Abstract
Background:
Many injured workers are reinjured, but reinjury risk is challenging to quantify. Because many injured workers face delayed return-to-work, or return to part-time or intermittent jobs, a calendar timescale may overestimate actual work-time at risk, yielding underestimated reinjury rates. Objectives included determining: (1) reinjury risk by degree of permanent impairment and other factors, and (2) how choice of timescale affects reinjury estimates.
Methods:
This retrospective cohort study included Washington State workers’ compensation (WC) claims for 43,114 injured workers, linked to state wage files (2003–2018). Three timescales were used to define at-risk denominators: (1) calendar quarters; (2) quarters with any wages; and (3) full-time equivalent (FTE) quarters, defined as cumulative work hours ÷ 520. Associations between reinjury outcomes and worker, injury, job, and WC vocational rehabilitation program participation characteristics were assessed using Cox proportional hazards regression.
Results:
Overall reinjury rates were 5.9 per 100 worker-years using a calendar timescale (95% CI: 5.8–6.0), 10.0 using any-wage quarters (95% CI: 9.9–10.2), and 12.5 using FTE quarters (95% CI: 12.3–12.7). Reinjury rates were highest in the first two quarters after initial injury, remaining elevated for about four years. Using FTE quarters, workers with ≥10% whole body impairment had a 34% higher risk of reinjury relative to workers with no permanent partial disability award (95% CI: 1.25–1.44); no difference was detected using calendar time.
Conclusions:
Timescale substantially affects reinjury estimates and comparisons between groups with differential return-to-work patterns. Linking wage data to WC claims facilitates measurement of long-term employment, yielding more accurate reinjury estimates.
Keywords: reinjury, occupational injuries, workers’ compensation, permanent impairment, vocational rehabilitation, permanent partial disability, disability evaluation, return to work, unemployment
1. INTRODUCTION
Injured workers are at heightened risk of both injury exacerbation and new work-related injuries, particularly during the first 12 to 18 months after initial injury and when working conditions have not changed.1–4 A prior work injury significantly increases the odds of a new or recurrent work injury.5,6 More specifically, workers who have returned to work after an injury involving time loss compensation are more likely to have a subsequent injury than other workers in the same firms.7 In an Australian workers’ compensation (WC) study involving nearly a million claims over 14 years, recurrent occupational injury and disease accounted for 53.4% of all claims.8 Compared to the initial injury, subsequent work injuries tend to result in longer work disability and higher costs.3,9
Work-related reinjury estimates vary, based in part on factors such as injury type, occupation/industry, timescale used, length of follow-up, and how reinjury was defined (e.g., self-report, report to a supervisor/employer, reopened and/or newly filed WC claims, and whether restricted to injuries involving time loss compensation). Across studies using varied methods, the percentage of workers reinjured within one year has been estimated to be between 14% and 30%; for example: 18% to 22% among workers who had previously filed WC claims in Alberta, Canada (back injuries);10 26% among workers surveyed who had previously filed Washington State WC claims (back injuries);1 and 14% of a cohort of workers who had previously filed WC claims in Ontario, Canada (restricted to workers with temporary total disability and soft tissue musculoskeletal injuries).11 In a study using an employer-based surveillance database rather than WC claims, 20% of registered nurses and 30% of nursing assistants administratively reported an occupational injury/illness occurring within a year of an initial injury/illness report (Veterans Health Administration; not restricted to those involving time lost from work).4
Several other studies used longer timeframes to calculate work reinjury estimates. At two San Francisco, California hospitals, 36% of injured workers interviewed reported work reinjury within two years. In a Wisconsin WC-based study, 32% of injured workers had at least one further compensable time-loss claim during the three years following the initial claim.7 In a Colorado WC-based study, 27% of injured workers filed a second claim within five years.12 During 9 to 14 years of follow-up in an Australian WC-based study, 37% of persons with an initial claim filed a second claim.3 That study,3 and a WC-based Canadian study with 10 years of follow-up,13 also used average time to work reinjury as an alternative metric to percentages, estimating mean calendar time from initial injury to work reinjury as 1,088 days (nearly three years) and 744 days (just over two years), respectively.
While many injured workers are reinjured at work, reinjury risk is challenging to quantify, in part because accurate estimation of work reinjury risk is dependent on identifying an appropriate at-risk denominator. Few studies have estimated time-dependent work reinjury rates using at-risk denominators other than calendar time. Lipscomb et al (2008)2 found that back reinjury rates among 18,768 injured Washington State carpenters who had returned to work peaked between 1000 and 1500 hours worked (equivalent to two to three quarters of full-time work), but elevated rates persisted for three to four years after the initial work injury. Consistent with those findings, a Colorado WC study including all injury types found that most second claims occurred within three years.12
Most other studies have used a calendar timescale (e.g., amount of calendar time between initial injury and reinjury) to calculate reinjury rates. But workers who have not yet returned to work are not at risk of a subsequent work-related injury, and workers who are working part-time or intermittently would generally be at lower risk than full-time workers. Hence, this approach may underestimate risk by falsely assuming continuous employment during the calendar time period; and it also may not account for differences in work exposure between full-time and part-time workers. Given these issues, use of the calendar timescale may be particularly problematic when workers face challenges returning to work or tend not to work continuously or full-time, such as in the case of injured workers with a permanent impairment.
Every year In the United States, about 300,000 workers—roughly 10% of all workers injured at work, and 38% of workers with WC claims involving compensation for temporary wage loss or permanent disability—experience serious work injuries that result in permanent impairment and a permanent partial disability (PPD) award.14 WC-based PPD awards provide compensation for work-related permanent impairment that does not preclude returning to work but prevents working at full physical capacity (e.g., vision or hearing loss, amputation, spinal impairment). Permanent impairment puts workers at higher risk of both mortality15 and return-to-work challenges associated with functional disability, pain, and unstable health.16–21 In an earlier study, we found that at least 22% of Washington State injured workers had not returned to work, even briefly, during the year after their WC claim closed with a PPD award.22 Injured workers with permanent impairments account for a large share of WC-based vocational rehabilitation program participants, and accumulating evidence suggests that vocational rehabilitation programs and policies affect initial return to work and sustained employment in both positive and negative ways.19,23–25 Even after vocational retraining to facilitate returning to work, workers disabled by an occupational injury face substantial employment challenges.19
After initially returning to work, many injured workers with permanent impairment face return-to-work interruption (i.e., breaks in employment due to reinjury, unstable health, disability, lay-off, etc.).16 A study of Ontario injured workers with permanent impairment found long-term intermittent impacts on return to work; only half of these workers returned to work in a sustained manner.16 Among Canadian workers who were 50–64 years of age and had a permanent impairment, a higher (more severe) impairment rating was associated with earlier labor force exit.26 Compared to other workers, disabled workers have unemployment rates that are 50% higher, and they are more likely to work part-time and in entry-level jobs.27,28 Mostly due to these employment patterns, workers with permanent impairment have considerably larger earning losses compared to other workers.29–31 In sum, there is substantial evidence that injured workers with permanent impairment are less likely to be fully employed compared to other workers; thus, the use of a calendar timescale to calculate time at risk could lead to underestimates of work reinjury risk for these workers.
Few studies have assessed work reinjury rates among workers with work-related permanent impairment. However, findings from various sources suggest that these workers may be at higher risk of a subsequent work injury compared to other workers. First, numerous studies have associated disability with higher occupational injury risk and poorer injury outcomes, which would likely generalize to workers with a work-related permanent impairment. Workers with disabilities are more than twice as likely to incur work injuries as those without disabilities.18 In addition to being more common, occupational injuries are more severe and more costly among workers with hearing and visual impairments32–34 and other persistent disabilities.35–38 In research using data from the National Longitudinal Survey of Youth, having an early-onset (before age 23) health-limiting condition was one of the strongest predictors of recurrent occupational injury.39 Second, in a Washington State WC-based study, more than half of workers surveyed thought their permanent impairment put them at higher risk of being reinjured at work.22 Third, in a reinjury study using data from the Ontario Survey of Permanently Disabled Workers, about 50% of the 7,915 surveyed injured workers had at least one additional work absence related to the first injury.11 Although this estimate was not tied to a specific timeframe and did not include new work injuries, it was markedly higher than the reinjury estimates that were not specific to workers with permanent impairment (noted earlier). On the other hand, a Wisconsin study found that workers who received temporary total disability benefits were more likely to be reinjured (i.e., file a second WC claim) than those who received a PPD award.7
In summary, many injured workers are reinjured at work, but reinjury risk is challenging to quantify, and there are knowledge gaps with respect to potentially heightened reinjury risk faced by injured workers with a permanent impairment. Injured workers may face delayed return to work, or may return to work part-time or intermittently. A calendar timescale may overestimate time at risk (via the assumption of full employment during that time, or the assumption that the amount of calendar time spent working is comparable across groups), yielding underestimated reinjury rates and biased comparisons between groups having differential return-to-work patterns. In particular, calendar time might differentially overestimate time at risk for workers with permanent impairment, which would lead to underestimated reinjury risk estimates. In addressing this issue, state wage files—constructed from mandatory unemployment insurance-related employer tax and wage reports—provide an efficient but underused approach to identifying return-to-work patterns. In order to improve estimates of reinjury risk, we used state wage data to identify periods of employment and unemployment. The aims of this study were to: (1) estimate reinjury risk for workers by degree of permanent impairment; (2) estimate variation in reinjury risk by other worker, injury, and job characteristics, and by time since injury; and (3) assess whether choice of timescale (at-risk denominator) substantially affects reinjury risk estimates. We hypothesized that workers with work-related permanent impairment would be at elevated risk of reinjury compared to other injured workers, particularly in the first year after returning to work. Secondarily, we explored program-related outcomes for injured workers participating in vocational rehabilitation, many of whom have a work-related permanent impairment.
2. MATERIALS AND METHODS
2.1. Study setting
No-fault workers’ compensation coverage for work-related injuries and illnesses is compulsory in Washington State.40 The Washington State Department of Labor and Industries (L&I) is the exclusive State Fund insurer for about 70% of workers specified by Washington’s Industrial Insurance Act.41 Self-insured employers account for the remaining 30%; no private WC insurers operate in WA. L&I administers the state WC system for both State Fund and self-insured employers, and maintains population-based administrative databases of WC claims.42,43
2.2. Study design and cohort
We employed a retrospective cohort design, using administrative WC claims data along with state wage data to measure long-term reinjury outcomes and time at risk. The eligible cohort included injured workers with an accepted compensable State Fund WC claim that: (1) was their first known WC claim filed in Washington State (i.e., the worker had no prior State Fund or self-insured claim); and (2) closed for the first time during 2009 to 2017, whether or not it later reopened (i.e., if there were multiple claim closure dates for a claim, the first claim closure date was used to determine cohort eligibility). Injured workers with self-insured employers were not included in the eligible cohort, due to incomplete vocational rehabilitation and medical billing data for those WC claims.
Prior to delivering administrative data to the research team, L&I staff applied six exclusion criteria: (1) under age 18 when injured, (2) residence outside Washington State, (3) medical-only claims (<4 work days lost due to the injury, hence no time loss compensation), (4) fatal or total permanent disability claims, (5) confidentiality exclusions imposed by L&I (e.g., L&I employees), and (6) no valid Social Security number. After these exclusions, 4.01% (n=1842) had no state wage data before and after the injury, and were excluded during data analysis; these workers may have been self-employed or working in occupations exempt from unemployment insurance coverage and wage reporting requirements,44 and therefore it could not be assumed that absence of wages after the injury indicated no return to work. The resulting cohort consisted of 44,068 injured workers. This study was approved by the University of Washington Institutional Review Board. Informed consent requirements were waived for this study; administrative data provided to the researchers contained no direct identifiers.
2.3. Reinjury outcomes
After the eligible cohort was identified, further administrative data were obtained from L&I for these workers. These data included all WC claims with injury dates subsequent to the initial injury through the end of 2018, regardless of claim status (e.g., medical-only, fatal, total permanent disability), and included both State Fund and self-insured claims. The operational definition of reinjury included both reopened claims (likely reflecting aggravation, exacerbation or recurrence of the initial injury) and new claims (likely reflecting new injuries).45,46 This allowed for observation of reinjury outcomes for at least one year after the initial injury, and—depending on year of injury—up to 19 years.
2.4. Time at risk
State wage files from the Washington State Employment Security Department were used to construct at-risk denominators. These files include quarterly wages and hours worked for workers covered by unemployment insurance, which excludes self-employment and exempt occupations.44 For this study, L&I staff used Social Security numbers to link administrative WC claims with quarterly wage data, and then transmitted linked data, without identifiers, to our research team. Wages were adjusted to December 2018 dollars using the Consumer Price Index.
For comparison purposes, three at-risk timescales were used to measure time from initial injury to the first reinjury or censoring: (1) calendar quarters (i.e., observed calendar time, regardless of wages/hours worked); (2) any-wage quarters (i.e., excluding quarters with no wages, when presumably not at risk for work injury); and (3) full-time equivalent (FTE) quarters (i.e., cumulative work hours divided by 520—approximating quarters of full-time work). The latter two timescales used work-status measures (wages or hours) rather than calendar time to measure time at risk, and were not necessarily synchronous with calendar time. Because a few workers had an impossibly high number of hours worked in some quarters, work hours were winsorized at 2,190 hours per quarter—the maximum possible hours if working around the clock (i.e., workers with >2,190 hours per quarter were retained but the value for hours was recoded to this cap). In sensitivity analyses, this procedure had negligible impact on estimates. Data were censored on the earliest of three dates: (1) administrative follow-up end date (December 31, 2018), (2) total permanent disability effective date, or (3) date of death.
2.5. Permanent impairment and vocational rehabilitation programs
The primary predictor of interest was degree of permanent impairment, classified into three mutually exclusive groups based on the permanent impairment rating for the initial injury: (1) no permanent impairment (i.e., no PPD award), (2) a PPD award with whole body impairment (WBI) <10%, or (3) a PPD award with WBI ≥10%. Washington State defines impairment as permanent anatomic or functional abnormality or loss of function after maximum medical improvement has been achieved.47 For workers who have suffered a permanent loss of function but are still able to work, degree of impairment is rated prior to claim closure, after treatment has been completed.48 PPD awards are made at claim closure, and may be paid as a lump sum or in monthly installments, depending on the size of the award.48
Administrative WC PPD rating data were challenging to summarize. Several impairment rating/award systems were involved. In addition, multiple entries for the same PPD award were often indistinguishable as to whether they represented duplicate entries, multiple/bilateral injuries, pre-existing unpaid impairment based on evaluation, protests, repayments, or other subsequent increases or decreases in the PPD award. We constructed a measure of WBI that would allow us to compare workers based on a conservative estimate of WBI percentage, regardless of the rating system used to produce an individual worker’s rating or award. The resulting estimate can best be thought of as a lower bound estimate of WBI, based on the single largest contribution from the single impaired body part contributing most to WBI. A more detailed description of how WBI was constructed and classified can be found in an earlier publication.22
To explore program-related outcomes for injured workers participating in vocational rehabilitation, we estimated reinjury risk for two subsets of injured workers: (1) workers who completed a vocational retraining plan, compared to those who did not complete their plan; and (2) workers who chose self-directed retraining funds (known as Option 2), compared to those who chose a conventional retraining plan (whether completed or not). For these analyses, subgroup assignments were based on events occurring prior to the first claim closure date for the initial WC claim. To our knowledge, reinjury outcomes have not previously been assessed for either scenario. However, completion of an L&I-approved vocational rehabilitation training plan by an eligible injured worker is associated with faster return to work and better long-term employment outcomes, compared with workers who do not complete their plan.24,25 Option 2 became available as of January 1, 2008, as a voluntary alternative to participating in the approved conventional retraining plan. Workers have 15 days after plan approval to decide whether to participate in the approved plan or choose Option 2. When workers choose Option 2, their claim is closed, time-loss benefits end, a vocational award of roughly six to nine months of time-loss benefits is paid, and vocational retraining funds are set aside. The worker can access their vocational retraining funds for tuition, training fees, and certain related expenses for up to five years. The worker can seek training at any L&I-approved program or course, and the retraining goal can differ from that in the approved retraining plan.
2.6. Covariates
Worker and injury characteristics (i.e., gender, age at initial injury, preferred language, residence county, injured body part, comorbidities) were extracted from WC claims data. Urban-rural residence was based on the worker’s residence county, and was classified using the six-level 2013 National Center for Health Statistics Urban-Rural Classification Scheme for Counties.49 Injured body part was categorized as spine/neck, upper extremity, lower extremity, or other/multiple. For workers with a PPD award, body part was based on the impaired body part used for the WBI percentage estimate. For workers with no PPD award, body part was based on Occupational Injury and Illness Classification System (version 1.01) codes present in the WC claims file. We obtained professional and facility WC billing data for the first visit or admission for the initial injury, which was used to construct the Functional Comorbidity Index.50
Pre-injury quarterly wages were based on state wage data, averaged over the four quarters prior to the injury quarter, and adjusted to December 2018 dollars using the Consumer Price Index. Information about the job where the initial injury occurred included employer size, industry sector, and hazard group. Large employers were defined as those with ≥50 FTE workers during the injury quarter. Industry sector was based on North American Industry Classification System (NAICS) two-digit sector codes, but—due to small numbers in some sectors—was further collapsed into nine groups: (1) Agriculture, Forestry, Fishing, Hunting (NAICS sector: 11); (2) Construction, Utilities, Mining (NAICS sectors: 21, 22, 23); (3) Manufacturing (NAICS sectors: 31, 32, 33); (4) Retail/Wholesale Trade (NAICS sectors: 42, 44, 45); (5) Transportation, Warehousing (NAICS sectors: 48, 49); (6) Information, Finance, Real Estate, Professional (NAICS sectors: 51, 52, 53, 54, 55); (7) Administrative, Support, Other Services (NAICS sectors: 56, 81, 92); (8) Education, Health Care, Social Services (NAICS sectors: 61, 62); and (9) Arts, Entertainment, Hospitality (NAICS sectors: 71, 72). We also constructed a continuous hazard group variable based on L&I-assigned employer risk class; this was developed for WC insurance administration purposes, to estimate potential for loss (claim costs) by nature of business. Hazard group classifies employer risk from one (lowest risk) to nine (highest risk).51
2.7. Data analysis
All analyses were conducted using Stata/MP 15.1 for Windows (StataCorp, College Station, TX, USA).52 The amount of missing data was negligible (<1%) for all variables. We therefore used the subset of cases with complete data for all variables (retaining N=43,114 injured workers, or 97.8% of the eligible sample of 44,068 injured workers) for all analyses presented herein. This also ensured that comparisons across the three timescales would be based on the same sample (wages and hours were not always missing synchronously).
Unadjusted Kaplan-Meier survival curves were used to illustrate differences in the proportions of injured workers not reinjured, by degree of impairment and timescale. Survival functions were used to quantify the proportions of injured workers not reinjured for each timescale. Data presentation via Kaplan-Meier curves and survival function tables was limited to 60 quarters for all three timescales, because so few workers (<30) remained at risk beyond that point.
Rates of first reinjury per 100 worker-years were calculated by degree of impairment, using each of the three timescales. Reinjury rates were also calculated for each two-quarter interval after initial injury, in order to assess rate variation over time.
Unadjusted and adjusted Cox proportional hazard regression models were used to estimate reinjury risk by degree of permanent impairment; separate models were run using each of the three timescales. Adjusted models included all covariates described in Section 2.6 above, and were fully stratified by year of injury, which ran from 2003 to 2017 for this sample (i.e., coefficients were held equal across strata, but baseline hazards were unique to each injury year). Robust variance estimates were used to produce 95% confidence intervals (CI).
Parallel models were used to explore program-related outcomes for two subsets of injured workers participating in vocational rehabilitation. The first set of models estimated reinjury risk for injured workers who completed a vocational retraining plan versus those who did not complete their plan, among the subset of workers who: (1) had an approved vocational retraining plan for the initial injury, and (2) did not choose self-directed retraining funds (known as Option 2) in place of the approved conventional retraining plan (N=1,242). The second set of models estimated reinjury risk for injured workers selecting Option 2 versus a conventional retraining plan, among the subset of workers who: (1) had an approved vocational retraining plan for the initial injury, and (2) had access to Option 2, which was first offered January 1, 2008 (N=1,209).
3. RESULTS
In this sample, 74.0% had no PPD award, 19.5% were in the WBI <10% group and 6.5% were in the WBI ≥10% group (Table I). All characteristics in Table I were differentially distributed across these groups, to a statistically significant degree. For example, nearly half (48.1%) of those in the WBI ≥10% group had spine/neck injury compared to about a quarter (26.1%) overall. Compared to the WBI ≥10% group, the WBI <10% group had markedly higher percentages of upper and lower extremity injuries, and markedly lower percentages of spine/neck and other/multiple injuries. Spanish language preference applied to 19.9% of workers in the WBI ≥10% group, but only 12.0% of workers with no PPD award. Construction/utilities/mining was the most common industry category for the WBI ≥10% group (17.6%), but only accounted for 9.4% of workers with no PPD award.
TABLE I.
Worker, injury, job, and vocational rehabilitation characteristics, by degree of impairment (N=43,114)
| Variable | Total (N=43,114) |
No PPD award (n=31,912) |
WBI <10% (n=8,404) |
WBI ≥10% (n=2,798) |
||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Body part | ||||||||
| Spine/neck | 11,250 | 26.1 | 8,671 | 27.2 | 1,233 | 14.7 | 1,346 | 48.1 |
| Upper extremity | 14,273 | 33.1 | 9,195 | 28.8 | 4,418 | 52.6 | 660 | 23.6 |
| Lower extremity | 9,635 | 22.3 | 6,692 | 21.0 | 2,640 | 31.4 | 303 | 10.8 |
| Other/multiple | 7,956 | 18.5 | 7,354 | 23.0 | 113 | 1.3 | 489 | 17.5 |
| Gender | ||||||||
| Male | 24,497 | 56.8 | 17,841 | 55.9 | 4,980 | 59.3 | 1,676 | 59.9 |
| Female | 18,617 | 43.2 | 14,071 | 44.1 | 3,424 | 40.7 | 1,122 | 40.1 |
| Age | ||||||||
| 18–24 | 9,433 | 21.9 | 7,911 | 24.8 | 1,206 | 14.3 | 316 | 11.3 |
| 25–34 | 13,162 | 30.5 | 10,241 | 32.1 | 2,223 | 26.5 | 698 | 25.0 |
| 35–44 | 8,828 | 20.5 | 6,158 | 19.3 | 1,945 | 23.1 | 725 | 25.9 |
| 45–54 | 6,877 | 15.9 | 4,512 | 14.1 | 1,743 | 20.7 | 622 | 22.2 |
| 55–64 | 3,959 | 9.2 | 2,554 | 8.0 | 1,047 | 12.5 | 358 | 12.8 |
| ≥65 | 855 | 2.0 | 536 | 1.7 | 240 | 2.9 | 79 | 2.8 |
| Preferred language | ||||||||
| English | 35,817 | 83.1 | 27,113 | 85.0 | 6,544 | 77.9 | 2,160 | 77.2 |
| Spanish | 5,990 | 13.9 | 3,841 | 12.0 | 1,592 | 18.9 | 557 | 19.9 |
| Other | 1,207 | 3.0 | 958 | 3.0 | 268 | 3.2 | 81 | 2.9 |
| Urban-rural residence county | ||||||||
| Large central metropolitan | 11,487 | 26.6 | 8,878 | 27.8 | 2,059 | 24.5 | 550 | 19.7 |
| Large fringe metropolitan | 12,750 | 29.6 | 9,408 | 29.5 | 2,489 | 29.6 | 853 | 30.5 |
| Medium metropolitan | 8,202 | 19.0 | 6,036 | 18.9 | 1,587 | 18.9 | 579 | 20.7 |
| Small metropolitan | 5,820 | 13.5 | 4,023 | 12.6 | 1,293 | 15.4 | 504 | 18.0 |
| Micropolitan | 3,844 | 8.9 | 2,806 | 8.8 | 780 | 9.3 | 258 | 9.2 |
| Noncore | 1,011 | 2.4 | 761 | 2.4 | 196 | 2.3 | 54 | 1.9 |
| Employer size | ||||||||
| Small (<50 FTE employees) | 19,554 | 45.4 | 14,056 | 44.0 | 4,062 | 48.3 | 1,436 | 51.3 |
| Large (≥50 FTE employees) | 23,560 | 54.6 | 17,856 | 56.0 | 4,342 | 51.7 | 1,362 | 48.7 |
| Industry sector | ||||||||
| Agriculture, Forestry, Fishing, Hunting | 3,002 | 7.0 | 2,052 | 6.4 | 703 | 8.4 | 247 | 8.8 |
| Construction, Utilities, Mining | 4,747 | 11.0 | 2,987 | 9.4 | 1,268 | 15.1 | 492 | 17.6 |
| Manufacturing | 3,107 | 7.2 | 2,147 | 6.7 | 747 | 8.9 | 213 | 7.6 |
| Retail/Wholesale Trade | 6,794 | 15.7 | 5,099 | 16.0 | 1,297 | 15.4 | 398 | 14.2 |
| Transportation, Warehousing | 2,367 | 5.5 | 1,864 | 5.8 | 359 | 4.3 | 144 | 5.2 |
| Information, Finance, Real Estate, Professional | 2,798 | 6.5 | 2,029 | 6.4 | 590 | 7.0 | 179 | 6.4 |
| Administrative, Support, Other Services | 7,671 | 17.8 | 5,766 | 18.1 | 1,433 | 17.1 | 472 | 16.9 |
| Education, Health Care, Social Services | 7,108 | 16.5 | 5,561 | 17.4 | 1,147 | 13.6 | 400 | 14.3 |
| Arts, Entertainment, Hospitality | 5,520 | 12.8 | 4,407 | 13.8 | 860 | 10.2 | 253 | 9.0 |
| Vocational retraining plan subseta | (N=1,242) | (n=134) | (n=579) | (n=529) | ||||
| Plan not completed | 748 | 60.2 | 66 | 49.3 | 343 | 59.2 | 339 | 64.1 |
| Plan completed | 494 | 39.8 | 68 | 50.7 | 236 | 40.8 | 190 | 35.9 |
| Vocational retraining approach subsetb | (N=1,209) | (n=128) | (n=566) | (n=515) | ||||
| Conventional vocational retraining plan | 577 | 47.7 | 80 | 62.5 | 283 | 50.0 | 214 | 41.6 |
| Option 2: Self-directed retraining funds | 632 | 52.3 | 48 | 37.5 | 283 | 50.0 | 301 | 58.4 |
Note: All variables in Table I were significantly associated with degree of impairment (P<.001 for all variables, with exception of P=.006 for vocational retraining plan completion).
Abbreviations: FTE, full-time equivalent; PPD, permanent partial disability; WBI, whole body impairment.
Conditional on having an approved vocational retraining plan and not having selected Option 2.
Conditional on having an approved vocational retraining plan (completed or not completed) and availability of Option 2 before first claim closure.
Nearly 90% of the workers in each of the vocational rehabilitation program subsets had a permanent impairment (Table I). Over half (52.3%) of workers with an approved vocational retraining plan selected self-directed retraining funds (Option 2) in place of the conventional retraining plan; 58.4% of the WBI ≥10% group chose Option 2, compared to only 37.5% of those with no PPD award. Of workers with an approved vocational retraining plan (excluding those who chose Option 2), 39.8% completed their plan; 35.9% of the WBI ≥10% group completed their plan, compared to more than half (50.7%) of those with no PPD award.
The Functional Comorbidity Index ranged from 0 to 8, with more than 90% having no identified comorbidities; mean values were 0.07 (SD 0.31; 95% CI: 0.07, 0.08) for the no PPD award group, 0.09 (SD 0.33; 95% CI: 0.08, 0.09) for the WBI <10% group, and 0.18 (SD 0.52; 95% CI: 0.16, 0.20) for the WBI ≥10% group. Mean adjusted pre-injury quarterly wages were $6202 (SD $5846; 95% CI: $6138, $6266) for the no PPD award group, $7219 (SD $6730; 95% CI: $7075, $7363) for the WBI <10% group, and $7174 (SD $7080; 95% CI: 6912, $7437) for the WBI ≥10% group. Hazard group ranged from 1 to 9, with a mean of 3.70 (SD 2.27; 95% CI: 3.68, 3.73) for the no PPD award group, 4.08 (SD 2.41; 95% CI: 4.03, 4.13) for the WBI <10% group), and 4.36 (SD 2.50; 95% CI: 4.27, 4.45) for the WBI ≥10% group.
Unadjusted Kaplan-Meier survival curves were used to depict the proportion of injured workers not reinjured over time, by degree of impairment and for each timescale (Figure 1). When using the calendar timescale, workers with no PPD award appeared slightly more likely to be reinjured. When using timescales based on wages or hours worked, in contrast, degree of impairment sorted out in the hypothesized manner, i.e., workers with a higher degree of impairment were more likely to be reinjured.
FIGURE 1.
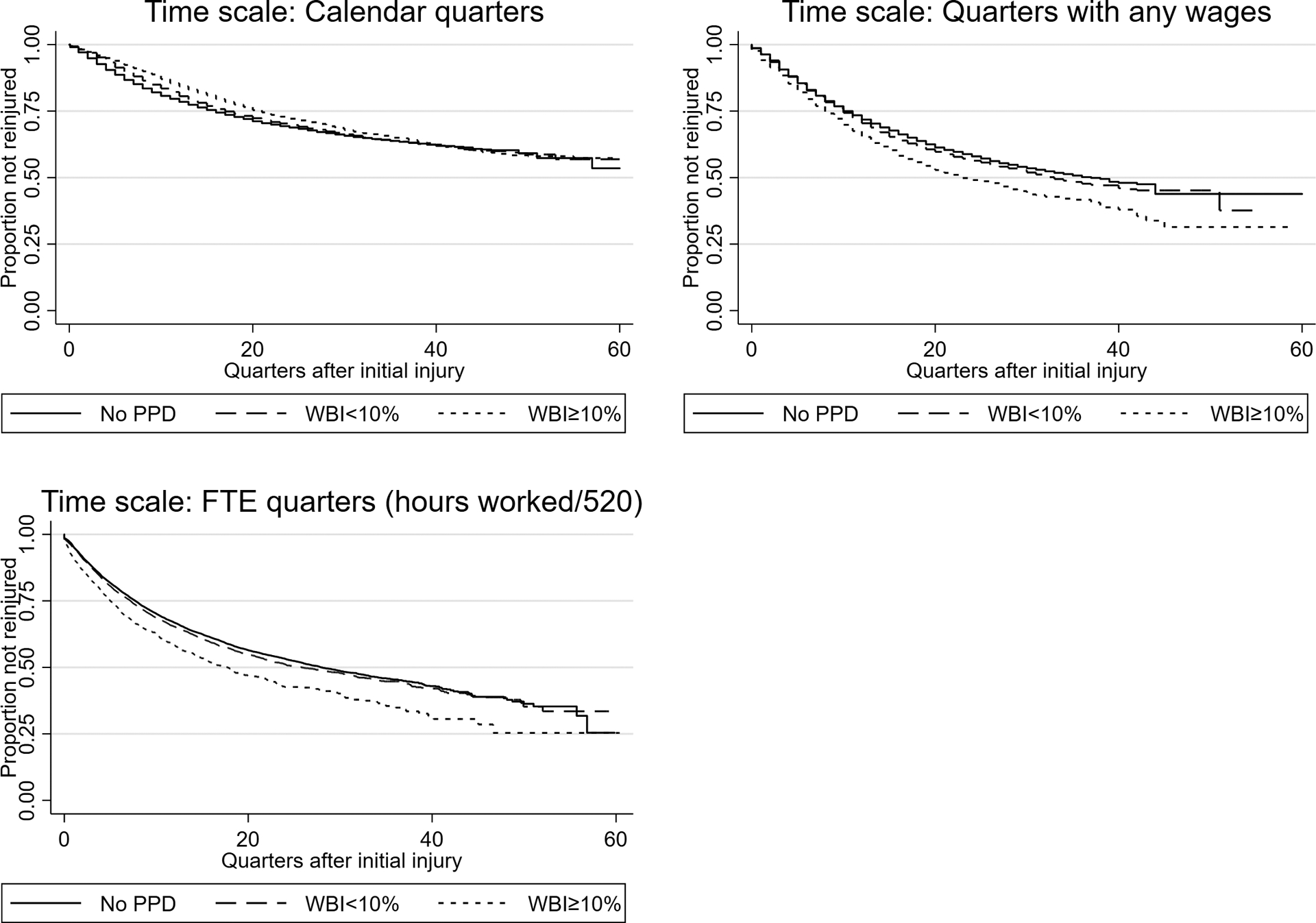
Unadjusted Kaplan-Meier survival curves (proportion of injured workers not reinjured), by degree of impairment and timescale. FTE, full-time equivalent; PPD, permanent partial disability; WBI, whole body impairment
Comparing survival functions by timescale provides a direct assessment of the difference between using calendar time versus more accurate measures of time at risk. Based on survival functions (Table II), 16% of all workers in our sample were reinjured within four FTE quarters (i.e., one year of full-time work) after initial injury, whereas it took an estimated eight calendar quarters (i.e., two calendar years) for the same percentage to be reinjured. At 15 years (60 quarters) of follow-up, fewer than half were estimated to be reinjured when using the calendar timescale, whereas nearly 70% were estimated to be reinjured when using the FTE timescale.
TABLE II.
Survival function (proportion of injured workers not reinjured), by timescale
| Quarter | Calendar quarters | Quarters with any wages | FTE quarters (hours worked/520) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N at risk |
Survival Function |
95% CI | N at risk |
Survival function |
95% CI | N at risk |
Survival function |
95% CI | |
| 0 | 43,114 | 1.00 | 43,114 | 1.00 | - | 43,114 | 1.00 | ||
| 1 | 42,733 | 0.97 | 0.97–0.98 | 41,060 | 0.96 | 0.96–0.96 | 36,165 | 0.95 | 0.95–0.95 |
| 4 | 40,232 | 0.91 | 0.91–0.92 | 33,704 | 0.88 | 0.88–0.88 | 27,283 | 0.84 | 0.84–0.84 |
| 8 | 35,590 | 0.85 | 0.84–0.85 | 25,123 | 0.78 | 0.78–0.79 | 18,915 | 0.74 | 0.73–0.74 |
| 12 | 30,161 | 0.79 | 0.79–0.80 | 18,272 | 0.71 | 0.71–0.72 | 13,114 | 0.66 | 0.66–0.67 |
| 24 | 17,080 | 0.69 | 0.69–0.70 | 6,450 | 0.57 | 0.57–0.58 | 4,299 | 0.52 | 0.52–0.53 |
| 36 | 6,930 | 0.63 | 0.63–0.64 | 1,332 | 0.49 | 0.48–0.50 | 1,008 | 0.45 | 0.44–0.46 |
| 48 | 576 | 0.59 | 0.58–0.60 | 38 | 0.44 | 0.42–0.46 | 146 | 0.38 | 0.37–0.40 |
| 60 | 12 | 0.56 | 0.54–0.58 | 1 | 0.41 | 0.36–0.47 | 28 | 0.34 | 0.30–0.37 |
Abbreviations: CI, confidence interval; FTE, full-time equivalent.
Using any of the three timescales, rates of first reinjury per 100 worker-years were highest in the first two quarters after initial injury (Figure 2). These elevated reinjury rates (nearly double the long-term rates shown in Table III) gradually decreased, and then leveled off after about four years.
FIGURE 2.
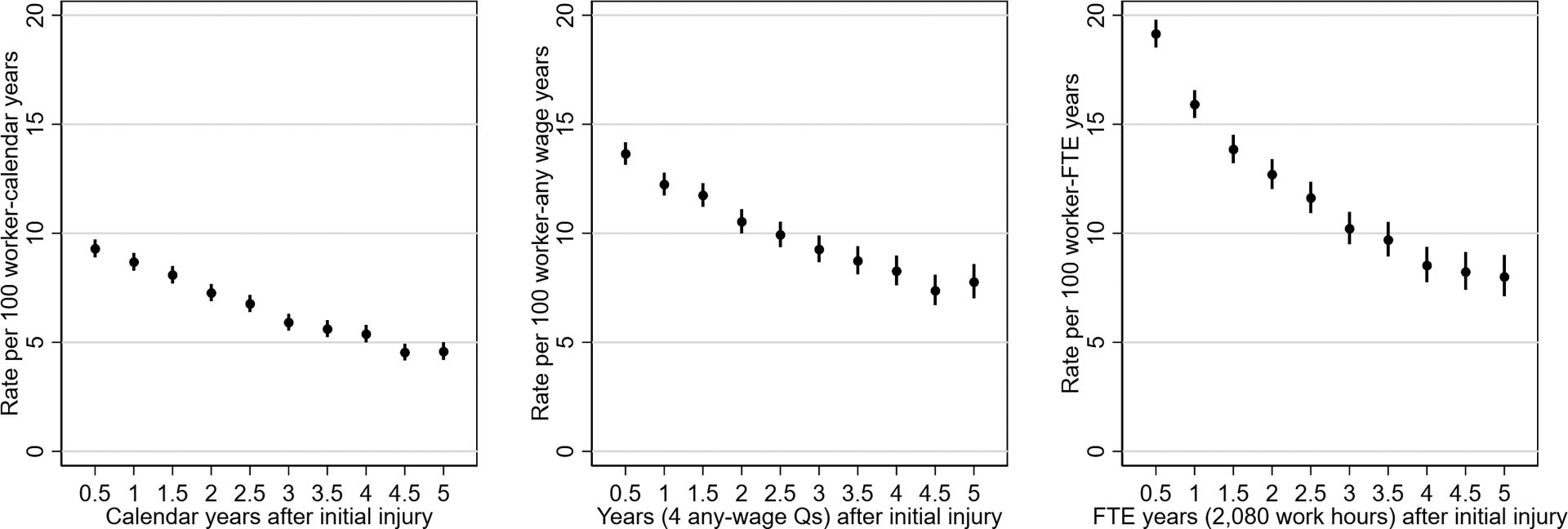
Time-varying rate of first reinjury per 100 worker-years during the first five years (20 quarters) after initial injury, by timescale. FTE, full-time equivalent; Q, quarter
TABLE III.
Time from initial injury to first reinjury, and rate of first reinjury per 100 worker-years, by degree of impairment and timescale
| Impairment | N | Calendar quarters | Quarters with any wages | FTE quarters (hours worked/520) | |||
|---|---|---|---|---|---|---|---|
| P25 (95% CI) | Rate (95% CI) | P25 (95% CI) | Rate (95% CI) | P25 (95% CI) | Rate (95% CI) | ||
| Overall | 43,114 | 17 (16–17) | 5.9 (5.8–6.0) | 10 (10–11) | 10.0 (9.9–10.2) | 7.4 (7.2–7.6) | 12.5 (12.3–12.7) |
| No PPD | 31,912 | 16 (15–16) | 6.1 (6.0–6.3) | 11 (10–11) | 9.8 (9.6–10.0) | 7.7 (7.5–8.0) | 12.2 (12.0–12.5) |
| WBI <10% | 8,404 | 17 (16–18) | 5.5 (5.3–5.7) | 10 (10–11) | 10.1 (9.7–10.4) | 7.2 (6.8–7.6) | 12.4 (12.0–12.9) |
| WBI ≥10% | 2,798 | 21 (19–23) | 4.9 (4.6–5.2) | 8 (8–9) | 12.7 (11.9–13.5) | 5.0 (4.6–5.6) | 16.8 (15.7–17.9) |
Note: The 25th percentile was used for this table because the median was not observed for calendar quarters (i.e., <50% of injured workers were reinjured during follow-up).
Abbreviations: CI, confidence interval; FTE, full-time equivalent; P25, 25th percentile; PPD, permanent partial disability; WBI, whole body impairment.
Estimated time from initial injury to first reinjury at the 25th percentile, and rate of first reinjury per 100 worker-years are presented in Table III, by degree of impairment and timescale. (The 25th percentile was used because the median was not observed for calendar quarters, i.e., <50% of injured workers were reinjured during follow-up.) When using the calendar timescale, we found that workers with the highest degree of impairment had the longest estimated time to reinjury and the lowest overall reinjury rate. On the other hand, using timescales based on wages or hours worked generated findings in accord with our hypothesis that, when accounting for work-time at risk, higher degrees of impairment would be associated with shorter times to reinjury and higher overall reinjury rates.
For each timescale in turn, we used unadjusted and adjusted regression models to estimate reinjury risk by degree of permanent impairment (Table IV). In unadjusted models, when using the calendar timescale, both subgroups of workers with PPD awards (WBI <10% and WBI ≥10%) were estimated to have a lower reinjury risk than workers without a PPD award. After adjusting for covariates, reinjury risk no longer appeared to differ across the three groups. However, a very different picture emerged when using timescales based on any-wage or FTE quarters. Those models, whether unadjusted or adjusted, evidenced a significant monotonic trend of increasing reinjury risk as degree of impairment increased. Covariate adjustment was not enough to reveal this pattern—adjustment for time at risk via timescale choice was more important. Similarly, choice of timescale markedly affected other subgroup comparisons of reinjury risk, including those based on Functional Comorbidity Index, age, and pre-injury wages (Table IV).
TABLE IV.
Unadjusted and adjusted regression models of reinjury risk, by timescale (N=43,114)
| Characteristic/Model | Calendar quarters | Quarters with any wages | FTE quarters (hours worked/520) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | HR | 95% CI | Pa | HR | 95% CI | Pa | HR | 95% CI | Pa |
| Impairment (Ref: No PPD award) | .001 | <.001 | <.001 | ||||||
| WBI <10% | 0.95 | 0.91–0.99 | 1.05 | 1.01–1.09 | 1.05 | 1.01–1.10 | |||
| WBI ≥10% | 0.90 | 0.84–0.96 | 1.29 | 1.21–1.38 | 1.37 | 1.28–1.47 | |||
| Adjusted | HR | 95% CI | Pa | HR | 95% CI | Pa | HR | 95% CI | Pa |
| Impairment (Ref: No PPD award) | .947 | <.001 | <.001 | ||||||
| WBI <10% | 1.00 | 0.95–1.05 | 1.06 | 1.01–1.11 | 1.08 | 1.03–1.13 | |||
| WBI ≥10% | 1.00 | 0.92–1.06 | 1.26 | 1.18–1.36 | 1.34 | 1.25–1.44 | |||
| Body part (Ref: Spine/neck) | .423 | .005 | .004 | ||||||
| Upper extremity | 0.99 | 0.94–1.03 | 0.94 | 0.90–0.98 | 0.94 | 0.89–0.98 | |||
| Lower extremity | 0.97 | 0.92–1.02 | 0.92 | 0.87–0.97 | 0.92 | 0.87–0.96 | |||
| Other/multiple | 0.96 | 0.91–1.01 | 0.95 | 0.90–1.00 | 0.95 | 0.90–1.00 | |||
| Functional Comorbidity Index | 0.93 | 0.88–0.99 | .017 | 0.97 | 0.92–1.03 | .364 | 0.98 | 0.92–1.04 | .405 |
| Female (Ref: Male) | 0.85 | 0.82–0.89 | <.001 | 0.84 | 0.81–0.88 | <.001 | 0.91 | 0.87–0.94 | <.001 |
| Age (Ref: 18–24) | <.001 | <.001 | .004 | ||||||
| 25–34 | 0.93 | 0.88–0.97 | 1.02 | 0.97–1.06 | 1.01 | 0.97–1.06 | |||
| 35–44 | 0.95 | 0.91–1.01 | 1.09 | 1.03–1.15 | 1.09 | 1.04–1.16 | |||
| 45–54 | 0.88 | 0.83–0.93 | 1.04 | 0.98–1.10 | 1.04 | 0.98–1.11 | |||
| 55–64 | 0.74 | 0.68–0.80 | 0.95 | 0.88–1.02 | 1.00 | 0.93–1.08 | |||
| ≥65 | 0.45 | 0.38–0.54 | 0.70 | 0.59–0.83 | 0.87 | 0.73–1.04 | |||
| Preferred language (Ref: English) | <.001 | <.001 | <.001 | ||||||
| Spanish | 1.14 | 1.08–1.20 | 1.19 | 1.12–1.25 | 1.11 | 1.05–1.17 | |||
| Other | 0.81 | 0.73–0.91 | 0.80 | 0.71–0.90 | 0.74 | 0.66–0.83 | |||
| Urban-rural residence county (Ref: Large central metropolitan) | .025 | <.001 | <.001 | ||||||
| Large fringe metropolitan | 1.06 | 1.01–1.11 | 1.09 | 1.04–1.14 | 1.10 | 1.05–1.15 | |||
| Medium metropolitan | 1.05 | 1.00–1.11 | 1.07 | 1.01–1.12 | 1.08 | 1.03–1.14 | |||
| Small metropolitan | 1.01 | 0.95–1.07 | 1.00 | 0.94–1.06 | 1.02 | 0.96–1.08 | |||
| Micropolitan | 0.99 | 0.92–1.06 | 0.98 | 0.92–1.05 | 0.99 | 0.92–1.06 | |||
| Noncore | 0.93 | 0.82–1.05 | 1.00 | 0.89–1.14 | 1.04 | 0.92–1.19 | |||
| Pre-injury wages ($10,000 increments) | 1.05 | 1.03–1.08 | <.001 | 0.82 | 0.80–0.85 | <.001 | 0.69 | 0.67–0.72 | <.001 |
| Large employer (Ref: Small employer) | 1.22 | 1.17–1.26 | <.001 | 1.16 | 1.12–1.21 | <.001 | 1.13 | 1.09–1.17 | <.001 |
| Industry sector (Ref: Information, Finance, Real Estate, Professional) | <.001 | <.001 | <.001 | ||||||
| Agriculture, Forestry, Fishing, Hunting | 1.18 | 1.06–1.31 | 1.21 | 1.09–1.35 | 1.20 | 1.08–1.34 | |||
| Construction, Utilities, Mining | 1.08 | 0.98–1.19 | 1.14 | 1.04–1.26 | 1.22 | 1.11–1.34 | |||
| Manufacturing | 1.34 | 1.22–1.47 | 1.33 | 1.21–1.46 | 1.28 | 1.17–1.41 | |||
| Retail/Wholesale Trade | 1.13 | 1.04–1.23 | 1.11 | 1.02–1.21 | 1.09 | 1.00–1.19 | |||
| Transportation, Warehousing | 1.24 | 1.12–1.38 | 1.30 | 1.18–1.44 | 1.28 | 1.15–1.42 | |||
| Administrative, Support, Other Services | 1.15 | 1.06–1.25 | 1.20 | 1.11–1.30 | 1.22 | 1.12–1.32 | |||
| Education, Health Care, Social Services | 1.27 | 1.17–1.38 | 1.25 | 1.15–1.36 | 1.24 | 1.14–1.35 | |||
| Arts, Entertainment, Hospitality | 1.13 | 1.03–1.24 | 1.13 | 1.03–1.24 | 1.17 | 1.06–1.28 | |||
| Hazard group | 1.03 | 1.02–1.04 | 1.04 | 1.03–1.05 | 1.04 | 1.03–1.05 | |||
Note: In addition to covariates shown, models were fully stratified by year of initial injury (baseline hazard unique to each year).
Abbreviations: CI, confidence interval; FTE, full-time equivalent; HR, hazard ratio; PPD, permanent partial disability; Ref, reference category; WBI, whole body impairment.
P value on referent line reflects joint test for set of categories within variable
We used the regression models described previously to estimate associations between two aspects of vocational rehabilitation program participation and reinjury risk. Adjusted models included all covariates presented in Table IV, and also included the specified vocational rehabilitation variable (Table V). We found that workers who completed a vocational retraining plan were significantly and substantially less likely to be reinjured, compared to those who did not complete their plan (Table V). In addition, we found that workers who chose self-directed retraining funds (Option 2) were significantly and substantially more likely to be reinjured, compared to those who chose a conventional retraining plan (Table V). Although all three timescales resulted in the same direction of effect for both vocational factors, the adjusted models resulted in statistically significant associations when using timescales based on any-wage or FTE quarters, but not when using calendar time. Estimated effect sizes were largest when using the FTE quarters timescale.
TABLE V.
Unadjusted and adjusted regression models of reinjury risk for injured workers participating in vocational rehabilitation, by timescale
| Subset/Model | Calendar quarters | Quarters with any wages | FTE quarters (hours worked/520) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P | HR | 95% CI | P | HR | 95% CI | P | |
| Completed vocational retraining plan (Ref: Approved plan not completed) | |||||||||
| Unadjusted (N=1,242a) | 0.77 | 0.62–0.97 | .026 | 0.72 | 0.58–0.90 | .004 | 0.68 | 0.55–0.86 | .001 |
| Adjustedb (N=1,242a) | 0.83 | 0.65–1.06 | .134 | 0.72 | 0.56–0.92 | .009 | 0.68 | 0.53–0.88 | .003 |
| Option 2: Self-directed retraining funds (Ref: Conventional vocational retraining plan) | |||||||||
| Unadjusted (N=1,209c) | 1.29 | 1.03–1.62 | .026 | 1.45 | 1.16–1.82 | .001 | 1.58 | 1.26–1.98 | <.001 |
| Adjustedb (N=1,209c) | 1.23 | 0.95–1.59 | .116 | 1.50 | 1.15–1.95 | .003 | 1.66 | 1.27–2.17 | <.001 |
Abbreviations: CI, confidence interval; FTE, full-time equivalent; HR, hazard ratio; Ref, reference category.
Conditional on having an approved vocational retraining plan and not having selected Option 2.
Adjusted models included the same variables as shown for the adjusted models in Table IV.
Conditional on having an approved vocational retraining plan (completed or not completed) and availability of Option 2 before first claim closure.
4. DISCUSSION
In this study, we demonstrated the importance of using a timescale that reflects work-time at risk (versus calendar time) when estimating reinjury risk, which is particularly important for workers who work less than full-time or have employment interruptions, and when comparing groups of workers with differential employment patterns. We found that choice of timescale markedly affected rate estimation, even for our full cohort of injured workers. Overall reinjury rates nearly doubled when using hours worked (12.5 per 100 worker-years) compared to using calendar time (5.9 per 100 worker-years). Using any-wage quarters gave an intermediate estimate that was more similar to hours worked than to calendar time (10.0 per 100 worker-years); using any-wage quarters may be a reasonable alternative to using hours worked, depending on characteristics of a particular state’s wage files.
In contrast to regression models based on calendar time, regression models based on any-wage or FTE quarters evidenced a significant monotonic trend of increased reinjury risk as degree of impairment increased. Covariate adjustment was not enough to reveal this pattern—adjustment for time at risk via timescale choice was more important. In line with our hypothesis, workers with ≥10% WBI (compared to workers with no PPD award) had an estimated 34% higher risk of reinjury when using hours worked; no difference was detected when using calendar time. This stands in contrast to a study by Gotz et al (2000),7 who found that Wisconsin workers with a PPD award were less likely to be reinjured compared to other Wisconsin workers, even after excluding quarters with no wages from the denominator (comparable to our any-wage quarter timescale). The reason for the difference in findings is unclear. Although Gotz et al did not distinguish subgroups based on degree of impairment, this would not account for the difference, as we observed increased reinjury risk among workers with any degree of permanent impairment. One notable difference was that Gotz et al excluded aggravations of the initial injury (reopened WC claims), focusing instead on unrelated new WC claims; however, compared to workers with an injury involving only temporary disability, workers with permanent impairment may be more likely to have aggravations/exacerbations of their existing injury, rather than an unrelated new injury.
Our finding of elevated reinjury risk among workers with permanent impairment comports with findings from a related survey, which revealed that more than half of respondents thought their permanent impairment put them at higher risk of being reinjured at work, compared to pre-injury (65.2%), or compared to coworkers in the same job (54.4%).22 The importance of our findings regarding elevated reinjury risk extends beyond workers who have filed WC claims; functional limitations are highly prevalent in the workplace, affecting as many as 22% of employed U.S. workers.53
In addition to permanent impairment, findings related to several other subgroup comparisons reinforce the importance of timescale choice. For example, when using calendar time, there appeared to be a monotonic trend of lower reinjury risk with increasing age, compared to ages 18–24, but this changed using other timescales. Of particular note, reinjury risk for older workers was markedly underestimated using calendar time and, importantly, also using any-wage quarters. This may be due to the much higher prevalence of part-time work in this age group.54 In another example, having more comorbidities (as measured by the Functional Comorbidity Index), was significantly associated with lower reinjury risk when using a calendar timescale; however, this association was no longer substantial nor significant when using any-wage or FTE quarters. In a study of injured workers in Colorado, Schwatka et al (2018)5 found that certain comorbidities were associated with lower odds of a future WC claim; they did not control for amount of work-time at risk during the follow-up period, which may have contributed to that finding.
Reinjury outcomes for injured workers participating in WC vocational rehabilitation programs were of particular interest because nearly 90% of these workers had a work-related permanent impairment. We found that workers who completed their approved vocational retraining plan were significantly and substantially less likely to be reinjured, compared to those who did not complete their plan. In addition, we found that workers who chose self-directed retraining funds (Option 2) were significantly and substantially more likely to be reinjured, compared to those who chose a conventional retraining plan. These findings merit further inquiry to understand the underlying mechanisms, especially as these programs operate at the WC system level and thus could have important impacts on the health and safety of a large number of workers.
Another important finding relates to the variation in reinjury risk over time. Using any of the three timescales, rates of first reinjury per 100 worker-years were highest in the first two quarters after initial injury—nearly double the longer-term rates. Reinjury rates gradually decreased over time since initial injury, and then leveled off after about four years. These findings identify the first six months after returning to work as a particularly important window of opportunity for prevention efforts, but it is also important to note that elevated risk persists for years. In accord with our findings, Lipscomb et al (2008)2 found that carpenters with back injuries remained at elevated reinjury risk for over three years after their initial injury.
Strengths of this study included the large cohort, for which the first-known WC claim filed in Washington State could be identified. Assembling the cohort based on the first-known WC claim allowed for definitive identification of the PPD rating with the initial injury; for subsequent claims, the PPD rating can reflect adjustment of a rating from a prior injury that caused permanent impairment—a circumstance that would not be clearly distinguishable using the available WC claims data. Washington State is one of only four states with no private WC insurers, which facilitates population-based research.42,43 In addition, access to state wage files enabled us to avoid conflating the end of time loss compensation with actual return to work, thereby avoiding an inherent limitation of reinjury studies that rely solely on WC claims data and do not measure employment directly.3,8,13,55 Though common practice, using the end of time loss compensation as a proxy for return to work leads to underestimation of time lost from work,56 as well as to underestimation of reinjury rates via inflated at-risk denominators. State wage files are an efficient but underused approach for identifying return-to-work patterns.57 In a unique back reinjury study, person-hours of work based on union carpenter work records were used to measure time at risk, but this approach is not feasible for statewide or cross-sector studies.2 Using wage files, we were able to measure time worked (and thus reinjury rates) even while the initial WC claim was open, and irrespective of time loss payments.
This study also had several limitations. First, identification of reinjury relied on reopening or filing a WC claim, and many work-related injuries are not reported to WC, particularly among workers 65 and older.58–60 This limitation may have been mitigated by the fact that this cohort of workers had already filed an initial WC claim. However, reinjury definitions based on WC claims generally result in lower risk estimates compared to definitions based on recurrence of pain or health care utilization;61 as such, our reinjury estimates are likely to be conservative. Second, the accuracy of the hours-worked data in the wage files is unclear. Fortunately, use of any-wage quarters resulted in estimates closer to those using hours worked than those using calendar quarters, and may be a reasonable alternative when hours worked are unavailable or data quality is suspect. Third, state wage files do not capture earnings for workers who are self-employed or work in exempt occupations.44 A study based on the Current Population Survey found that self-employment rates were higher among workers with limitations, compared to workers without limitations, and the self-employment differential also increased with education and age.62 Such differential inclusion in wage files may have affected our reinjury estimates for permanent impairment and age subgroups, to an unknown degree. Finally, all covariates were also based on administrative data, and thus have measurement limitations (e.g., the WBI variable was essentially a lower bound estimate,22 and the Functional Comorbidity Index was almost certainly underestimated, because diagnoses unrelated to the WC injury may not be reported to WC for billing purposes50).
5. CONCLUSIONS
Linking state wage data to WC claims facilitates measurement of long-term employment patterns, yielding more accurate reinjury estimates. Choice of timescale substantially affects reinjury estimates and comparisons between groups with differential return-to-work patterns. We found that overall reinjury rates nearly doubled when using hours worked, compared to using calendar time. Using hours worked, workers with ≥10% WBI had a 34% higher risk of reinjury, relative to workers with no PPD award; no such difference was detected using calendar time. Choice of timescale also had substantial impact on comparisons by age category and by number of comorbidities. This study identified the first six months after returning to work as a particularly important window of opportunity for prevention efforts, though elevated reinjury risk persisted for about four years.
Acknowledgments:
We thank Research and Data Services personnel at the Washington State Department of Labor and Industries, specifically Lisann Rolle, Program Manager, and Sarah West, Data Analyst, for facilitating access to the necessary administrative data and providing extensive data documentation.
Funding:
Grant sponsor: National Institute for Occupational Safety and Health (NIOSH); Grant number: R21OH011355.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute for Occupational Safety and Health.
Disclosure (Authors): The authors declare no conflicts of interest.
Institution and Ethics approval and informed consent: This study was approved by the University of Washington Institutional Review Board. Informed consent requirements were waived for this study; administrative data provided to the researchers contained no direct identifiers.
Data Availability Statement: Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1.Keeney BJ, Turner JA, Fulton-Kehoe D, Wickizer TM, Chan KC, Franklin GM. Early predictors of occupational back reinjury: results from a prospective study of workers in Washington State. Spine (Phila Pa 1976). 2013;38(2):178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipscomb HJ, Cameron W, Silverstein B. Incident and recurrent back injuries among union carpenters. Occup Environ Med. 2008;65(12):827–834. [DOI] [PubMed] [Google Scholar]
- 3.Ruseckaite R, Collie A. Repeat workers’ compensation claims: risk factors, costs and work disability. BMC Public Health. 2011;11:492–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Welch CE 3rd. Long-term risk of repeat occupational injury or illness incidents among Veterans Health Administration nursing employees. AAOHN J. 2010;58(8):323–329. [DOI] [PubMed] [Google Scholar]
- 5.Schwatka NV, Shore E, Atherly A, et al. Reoccurring injury, chronic health conditions, and behavioral health: gender differences in the causes of workers’ compensation claims. J Occup Environ Med. 2018;60(8):710–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SJ, You D, Gillen M, Blanc PD. Psychosocial work factors in new or recurrent injuries among hospital workers: a prospective study. Int Arch Occup Environ Health. 2015;88(8):1141–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gotz GA, Liu T, Galizzi M. Predictors of Multiple Workers’ Compensation Claims in Wisconsin. Cambridge, Mass: Workers Compensation Research Institute;2000. [Google Scholar]
- 8.Ruseckaite R, Collie A. The incidence and impact of recurrent workplace injury and disease: a cohort study of WorkSafe Victoria, Australia compensation claims. BMJ Open. 2013;3(3):e002396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wasiak R, Kim J, Pransky G. Work disability and costs caused by recurrence of low back pain: longer and more costly than in first episodes. Spine (Phila Pa 1976). 2006;31(2):219–225. [DOI] [PubMed] [Google Scholar]
- 10.Gross DP, Battie MC. Predicting timely recovery and recurrence following multidisciplinary rehabilitation in patients with compensated low back pain. Spine (Phila Pa 1976). 2005;30(2):235–240. [DOI] [PubMed] [Google Scholar]
- 11.Campolieti M Recurrence in workers’ compensation claims: estimates from a multiple spell hazard model. Journal of Risk and Uncertainty. 2001;23(1):75–94. [Google Scholar]
- 12.Keteyian C, Schwatka N, Dally M, et al. The impact of industry and body part injured on repeat workers’ compensation claims. Am J Ind Med. 2019;62(8):680–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cherry NM, Sithole F, Beach JR, Burstyn I. Second WCB claims: who is at risk? Can J Public Health. 2010;101 Suppl 1:S53–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiss E, Murphy G, Boden LI. Workers’ Compensation: Benefits, Costs, and Coverage (2017 data). Washington, DC: National Academy of Social Insurance; 2019. [Google Scholar]
- 15.Scott-Marshall HK, Tompa E, Wang Y, Liao Q. Long-term mortality risk in individuals with permanent work-related impairment. Can J Public Health. 2014;105(5):e330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Butler R, Johnson W, Baldwin M. Managing work disability: why first return to work is not a measure of success. Industrial and Labor Relations Review. 1995;48(3):452–469. [Google Scholar]
- 17.Young AE. Return to work following disabling occupational injury--facilitators of employment continuation. Scand J Work Environ Health. 2010;36(6):473–483. [DOI] [PubMed] [Google Scholar]
- 18.Price J, Shi J, Lu B, et al. Nonoccupational and occupational injuries to US workers with disabilities. Am J Public Health. 2012;102(9):e38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacEachen E, Kosny A, Ferrier S, et al. The ‘ability’ paradigm in vocational rehabilitation: challenges in an Ontario injured worker retraining program. J Occup Rehabil. 2012;22(1):105–117. [DOI] [PubMed] [Google Scholar]
- 20.de Jong M, de Boer AG, Tamminga SJ, Frings-Dresen MH. Quality of working life issues of employees with a chronic physical disease: a systematic review. J Occup Rehabil. 2015;25(1):182–196. [DOI] [PubMed] [Google Scholar]
- 21.Casey R, Ballantyne PJ. Diagnosed chronic health conditions among injured workers with permanent impairments and the general population. J Occup Environ Med. 2017;59(5):486–496. [DOI] [PubMed] [Google Scholar]
- 22.Sears JM, Schulman BA, Fulton-Kehoe D, Hogg-Johnson S. Workforce reintegration after work-related permanent impairment: a look at the first year after workers’ compensation claim closure. J Occup Rehabil. Online First: July 10, 2020; doi: 10.1007/s10926-020-09912-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacEachen E, Kosny A, Ferrier S, Chambers L. The “toxic dose” of system problems: why some injured workers don’t return to work as expected. J Occup Rehabil. 2010;20(3):349–366. [DOI] [PubMed] [Google Scholar]
- 24.Sears JM, Wickizer TM. Evaluation of the Vocational Rehabilitation Pilot Program Report to the Washington State Legislature as required by ESSB 5920 (Chapter 72, Laws of 2007). Tumwater, WA: Washington State Department of Labor and Industries;2012. [Google Scholar]
- 25.Sears JM, Wickizer TM, Schulman BA. Improving vocational rehabilitation services for injured workers in Washington State. Evaluation and Program Planning. 2014;44:26–35. [DOI] [PubMed] [Google Scholar]
- 26.Scott KA, Liao Q, Fisher GG, Stallones L, DiGuiseppi C, Tompa E. Early labor force exit subsequent to permanently impairing occupational injury or illness among workers 50–64 years of age. Am J Ind Med. 2018;61(4):317–325. [DOI] [PubMed] [Google Scholar]
- 27.Organisation for Economic Co-operation and Development (OECD). Sickness, Disability and Work: Breaking the Barriers A Synthesis of Findings across OECD Countries. Paris: OECD Publishing; 2010. [Google Scholar]
- 28.Kaye HS. Stuck at the bottom rung: occupational characteristics of workers with disabilities. J Occup Rehabil. 2009;19(2):115–128. [DOI] [PubMed] [Google Scholar]
- 29.Boden LI, Galizzi M. Economic consequences of workplace injuries and illnesses: lost earnings and benefit adequacy. Am J Ind Med. 1999;36(5):487–503. [DOI] [PubMed] [Google Scholar]
- 30.Reville RT, Schoeni RF. Disability from Injuries at Work: The Effects on Earnings and Employment. DRU-2554. Santa Monica, CA: RAND;2001. [Google Scholar]
- 31.Seabury SA, Scherer E, O’Leary P, Ozonoff A, Boden L. Using linked federal and state data to study the adequacy of workers’ compensation benefits. Am J Ind Med. 2014;57(10):1165–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zwerling C, Sprince NL, Davis CS, Whitten PS, Wallace RR, Heeringa SG. Occupational injuries among older workers with disabilities: a prospective cohort study of the Health and Retirement Survey, 1992 to 1994. Am J Public Health. 1998;88(11):1691–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zwerling C, Sprince NL, Wallace RB, Davis CS, Whitten PS, Heeringa SG. Risk factors for occupational injuries among older workers: an analysis of the Health and Retirement Study. Am J Public Health. 1996;86(9):1306–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zwerling C, Whitten PS, Davis CS, Sprince NL. Occupational injuries among older workers with visual, auditory, and other impairments. A validation study. J Occup Environ Med. 1998;40(8):720–723. [DOI] [PubMed] [Google Scholar]
- 35.Shi J, Gardner S, Wheeler KK, et al. Characteristics of nonfatal occupational injuries among U.S. workers with and without disabilities. Am J Ind Med. 2015;58(2):168–177. [DOI] [PubMed] [Google Scholar]
- 36.Shi J, Wheeler KK, Lu B, Bishai DM, Stallones L, Xiang H. Medical expenditures associated with nonfatal occupational injuries among U.S. workers reporting persistent disabilities. Disabil Health J. 2015;8(3):397–406. [DOI] [PubMed] [Google Scholar]
- 37.Harcombe H, Derrett S, Samaranayaka A, Davie G, Wyeth E, Wilson S. Factors predictive of subsequent injury in a longitudinal cohort study. Inj Prev. 2014;20(6):393–400. [DOI] [PubMed] [Google Scholar]
- 38.Harcombe H, Davie G, Wyeth E, Samaranayaka A, Derrett S. Injury upon injury: a prospective cohort study examining subsequent injury claims in the 24 months following a substantial injury. Inj Prev. 2018;24(6):437–444. [DOI] [PubMed] [Google Scholar]
- 39.Galizzi M On the recurrence of occupational injuries and workers’ compensation claims. Health Econ. 2013;22(5):582–599. [DOI] [PubMed] [Google Scholar]
- 40.Rothkin K Workers’ Compensation Laws as of January 1, 2019. WC-19–22 Cambridge, Mass: Workers Compensation Research Institute;2019. [Google Scholar]
- 41.State of Washington. RCW Title 51: Chapter 51.12. Employments and occupations covered. http://apps.leg.wa.gov/rcw/default.aspx?Cite=51.12. Accessed September 18, 2020.
- 42.Franklin GM, Fulton-Kehoe D. Outcomes research in Washington state workers’ compensation. Am J Ind Med. 1996;29(6):642–648. [DOI] [PubMed] [Google Scholar]
- 43.Franklin GM, Wickizer TM, Fulton-Kehoe D, Turner JA. Policy-relevant research: when does it matter? NeuroRx. 2004;1(3):356–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Washington State Employment Security Department. Occupations Exempted from Unemployment Insurance Coverage. https://esdorchardstorage.blob.core.windows.net/esdwa/Default/ESDWAGOV/employer-Taxes/ESD-exempt-professions-chart.pdf. Accessed October 1, 2020.
- 45.Gross DP, Battie MC. Work-related recovery expectations and the prognosis of chronic low back pain within a workers’ compensation setting. J Occup Environ Med. 2005;47(4):428–433. [DOI] [PubMed] [Google Scholar]
- 46.Oranye NO. Nature of Injury and risk of multiple claims among workers in Manitoba health care. Workplace Health Saf. 2018;66(2):70–83. [DOI] [PubMed] [Google Scholar]
- 47.Washington State Department of Labor and Industries. Medical Examiners’ Handbook. Publication F252–001-0002019. [Google Scholar]
- 48.Washington State Department of Labor and Industries.Permanent Partial Disability. PPD Award Schedules. https://lni.wa.gov/claims/for-workers/claim-benefits/permanent-partial-disability. Accessed May 17, 2020.
- 49.Ingram DD, Franco SJ. 2013 NCHS Urban–Rural Classification Scheme for Counties Vital Health Statistics. Vol 2 Washington, DC: National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 50.Sears JM, Rundell SD. Development and testing of compatible diagnosis code lists for the Functional Comorbidity Index: International Classification of Diseases, Ninth Revision, Clinical Modification and International Classification of Diseases, 10th Revision, Clinical Modification. Med Care. Online first: September 29, 2020; doi: 10.1097/MLR.0000000000001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.State of Washington. Washington Administrative Code 296–17-901. Risk classification hazard group table. Effective June 30, 2017. https://apps.leg.wa.gov/wac/default.aspx?cite=296-17-901. Accessed June 18, 2020.
- 52.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 53.National Institute for Occupational Safety and Health. Morbidity and disability among workers 18 years and older in the Healthcare and Social Assistance sector, 1997–2007. DHHS (NIOSH) Publication No. 2012–161. 2012; http://www.cdc.gov/niosh/docs/2012-161/pdfs/2012-161.pdf. Accessed April 30, 2017.
- 54.Schramm J Older Workers and Part-Time Employment. Fact Sheet 640, February 2018. 2018; https://www.aarp.org/ppi/info-2018/older-workers-and-part-time-employment.html. Accessed July 30, 2020.
- 55.Berecki-Gisolf J, Clay FJ, Collie A, McClure RJ. Predictors of sustained return to work after work-related injury or disease: insights from workers’ compensation claims records. J Occup Rehabil. 2012;22(3):283–291. [DOI] [PubMed] [Google Scholar]
- 56.Dasinger LK, Krause N, Deegan LJ, Brand RJ, Rudolph L. Duration of work disability after low back injury: a comparison of administrative and self-reported outcomes. Am J Ind Med. 1999;35(6):619–631. [DOI] [PubMed] [Google Scholar]
- 57.Reville RT, Bhattacharya J, Sager Weinstein LR. New methods and data sources for measuring economic consequences of workplace injuries. Am J Ind Med. 2001;40(4):452–463. [DOI] [PubMed] [Google Scholar]
- 58.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health. 2002;92(9):1421–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fan ZJ, Bonauto DK, Foley MP, Silverstein BA. Underreporting of work-related injury or illness to workers’ compensation: individual and industry factors. J Occup Environ Med. 2006;48(9):914–922. [DOI] [PubMed] [Google Scholar]
- 60.Sears JM, Bowman SM, Blanar L, Hogg-Johnson S. Industrial injury hospitalizations billed to payers other than workers’ compensation: characteristics and trends by state. Health Serv Res. 2017;52(2):763–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wasiak R, Pransky GS, Webster BS. Methodological challenges in studying recurrence of low back pain. J Occup Rehabil. 2003;13(1):21–31. [DOI] [PubMed] [Google Scholar]
- 62.Gouskova E Why self-employment rates are higher among people with work limitations. J. Disabil. Policy Stud. 2020;31(1):15–25. [Google Scholar]


