMed] [Google Scholar]
- 46. Arpaia N, Campbell C, Fan X, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature. 2013;504(7480):451–455. doi:10.1038/nature12726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Eibl G, Rozengurt E. KRAS, YAP, and obesity in pancreatic cancer: a signaling network with multiple loops. Semin Cancer Biol. 2019;54:50–62. doi:10.1016/j.semcancer.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hold GL, Smith M, Grange C, Watt ER, El-Omar EM, Mukhopadhya I. Role of the gut microbiota in inflammatory bowel disease pathogenesis: what have we learnt in the past 10 years? World J Gastroenterol. 2014;20(5):1192–1210. doi:10.3748/wjg.v20.i5.1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Schwabe RF, Jobin C. The microbiome and cancer. Nat Rev Cancer. 2013;13(11):800–812. doi:10.1038/nrc3610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Staley C, Weingarden AR, Khoruts A, Sadowsky MJ. Interaction of gut microbiota with bile acid metabolism and its influence on disease states. Applied Microbiology and Biotechnology. 2017;101(1):47–64. doi:10.1007/s00253-016-8006-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Tilg H, Adolph TE. Beyond digestion: the pancreas shapes intestinal microbiota and immunity. Cell Metabolism. 2017;25(3):495–496. doi:10.1016/j.cmet.2017.02.018 [DOI] [PubMed] [Google Scholar]
- 52. Zitvogel L, Galluzzi L, Viaud S, et al. Cancer and the gut microbiota: an unexpected link. Science Transl Med. 2015;7(271):271ps1 doi:10.1126/scitranslmed.3010473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Arthur JC, Perez-Chanona E, Mühlbauer M, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 2012;338(6103):120–123. doi:10.1126/science [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ertz-Archambault N, Keim P, Von Hoff D. Microbiome and pancreatic cancer: a comprehensive topic review of literature. World J Gastroenterol. 2017;23(10):1899–1908. doi:10.3748/wjg.v23.i10.1899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hayashi C, Gudino CV, Gibson FC, 3rd, Genco CA. Review: pathogen-induced inflammation at sites distant from oral infection: bacterial persistence and induction of cell-specific innate immune inflammatory pathways. Mol Oral Microbiol. 2010;25(5):305–316. doi:10.1111/j.2041-1014.2010.00582.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Fan X, Alekseyenko AV, Wu J, et al. Human oral microbiome and prospective risk for pancreatic cancer: a population-based nested case-control study. Gut. 2018;67(1):120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ahn J, Segers S, Hayes RB. Periodontal disease, Porphyromonas gingivalis serum antibody levels and orodigestive cancer mortality. Carcinogenesis. 2012;33(5):1055–1058. doi:10.1093/carcin/bgs112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Bracci PM. Oral health and the oral microbiome in pancreatic cancer: an overview of epidemiological studies. Cancer J. 2017;23(6):310–314. doi:10.1097/ppo.0000000000000287 [DOI] [PubMed] [Google Scholar]
- 59. Heikkila P, But A, Sorsa T, Haukka J. Periodontitis and cancer mortality: register-based cohort study of 68,273 adults in 10-year follow-up. Int J Cancer. 2018;142(11):2244–2253. doi:10.1002/ijc.31254 [DOI] [PubMed] [Google Scholar]
- 60. Mai X, LaMonte MJ, Hovey KM, et al. History of periodontal disease diagnosis and lung cancer incidence in the women’s health initiative observational study. Cancer Causes Control. 2014;25(8):1045–1053. doi:10.1007/s10552-014-0405-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Freudenheim JL, Genco RJ, LaMonte MJ, et al. Periodontal disease and breast cancer: prospective cohort study of postmenopausal women. Cancer Epidemiol, Biomarkers Prev. 2016;25(1):43–50. doi:10.1158/1055-9965.Epi-15-0750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Nwizu NN, Marshall JR, Moysich K, et al. Periodontal disease and incident cancer risk among postmenopausal women: results from the women’s health initiative observational cohort. Cancer Epidemiol, Biomarkers Prev. 2017;26(8):1255–1265. doi:10.1158/1055-9965.Epi-17-0212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mishra AK, Dubey V, Ghosh AR. Obesity: an overview of possible role(s) of gut hormones, lipid sensing and gut microbiota. Metabolism. 2016;65(1):48–65. doi:10.1016/j.metabol.2015.10.008 [DOI] [PubMed] [Google Scholar]
- 64. Fritz S, Hackert T, Hartwig W, et al. Bacterial translocation and infected pancreatic necrosis in acute necrotizing pancreatitis derives from small bowel rather than from colon. Am J Surg. 2010;200(1):111–117. doi:10.1016/j.amjsurg.2009.08.019 [DOI] [PubMed] [Google Scholar]
- 65. Pushalkar S, Hundeyin M, Daley D, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 2018;8(4):403–416. doi:10.1158/2159-8290.Cd-17-1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yu G, Murphy G, Michel A, et al. Seropositivity to Helicobacter pylori and risk of pancreatic cancer. Cancer Epidemiol, Biomarkers Prev. 2013;22(12):2416–2419. doi:10.1158/1055-9965.Epi-13-0680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Chen XZ, Wang R, Chen HN, Hu JK. Cytotoxin-associated gene a-negative strains of helicobacter pylori as a potential risk factor of pancreatic cancer: a meta-analysis based on nested case-control studies. Pancreas. 2015;44(8):1340–1344. doi:10.1097/mpa.0000000000000414 [DOI] [PubMed] [Google Scholar]
- 68. Wang Y, Zhang FC, Wang YJ. Helicobacter pylori and pancreatic cancer risk: a meta-analysis based on 2,049 cases and 2,861 controls. Asian Pac J Cancer Prev. 2014;15(11):4449–4454. doi:10.7314/apjcp.2014.15.11.4449 [DOI] [PubMed] [Google Scholar]
- 69. Risch HA, Lu L, Kidd MS, et al. Helicobacter pylori seropositivities and risk of pancreatic carcinoma. Cancer Epidemiol Biomarkers Prev. 2014;23(1):172–178. doi:10.1158/1055-9965.Epi-13-0447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Bao Y, Spiegelman D, Li R, Giovannucci E, Fuchs CS, Michaud DS. History of peptic ulcer disease and pancreatic cancer risk in men. Gastroenterology. 2010;138(2):541–549. doi:10.1053/j.gastro.2009.09.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Lindkvist B, Johansen D, Borgstrom A, Manjer J. A prospective study of Helicobacter pylori in relation to the risk for pancreatic cancer. BMC Cancer. 2008;8(1):321 doi:10.1186/1471-2407-8-321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Xiao M, Wang Y, Gao Y. Association between helicobacter pylori infection and pancreatic cancer development: a meta-analysis. PloS One. 2013;8(9):e75559 doi:10.1371/journal.pone.0075559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Risch HA, Yu H, Lu L, Kidd MS. ABO blood group, helicobacter pylori seropositivity, and risk of pancreatic cancer: a case-control study. J Natl Cancer Inst. 2010;102(7):502–505. doi:10.1093/jnci/djq007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Schulte A, Pandeya N, Fawcett J, et al. Association between helicobacter pylori and pancreatic cancer risk: a meta-analysis. Cancer Cause Control. 2015;26(7):1027–1035. doi:10.1007/s10552-015-0595-3 [DOI] [PubMed] [Google Scholar]
- 75. Jesnowski R, Isaksson B, Möhrcke C, et al. Helicobacter pylori in autoimmune pancreatitis and pancreatic carcinoma. Pancreatology. 2010;10(4):462–466. doi:10.1159/000264677 [DOI] [PubMed] [Google Scholar]
- 76. Maekawa T, Fukaya R, Takamatsu S, et al. Possible involvement of enterococcus infection in the pathogenesis of chronic pancreatitis and cancer. Biochem Biophys Res Commun. 2018;506(4):962–969. doi:10.1016/j.bbrc.2018.10.169 [DOI] [PubMed] [Google Scholar]
- 77. Dickson I. Microbiome promotes pancreatic cancer. Nat Rev Gastroenterol Hepatol. 2018;15(6):328 doi:10.1038/s41575-018-0013-x [DOI] [PubMed] [Google Scholar]
- 78. Geller LT, Barzily-Rokni M, Danino T, et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science. 2017;357(6356):1156–1160. doi:10.1126/science.aah5043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Takayama S, Takahashi H, Matsuo Y, Okada Y, Manabe T. Effects of helicobacter pylori infection on human pancreatic cancer cell line. Hepato-Gastroenterology. 2007;54(80):2387–2391. [PubMed] [Google Scholar]
- 80. Mitsuhashi K, Nosho K, Sukawa Y, et al. Association of fusobacterium species in pancreatic cancer tissues with molecular features and prognosis. Oncotarget. 2015;6(9):7209–7220. doi:10.18632/oncotarget.3109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Iodice S, Gandini S, Maisonneuve P, Lowenfels AB. Tobacco and the risk of pancreatic cancer: a review and meta-analysis. Langenbeck’s Arch Surg. 2008;393(4):535–545. doi:10.1007/s00423-007-0266-2 [DOI] [PubMed] [Google Scholar]
- 82. Montes EM, Van Hoogstraten L, Rubio PG, et al. Pancreatic cancer risk in relation to lifetime smoking patterns, tobacco type, and dose-response relationships. Cancer Epidemiol Biomar Prev. 2020;29(5):1009–1018. doi:10.1158/1055-9965.Epi-19-1027 [DOI] [PubMed] [Google Scholar]
- 83. Nimmakayala RK, Seshacharyulu P, Lakshmanan I, et al. Cigarette smoke induces stem cell features of pancreatic cancer cells via PAF1. Gastroenterology. 2018;155(3):892–908.e896. doi:10.1053/j.gastro.2018.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Genkinger JM, Spiegelman D, Anderson KE, et al. Alcohol intake and pancreatic cancer risk: a pooled analysis of fourteen cohort studies. Cancer Epidemiol Biomar Prev. 2009;18(3):765–776. doi:10.1158/1055-9965.Epi-08-0880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wang YT, Gou YW, Jin WW, Xiao M, Fang HY. Association between alcohol intake and the risk of pancreatic cancer: a dose-response meta-analysis of cohort studies. BMC Cancer. 2016;16(1):212 doi:10.1186/s12885-016-2241 -1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Samokhvalov AV, Rehm J, Roerecke M. Alcohol consumption as a risk factor for acute and chronic pancreatitis: a systematic review and a series of meta-analyses. EBioMed. 2015;2(12):1996–2002. doi:10.1016/j.ebiom.2015.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144(6):1252–1261. doi:10.1053/j.gastro.2013.01.068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Downes DP, Daurio NA, McLaren DG, Carrington P, Previs SF, Williams KB. The impact of extracellular fatty acids and oxygen tension on lipid synthesis and assembly in pancreatic cancer cells. ACS Chem Biol. 2020. doi:10.1021/acschembio.0c00219 [DOI] [PubMed] [Google Scholar]
- 89. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):7–30. doi:10.3322/caac.21387 [DOI] [PubMed] [Google Scholar]
- 90. Djuric Z. Obesity-associated cancer risk: the role of intestinal microbiota in the etiology of the host proinflammatory state. Transl Res. 2017;179:155–167. doi:10.1016/j.trsl.2016.07.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Li J, Song J, Zaytseva YY, et al. An obligatory role for neurotensin in high-fat-diet-induced obesity. Nature. 2016;533(7603):411–415. doi:10.1038/nature17662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Siergiejko ASK, Gomez-Chou SB, Cruz-Monserrate Z, et al. Chronic inflammation initiates multiple forms of K-Ras-independent mouse pancreatic cancer in the absence of TP53. Oncogene. 2017;36(22):3149–3158. doi:10.1038/onc.2016.461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Ge L, Pan B, Song F, et al. Comparing the diagnostic accuracy of five common tumour biomarkers and CA19-9 for pancreatic cancer: a protocol for a network meta-analysis of diagnostic test accuracy. BMJ Open. 2017;7(12):e018175 doi:10.1136/bmjopen-2017-018175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Gemmel C, Eickhoff A, Helmstadter L, Riemann JF. Pancreatic cancer screening: state of the art. Expert Rev Gastroenterol Hepatol. 2009;3(1):89–96. doi:10.1586/17474124.3.1.89 [DOI] [PubMed] [Google Scholar]
- 95. Kamisawa T, Wood LD, Itoi T, Takaori K. Pancreatic cancer. Lancet. 2016;388(10039):73–85. doi:10.1016/s0140-6736(16)00141-0 [DOI] [PubMed] [Google Scholar]
- 96. Zhang Y, Yang J, Li H, et al. Tumor markers CA19-9, CA242 and CEA in the diagnosis of pancreatic cancer: a meta-analysis. Int J Clin Exp Med. 2015;8(7):11683–11691. [PMC free article] [PubMed] [Google Scholar]
- 97. Gu J, Wang D, Huang Y, Lu Y, Peng C. Diagnostic value of combining CA 19-9 and K-ras gene mutation in pancreatic carcinoma: a meta-analysis. Int J Clin Exp Med. 2014;7(10):3225–3234. [PMC free article] [PubMed] [Google Scholar]
- 98. Li H, Hu Z, Chen J, Guo X. Comparison of ERCP, EUS, and ERCP combined with EUS in diagnosing pancreatic neoplasms: a systematic review and meta-analysis. Tumour Biol. 2014;35(9):8867–8874. doi:10.1007/s13277-014-2154-z [DOI] [PubMed] [Google Scholar]
- 99. Goonetilleke KS, Siriwardena A. K. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol. 2007;33(3):266-270. doi:10.1016/j.ejso.2006.10.004 [DOI] [PubMed] [Google Scholar]
- 100. Liu J, Gao J, Du Y, et al. Combination of plasma microRNAs with serum CA19-9 for early detection of pancreatic cancer. Int J Cance. 2012;131(3):683–691. doi:10.1002/ijc.26422 [DOI] [PubMed] [Google Scholar]
- 101. Schultz NA, Dehlendorff C, Jensen BV, et al. MicroRNA biomarkers in whole blood for detection of pancreatic cancer. JAMA. 2014;311(4):392–404, doi:10.1001/jama.2013.284664 [DOI] [PubMed] [Google Scholar]
- 102. Lee B, Gibbs P. Inflammation, biomarkers and immuno-oncology pathways in pancreatic cancer. J Pers Med. 2019;9(2): 20 doi:10.3390/jpm9020020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Steele CW, Jamieson NB, Evans TR, et al. Exploiting inflammation for therapeutic gain in pancreatic cancer. Br J Cancer. 2013;108(5):997–1003. doi:10.1038/bjc.2013.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Cicenas J, Kvederaviciute K, Meskinyte I, et al. KRAS, TP53, CDKN2A, SMAD4, BRCA1, and BRCA2 mutations in pancreatic cancer. Cancers. 2017; 9(5):42 doi:10.3390/cancers9050042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Daamen LA, Vincent PG, Hanne DH, et al. Systematic review on the role of serum tumor markers in the detection of recurrent pancreatic cancer. HPB (Oxford). 2018;20(4):297–304. doi:10.1016/j.hpb.2017.11.009 [DOI] [PubMed] [Google Scholar]
- 106. Shen L, Yun Q, Weigen W, et al. B7-H4 is a prognostic biomarker for poor survival in patients with pancreatic cancer. Hum Pathol. 2017;66:79–85. doi:10.1016/j.humpath.2017.05.023 [DOI] [PubMed] [Google Scholar]
- 107. Feng L, Qi Q, Peng W, et al. Serum levels of IL-6, IL-8, and IL-10 are indicators of prognosis in pancreatic cancer. J Int Med Res. 2018;46(12):5228–5236. doi:10.1177/0300060518800588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Hufnagl C, Leisch M, Weiss L, et al. Evaluation of circulating cell-free DNA as a molecular monitoring tool in patients with metastatic cancer. Oncol Lett. 2020;19(2):1551–1558. doi:10.3892/ol.2019.11192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Ahn SS, Kim MJ, Choi JY, et al. Indicative findings of pancreatic cancer in pre diagnostic CT Eur Radiol. 2009;19(10):2448–2455. doi:10.1007/s00330-009-1422-6 [DOI] [PubMed] [Google Scholar]
- 110. Ghaneh P, Hanson R, Titman A, et al. PET-PANC: multicentre prospective diagnostic accuracy and health economic analysis study of the impact of combined modality 18fluorine-2-fluoro-2-deoxy-d-glucose positron emission tomography with computed tomography scanning in the diagnosis and management of pancreatic cancer. Health Technol Assess. 2018;22(7):1–114. doi:10.3310/hta22070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Yeo SJ, Cho CM, Jung MK, Seo AN, Bae HI. Comparison of the diagnostic performances of same-session endoscopic ultrasound- and endoscopic retrograde cholangiopancreatography-guided tissue sampling for suspected biliary strictures at different primary tumor sites. Korean J Gastroenterol. 2019;73(4):213–218. doi:10.4166/kjg.2019.73.4.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Fattahi R, Balci NC, Perman WH, et al. Pancreatic diffusion-weighted imaging (DWI): comparison between mass-forming focal pancreatitis (FP), pancreatic cancer (PC), and normal pancreas. J Magn Reson Imaging. 2009;29(2):350–356. doi:10.1002/jmri.21651 [DOI] [PubMed] [Google Scholar]
- 113. Yang S, Liu J, Jin H, He X, Nie P, Wang C. Value of magnetic resonance images in preoperative staging and resectability assessment of pancreatic cancer. J Cancer Res Ther. 2018;14(1):155–158. doi:10.4103/jcrt.JCRT_590_17 [DOI] [PubMed] [Google Scholar]
- 114. Mikata R, Ishihara T, Tada M, et al. Clinical usefulness of repeated pancreatic juice cytology via endoscopic naso-pancreatic drainage tube in patients with pancreatic cancer. J Gastroenterol. 2013;48(7):866–873. doi:10.1007/s00535-012-0684-y [DOI] [PubMed] [Google Scholar]
- 115. Rustgi SD, Amin SP, Kim MK, et al. Age, socioeconomic features, and clinical factors predict receipt of endoscopic retrograde cholangiopancreatography in pancreatic cancer. World J Gastrointest Endosc. 2019;11(2):133–144. doi:10.4253/wjge.v11.i2.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. He J, Page AJ, Weiss M, et al. Management of borderline and locally advanced pancreatic cancer: where do we stand? World J Gastroenterol. 2014;20(9):2255–2266. doi:10.3748/wjg.v20.i9.2255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Hackert T, Sachsenmaier M, Hinz U, et al. locally advanced pancreatic cancer: neoadjuvant therapy with folfirinox results in resectability in 60% of the patients. Ann Surg. 2016;264(3):457–463. doi:10.1097/sla.0000000000001850 [DOI] [PubMed] [Google Scholar]
- 118. Dai HM, Hong XF, Pang HY, Wu WM, Zhao YP. [The effect of para-aortic lymph node metastasis on the resectability of pancreatic cancer]. Zhonghua Wai Ke Za Zhi. 2019;57(1):68–71. doi:10.3760/cma.j.issn.0529-5815.2019.01.014 [DOI] [PubMed] [Google Scholar]
- 119. Shin SH, Kim SC, Song KB, et al. A comparative study of laparoscopic vs. open distal pancreatectomy for left-sided ductal adenocarcinoma: a propensity score-matched analysis. J Am Coll Surg. 2015;220(2):177–185. doi:10.1016/j.jamcollsurg.2014.10.014 [DOI] [PubMed] [Google Scholar]
- 120. Strobel O, Neoptolemos J, Jager D, Buchler MW. Optimizing the outcomes of pancreatic cancer surgery. Nat Rev Clin Oncol. 2019;16(1):11–26. doi:10.1038/s41571-018-0112 -1 [DOI] [PubMed] [Google Scholar]
- 121. Seufferlein T, Hammel P, Delpero JR, et al. Optimizing the management of locally advanced pancreatic cancer with a focus on induction chemotherapy: expert opinion based on a review of current evidence. Cancer Treat Rev. 2019;77:1–10. doi:10.1016/j.ctrv.2019.05.007 [DOI] [PubMed] [Google Scholar]
- 122. Springfeld C, Jäger D, Büchler MW, et al. Chemotherapy for pancreatic cancer. Presse Med. 2019;48(3 Pt 2):e159–e174. doi:10.1016/j.lpm.2019.02.025 [DOI] [PubMed] [Google Scholar]
- 123. Loehrer PJSr, Feng Y, Cardenes H, et al. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an eastern cooperative oncology group trial. J Clin Oncol. 2011;29(31):4105–4112. doi:10.1200/jco.2011.34.8904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Takaori K, Bassi C, Biankin A, et al. International association of pancreatology (iap)/european pancreatic club (epc) consensus review of guidelines for the treatment of pancreatic cancer. Pancreatology. 2016;16(1):14–27. doi:10.1016/j.pan.2015.10.013 [DOI] [PubMed] [Google Scholar]
- 125. Chin V, Nagrial A, Sjoquist K, et al. Chemotherapy and radiotherapy for advanced pancreatic cancer. Cochrane Database Syst Rev. 2018;3(3):CD011044 doi:10.1002/14651858.CD011044.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Zhen DB, Coveler A, Zanon S, Reni M, Chiorean EG. Biomarker-driven and molecularly targeted therapies for pancreatic adenocarcinoma. Semin Oncol. 2018;45(3):107–115. doi:10.1053/j.seminoncol.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 127. Tesfaye AA, Wang H, Hartley ML, et al. A Pilot trial of molecularly tailored therapy for patients with metastatic pancreatic ductal adenocarcinoma. J Pancreat Cancer. 2019;5(1):12–21. doi:10.1089/pancan.2019.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Kimura H, Yamamoto H, Harada T, et al. CKAP4, a dkk1 receptor, is a biomarker in exosomes derived from pancreatic cancer and a molecular target for therapy. Clin Cancer Res. 2019;25(6):1936–1947. doi:10.1158/1078-0432.Ccr-18-2124 [DOI] [PubMed] [Google Scholar]
- 129. Haanen J, Carbonnel F, Robert C, et al. Management of toxicities from immunotherapy: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29(Suppl 4):iv264–iv266. doi:10.1093/annonc/mdy162 [DOI] [PubMed] [Google Scholar]
- 130. Sahin IH, Askan G, Hu ZI, O’Reilly EM. Immunotherapy in pancreatic ductal adenocarcinoma: an emerging entity? Ann Oncol. 2017;28(12):2950–2961. doi:10.1093/annonc/mdx503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Middleton G, Greenhalf W, Costello E, et al. Immunobiological effects of gemcitabine and capecitabine combination chemotherapy in advanced pancreatic ductal adenocarcinoma. Br J Cancer. 2016;114(5):510–518. doi:10.1038/bjc.2015.468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Middleton G, Silcocks P, Cox T, et al. Gemcitabine and capecitabine with or without telomerase peptide vaccine GV1001 in patients with locally advanced or metastatic pancreatic cancer (TeloVac): an open-label, randomised, phase 3 trial. Lancet Oncol. 2014;15(8):829–840. doi:10.1016/s1470-2045(14)70236-0 [DOI] [PubMed] [Google Scholar]
- 133. Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409–413. doi:10.1126/science.aan6733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Patel SA, Minn AJ. Combination cancer therapy with immune checkpoint blockade: mechanisms and strategies. Immunity. 2018;48(3):417–433. doi:10.1016/j.immuni.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Oh JH, Kim MJ, Choi SJ, et al. Sustained type I interferon reinforces NK cell-mediated cancer immunosurveillance during chronic virus infection. Cancer Immunol Res. 2019;7(4):584–599. doi:10.1158/2326-6066.Cir-18-0403 [DOI] [PubMed] [Google Scholar]
- 136. Benci JL, Johnson LR, Choa R, et al. Opposing functions of interferon coordinate adaptive and innate immune responses to cancer immune checkpoint blockade. Cell. 2019;178(4):933–948. e914. doi:10.1016/j.cell.2019.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Riquelme E, Maitra A, McAllister F. Immunotherapy for pancreatic cancer: more than just a gut feeling. Cancer Discovery. 2018;18(4), 386–388. [DOI] [PubMed] [Google Scholar]
- 138. Benakis C, Brea D, Caballero S, et al. Commensal microbiota affects ischemic stroke outcome by regulating intestinal gammadelta T cells. Nat Med. 2016;22(5):516–523. doi:10.1038/nm.4068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Daley D, Mani VR, Mohan N, et al. Dectin 1 activation on macrophages by galectin 9 promotes pancreatic carcinoma and peritumoral immune tolerance. Nat Med. 2017;23(5):556–567. doi:10.1038/nm.4314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Schulz MD, Atay Ç, Heringer J, et al. High-fat-diet-mediated dysbiosis promotes intestinal carcinogenesis independently of obesity. Nature. 2014;514(7523):508–512. doi:10.1038/nature13398 [DOI] [PMC free article] [PubMed] [Google Scholar]


