Abstract
Objective:
To investigate the association of psychological resources with the prevalence of chronic conditions up to 10 years later, and the mediating roles of health behaviors and allostatic load.
Design:
Participants from the Midlife in the United States study (N=850) completed surveys and biomarker assessments over the course of 10 years.
Main Outcome Measures:
Primary outcome was the prevalence of chronic conditions later in life, controlling for baseline chronic conditions. Secondary outcomes were health behaviors and allostatic load. Direct and indirect associations between psychological resources and chronic conditions were examined.
Results:
Psychological resources were negatively associated with chronic conditions directly (ƅ = −.177, p <.05) and indirectly through health behaviors (ƅ = −.026, p <.05), but not through allostatic load (ƅ = −.000, p >.05). Psychological resources were positively associated with health behaviors (ƅ = .130, p <.01), but no association was found between psychological resources and allostatic load (ƅ = −.002, p >.05). Health behaviors were negatively associated with chronic conditions (ƅ = −.201, p <.01), and allostatic load was positively associated with chronic conditions (ƅ = .197, p <.05).
Conclusion:
Findings highlight the beneficial influence of psychological resources on chronic conditions, and the mediating role of health behaviors.
Keywords: Psychological resources, chronic conditions, health behaviors, allostatic load, longitudinal
Introduction
The prevalence of chronic health conditions among adults in the U.S. is increasing, and is compounded by the rising prevalence of multiple chronic conditions (Ward & Schiller, 2013). As of 2012, 50 percent of adults had at least one chronic condition, 25 percent had two or more, and of those aged 65 and older, 23 percent had more than three (Chevarley, 2015; Ward, Schiller, & Goodman, 2014). The high prevalence of chronic conditions is a serious problem, given its negative impact on public health and the economy. Chronic conditions represent seven of the top 10 causes of death in the U.S., and multiple chronic conditions account for 71 percent of the nation’s total health care expenditures (Gerteis et al., 2014; National Center for Health Statistics, 2017). Chronic conditions are also associated with a lower quality of life, higher risk of physical disabilities, and premature death (Bauer, Briss, Goodman & Bowman, 2014). Given the significant physical, psychological, and economic consequences associated with chronic conditions, it is crucial to examine modifiable factors that positively influence these health conditions.
Chronic conditions and psychological resources
Psychological resources have demonstrated beneficial associations with chronic conditions, but have not received as much attention from researchers as lifestyle-related factors (e.g., exercise and diet). Psychological resources are defined as individual differences in positive psychological functioning that influence mental and physical health outcomes (Taylor & Broffman, 2011), and include inner abilities, strengths, skills, and beliefs that influence how individuals manage challenging life events (Taylor & Stanton, 2007). Evidence supports protective associations between psychological resources and health outcomes: Greater psychological resources are associated with lower risk of morbidity (Pressman & Cohen, 2005) and mortality (Chida & Steptoe, 2008), and have a positive impact on chronic conditions including cardiovascular diseases (Cohen, Bavishi, & Rozanski, 2016), depression (Scheier, Carver, & Bridges, 1994), and type 2 diabetes (Tsenkova, Love, Singer, & Ryff, 2007).
The theoretical model of psychological well-being suggests that certain psychological resources promote healthy living and thriving (Ryff, 1995). These resources include positive affect, life satisfaction, purpose in life, self-acceptance, positive relations with others, and environmental mastery. In addition to those six constructs, a review of psychosocial resources in the context of chronic disease highlights optimism and self-esteem as the two leading personality and self/ego-related resources with a large amount of evidence supporting their association with physical and mental health outcomes (Schetter & Dolbier, 2011). These psychological resources are multidimensional and encompass the extent to which individuals maintain positive outcome expectancies (Masten, Cutuli, Herbers, & Reed, 2009); have a positive sense of self (Taylor & Broffman, 2011); experience positive emotions (Folkman & Moskowitz, 2000); favorably evaluate their overall quality of life; have purpose and direction in life; accept personal strengths and weaknesses; have satisfying and trusting relationships with others; and have a sense of control over their environments (Ryff, 2014). The beneficial association between these individual psychological resources and health outcomes is well-documented. However, few studies have examined the combined influences of these psychological resources on health outcomes. Integrated resource theories view psychological resources broadly, and rather than focus on a single psychological resource, suggest that psychological resources tend to correlate with one another and cluster together synergistically (Hobfoll, 2002). Possessing a strong reservoir of psychological resources can therefore benefit physical and mental health.
The above psychological resources have shown particularly beneficial influences on chronic conditions. According to a meta-analysis, greater optimism is consistently associated with lower prevalence of numerous physical health outcomes including cardiovascular disease, cancer, diabetes, hypertension, and HIV/AIDS (Rasmussin, Scheier, & Greenhouse, 2009), and has also been associated with lower incidence of depressive symptoms (Giltay, Zitman, & Kromhout, 2006). Self-esteem has been found to protect against coronary heart disease (Lundgren, Garvin, Jonasson, Andersson, & Kristenson, 2015), and is associated with improved symptom severity among individuals with rheumatoid arthritis and asthma (Juth, Smyth, & Santuzzi, 2008). Positive affect has been negatively associated with both adverse physical symptoms and morbidity (Pressman & Cohen, 2005), and life satisfaction has been linked with lowered risk of cancer, stroke, and type 2 diabetes (Feller, Teucher, Kaaks, Boeing, & Vigl, 2013). Purpose in life has been inversely associated with cardiovascular disease (Cohen et al., 2016), and low self-acceptance has been related to higher depression and anxiety (MacInnes, 2006). Positive relations with others and environmental mastery have been associated with fewer chronic conditions and adverse health symptoms (Ryff, Radler, & Friedman, 2015). Individuals possessing larger quantities of these specific psychological resources may thus be protected against the development of chronic diseases.
Mediators linking psychological resources to chronic conditions
Emerging research suggests two potential mechanisms through which psychological resources may exert beneficial influences on chronic conditions: (1) health behaviors and (2) physiological stress regulatory systems (i.e., allostatic load). Engagement in unhealthy behaviors and greater activation of stress regulatory systems predispose individuals to chronic conditions (Christensen & Antoni, 2002; Salleh, 2008), but psychological resources positively influence health behaviors (Boehm et al., 2018; Taylor & Broffman, 2011) and help reduce the activation of stress regulatory systems (Jamieson, Mendes, & Nock, 2013; Wiley, Bei, Bower, & Stanton, 2017). Prior empirical and conceptual research supports the mediational role of health behaviors (Steptoe, Wright, Kunz‐Ebrecht, & Iliffe, 2006) and allostatic load (Wiley et al., 2017) in the association between various psychological resources and health outcomes. Additionally, various health behaviors including smoking, physical activity, and alcohol intake have been associated with allostatic load (Forrester, Leoutsakos, Gallo, Thorpe, & Seeman, 2019; Hampson, Goldberg, Vogt, Hillier, & Dubanoski, 2009), suggesting a potential bidirectional relationship between health behaviors and allostatic load.
Health behaviors
Health-related behaviors are a major determinant of chronic conditions (Fine, Philogene, Gramling, Coups, & Sinha, 2004). Unhealthy behaviors increase the risk of developing a wide range of health conditions including type 2 diabetes and hypertension, while health-promoting behaviors such as regular exercise are consistently associated with a lower prevalence of chronic conditions (Agborsangaya et al., 2013; Stenholm et al., 2016; Livingstone & McNaughton, 2017). Psychological resources can directly increase engagement in healthy behaviors, i.e., individuals possessing greater levels of psychological resources are more likely to perform health-promoting behaviors (Diener & Chan, 2011; Taylor et al., 2000). Grant et al. (2009) found that a high level of life satisfaction was related to not smoking, exercise, and consumption of a healthier diet. Another study found that optimism was a strong predictor of sleep quality (Lau, Hui, Lam, & Cheung, 2017). Psychological resources can also prevent maladaptive coping behaviors such as smoking and overeating by helping individuals adopt adaptive coping strategies when facing adversity (Conversano et al., 2010; Krasikova, Lester, & Harms, 2015). Given that health behaviors are a major predictor of chronic conditions and positively influenced by psychological resources, health behaviors may mediate the association between psychological resources and chronic conditions.
Allostatic load
Allostatic load is the wear and tear on the body representing cumulative dysregulation in multiple physiological systems (Beckie, 2012). It is driven by prolonged activation of stress regulatory systems, resulting from chronic exposure to stress and adversity over the life span (McEwen, 1998). Long-term activation of these systems can lead to physical and mental health issues such as cardiovascular diseases and depressive symptoms (McEwen, 2004; McEwen & Wingfield, 2003). Psychological resources can help individuals perceive less stress by promoting positive relations with others (Segrin & Rynes, 2009), positive reappraisal, and a problem-solving approach toward stressful situations, thereby reducing activation of stress regulatory systems and in turn allostatic load (Fogelman & Canli, 2015; Taylor & Broffman, 2011; Wiley et al., 2017). When faced with adversity, individuals with more psychological resources show reduced physiological responses, including lower heart rate, blood pressure, and cortisol (Creswell et al., 2005), which contribute to lower allostatic load over time. In one study, psychological resources such as self-acceptance and purpose in life were associated with lower allostatic load (Johansson, Huang, & Lindfors, 2007). Given that allostatic load is a significant determinant of chronic conditions, and that psychological resources can lower stress-related allostatic load biomarkers, allostatic load may mediate the association between psychological resources and chronic conditions.
Current study
The purpose of this study is to investigate the association of psychological resources with the prevalence of chronic conditions 7–10 years later, and the mediating roles of health behaviors and allostatic load. We hypothesize that psychological resources are negatively associated with the prevalence of chronic conditions later in life. Further, we expect that health behaviors and allostatic load will both partially mediate the negative association between psychological resources and the prevalence of chronic conditions.
Method
Sample
The present study is a secondary analysis of data from Midlife in the United States (MIDUS), a national longitudinal study of the role of behavioral and psychosocial factors in health and well-being. Participants were recruited using random digit dialing and were English-speaking, non-institutionalized adults aged 25 to 74 living in the U.S. MIDUS surveys consisted of a phone interview and self-administered questionnaires about psychosocial, physical, and mental health. The original MIDUS cohort (1995–1996; N = 7,108) was followed longitudinally, with a second wave of data (MIDUS 2; N = 4,963) collected in 2004–2006. Participants who completed MIDUS 2 were eligible to participate in a Biomarker Project during 2004–2009 (N = 1,255). The third wave of data (MIDUS 3; N = 3,294) was collected in 2013–2014 using the same survey procedures as those for MIDUS 2. Detailed information about sampling procedures and retention rates of the MIDUS cohort are available elsewhere (Radler & Ryff, 2010).
This study’s analysis is based on a subsample of individuals aged 34 to 83 (N = 850) who participated in the MIDUS 2 survey (Wave 2), the Biomarker Project (Wave 2–1), and the MIDUS 3 survey (Wave 3). The subsample was not significantly different from the larger MIDUS cohort on most study variables, including sociodemographic characteristics (age, sex, race, education), psychological resources, and health characteristics (chronic conditions, exercise), although they were significantly more likely to have a college degree and less likely to smoke (Love et al., 2010).
Measures
Demographics
Demographic variables—age, sex, marital status, race, and education—from Wave 2 were examined as control variables. Additionally, chronic conditions assessed at Wave 2 were included in the analysis as a control variable (Table 1).
Table 1.
Descriptive Statistics of Demographics, Health Behaviors and Chronic Conditions Measures
| Type | Variable Description | N/Range | Mean (SD) or % |
|---|---|---|---|
| Demographics | Age | 34–83 | 54.73 (11.02) |
| Sex (% female) | 474 | 55.8% | |
| Marital Status (% currently married) | 849 | 72.6% | |
| Race | |||
| White | 791 | 93.1% | |
| Non-White | 59 | 6.9% | |
| Education | |||
| Less than high school | 25 | 2.9% | |
| High school diploma | 175 | 20.6% | |
| Some college | 179 | 21.1% | |
| College degree | 266 | 31.2% | |
| Graduate school and above | 205 | 24.1% | |
| Health Behaviors | Smoking (% never regularly smoked) | 0–2 | 56.7% |
| Physical activity (% active) | 0–2 | 56.4% | |
| Fruits and vegetable consumption (% recommended consumption) | 0–2 | 60.4% | |
| Fast food consumption (% no consumption) | 0–2 | 16% | |
| Sleep (% good quality sleep) | 0–2 | 83.8% | |
| Health Behavior Index (Sum) | 0–10 | 6.83 (1.6) | |
| Chronic Conditions | Number of chronic conditions (Wave 2) | 0–30 | 2.15 (2.10) |
| Number of chronic conditions (Wave 3) | 0–30 | 3.19 (3.01) |
Psychological resources
Measures of the eight psychological resources assessed at Wave 2 were: the three-item Life Orientation Test-Revised, a measure of dispositional optimism (Scheier & Carver, 1985); the seven-item Self-Esteem scale (Rosenberg, 1965); the six-item Positive Affect scale (Mroczek & Kolarz, 1998); the five-item Life Satisfaction scale (Prenda & Lachman, 2001); the seven-item Purpose in Life scale; the seven-item Self-Acceptance scale; the seven-item Positive Relations with Others scale; and the seven-item Environmental Mastery scale (Ryff & Keyes, 1995).
Previous research suggests that psychological resources commonly coexist, are highly inter-correlated, and load on a central psychological resource construct (Hobfoll, 2002). The eight psychological resources used in the present study showed moderate to high correlations (.39 to .76) with each other. Supporting the concept of a central psychological resource construct, principal components analysis suggested that these eight psychological resource scales were described by a single factor (eigenvalue = 4.9, 61.52% of scale variance explained; all factor loadings >.68). Confirmatory factor analysis was then performed, and the eight psychological resources were combined into a single composite variable (α = .86) representing an individual’s overall level of psychological resources. Model fit indices of the composite variable suggested a good fit (CFI = .988, TLI = .982, RMSEA = .055). Factor loadings of all eight observed resource indicators on the psychological resources latent variable were greater than .60 (Figure 1).
Figure 1.
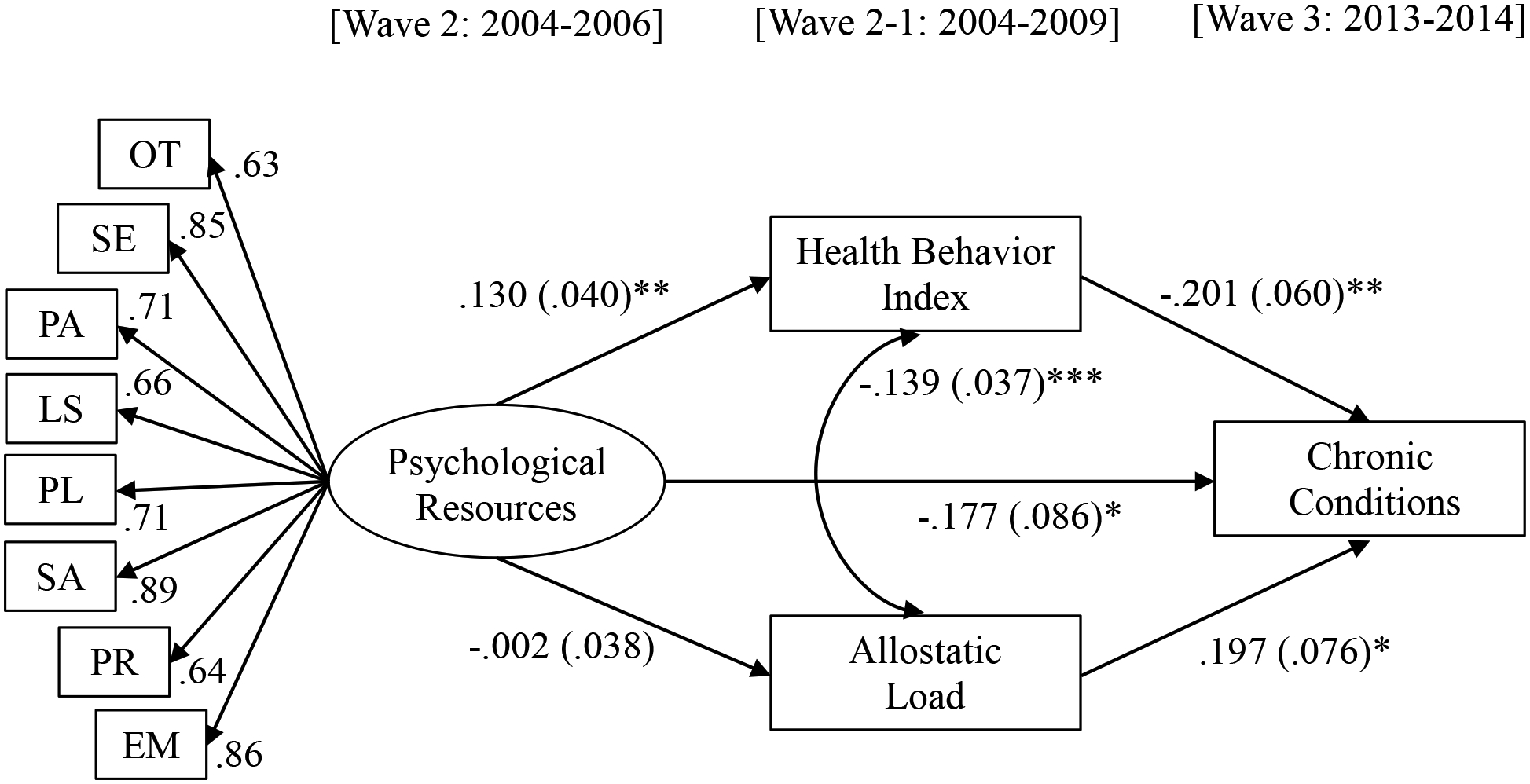
Results from the hypothesized model testing. Standardized coefficients (standard errors) are shown above. Akaike (AIC) = 42328, Bayesian (BIC) = 42651. Demographic variables were included in the model as covariates. OT = optimism, SE = self-esteem, PA = positive affect, LS = life satisfaction, PL = purpose in life, SA = self-acceptance, PR = positive relations with others, EM = environmental mastery.
Note: *p < .05; **p < .01; ***p < .001.
Health behaviors
Health behaviors were measured at Wave 2–1 using a health behavior index similar to those in other studies (e.g., Heinrich & Maddock, 2011). This index included five health behaviors, and engagement in each behavior was categorized into three levels representing unhealthy engagement, moderate engagement, and healthy engagement: Sleep (poor, adequate, good sleep quality), physical activity (inactive, lightly active, active), fruit and vegetable consumption (no or little consumption, light consumption, recommended consumption), fast food consumption (more than once per week, less than once per week, no consumption) and smoking (current smoker, former smoker, never smoked). Unhealthy engagement in each behavior was scored as 0, moderate engagement in each behavior was scored as 1, and healthy engagement in each behavior was scored as 2. Scores were summed to represent individuals’ overall engagement in health behaviors, and ranged from 0 to 10, with higher scores indicating greater engagement in health-promoting behaviors (Table 1).
Chronic conditions
At Wave 2 and Wave 3, participants were asked whether they been treated/diagnosed for 30 different chronic conditions such as diabetes, hypertension, joint/bone diseases, anxiety/depression, and stroke in the past 12 months. The presence of each condition was dichotomized as yes (1) or no (0), and scores for each condition were summed. The possible range for chronic condition scores was 0 to 30, with higher scores indicating a greater number of chronic conditions (Table 1).
Allostatic load
Consistent with previous studies using the MIDUS cohort, allostatic load indicators were measured at Wave 2–1 and included 23 biomarkers from seven physiological systems: 1) cardiovascular system (resting systolic blood pressure, resting diastolic blood pressure, and resting heart rate), 2) lipid metabolism system (waist-to-hip ratio, triglycerides, high density lipoprotein cholesterol [HDL], and low density lipoprotein cholesterol [LDL]), 3) glucose metabolism system (glycosylated hemoglobin [HbA1c], fasting glucose, and homeostasis model of insulin resistance [HOMA-IR]), 4) inflammation system (C-reactive protein [CRP], Interleukin-6 [IL-6], fibrinogen, sE-Selectin, and soluble intercellular adhesion molecule-1 [sICAM-1]), 5) sympathetic nervous system (urine epinephrine and urine norepinephrine), 6) hypothalamic-pituitary-adrenal system (urine cortisol and blood dehydroepiandrosterone sulfate [DHEA-S]), and 7) parasympathetic nervous system (heart rate variability: standard deviation of R-R intervals [SDRR], root mean square of successive differences [RMSSD], low-frequency spectral power, and high-frequency spectral power).
Allostatic load scores were calculated as the sum of the seven physiological systems as described previously (see Gruenewald et al., 2012; Wiley, Gruenewald, Karlamangla, & Seeman, 2016), according to the following steps. Each biomarker in the system was given a score of 0 or 1, based on being below or above the high-risk cut point value. These scores were summed and divided by the number of biomarkers in each system. Each system score ranged from 0 to 1. System scores were given only for participants with recorded values on at least half of the biomarkers in each system. This method of calculation was repeated for all seven biological systems, and allostatic load scores were calculated for participants with values on at least six of the seven systems. To account for the influence of medications on relevant physiological systems, participants who reported taking prescription medications for cardiovascular health, cholesterol, or diabetes were given a score of 1 for the cardiovascular system, lipid metabolism system, or glucose metabolism system, respectively. Scores for each system were summed to create an allostatic load score ranging from 0 to 7; higher scores indicated greater allostatic load (Table 2).
Table 2.
Descriptive Statistics and High-Risk Cut Point Values for Individual Biomarkers and the Multi-System Allostatic Load Score
| Systems and Representative Biomarkers | N | M | SD | High-risk Cut Point |
|---|---|---|---|---|
| Cardiovascular System | ||||
| Resting SBP (mmHg) | 850 | 130.82 | 17.51 | ≥143.00 |
| Resting DBP (mmHg) | 850 | 75.05 | 10.29 | ≥82.00 |
| Resting Heart Rate (bpm) | 849 | 70.22 | 11.03 | ≥77.00 |
| Metabolic – Lipids System | ||||
| Waist-to-Hip Ratio | 849 | .89 | .10 | ≥.97 |
| Triglycerides (mg/dL) | 845 | 133.29 | 80.37 | ≥160.00 |
| HDL Cholesterol (mg/dL) | 845 | 55.00 | 17.38 | ≤41.37 |
| LDL Cholesterol (mg/dL) | 845 | 107.47 | 35.40 | ≥128.00 |
| Metabolic – Glucose Metabolism System | ||||
| Glycosylated Hemoglobin (HbA1c) | 840 | 5.97 | .88 | ≥6.10 |
| Fasting Glucose (mg/dL) | 841 | 100.29 | 24.42 | ≥105 |
| Insulin Resistance (HOMA-IR) | 841 | 3.26 | 3.54 | ≥4.05 |
| Inflammation System | ||||
| CRP (mg/L) | 840 | 2.58 | 3.77 | ≥3.18 |
| IL6 (pg/mL) | 845 | 2.59 | 2.41 | ≥3.18 |
| Fibrinogen (mg/dL) | 840 | 337.08 | 80.77 | ≥390.00 |
| sE-Selectin (ng/MI) | 845 | 41.08 | 20.95 | ≥50.58 |
| sICAM-1 (ng/MI) | 845 | 282.51 | 96.45 | ≥329.65 |
| Sympathetic Nervous System | ||||
| Urine Epinephrine (ug/g creatine) | 837 | 2.00 | 1.25 | ≥2.54 |
| Urine Norepinephrine (ug/g creatine) | 842 | 27.20 | 12.45 | ≥33.33 |
| Hypothalamic Pituitary Adrenal Axis | ||||
| Urine Cortisol (ug/g creatine) | 842 | 17.09 | 27.93 | ≥21.00 |
| Blood DHEA-S (ug/dL) | 849 | 105.97 | 76.20 | ≤51.00 |
| Parasympathetic Nervous System | ||||
| SDRR (msec) | 795 | 35.01 | 17.13 | ≤23.54 |
| RMSSD | 795 | 21.53 | 16.92 | ≤11.83 |
| Low-frequency Spectral Power | 795 | 424.23 | 614.32 | ≤113.96 |
| High-frequency Spectral Power | 795 | 276.59 | 716.79 | ≤54.16 |
| Allostatic Load Sum Score | 845 | 2.13 | 1.20 |
Statistical analysis
Structural equation modeling (SEM) was performed in Mplus to test the hypothesized model presented in Figure 1. Chronic conditions were specified as a count variable in the analysis and Maximum Likelihood Robust estimator was used, which is robust to violations of normality including skewness (Muthen & Muthen, 2017). Since the MIDUS cohort includes twin pairs and siblings, family clustering was added to account for the violation of independence. One participant was missing health behavior index scores, and five participants were missing allostatic load scores. The model tested the direct association of psychological resources at Wave 2 and the indirect associations via health behaviors and allostatic load at Wave 2–1 with chronic conditions at Wave 3. Age, sex, marital status, race, education, number of chronic conditions at Wave 2 at Wave 2 were included in the model as covariates.
Results
Table 3 presents bivariate correlations among study variables. Among primary variables in the main analysis, psychological resources were positively associated with health behaviors and negatively associated with Wave 3 chronic conditions. Health behaviors were negatively associated with allostatic load and Wave 3 chronic conditions, and allostatic load was positively associated with Wave 3 chronic conditions.
Table 3.
Correlations Among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | - | |||||||||
| 2. Sex | .031 | - | ||||||||
| 3. Marital status | .059 | .130*** | - | |||||||
| 4. Race | .083* | .010 | .082* | - | ||||||
| 5. Education | −.097** | .084* | −.011 | .037 | - | |||||
| 6. M2 chronic conditions | .080* | −.193*** | −.087* | −.013 | −.081* | - | ||||
| 7. Psychological resources | .256*** | .032 | .173*** | .053 | .116** | −.300*** | - | |||
| 8. Health behaviors | .107** | −.054 | .068* | .053 | .188** | −.138*** | .216*** | - | ||
| 9. Allostatic load | .438*** | .057 | .044 | −.028 | −.134** | .173*** | .055 | −.115** | - | |
| 10. M3 chronic conditions | .088** | −.149*** | −.059 | −.047 | −.109** | .551*** | −.234*** | −.189*** | .193*** | |
Note: Sex (female = 0, male = 1); Marital status (not married = 0, married = 1); Race (non-white = 0, white = 1).
p < .05;
p < .01;
p < .001.
Figure 1 shows standardized regression coefficients among variables in the SEM. Psychological resources at Wave 2 were positively associated with health behaviors at Wave 2–1; however, no significant association was found between psychological resources and allostatic load. Health behaviors at Wave 2–1 were negatively associated with chronic conditions at Wave 3, and allostatic load at Wave 2–1 was positively associated with chronic conditions at Wave 3. There was a negative association between health behaviors and allostatic load.
As hypothesized, psychological resources at Wave 2 had a direct association with chronic conditions at Wave 3. Health behaviors at Wave 2–1 partially mediated the association between psychological resources and chronic conditions (ƅ for indirect effect = −.026, SE = .011, p < .05). Allostatic load at Wave 2–1 did not mediate the association between psychological resources and chronic conditions (ƅ for indirect effect = −.000, SE = .008, p > .05).
Discussion
The findings of this study highlight the importance of psychological resources and their positive influence on chronic conditions, and suggest directions for future research. Individuals reporting more psychological resources had a lower prevalence of chronic conditions after 7–10 years while controlling for baseline chronic conditions and demographic variables. This association was partially mediated by health behaviors, but not by allostatic load. The finding of a direct beneficial association between psychological resources and subsequent chronic conditions builds on prior longitudinal research. Life satisfaction has been found to protect against cardiometabolic conditions 8–11 years later (Boehm, Chen, Williams, Ryff, & Kubzansky, 2016), positive affect has been negatively associated with a 10-year incidence of coronary heart disease (Davidson, Mostofsky, & Whang, 2010), and higher self-esteem has predicted a lower prevalence of depression and anxiety later in life (Sowislo & Orth, 2013). Yet, evidence linking a composite variable of psychological resources to chronic conditions has been limited. The present study addressed that gap, finding that individuals with a large reservoir of psychological resources had fewer chronic conditions later in life.
Health behaviors partially mediated the association between psychological resources and chronic conditions, such that individuals who had more psychological resources had greater engagement in health-promoting behaviors, which in turn contributed to a lower prevalence of chronic conditions later in life. In previous studies, optimism has been associated with sustained physical activity (Progovac et al., 2017), and positive affect has been related to better sleep habits and greater fruit and vegetable consumption (Steptoe, O’Donnell, Marmot, & Wardle, 2008; White, Horwath, & Conner, 2013). Also, life satisfaction was predictive of 10-year behavioral cardiovascular risk factors (Łopuszańska, Szklarska, Lipowicz, Jankowska, & Kozieł, 2013). The mediating role of health behaviors in the present study supports previous research demonstrating that psychological resources influence health behaviors which in turn impact health conditions (Gallo & Matthews, 2003; Matthews & Gallo, 2011). The present study showed the beneficial influence of psychological resources on health behaviors up to 3–5 years later, and health behaviors on chronic conditions 7–10 years later, advancing the research linking psychological resources to subsequent chronic conditions via health behaviors.
Allostatic load was not a significant mediator between psychological resources and chronic conditions. This null finding was due to psychological resources not being associated with allostatic load at Wave 2–1, which did not support our hypothesis. Although some previous research has found evidence that psychological resources were associated with allostatic load (Glei, Goldman, Chuang, & Weinstein, 2007; Seeman et al., 2014), this association did not emerge in the present study. Several longitudinal and cross-sectional studies have reported significant associations between a single psychosocial resource and allostatic load (Hernandez et al., 2015; Ryff et al., 2006), but there is a lack of research demonstrating effects of composite psychological resources on allostatic load. Additionally, according to a meta-analysis, the association between psychological resources and allostatic load depends on other sociodemographic contexts such as socioeconomic status, social integration, and neighborhood poverty (Wiley et al., 2017). The absence of an association between psychosocial resources and allostatic load in the present study may indicate a need for more comprehensive measurement of such social and environmental moderators. Nonetheless, in the present study, individuals with lower allostatic load had a lower prevalence of chronic conditions later in life, which is consistent with prior research supporting allostatic load as a major predictor of chronic conditions, including hypertension, type 2 diabetes, and arthritis (Beckie, 2012; Mattei, Demissie, Falcon, Ordovas, & Tucker, 2010).
Results of this study should be considered in light of several limitations. First, the MIDUS cohort is not representative of the U.S. population, with a limited number of individuals from racial and ethnic minority groups. Most participants were white and well-educated, so the study findings may not generalize to racially/ethnically diverse and low socioeconomic status populations. Second, this study’s outcome was a sum score of chronic conditions, which does not capture the severity of functional limitations. One severe chronic condition may cause serious restrictions in activities of daily living while two or three minor chronic conditions may not cause limitations in activities of daily living. Given that functional limitations may better reflect health in an aging population than simply the number of chronic conditions, future research should examine measures of quality of life in addition to traditional disease outcomes. Additionally, the current study explored associations between psychological resources and the prevalence—rather than the development—of chronic conditions later in life. Therefore, causality between psychological resources and chronic conditions cannot be ascertained. However, baseline chronic conditions were controlled for in the model, and a temporal precedence of nearly a decade between the psychological resources survey and Wave 3 chronic condition measurements provides more compelling evidence for the observed beneficial associations than does a cross-sectional study.
Lastly, the contribution of chronic conditions to other study variables is unclear. Individuals may have had lower levels of psychological resources because they had chronic conditions, and it is also possible that individuals may have engaged in more health-promoting behavior in response to being diagnosed with one or more chronic conditions. Moreover, individuals’ level of psychological resources may fluctuate over time, and it is unclear how changes in psychological resources would influence development and severity of health outcomes. These limitations may suggest a need to examine subgroups who behave differently when diagnosed with chronic conditions, and future research to establish causality between psychological resources and chronic conditions.
Despite these limitations, the present study contributes significantly to our understanding of mechanisms by which psychological resources play a beneficial role with respect to chronic conditions. To our knowledge, this is the first study to longitudinally investigate the mediating roles of health behaviors and allostatic load in the association between psychological resources and chronic conditions. Findings of the present study show that psychological resources are a meaningful predictor of health outcomes, and that psychological resources contribute to a strong foundation for physical and mental health across the lifespan. Future research should examine whether these findings generalize to a diverse population, and explore other potential mechanisms linking psychological resources to health outcomes.
Funding
This research received no specific grant from any public, commercial, or not-for-profit funding agency. H. Matthew Lehrer received partial support during the preparation of the manuscript from NIH grant T32HL082610.
Footnotes
Disclosure statement
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data Availability Statement
The data that support the findings of this study are openly available in “ICPRS” at
http://doi.org/10.3886/ICPSR04652.v7 (MIDUS 2)
http://doi.org/10.3886/ICPSR29282.v7 (Biomarker)
http://doi.org/10.3886/ICPSR36346.v6 (MIDUS 3)
References
- Agborsangaya CB, Gee ME, Johnson ST, Dunbar P, Langlois M-F, Leiter LA, … Johnson JA (2013). Determinants of lifestyle behavior in type 2 diabetes: results of the 2011 cross-sectional survey on living with chronic diseases in Canada. BMC Public Health, 13, 451 10.1186/1471-2458-13-451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer UE, Briss PA, Goodman RA, & Bowman BA (2014). Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet (London, England), 384(9937), 45–52. 10.1016/S0140-6736(14)60648-6 [DOI] [PubMed] [Google Scholar]
- Beckie TM (2012). A systematic review of allostatic load, health, and health disparities. Biological Research for Nursing, 14(4), 311–346. 10.1177/1099800412455688 [DOI] [PubMed] [Google Scholar]
- Boehm JK, Chen Y, Koga H, Mathur MB, Vie LL, & Kubzansky LD (2018). Is Optimism Associated With Healthier Cardiovascular-Related Behavior? Meta-Analyses of 3 Health Behaviors. Circulation Research, 122(8), 1119–1134. 10.1161/CIRCRESAHA.117.310828 [DOI] [PubMed] [Google Scholar]
- Boehm JK, Chen Y, Williams DR, Ryff CD, & Kubzansky LD (2016). Subjective well-being and cardiometabolic health: An 8–11 year study of midlife adults. Journal of Psychosomatic Research, 85, 1–8. 10.1016/j.jpsychores.2016.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevarley FM (2015). Health Expenditures for Adults by Number of Treated Chronic Condition, Race/Ethnicity, and Age, 2012 (Statistical Brief 485). Rockville, MD: Agency for Healthcare Research and Quality; Retrieved from http://meps.ahrq.gov/mepsweb/data_files/publications/st485/stat485.shtml (accessed 17 October 2018). [PubMed] [Google Scholar]
- Chida Y, & Steptoe A (2008). Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosomatic Medicine, 70(7), 741–756. 10.1097/PSY.0b013e31818105ba [DOI] [PubMed] [Google Scholar]
- Christensen A, & Antoni M (eds) (2002). Chronic Physical Disorders: Behavioral Medicine’s Perspective. Oxford, U.K.: Blackwell Publishers. [Google Scholar]
- Cohen R, Bavishi C, & Rozanski A (2016). Purpose in life and its relationship to all-cause mortality and cardiovascular events: A meta-analysis. Psychosomatic Medicine, 78(2), 122–133. 10.1097/PSY.0000000000000274 [DOI] [PubMed] [Google Scholar]
- Conversano C, Rotondo A, Lensi E, Della Vista O, Arpone F, & Reda MA (2010). Optimism and its impact on mental and physical well-being. Clinical Practice & Epidemiology in Mental Health, 6, 25–29. 10.2174/1745017901006010025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD, Welch WT, Taylor SE, Sherman DK, Gruenewald TL, & Mann T (2005). Affirmation of personal values buffers neuroendocrine and psychological stress responses. Psychological Science, 16(11), 846–851. 10.1111/j.1467-9280.2005.01624.x [DOI] [PubMed] [Google Scholar]
- Davidson KW, Mostofsky E, & Whang W (2010). Don’t worry, be happy: Positive affect and reduced 10-year incident coronary heart disease: The Canadian Nova Scotia Health Survey. European Heart Journal, 31(9), 1065–1070. 10.1093/eurheartj/ehp603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E, & Chan MY (2011). Happy people live longer: Subjective well-being contributes to health and longevity. Applied Psychology: Health and Well-Being, 3(1), 1–43. 10.1111/j.1758-0854.2010.01045.x [DOI] [Google Scholar]
- Feller S, Teucher B, Kaaks R, Boeing H, & Vigl M (2013). Life satisfaction and risk of chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Germany study. PLoS One, 8(8), e73462 10.1371/journal.pone.0073462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine LJ, Philogene GS, Gramling R, Coups EJ, & Sinha S (2004). Prevalence of multiple chronic disease risk factors: 2001 National Health Interview Survey. American Journal of Preventive Medicine, 27(2, Suppl.), 18–24. 10.1016/j.amepre.2004.04.017 [DOI] [PubMed] [Google Scholar]
- Fogelman N, & Canli T (2015). “Purpose in Life” as a psychosocial resource in healthy aging: An examination of cortisol baseline levels and response to the Trier Social Stress Test. NPJ Aging and Mechanisms of Disease, 1, 15006 10.1038/npjamd.2015.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, & Moskowitz JT (2000). Positive affect and the other side of coping. American Psychologist, 55(6), 647–654. 10.1037/0003-066X.55.6.647 [DOI] [PubMed] [Google Scholar]
- Forrester S, Leoutsakos J-M, Gallo J, Thorpe R, & Seeman T (2019). Association between allostatic load and health behaviours: A latent class approach. Journal of Epidemiology and Community Health. 10.1136/jech-2018-211289 [DOI] [PubMed] [Google Scholar]
- Gallo LC, & Matthews KA (2003). Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychological Bulletin, 129(1), 10–51. [DOI] [PubMed] [Google Scholar]
- Gerteis J, Izrael D, Leroy L, Ricciardi R, Miller T, & Basu J (2014). Multiple Chronic Conditions Chartbook: 2010 Medical Expenditure Panel Survey Data (AHRQ Pub. No. Q14–0038). Rockville, MD: Agency for Healthcare Research and Quality; Retrieved from https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf [Google Scholar]
- Glei DA, Goldman N, Chuang Y-L, & Weinstein M (2007). Do chronic stressors lead to physiological dysregulation? Testing the theory of allostatic load. Psychosomatic Medicine, 69(8), 769–776. 10.1097/PSY.0b013e318157cba6 [DOI] [PubMed] [Google Scholar]
- Giltay EJ, Zitman FG, & Kromhout D (2006). Dispositional optimism and the risk of depressive symptoms during 15 years of follow-up: The Zutphen Elderly Study. Journal of Affective Disorders, 91(1), 45–52. 10.1016/j.jad.2005.12.027 [DOI] [PubMed] [Google Scholar]
- Grant N, Wardle J, & Steptoe A (2009). The relationship between life satisfaction and health behavior: A cross-cultural analysis of young adults. International Journal of Behavioral Medicine, 16(3), 259–268. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Karlamangla AS, Hu P, Stein-Merkin S, Crandall C, Koretz B, & Seeman TE (2012). History of socioeconomic disadvantage and allostatic load in later life. Social Science & Medicine, 74(1), 75–83. 10.1016/j.socscimed.2011.09.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson SE, Goldberg LR, Vogt TM, Hillier TA, & Dubanoski JP (2009). Using physiological dysregulation to assess global health status: Associations with self-rated health and health behaviors. Journal of Health Psychology, 14(2), 232–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrich KM, & Maddock J (2011). Multiple health behaviors in an ethnically diverse sample of adults with risk factors for cardiovascular disease. The Permanente Journal, 15(1), 12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez R, Kershaw K, Seeman T, Boehm J, Vu T-H, Ning H, & Lloyd-Jones D (2015). Associations of Positive Psychological Well-being on Changes in Allostatic Load: Multi-Ethnic Study of Atherosclerosis (MESA). Circulation, 131(Suppl 1), AMP82–AMP82. [Google Scholar]
- Hobfoll SE (2002). Social and psychological resources and adaptation. Review of General Psychology, 6(4), 307–324. 10.1037/1089-2680.6.4.307 [DOI] [Google Scholar]
- Jamieson JP, Mendes WB, & Nock MK (2013). Improving acute stress responses: The power of reappraisal. Current Directions in Psychological Science, 22(1), 51–56. 10.1177/0963721412461500 [DOI] [Google Scholar]
- Johansson G, Huang Q, & Lindfors P (2007). A life-span perspective on women’s careers, health, and well-being. Social Science & Medicine, 65(4), 685–697. 10.1016/j.socscimed.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Juth V, Smyth JM, & Santuzzi AM (2008). How do you feel? Self-esteem predicts affect, stress, social interaction, and symptom severity during daily life in patients with chronic illness. Journal of Health Psychology, 13(7), 884–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasikova DV, Lester PB, & Harms PD (2015). Effects of psychological capital on mental health and substance abuse. Journal of Leadership & Organizational Studies, 22(3), 280–291. 10.1177/1548051815585853 [DOI] [Google Scholar]
- Lau EYY, Hui CH, Lam J, & Cheung S-F (2017). Sleep and optimism: A longitudinal study of bidirectional causal relationship and its mediating and moderating variables in a Chinese student sample. Chronobiology International, 34(3), 360–372. 10.1080/07420528.2016.1276071 [DOI] [PubMed] [Google Scholar]
- Livingstone KM, & McNaughton SA (2017). A health behavior score is associated with hypertension and obesity among Australian adults. Obesity, 25(9), 1610–1617. 10.1002/oby.21911 [DOI] [PubMed] [Google Scholar]
- Łopuszańska M, Szklarska A, Lipowicz A, Jankowska EA, & Kozieł S (2013). Life satisfaction and cardiovascular disease risk in Poland. Archives of Medical Science : AMS, 9(4), 629–634. 10.5114/aoms.2013.36909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love GD, Seeman TE, Weinstein M, & Ryff CD (2010). Bioindicators in the MIDUS National Study: Protocol, measures, sample, and comparative context. Journal of Aging and Health, 22(8), 1059–1080. 10.1177/0898264310374355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundgren O, Garvin P, Jonasson L, Andersson G, & Kristenson M (2015). Psychological resources are associated with reduced incidence of coronary heart disease: An 8-year follow-up of a community-based Swedish sample. International Journal of Behavioral Medicine, 22, 77–84. 10.1007/s12529-014-9387-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacInnes DL (2006). Self-esteem and self-acceptance: An examination into their relationship and their effect on psychological health. Journal of Psychiatric and Mental Health Nursing, 13(5), 483–489. 10.1111/j.1365-2850.2006.00959.x [DOI] [PubMed] [Google Scholar]
- Masten AS, Cutuli JJ, Herbers JE, & Gabrielle-Reed MJ (2009). Resilience in development In Snyder CR, & Lopez SJ (Eds.), The handbook of positive psychology (2nd Edition ed., pp. 117–131). New York, NY: Oxford University Press. [Google Scholar]
- Matthews KA, & Gallo LC (2011). Psychological Perspectives on Pathways Linking Socioeconomic Status and Physical Health. Annual Review of Psychology, 62, 501–530. 10.1146/annurev.psych.031809.130711 Akaike (AIC) : 47772.097, Bayesian (BIC) : 48132.735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei J, Demissie S, Falcon LM, Ordovas JM, & Tucker K (2010). Allostatic load is associated with chronic conditions in the Boston Puerto Rican Health Study. Social Science & Medicine (1982), 70(12), 1988–1996. 10.1016/j.socscimed.2010.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44. [DOI] [PubMed] [Google Scholar]
- McEwen BS (2004). Protection and damage from acute and chronic stress: Allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Annals of the New York Academy of Sciences, 1032, 1–7. [DOI] [PubMed] [Google Scholar]
- McEwen BS, & Wingfield JC (2003). The concept of allostasis in biology and biomedicine. Hormones and Behavior, 43(1), 2–15. [DOI] [PubMed] [Google Scholar]
- Mroczek DK, & Kolarz CM (1998). The effect of age on positive and negative affect: A developmental perspective on happiness. Journal of Personality and Social Psychology, 75(5), 1333–1349. [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition Los Angeles, CA: Muthén & Muthén [Google Scholar]
- National Center for Health Statistics (2017) Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Retrieved from https://www.cdc.gov/nchs/data/hus/hus15.pdf#019 (accessed 17 October 2018) [PubMed]
- Prenda KM, & Lachman ME (2001). Planning for the future: A life management strategy for increasing control and life satisfaction in adulthood. Psychology and Aging, 16(2), 206–216. [PubMed] [Google Scholar]
- Pressman SD, & Cohen S (2005). Does positive affect influence health? Psychological Bulletin, 131(6), 925–971. 10.1037/0033-2909.131.6.925 [DOI] [PubMed] [Google Scholar]
- Progovac AM, Donohue JM, Matthews KA, Chang CCH, Habermann EB, Kuller LH, … Tindle HA (2017). Optimism predicts sustained vigorous physical activity in postmenopausal women. Preventive Medicine Reports, 8, 286–293. 10.1016/j.pmedr.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radler BT, & Ryff CD (2010). Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. Journal of Aging and Health, 22(3), 307–331. 10.1177/0898264309358617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen HN, Scheier MF, & Greenhouse JB (2009). Optimism and physical health: A meta-analytic review. Annals of Behavioral Medicine, 37(3), 239–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M (1965). Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Ryff CD (2014). Psychological Well-Being Revisited: Advances in Science and Practice. Psychotherapy and Psychosomatics, 83(1), 10–28. 10.1159/000353263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD, Dienberg Love G, Urry HL, Muller D, Rosenkranz MA, Friedman EM, … Singer B (2006). Psychological well-being and ill-being: do they have distinct or mirrored biological correlates? Psychotherapy and Psychosomatics, 75(2), 85–95. 10.1159/000090892 [DOI] [PubMed] [Google Scholar]
- Ryff CD, & Keyes CLM (1995). The structure of psychological well-being revisited. Journal of Personality and Social Psychology, 69(4), 719–727. 10.1037/0022-3514.69.4.719 [DOI] [PubMed] [Google Scholar]
- Ryff CD, Radler BT, & Friedman EM (2015). Persistent psychological well-being predicts improved self-rated health over 9–10 years: Longitudinal evidence from MIDUS. Health Psychology Open, 2(2). 10.1177/2055102915601582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD, Singer BH, & Love GD (2004). Positive Health: Connecting Well-Being with Biology. Philosophical Transactions: Biological Sciences, 359(1449), 1383–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salleh MR (2008). Life event, stress and illness. The Malaysian Journal of Medical Sciences, 15(4), 9–18. [PMC free article] [PubMed] [Google Scholar]
- Scheier MF, & Carver CS (1985). Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychology, 4(3), 219–247. 10.1037//0278-6133.4.3.219 [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, & Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology, 67(6), 1063–1078. [DOI] [PubMed] [Google Scholar]
- Schetter CD, & Dolbier C (2011). Resilience in the Context of Chronic Stress and Health in Adults. Social and Personality Psychology Compass, 5(9), 634–652. 10.1111/j.1751-9004.2011.00379.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segrin C, & Rynes KN (2009). The mediating role of positive relations with others in associations between depressive symptoms, social skills, and perceived stress. Journal of Research in Personality, 43(6), 962–971. [Google Scholar]
- Sowislo JF, & Orth U (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological Bulletin, 139(1), 213–240. 10.1037/a0028931 [DOI] [PubMed] [Google Scholar]
- Stenholm S, Head J, Kivimäki M, Kawachi I, Aalto V, Zins M, … Vahtera J (2016). Smoking, physical inactivity and obesity as predictors of healthy and disease-free life expectancy between ages 50 and 75: a multicohort study. International Journal of Epidemiology, 45(4), 1260–1270. 10.1093/ije/dyw126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, O’Donnell K, Marmot M, & Wardle J (2008). Positive affect, psychological well-being, and good sleep. Journal of Psychosomatic Research, 64(4), 409–415. 10.1016/j.jpsychores.2007.11.008 [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wright C, Kunz‐Ebrecht SR, & Iliffe S (2006). Dispositional optimism and health behaviour in community‐dwelling older people: Associations with healthy ageing. British journal of health psychology, 11(1), 71–84. 10.1348/135910705X42850 [DOI] [PubMed] [Google Scholar]
- Taylor SE, & Broffman JI (2011). Psychosocial resources: Functions, origins, and links to mental and physical health. Advances in Experimental Social Psychology, 44, 1–57. 10.1016/B978-0-12-385522-0.00001-9 [DOI] [Google Scholar]
- Taylor SE, Kemeny ME, Reed GM, Bower JE, & Gruenewald TL (2000). Psychological resources, positive illusions, and health. American Psychologist, 55(1), 99–109. [DOI] [PubMed] [Google Scholar]
- Taylor SE, & Stanton AL (2007). Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology, 3, 377–401. 10.1146/annurev.clinpsy.3.022806.091520 [DOI] [PubMed] [Google Scholar]
- Tsenkova VK, Love GD, Singer BH, & Ryff CD (2007). Socioeconomic status and psychological well-being predict cross-time change in glycosylated hemoglobin in older women without diabetes. Psychosomatic Medicine, 69(8), 777–784. 10.1097/PSY.0b013e318157466f [DOI] [PubMed] [Google Scholar]
- Ward BW, & Schiller JS (2013). Prevalence of multiple chronic conditions among US adults: Estimates from the National Health Interview Survey, 2010. Preventing Chronic Disease, 10 10.5888/pcd10.120203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward BW, Schiller JS, & Goodman RA (2014). Multiple chronic conditions among US adults: A 2012 update. Preventing Chronic Disease, 11 10.5888/pcd11.130389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley JF, Bei B, Bower JE, & Stanton AL (2017). Relationship of psychosocial resources with allostatic load: A systematic review. Psychosomatic Medicine, 79(3), 283–292. 10.1097/PSY.0000000000000395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley JF, Gruenewald TL, Karlamangla AS, & Seeman TE (2016). Modeling multisystem physiological dysregulation. Psychosomatic Medicine, 78(3), 290–301. 10.1097/PSY.0000000000000288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White BA, Horwath CC, & Conner TS (2013). Many apples a day keep the blues away–Daily experiences of negative and positive affect and food consumption in young adults. British Journal of Health Psychology, 18(4), 782–798. [DOI] [PubMed] [Google Scholar]


