Abstract
Hospital admissions in the US fell dramatically with the onset of the coronavirus disease 2019 (COVID-19) pandemic. However, little is known about differences in admissions patterns among patient groups or the extent of the rebound. In this study of approximately one million medical admissions from a large, nationally representative hospitalist group, we found that declines in non-COVID-19 admissions from February to April 2020 were generally similar across patient demographic subgroups and exceeded 20 percent for all primary admission diagnoses. By late June/early July 2020, overall non-COVID-19 admissions had rebounded to 16 percent below prepandemic baseline volume (8 percent including COVID-19 admissions). Non-COVID-19 admissions were substantially lower for patients residing in majority-Hispanic neighborhoods (32 percent below baseline) and remained well below baseline for patients with pneumonia (−44 percent), chronic obstructive pulmonary disease/asthma (−40 percent), sepsis (−25 percent), urinary tract infection (−24 percent), and acute ST-elevation myocardial infarction (−22 percent). Health system leaders and public health authorities should focus on efforts to ensure that patients with acute medical illnesses can obtain hospital care as needed during the pandemic to avoid adverse outcomes.
Hospital admissions fell precipitously with the declaration of the coronavirus disease 2019 (COVID-19) pandemic in the US in March 2020, with several reports of hospitals operating at less than 50 percent capacity.1–3 Volumes fell in part because hospitals purposefully curtailed elective surgery and other noncritical medical services. But hospitals have also reported puzzling declines in admissions for acute medical illness, including stroke and acute myocardial infarction.4–8 In addition to their implications for hospital solvency,9 falling hospitalization rates could portend substantial harm to public health if patients defer care for life-threatening conditions.
Early evidence on how the first wave of the COVID-19 pandemic has affected US hospital admissions has thus far been limited to individual hospital systems,8 Veterans Affairs patients,10 or elderly patients participating in bundled payment programs.11 Much less is known about variations in admissions by age, insurance coverage, and sociodemographic group in this initial period of decline and during the first “rebound” in health care use in June/July 2020.12
Given the widespread uncertainty, public anxiety, and stay-at-home orders and other restrictions imposed during the initial phase of the pandemic in April 2020, we hypothesized that many patients with acute medical illness, whether life threatening or not, did not seek hospital care out of fear of contagion or concerns about access at COVID-19-overrun hospitals.13 We also sought to gain insights on the extent to which patients continued to avoid hospital care as the first phase of the pandemic receded after April, restrictions eased, and businesses opened in many states.
A high percentage of medical admissions to US hospitals are for conditions that are reasonably managed at home in many circumstances.14 It is plausible that many patients, in consultation with their physicians, made informed decisions to defer or avoid hospitalization early during the pandemic. Informed or not, patients’ decisions to return to the hospital in the short and long term may also be influenced by patients’ age, race, ethnicity, insurance status, and income—factors often related to trust in or access to the health care system.15,16
A better understanding of the impact of COVID-19 on medical admissions over time would provide insight to health system leaders and public health authorities about groups of patients at continued risk for undertreatment of acute medical illness. In that context, we used recent data from a large, nationally distributed hospitalist group to examine admission patterns during the first four months of the COVID-19 pandemic in the US.
Study Data And Methods
Setting And Data
Sound Physicians is a national medical group specializing in hospital medicine, critical care, and emergency medicine. It employs or contracts with almost 4,000 physicians across a wide range of hospital settings—most commonly community hospitals with 100–500 beds. At most of the hospitals where it is based, Sound is the exclusive hospital medicine provider and manages the majority of hospital admissions and discharges. Sound serves many hospitals in states hit relatively hard by the first COVID-19 surge, including Washington, Michigan, and Ohio; although it serves no hospitals in New York City, it serves several in the broader metropolitan area. It is also well represented in states with lower initial COVID-19 prevalence but later surges, including Texas, Arizona, and California.
This analysis was based on data from 201 hospitals in 36 states. As detailed in the online appendix,17 we excluded Sound hospital practices not operating continuously from 2019 through 2020, those with critical care but not hospital medicine programs, and one hospital with fewer than fifty admissions in 2020. Our sample size was 1,056,951, including 505,060 admissions in 2020 and 551,891 admissions in 2019.
Data used for this analysis were collated in near–real time and derived from two sources. First, data from hospitals’ administrative systems provide information about patients’ characteristics, including age, dates of admission and discharge, ZIP code of residence, primary payer, and status at discharge. Second, Sound’s electronic medical record and billing platform provides clinical diagnoses (with International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, or ICD-10 codes) supplied by treating physicians and identifies patients with COVID-19 infection. With regard to the latter, physicians are prompted on every patient admission, “Is this patient being treated for COVID-19 infection?” For this analysis we counted all patients with a “yes” response from physicians, regardless of whether test results were positive, negative, or still pending at discharge.
Measures
Our primary outcome measures were non-COVID-19 and total medical admissions by week (Sunday to Saturday). A secondary outcome was in-hospital mortality. We considered all Sound admissions from week 5 in 2020 (February 2–8) through the week 27 of the same year (July 5–11). To adjust for seasonality in the incidence of disease (for example, pneumonia admissions are generally higher in February than in June), we also calculated overall and disease-specific admissions for weeks 5–27 in 2019 (February 3–9 through July 7–13).
For analyses of patient subgroups and in-hospital mortality rates, we aggregated weeks into “months” (the weekly periods corresponding most closely to each month) to allow for greater statistical power. In summarizing our main results, we focused on three specific periods in our analysis: weeks 5–8 (February) as the baseline period before substantive changes in admissions; weeks 13–16 (April) as the nadir period, when admissions sank to their lowest level; and weeks 23–26 (four weeks in June spilling into July, which we refer to as “June/July”), which correspond to the initial rebound.
Analysis
In our primary analysis we normalized weekly admissions using average weekly admissions for the four weeks in February. To adjust for seasonality in hospital admissions, we use the corresponding week or month in 2019 as our control. For example, suppose there were an average of 100 admissions weekly during the February 2020 baseline, dropping to 70 per week in April. Suppose that in 2019 admissions had fallen from 95 in February to 90 in April. Our statistical comparison is for admissions in April 2020 and April 2019 (or 70/90), but with an adjustment for the larger sample of baseline (February) admissions in 2020 compared with 2019 (95/100). The adjusted ratio is therefore (70/90)*(95/100) = 0.74, or a decline of 26 percent. The appendix contains further discussion of the statistical analysis.17
Subgroup Analysis
We performed subgroup analysis of admissions for several patient characteristics. First, patients whose ZIP codes were available in the billing data (77.4 percent) were matched by ZIP code to census data compiled by CUBIT Inc. We created categorical variables for patients based on their residence in ZIP codes with a majority (50 percent or more) of Black residents, a majority (50 percent or more) of Hispanic residents, or poverty rates in excess of 25 percent. For the in-hospital mortality analysis, we also created a variable measuring whether the patient’s ZIP code was in any of these categories.
Our ZIP code measure captured neighborhood effects, such as a lack of access to health care, which have been shown to exert an independent impact on health.4,18 In addition, we considered subsets of patients with Medicaid coverage, with “self-pay” (uninsured) status, younger than age fifty, and age seventy or older. Finally, we considered changes in admissions by the extent to which hospitals were directly affected by COVID-19 admissions. For this purpose, hospitals were grouped in quintiles on the basis of the proportion of all medical admissions with suspected COVID-19 infection for weeks 13–26.
To assess whether changes in admissions differed by medical condition or diagnosis, we identified the twenty top medical conditions responsible for admissions to hospital medicine practices. These conditions were defined according to the ICD-10 codes recorded in the primary diagnosis field in the physician’s admission billing claim (see the appendix).17 These codes were used rather than diagnosis-related groups to reduce clinical heterogeneity in each group and avoid timing lags associated with the latter, as the final diagnosis-related group is generally determined for billing purposes well after discharge.
In-Hospital Mortality Trends
We examined mortality trends to better understand changes in illness severity. If less seriously ill patients were disproportionately staying away from the hospital during the COVID-19 pandemic, we expected in-hospital mortality rates to rise.We estimated a logistic regression model for non-COVID-19 patients, adjusting for age, primary diagnosis, sex (male, female, or missing), and whether the patient resided in a high-minority or high-poverty ZIP code.We used corresponding 2019 in-hospital mortality rates to adjust for seasonality. The analysis was approved by the Dartmouth College Institutional Review Board; all statistical work was performed with STATA, version 16.1.
Limitations
There were several limitations to this study. First, our data might not reflect the clinical reality at every US hospital. Although Sound has a broad geographic distribution, it is underrepresented in New York City and a small number of quaternary care centers that served as COVID-19 referral centers during the height of the pandemic’s first wave. Second, we measured income and race/ethnicity at the ZIP code level, whereas age and insurance status were measured at the individual level; thus, our estimates capture a combination of neighborhood- and individual-level effects. Third, our data were limited to medical admissions. It is notable that two recent studies suggest similar patterns in outpatient visits and surgical admissions.11,12 Fourth, we measured in-hospital mortality only and therefore were unable to quantify out-of-hospital mortality for patients who were not admitted. Finally, our analysis reflects less than a full year of data and ends in early July 2020. Preliminary unpublished data from Sound Physicians suggest that lagging rates of utilization during the rebound persisted into August 2020.
Study Results
Exhibit 1 shows medical admissions trends in 2019 and 2020 relative to admission levels at baseline in February. In 2020 there was a sharp drop in total medical admissions and non-COVID-19 admissions beginning in March, reaching a nadir in April, with the rebound leveling off in June/July. By late June a secondary resurgence in suspected COVID-19 admissions (the gap between the “total admissions 2020” and “non-COVID-19 admissions 2020” lines) had begun in several states, as non-COVID-19 admissions flattened.
Exhibit 1. Total medical admissions in 2019 and 2020 and non-COVID-19 medical admissions in 2020 in a group of US hospitals, by week.
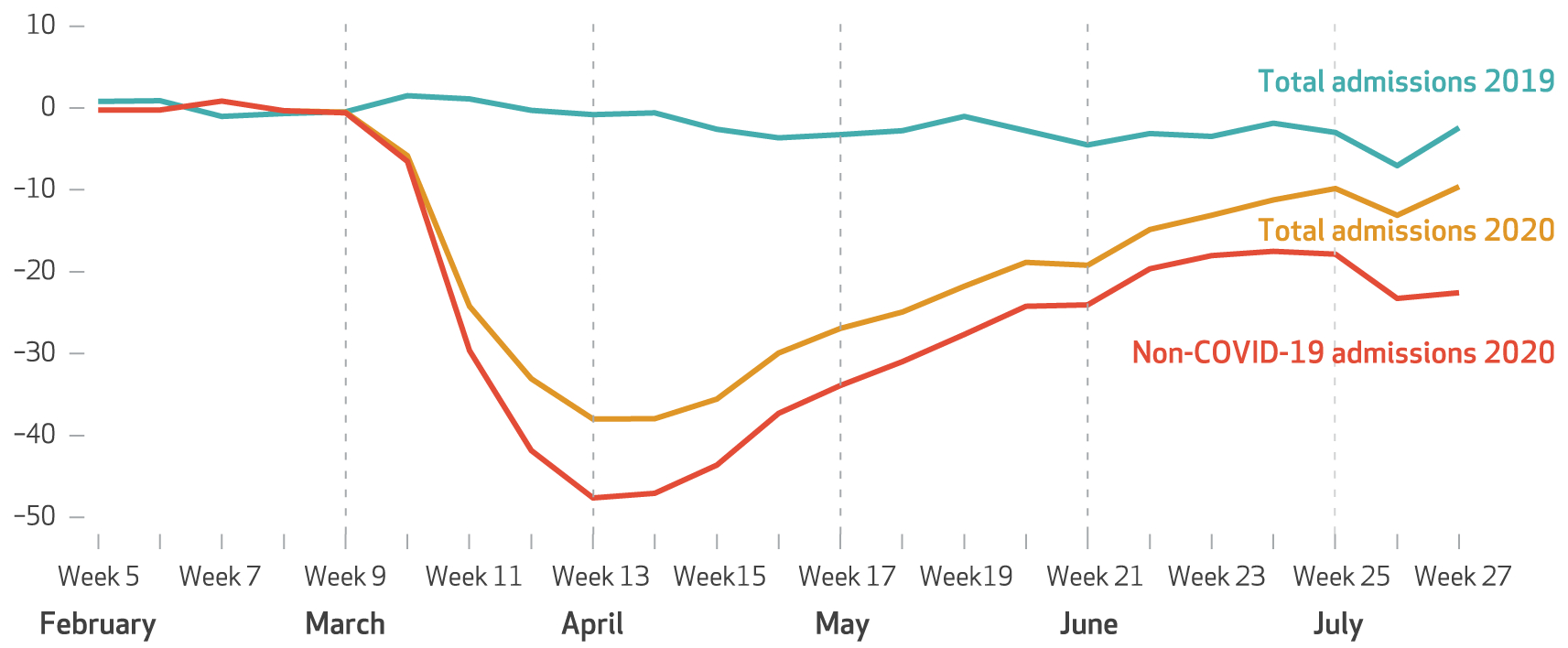
SOURCE Data from Sound Physicians hospital admissions. NOTES Data represent 1,056,951 admissions in 201 hospitals in 36 states. Non-COVID-19 admissions exclude all suspected or confirmed COVID-19 admissions based on physicians’ response to a specific prompt in the electronic medical record at admission starting in week 10, which corresponds to the beginning of the pandemic. The percentage decline is relative to the average weekly admissions during February (weeks 5–8). Week 5 corresponds to February 2–8 and week 27 to July 5–11, 2020.
Exhibit 2 quantifies the decline and rebound after seasonality in admissions is adjusted for. Confidence intervals for this and subsequent exhibits are in the appendix.17 Non-COVID-19 admissions during the nadir fell by 42.8 percent (95% confidence interval: −43.2, −42.4), and all medical admissions in April declined by 34.1 percent (95% CI: −34.6, −33.6). The difference, 8.7 percentage points, represents patients with suspected COVID-19 in the first surge. Medical admissions rebounded steadily after the nadir in April, and by June/July non-COVID-19 admissions were 15.9 percent (95% CI: −16.5, −15.4) lower relative to baseline volume, and all medical admissions were 8.3 percent below baseline (95% CI: −8.9, −7.7).
Exhibit 2.
Changes in non-COVID-19 medical admissions and all medical admissions in a group of US hospitals relative to baseline, total and by subgroup, 2020
| Change in non-COVID-19 admissions (%) | Change in all medical admissions (%) | ||||
|---|---|---|---|---|---|
| Patient subgroups | Sample size at baseline | Nadir (April) | Rebound (June/July) | Nadir (April) | Rebound (June/July) |
| Overall | 105,688 | −42.8 | −15.9 | −34.1 | −8.3 |
| Race, ethnicity, and poverty status of ZIP code | |||||
| >50% Black | 5,140 | −45.2 | −11.9 | −30.1 | −2.3a |
| >50% Hispanic | 9,161 | −44.2 | −31.8 | −34.8 | −14.1 |
| Poverty rate >25% | 6,761 | −44.0 | −16.7 | −31.5 | −2.7 |
| Insurance status | |||||
| Medicaid | 13,009 | −41.4 | −9.7 | −31.2 | −2.5 |
| Self-pay | 2,922 | −37.7 | −20.3 | −27.3 | −3.7 |
| Age | |||||
| Older (age 70+) | 42,384 | −45.4 | −19.1 | −37.5 | −13.2 |
| Younger (age <50) | 23,636 | −39.3 | −13.4 | −30.4 | −3.4 |
| Hospital COVID-19 volume | |||||
| Highest quintile | 21,285 | −50.0 | −23.3 | −31.2 | −9.9 |
| Lowest quintile | 21,231 | −39.5 | −6.8 | −36.5 | −5.5 |
SOURCE Data from Sound Physicians hospital admissions. NOTES Data from 201 hospitals in 36 states. These estimates adjust for seasonality by use of the corresponding weeks for 2019 data. The appendix contains details regarding estimates of confidence intervals (see note 17 in text). The sample size is for the initial (baseline) February 2020 admissions.
All differences in use relative to the seasonally adjusted baseline are significant at the 0.05 level except for this coefficient.
Admissions In Patient Subgroups
During the nadir, the decline in non-COVID-19 admissions in majority-Black neighborhoods was substantial but was only slightly larger in magnitude than the overall decline (−45.2 percent compared with −42.8 percent overall; p < 0:05) (exhibit 2). For non-COVID-19 admissions, neighborhoods with a majority of Hispanic residents also experienced a marginally larger admissions decline in April relative to baseline (−44.2 percent), as did neighborhoods with a high rate of poverty (−44.0 percent). Compared with the overall decline in non-COVID-19 admissions during the nadir, the reduction was slightly less for Medicaid patients (−41.4 percent) and self-pay patients (−37.7 percent). Non-COVID-19 admissions fell to a greater degree in patients older than age seventy than among patients younger than age fifty (−45.4 percent versus −39.3 percent; p < 0:05). Finally, non-COVID-19 admissions declined by more in hospitals in the highest quintile of COVID-19 exposure than in hospitals in the lowest quintile (−50.0 percent versus −39.5 percent; p < 0:05).
During the rebound period in June/July, non-COVID-19 admissions remained especially depressed for patients from majority-Hispanic neighborhoods (−31.8 percent; p < 0:05) and in hospitals in the highest quintile of COVID-19 exposure (−23.3 percent; p < 0:05), whereas admissions had rebounded nearly completely for hospitals in the lowest quintile (−6.8 percent; p < 0:05). Non-COVID-19 patients who were age seventy or older experienced a larger decline, relative to baseline (−19.1 percent; p < 0:05), than younger patients, and the admissions decline was greater among self-pay patients (−20.3 percent; p < 0:05) than among those with Medicaid (−9.7 percent; p < 0:05).
Admissions By Diagnosis
Non-COVID-19 admission volumes declined substantially for all twenty primary medical conditions or diagnoses in April 2020 (exhibit 3). Conditions that declined least included pancreatitis (−23.7 percent; p < 0:05), stroke (−24.7 percent; p < 0:05), and altered mental status (−27.1 percent; p < 0:05). Several conditions associated with much larger admission declines included chronic obstructive pulmonary disease (COPD)/asthma (−68.6 percent; p < 0:05), non-COVID-19 pneumonia (−53.6 percent, p < 0:05), and transient ischemic attack (−50.9 percent, p < 0:05). Although not highlighted in the exhibits, patients with COVID-19 accounted for a large proportion of admissions with respiratory failure (73.7 percent), pneumonia (70.1 percent), and sepsis (38.2 percent); total admissions fell less for these three conditions than they did for most other medical illnesses (data not shown).
Exhibit 3.
Changes in non-COVID-19 medical admissions and all medical admissions in US hospitals, by diagnosis, 2020 relative to equivalent periods in 2019
| Change in non-COVID-19 admissions (%) | Change in all medical admissions (%) | ||||
|---|---|---|---|---|---|
| Diagnoses | Sample size at baseline | Nadir (April) | Rebound (June/July) | Nadir (April) | Rebound (June/July) |
| Pancreatitis | 1,151 | −23.7 | −4.5a | −22.4 | −2.9a |
| Stroke | 2,350 | −24.7 | −16.9 | −23.1 | −15.8 |
| Altered mental status | 2,251 | −27.1 | −15.5 | −18.9 | −11.2 |
| Alcohol-related | 1,042 | −32.6 | 4.3a | −30.5 | 5.8a |
| Dehydration | 4,446 | −33.7 | −12.5 | −29.4 | −9.7 |
| Acute ST-elevation myocardial infarction | 416 | −34.9 | −22.2 | −33.1 | −21.1 |
| Diabetes | 2,283 | −38.5 | 0.8a | −35.8 | 3.5a |
| Gastrointestinal bleeding | 4,042 | −38.8 | −11.9 | −36.9 | −9.7 |
| Sepsis and sepsis shock | 6,712 | −40.1 | −25.1 | −24.8 | −14.4 |
| Acute myocardial infarction (non-ST-elevation) | 1,568 | −42.2 | −16.1 | −39.4 | −14.4 |
| Skin and soft tissue infection | 2,806 | −44.0 | −19.0 | −42.5 | −18.1 |
| Respiratory failure | 5,986 | −44.8 | −21.0 | −11.8 | 11.1 |
| Chest pain (excluding acute myocardial infarction) | 7,383 | −46.0 | −14.6 | −44.0 | −13.0 |
| Arrhythmia | 3,626 | −47.2 | −14.7 | −44.2 | −12.3 |
| Congestive heart failure | 3,878 | −47.5 | −20.1 | −43.8 | −17.8 |
| Abdominal pain | 4,893 | −48.5 | −14.4 | −46.1 | −11.9 |
| Urinary tract infection | 2,296 | −48.5 | −24.3 | −46.2 | −22.0 |
| Transient ischemic attack | 1,082 | −50.9 | −11.4 | −50.0 | −10.8 |
| Pneumonia | 3,953 | −53.6 | −44.1 | −16.0 | −19.6 |
| Chronic obstructive pulmonary disease/asthma | 3,192 | −68.6 | −40.1 | −61.6 | −35.5 |
SOURCE Data from Sound Physicians hospital admissions. NOTES Data from 201 hospitals in 36 states. Diagnostic category based on initial diagnosis code at admission.
The appendix contains all confidence intervals (see note 17 in text).
All results except these are statistically significant (p < 0:05).
By June/July, admissions for pancreatitis, alcohol-related conditions, and diabetes had returned to baseline levels. At the other end of the range, non-COVID-19 admissions for urinary tract infection (−24.3 percent; p < 0:05), sepsis (−25.1 percent; p < 0:05), COPD/asthma (−40.1 percent; p < 0:05), and pneumonia (−44.1 percent; p < 0:05) remained substantially depressed. Surprisingly, there were clinically meaningful declines in non-COVID admissions for patients with acute ST-elevation myocardial infarction (−22.2 percent; p < 0:05) and stroke (−16.9 percent; p < 0:05), two acute conditions generally requiring immediate hospitalization to avoid adverse outcomes.
In-Hospital Mortality
Relative to the 2.1 percent in-hospital mortality rate for non-COVID-19 admissions during February 2020, in-hospital mortality rose by 0.3 percent (p < 0:05) in April before returning to baseline in May and June. Because admission volumes fell to a larger degree than in-hospital mortality increased, the total number of non-COVID-19 patients who died in the hospital was lower in April (n = 691) than it was in February (n = 1,100) (data not shown). Stratified analysis of in-hospital mortality, shown in exhibit 4 (with coefficients reported in the appendix and adjusting for age, sex, and diagnosis),17 suggested that much of the increase in in-hospital mortality for non-COVID admissions during April occurred for patients living in majority-Black, majority-Hispanic, or high-poverty ZIP codes. In April, mortality in this subgroup was 0.5 percent higher than for those not in the subgroup (p = 0:03). By the end of May, that disparity in mortality had disappeared.
Exhibit 4. Adjusted in-hospital mortality rates for non-COVID-19 medical admissions in a group of US hospitals, by minority or poverty status in the patient’s ZIP code, February–June 2020.
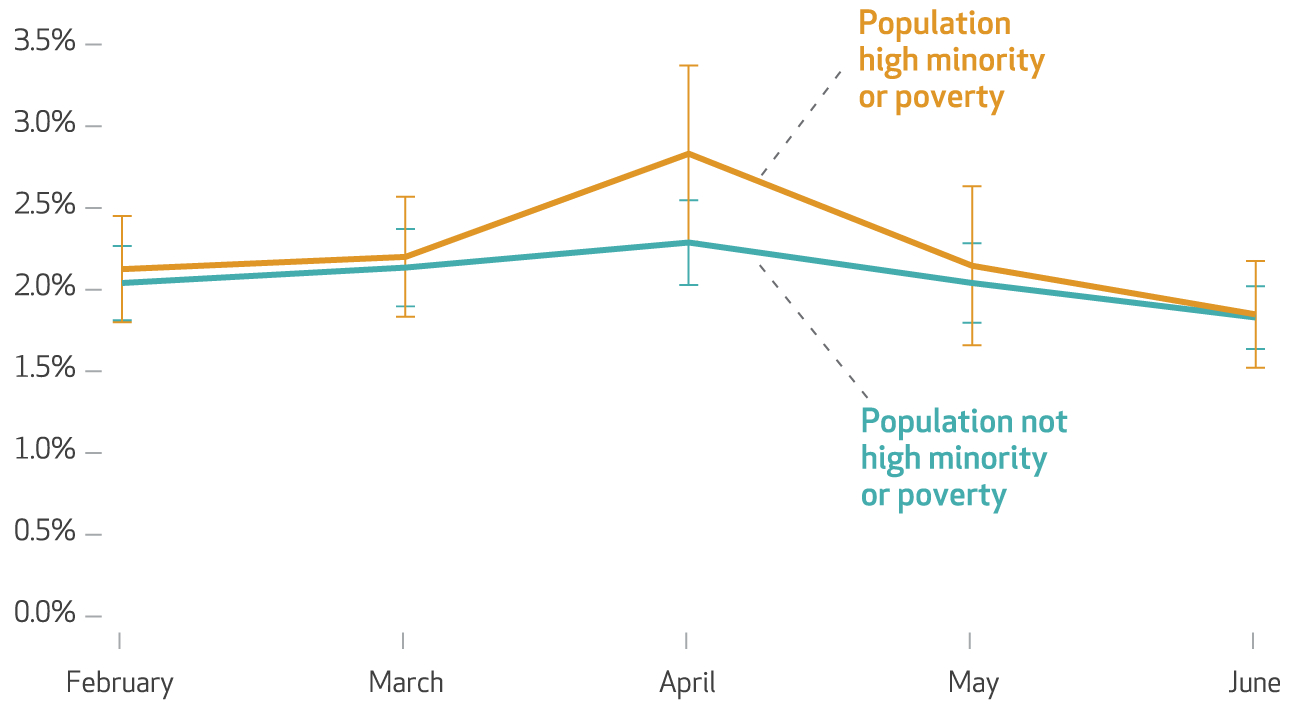
SOURCE Data from Sound Physicians hospital admissions. NOTES Data from 201 hospitals in 36 states. The orange (upper) line corresponds to estimates for patients living in ZIP codes with either majority-Black or majority-Hispanic populations or those with poverty rates higher than 25 percent; the teal (lower) line denotes all other patients. Estimates are from a logistic regression that adjusted for diagnosis, age, sex, and month by year by high-minority/poverty ZIP code categorical variables. The weeks correspond to months as follows: February (weeks 5–8), March (weeks 9–12), April (weeks 13–17), May (weeks 18–21), and June/July (weeks 22–26). Error bars represent 95% confidence intervals. The full regression analysis is in the appendix (see note 17 in text).
Discussion
Medical admissions fell dramatically with the spread of COVID-19 in March and April 2020. Sound Physicians admissions represent approximately 6 percent of acute medical admissions nationwide; simply extrapolating the observed reduction in admissions from our sample to all admissions nationwide suggests a decline of 0.7 million non-COVID-19 medical admissions in April 2020 relative to April 2019. Admissions declined in all patient groups defined by age, race and ethnicity, Medicaid and self-pay status, and income.
The most plausible explanation for the broad-based declines in medical admissions is that patients avoided seeking hospital care, perhaps in response to fear of contagion arising from media reports or as a result of state stay-at-home orders. Conversely, our results do not suggest access challenges at hospitals overrun with patients with COVID-19 as a major reason for admission declines. Even among hospitals experiencing a minimal impact from COVID-19 admissions, non-COVID-19 medical admissions fell by 39.5 percent; for hospitals with the greatest COVID-19 impact, non-COVID-19 admissions fell by 50.0 percent (exhibit 2).
A second, more surprising finding of this analysis is that during the nadir period, admissions declines varied only modestly by patient demographic factors, including insurance status and minority and income characteristics of the areas in which patients lived. The relatively uniform April 2020 declines in admissions across patient demographic groups may reflect offsetting factors. For example, relatively advantaged populations may have greater access to ambulatory care resources for safely deferring hospital-based care, including telemedicine services, which increased dramatically during the pandemic.19,20 Alternatively, our largely null findings in this regard may simply reflect that the pandemic affected patients’ decision making in a powerful, universal way that trumped the usual determinants of health care use.21
During the April nadir, non-COVID-19 admissions declined less for patients with some acute medical conditions than others. In our analysis the three medical conditions for which nonCOVID-19 admissions declined the least were stroke, altered mental status, and pancreatitis—conditions generally associated with new or severe symptoms not easily ignored or effectively managed at home. These findings are consistent with those of a study performed during the severe acute respiratory syndrome (SARS) epidemic, which reported that admission rates in Canadian hospitals fell less for acute, life-threatening illnesses than for less-urgent conditions.22
By the time of the rebound, non-COVID-19 medical admission volumes had returned to within 16 percent of baseline overall, although admissions for non-COVID-19 pneumonia, COPD/asthma, and sepsis remained well below prepandemic baselines. These findings are consistent with those of broader studies that suggest the discretionary nature and elasticity of admission decisions in patients with certain medical conditions.23 Less consistent with the elasticity view are the continued lower admissions for acute ST-elevation myocardial infarction and stroke, generally considered to be acute nondiscretionary admissions.
Although admissions declined consistently across patient demographic subgroups during the nadir, they recovered to a smaller degree for some groups than others. For example, non-COVID-19 admissions during late June and early July were 31.8 percent below baseline for patients residing in majority-Hispanic ZIP codes. This pattern may reflect the large Hispanic populations in the South and Southwest,24 where COVID-19 infection rates resurged in late June,25 but a larger concern is that it may reflect access challenges for Hispanic populations nationwide. Non-COVID-19 admissions also dropped by 20.3 percent for self-pay patients during the rebound. This finding could reflect changes in health care decisions or access among people who became uninsured as a result of job loss during the pandemic.26
It is too early to determine the extent to which hospitalizations will return to baseline levels. A new, lower norm is conceivable if clinicians become more comfortable with alternatives to inpatient admission, including home-based care with remote monitoring.14
Although we expected illness severity in non-COVID-19 medical admissions to increase as less-sick patients avoided the hospital, in-hospital mortality in patients without COVID-19 increased only modestly during the nadir of medical admissions in April before returning to pre-COVID-19 levels in June. Largely flat mortality rates imply that the total number of in-hospital deaths for non-COVID-19 medical conditions declined by nearly the same degree as admissions.
This pattern (as well as declines in non-COVID-19 acute ST-elevation myocardial infarction and stroke admissions) could be explained by lower incidence of disease. Several studies have noted that a sharp decline in pollution during the pandemic would be expected to reduce mortality.27–29 Similarly, there may have been fewer non-COVID-19-related respiratory disease admissions because of social distancing and the use of masks or face coverings. A reduction in disease incidence would also be consistent with previous studies finding temporarily lower mortality rates during recessions.30,31 Alternatively, the “missing” non-COVID-19 medical admissions could have resulted in elevated out-of-hospital deaths. One study of five states affected by the initial COVID-19 surge found higher mortality for heart disease, Alzheimer disease, and diabetes among patients not diagnosed with COVID-19.32
Notably, the increased in-hospital mortality rate during the nadir in April for non-COVID-19 medical admissions was more pronounced for patients residing in minority or poor neighborhoods. There is evidence that Black patients diagnosed with COVID-19 were more likely to be admitted to the hospital33 and to experience higher in-hospital mortality.34 Our results suggest an additional concern: that non-COVID-19 patients from minority or low-income neighborhoods may have experienced barriers in access during the nadir in April, potentially leading to higher mortality rates.
Conclusion
Our results provide empirical support for concerns about the broad public health impact of the pandemic on non-COVID-19 populations. Some medical conditions (for example, stroke, acute ST-elevation myocardial infarction) require effective hospital treatment to avoid adverse outcomes; therefore, fewer hospitalizations for such medical conditions are almost certainly associated with patient harm. Health system leaders and public health authorities should be focusing on how best to ensure that patients with conditions that require hospital care obtain it during the pandemic. Where the impact of hospital-based care is less clear, however, longer-term studies will be needed to determine the extent to which avoiding hospitalization during the pandemic may affect patients’ mortality, morbidity, and quality of life. ■
Supplementary Material
Acknowledgments
This study was supported by a grant from the National Institute on Aging (P01AG019783). John D. Birkmeyer and Robert M. Bessler have equity interests as officers for Sound Physicians. Nancy Birkmeyer is married to John Birkmeyer. An unedited version of this article was published online September 24, 2020, as a Fast Track Ahead Of Print article. That version is available in the online appendix.
Contributor Information
John D. Birkmeyer, chief clinical officer of Sound Physicians, in Tacoma, Washington, and an adjunct professor for health policy and clinical practice, Geisel School of Medicine at Dartmouth, in Lebanon, New Hampshire.
Amber Barnato, Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth..
Nancy Birkmeyer, principal research scientist at the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth..
Robert Bessler, Sound Physicians..
Jonathan Skinner, Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth..
NOTES
- 1.Cigna. Cigna study finds reduced rates of acute non-elective hospitalizations during the COVID-19 pandemic [Internet]. Bloomfield (CT): Cigna; 2020. April [cited 2020 Sep 25]. Available from: https://www.cigna.com/about-us/newsroom/studies-and-reports/deferring-care-during-covid-19 [Google Scholar]
- 2.Cox C, Kamal R, McDermott D. How have healthcare utilization and spending changed so far during the coronavirus pandemic? [Internet]. San Francisco (CA): Peterson-KFF Health System Tracker; 2020. August 6 [cited 2020 Sep 25]. Available from: https://www.healthsystemtracker.org/chart-collection/how-have-healthcare-utilization-and-spending-changed-so-far-during-the-coronavirus-pandemic/ [Google Scholar]
- 3.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23): 699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahmud N, Hubbard RA, Kaplan DE, Serper M. Declining cirrhosis hospitalizations in the wake of the COVID-19 pandemic: a national cohort study. Gastroenterology. 2020;159(3):1134–1136.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2020;29(8): 104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung S-H, et al. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–3. [DOI] [PubMed] [Google Scholar]
- 9.Khullar D, Bond AM, Schpero WL. COVID-19 and the financial health of US hospitals. JAMA. 2020;323(21): 2127–8. [DOI] [PubMed] [Google Scholar]
- 10.Baum A, Schwartz MD. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020; 324(1):96–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chernew ME, Fendrick AM, Armbrester K, de Brantes F. COVID-19 effects on care volumes: what they might mean and how we might respond. Health Affairs Blog [blog on the Internet] 2020. July 6 [cited 2020 Sep 25]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20200702.788062/full/ [Google Scholar]
- 12.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D, Schneider E (Harvard University; Cambridge, MA). The impact of the COVID-19 pandemic on outpatient visits: changing patterns of care in the newest COVID-19 hot spots [Internet]. New York (NY): Common-wealth Fund; 2020. August 13 [cited 2020 Sep 25]. Available from: https://www.commonwealthfund.org/publications/2020/aug/impact-covid-19-pandemic-outpatient-visits-changing-patterns-care-newest [Google Scholar]
- 13.Hafner K. Fear of Covid-19 leads other patients to decline critical treatment. New York Times [serial on the Internet]. 2020. May 25 [cited 2020 Oct 7]. Available from: https://www.nytimes.com/2020/05/25/health/coronavirus-cancer-heart-treatment.html [Google Scholar]
- 14.Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for medicare. Health Aff (Millwood). 2014;33(2): 244–50. [DOI] [PubMed] [Google Scholar]
- 15.Alsan M, Garrick O, Graziani G. Does diversity matter for health? Experimental evidence from Oakland. Am Econ Rev. 2019; 109(12):4071–111. [Google Scholar]
- 16.Dubay LC, Lebrun LA. Health, behavior, and health care disparities: disentangling the effects of income and race in the United States. Int J Health Serv. 2012;42(4):607–25. [DOI] [PubMed] [Google Scholar]
- 17. To access the appendix, click on the Details tab of the article online.
- 18.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11): 1783–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anthony Bokolo Jnr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020;44(7): 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med. 2020;382(18): 1679–81. [DOI] [PubMed] [Google Scholar]
- 21.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19): 1891–2. [DOI] [PubMed] [Google Scholar]
- 22.Schull MJ, Stukel TA, Vermeulen MJ, Zwarenstein M, Alter DA, Manuel DG, et al. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. 2007;176(13):1827–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health Aff (Millwood). 2002;(Suppl Web Exclusives):W96–114. DOI: 10.1377/hlthaff.w2.96 [DOI] [PubMed] [Google Scholar]
- 24.Stepler R, Lopez MH. 4. Ranking the Latino population in the states [Internet]. Washington (DC): Pew Research Center; 2016. September 8 [cited 2020 Sep 25]. Available from: https://www.pewresearch.org/hispanic/2016/09/08/4-ranking-the-latino-population-in-the-states/ [Google Scholar]
- 25.Frey WH. A roaring Sun Belt surge has inverted the demographics and politics of COVID-19. The Avenue [blog on the Internet]. 2020. July 2 [cited 2020 Sep 25]. Available from: https://www.brookings.edu/blog/the-avenue/2020/06/19/covid-19s-sun-belt-surge-has-recast-the-pandemics-impact/ [Google Scholar]
- 26.Stephenson J. More US adults report insurance coverage loss associated with COVID-19 recession. JAMA Health Forum [serial on the Internet]. 2020. July 7 [cited 2020 Sep 25]. Available from: https://jamanetwork.com/channels/health-forum/fullarticle/2768169 [DOI] [PubMed] [Google Scholar]
- 27.Berman JD, Ebisu K. Changes in U.S. air pollution during the COVID-19 pandemic. Sci Total Environ. 2020; 739:139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen K, Wang M, Huang C, Kinney PL, Anastas PT. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health. 2020;4(6): e210–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dutheil F, Baker JS, Navel V. COVID-19 as a factor influencing air pollution? Environ Pollut. 2020; 263(Pt A):114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bender K, Economou A, Theodossiou I. The temporary and permanent effects of unemployment on mortality in Europe. Int Labour Rev. 2013;152(2):275–86. [Google Scholar]
- 31.Ruhm C. Are recessions good for your health? Q J Econ. 2000; 115(2):617–50. [Google Scholar]
- 32.Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess deaths from COVID-19 and other causes, March–April 2020. JAMA. 2020;324(5):510–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Azar KMJ, Shen Z, Romanelli RJ, Lockhart SH, Smits K, Robinson S, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood). 2020;39(7):1253–62. [DOI] [PubMed] [Google Scholar]
- 34.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


