Abstract
Objectives:
Coagulopathy of coronavirus disease 2019 is largely described as hypercoagulability, yet both thrombotic and hemorrhagic complications occur. Although therapeutic and prophylactic anticoagulant interventions have been recommended, empiric use of antifactor medications (heparin/enoxaparin) may result in hemorrhagic complications, including death. Furthermore, traditional (antifactor) anticoagulation does not address the impact of overactive platelets in coronavirus disease 2019. The primary aim was to evaluate if algorithm-guided thromboelastography with platelet mapping could better characterize an individual’s coronavirus disease 2019-relatedcoagulopathic state and, secondarily, improve outcomes.
Design, Setting, and Patients:
Coronavirus disease 2019 patients (n = 100), receiving thromboelastography with platelet mapping assay upon admission to an 800-bed tertiary-care hospital, were followed prospectively by a hospital-based thromboelastography team. Treating clinicians were provided with the option of using a pre-established algorithm for anticoagulation, including follow-up thromboelastography with platelet mapping assays. Two groups evolved: 1) patients managed by thromboelastography with platelet mapping algorithm (algorithm-guided-thromboelastography); 2) those treated without thromboelastography with platelet mapping protocols (non-algorithm-guided). Outcomes included thrombotic/hemorrhagic complications, pulmonary failure, need for mechanical ventilation, acute kidney injury, dialysis requirement, and nonsurvival.
Interventions:
Standard-of-care therapy with or without algorithm-guided-thromboelastography support.
Measurements and Main Results:
Although d-dimer, C-reactive protein, and ferritin were elevated significantly in critically ill (nonsurvivors, acute kidney injury, pulmonary failure), they did not distinguish between coagulopathic and noncoagulopathic patients. Platelet hyperactivity (maximum amplitude-arachidonic acid/adenosine diphosphate > 50 min), with or without thrombocytosis, was associated with thrombotic/ischemic complications, whereas severe thrombocytopenia (platelet count < 100,000/μL) was uniformly fatal. Hemorrhagic complications were observed with decreased factor activity (reaction time > 8 min). Non-algorithm-guided patients had increased risk for subsequent mechanical ventilation (relative risk = 10.9; p < 0.0001), acute kidney injury (relative risk = 2.3; p = 0.0017), dialysis (relative risk = 7.8; p < 0.0001), and death (relative risk = 7.7; p < 0.0001), with 17 of 28 non-algorithm-guided patients (60.7%) dying versus four algorithm-guided-thromboelastography patients (5.6%) (p < 0.0001). Thromboelastography with platelet mapping–guided antiplatelet treatment decreased mortality 82% (p = 0.0002), whereas non-algorithm-guided (compared with algorithm-guided-thromboelastography) use of antifactor therapy (heparin/enoxaparin) resulted in 10.3-fold increased mortality risk (p = 0.0001).
Conclusions:
Thromboelastography with platelet mapping better characterizes the spectrum of coronavirus disease 2019 coagulation-related abnormalities and may guide more tailored, patient-specific therapies in those infected with coronavirus disease 2019.
Keywords: COVID-19 anticoagulation, COVID-19 coagulopathy, platelet hyperactivity, platelet mapping, TEG-PM, thromboelastrography
Significant infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may lead to development of coagulopathy, most typically a hypercoagulable state (1). This concern has led to empiric or pre-emptive treatment with anticoagulants (1). However, in addition to thrombotic conditions, coronavirus disease 2019 (COVID-19) patients may develop hemorrhagic complications, which have been underrecognized or inadequately emphasized in prior studies (1–5). Although most autopsy reports describe a high frequency of venous/arterial thromboemboli or microthrombi associated with pulmonary failure (PF) and acute kidney injury (AKI), some patients do present with manifestations of cerebrovascular, gastrointestinal, and/or pulmonary bleeding (3–7). Under these circumstances, incorrect anticoagulation therapy might be harmful. Early characterization of patient-specific coagulopathy may not only avoid iatrogenic incidents but may also improve outcomes, especially when considering that COVID-19 coagulopathy can insidiously lead to respiratory and renal complications, disseminated intravascular coagulation (DIC), and death (8, 9).
Marked elevation in coagulation-related markers such as d-dimer, C-reactive protein (CRP), and fibrin degradation products (FDPs) are typically found among those with isolated thromboses, encouraging a similar diagnostic approach when evaluating coagulopathic complications seen in patients with COVID-19 (9–11). However, d-dimer, CRP, and FDP can also indicate a marked inflammatory state and, together with conventional coagulation tests (CCTs)—prothrombin time (PT), partial thromboplastin time (PTT), and international normalized ratio (INR), do not reflect the complexities of COVID-19 coagulopathy (8, 12, 13). Most importantly, these laboratory variables do not characterize the significant and multifaceted platelet activity abnormalities of COVID-19 (14, 15). Studies have now identified altered platelet gene expression leading to increased platelet aggregation and hypercoagulability (14, 15). Overall, the various components of COVID-19 coagulopathy, thrombotic or hemorrhagic, still need to be characterized better, and, in turn, COVID-19 coagulopathy remains a complex diagnostic and treatment challenge.
Thromboelastography (TEG), being a whole blood assay, is a more inclusive technology that evaluates the overall contribution of blood cells, platelets, and plasma during clot formation by mimicking in vivo coagulation processes (16–18). TEG can measure profound hemostatic derangements, and it identifies key dysfunctional components, from the initiation phase of blood clotting to the fibrinolysis phase (1, 12, 13, 16–21). Accordingly, TEG could be considered another useful tool in the current pandemic (1, 18, 21). Moreover, recognizing the frequent platelet abnormalities in COVID-19, platelet mapping (PM) can be added as an adjunct to TEG, particularly as platelet aggregation and microthrombi formation have now become key clinical concerns (14). However, clinical data are lacking with regard to characterization of platelet dysfunction and particularly when using TEG with platelet mapping (TEG-PM). Considering its potential advantages, TEG-PM might be able to better guide treatment of patients with identified platelet dysfunction (22, 23).
Most important, it is not known if TEG-PM can better identify an individual’s coagulopathic state and, in turn, better guide treatment. We hypothesized that: 1) TEG-PM could become a facile tool for improved characterization of patient-specific COVID-19 coagulopathy, 2) TEG-PM would more accurately delineate the platelet-related contribution to any COVID-19 coagulopathy, and 3) TEG-PM-guided therapy intended to target patient-specific dysfunctional blood components will not only help to avoid iatrogenic complications but also likely lead to improved patient outcomes.
METHODS
Participants and Design
Over a 5-month period during the SARS-CoV-2 pandemic, patients (age 18 years or older) admitted to an 800-bed tertiary care facility with a confirmed diagnosis of COVID-19 were entered into the study. Per routine, in addition to the standard work-up, during the emergency department evaluation, patients with hypoxemia (oxygen saturation < 92% on room air) received coagulopathy evaluation using TEG-PM. The hospital-based Thromboelastography Task Force (TTF) prospectively followed 100 patients meeting these criteria to assist with the application and interpretation of initial and on-going TEG findings. TTF members provided treating clinicians with the option of using pre-established (pre-COVID) TEG-PM protocols/algorithms for managing coagulopathy, both thrombotic and hemorrhagic. As a part of the TEG-PM algorithm, TEG-PM was repeated every 48–72 hours or with any significant clinical deterioration (e.g. worsening hypoxemia, cardiac arrhythmia, escalation of care). Although the TTF could be consulted for TEG interpretation and anticoagulant suggestions, the primary team made all final therapeutic decisions.
All study patients were followed and observed throughout their hospital course to evaluate the following: 1) the accuracy of TEG readings as interpreted or reported by the attending clinician of record, 2) any noted justifications for medication adjustments, and 3) relevant laboratory and clinical data with eventual outcomes. Patient charts were also abstracted and reviewed for demographics, medical history, hospital course, and imaging interpretations, both prospectively and in retrospective fashion, when necessary to complete the data collection. Inflammatory markers as well as at-home or in-hospital use of anticoagulants were noted, including antifactor (e.g., warfarin, heparin, enoxaparin, argatroban, or rivaroxaban) and antiplatelet medications (e.g., aspirin, clopidogrel, or ticagrelor).
The study was approved by the Memorial Healthcare Institutional Review Board with waiver of consent.
Interventions
The hospital’s multidisciplinary TTF team had been an established entity prior to the COVID-19 crisis. Comprised of cross-specialty physicians, pharmacists, laboratory staff, and registered nurses, the team had constructed both hypo- (Appendix 1, Supplemental Digital Content 1, http://links.lww.com/CCX/A430) and hypercoagulable (Fig. 1) TEG treatment algorithms for various applicable conditions in order to aid treating clinicians in choosing appropriate anticoagulant therapies. When patients were identified as medication nonresponders, alternate treatments were suggested by the algorithm in order to create the most comprehensive, individualized approach to treating patients’ hypercoagulability. Per routine, most patients received an initial prophylactic dose of enoxaparin or heparin at the time of admission.
Figure 1.
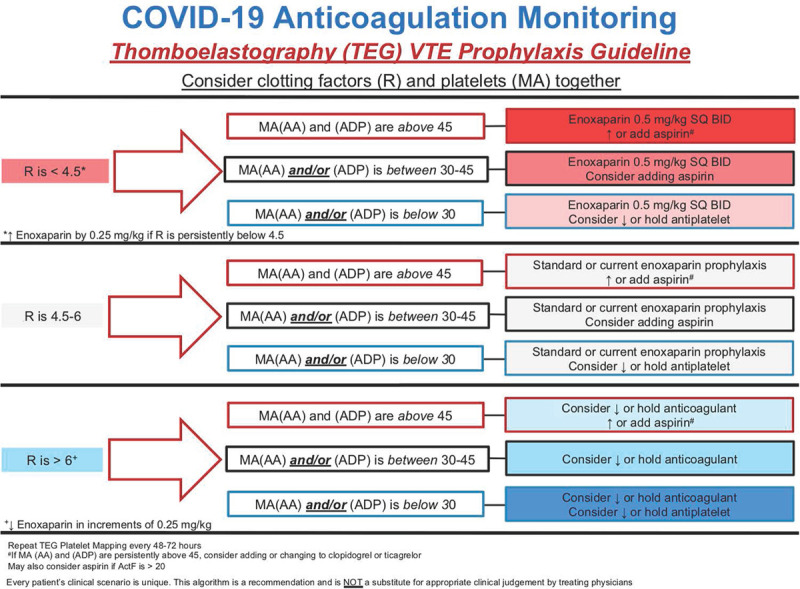
Thromboelastography (TEG)–guided venous thromboembolism (VTE) prophylaxis in a setting of a hypercoagulable TEG. AA = arachidonic acid, ADP = adenosine phosphate, COVID-19 = coronavirus disease 2019, MA = maximum amplitude, R = reaction time, SQ = subcutaneous.
Identification of Coagulopathy Based on TEG-PM
The processing device used was TEG 5000 Thrombelastograph Hemostasis Analyzer (manufactured by Haemonetics, Boston, MA), with PM employed to specifically assess activation of the platelet’s cyclooxygenase 1 (maximum amplitude [MA]-arachidonic acid [AA]) and P2Y12 pathways (MA-adenosine diphosphate [ADP]). Additional Methodological Details (Supplemental Digital Content 2, http://links.lww.com/CCX/A429), which contain specific information regarding hyper-, hypo-, and normocoagulable TEG variables, are appended as an online supplement (24–26).
Follow-up TEG-PM assays were clinician ordered and collected every 48–72 hours when possible. The treating clinicians could contact the TTF at any time to assist in TEG interpretations and for guidance with the treatment algorithm, taking into consideration that coagulation status can be an ever-changing dynamic, often varying with patient’s clinical condition. Again, final diagnostic and therapeutic decisions, including the ordering and use of the TEG algorithm, were made by the primary treating clinicians.
Categorization of Patients
Although many clinicians used the TEG algorithm and consulted the TTF for on-going TEG support, not all practitioners chose to follow the proscribed TEG-guided approach. As a result, two groups evolved allowing for a de facto comparative analysis: (1) the algorithm-guided (AG)-TEG group which included patients managed by TEG algorithm and (2) the non-AG group which was managed without those protocols. Patients in the non-AG group received prophylaxis or treatment doses of anticoagulants (heparin, enoxaparin and other antifactor medications) based on clinical judgment. Nevertheless, once identified by the initial TEG in the emergency department, all 100 patients were followed to discharge.
Main Outcomes Analyzed
In addition to the demographic, historical, TEG-PM, and clinical laboratory data, patients were monitored for therapies initiated, their general clinical course, and significant clinical decision-making. Specific study outcomes included rates of PF and need for mechanical ventilation (MV), ICU admission and length of stay (LOS), AKI and need for dialysis, and the rates of survival/mortality.
Statistical Analysis
Univariate comparison was performed using Student t test and Wilcoxon rank sum test for continuous variables. Paired continuous data was analyzed using paired t test. Categorical data were evaluated using chi-square or Fisher exact test, depending on the sample size. Relative risk of mortality was also calculated. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Among the 100 patients studied, ages ranged from 32 to 91 years, and 67% were male, 46.5% African American, 29.3% Hispanic. At presentation, 78% had fever, 79% respiratory symptoms (cough and/or dyspnea), and 21% gastrointestinal symptoms (abdominal pain, diarrhea, nausea, vomiting, constipation). Past medical history included hypertension (55%), diabetes (38%), hyperlipidemia (33%), remote history of smoking (17%), chronic obstructive pulmonary disease or asthma (9%), and smoking prior to hospitalization (2%). Following admission, one third of all patients were transferred to the ICU for closer monitoring, and 37% were diagnosed with AKI, 8% required dialysis, whereas 21% were intubated and ultimately succumbed to COVID-19.
On initial presentation, TEG-PM was balanced (e.g. contained normal variables) in 38% of the patients; however, TEG factors fluctuated throughout the hospital course paralleling clinical progression and medication adjustments. Ultimately, 72 patients were categorized as having followed TEG algorithms (AG-TEG group), whereas 28 patients were included in the non-AG group for whom anticoagulation was managed independent of TEG variables.
Table 1 provides comparison demographics for AG-TEG versus non-AG patients. Overall, the two groups were comparable. The AG-TEG group had more male patients and fewer patients with hypertension history, but there were no significant differences in home use of antifactor and/or antiplatelet anticoagulants or the number of non-AG and AG-TEG patients who required initial/early ICU (within 48 hours) admission or MV (Table 1).
TABLE 1.
Demographics of Patients With Algorithm-Guided (AG)-Thromboelastography and Non-AG-Guided Care
| Comparative Characteristics | Non-AG (n = 28) | % | AG-TEG (n = 72) | % |
|---|---|---|---|---|
| Age | ||||
| Mean ± se | 64.4 ± 2.9 | 59.8 ± 1.8 | ||
| Median (IQR) | 66 (61–77) | 60 (46–70) | ||
| Gender, n | ||||
| Male | 13 | 46.4 | 54 | 75.0 |
| Race, n | ||||
| Caucasian | 6 | 22.2 | 14 | 19.4 |
| African American | 14 | 51.9 | 32 | 44.4 |
| Hispanic | 5 | 18.5 | 24 | 33.3 |
| Asian | 1 | 3.7 | 1 | 1.4 |
| Native American | 1 | 3.7 | 1 | 1.4 |
| Medical history | ||||
| Body mass index | ||||
| Mean ± se | 33.9 ± 1.6 | 30.9 ± 1.0 | ||
| Median (IQR) | 32.6 (30–36) | 28.8 (25–34) | ||
| Coronary artery disease/congestive heart failure | 3 | 10.7 | 11 | 15.3 |
| Myocardial infarction | 0 | 0.0 | 6 | 6.9 |
| Cardiac arrhythmia | 4 | 14.3 | 5 | 6.9 |
| Hyperlipidemia | 7 | 25.0 | 26 | 36.1 |
| Hypertension | 20 | 71.4 | 35 | 48.6 |
| Diabetes mellitus | 15 | 53.6 | 23 | 31.9 |
| Asthma/chronic obstructive pulmonary disease | 2 | 7.1 | 7 | 9.7 |
| Smoking (current) | 1 | 3.6 | 1 | 1.4 |
| Smoking (past) | 6 | 21.4 | 11 | 15.3 |
| Malignancy | 3 | 10.7 | 5 | 6.9 |
| Chronic renal disease | 5 | 17.9 | 8 | 11.1 |
| Hemodialysis | 3 | 10.7 | 4 | 5.6 |
| Deep venous thrombosis/pulmonary embolus | 1 | 3.6 | 4 | 5.6 |
| Steroids/immunosuppression | 0 | 0.0 | 3 | 4.2 |
| Home anticoagulant use | 8 | 28.6 | 21 | 29.3 |
| Full anticoagulant (antifactor) | 3 | 10.7 | 4 | 5.6 |
| Antiplatelet | 6 | 21.4 | 18 | 25.0 |
| Initial admission | ||||
| Initial noncoagulopathic TEG | 8 | 28.6 | 30 | 41.7 |
| ICU (within 24 hr) | 7 | 25.0 | 15 | 20.8 |
| Intubated (within 24 hr) | 2 | 7.1 | 1 | 1.4 |
AG = algorithm-guided, IQR = interquartile range, TEG = thromboelastography.
Full anticoagulant (antifactor) includes medications like coumadin, apixaban, enoxaparin.
Inflammatory markers were associated with clinical deterioration, PF, AKI, and death (data not shown). d-dimer was significantly higher in non-AG patients, but ferritin and CRP were not significantly different between the two groups (Table 2). These markers reached peak measurements of varying levels within 1–4 days of maximal respiratory requirements, but they did not differentiate between coagulopathic and noncoagulopathic patients, making them less clinically applicable regarding the COVID-19 coagulation status.
TABLE 2.
Outcomes of Patients With Algorithm-Guided (AG)-Thromboelastography and Non-AG-Guided Care
| Key Findings | Non-AG (n = 28) | % | AG-Thromboelastography (n = 72) | % | p |
|---|---|---|---|---|---|
| Hospital course | |||||
| Inflammatory markers | |||||
| d-dimer | |||||
| Mean ± se | 12.0 ± 2.0 | 5.4 ± 0.9 | 0.0012 | ||
| Median (IQR) | 8.7 (4–19) | 1.8 (1–6) | 0.0010 | ||
| C-reactive protein | |||||
| Mean ± se | 16.7 ± 1.3 | 37.6 ± 23.4 | 0.3755 | ||
| Median (IQR) | 16.5 (12–20) | 13.6 (8–18) | 0.0938 | ||
| Ferritin | |||||
| Mean ± se | 2,946.6 ± 710.6 | 1,579.9 ± 257.8 | 0.0797 | ||
| Median (IQR) | 1,728 (752–3,519) | 1,143 (624–1,934) | 0.0915 | ||
| Platelets | |||||
| Mean ± se | 393.2 ± 33.3 | 404.0 ± 20.5 | 0.7819 | ||
| Median (IQR) | 390.0 (277–470) | 372.5 (288–519) | 0.8572 | ||
| Treatment | |||||
| Remdesivir | 12 | 42.9 | 34 | 47.2 | 0.6941 |
| Tocilizumab | 10 | 35.7 | 18 | 25.0 | 0.2840 |
| Steroids | 23 | 85.2 | 39 | 54.2 | 0.0045 |
| Convalescent plasma | 13 | 46.4 | 25 | 34.7 | 0.2789 |
| Hospital (anticoagulant) administration | |||||
| Full anticoagulant (antifactor) | 19 | 70.4 | 26 | 36.1 | 0.0023 |
| Nonsurvivors | 12 | 42.9 | 3 | 4.2 | < 0.0001 |
| Antiplatelet | 11 | 39.3 | 59 | 81.9 | < 0.0001 |
| Nonsurvivors | 8 | 28.6 | 3 | 4.3 | 0.0005 |
| Outcomes | |||||
| Nonsurvivors | 17 | 60.7 | 4 | 5.6 | < 0.0001 |
| Overall hospitalization | |||||
| ICU admission (all) | 19 | 67.9 | 21 | 29.2 | 0.0004 |
| Intubated (all) | 17 | 60.7 | 4 | 5.6 | < 0.0001 |
| ICU LOS | |||||
| Mean ± se | 11.0 ± 3.3 | 3.7 ± 1.1 | 0.0456 | ||
| Median (IQR) | 8 (0–14) | 0 (0–7) | 0.0346 | ||
| Hospital LOS | |||||
| Mean ± se | 23.2 ± 3.1 | 14.2 ± 1.3 | 0.0122 | ||
| Median (IQR) | 18 (12–28) | 10.5 (6–17) | 0.0016 | ||
| Acute kidney injury | 17 | 68.0 | 20 | 29.4 | 0.0007 |
| Hemodialysis | 6 | 22.2 | 2 | 2.8 | 0.0017 |
AG = algorithm-guided, IQR = interquartile range, LOS = length of stay.
Antifactor (heparin, enoxaparin); antiplatelet (aspirin, clopidogrel, ticagrelor).
Main Outcomes
The non-AG patients had prolonged LOS, increased frequency of eventual ICU admission, PF, MV, AKI, and dialysis. Compared with only four AG-TEG patients, 17 non-AG patients died (p < 0.0001) (Table 2). The non-AG group had a nearly 11-fold increased risk for MV (p < 0.0001), 2.3 for AKI (p = 0.0017), 7.8 for dialysis (p < 0.0001), and a 7.7-fold increased risk of death (p < 0.0001).
Complications
Table 3 demonstrates 18 representative coagulopathic TEG-PM assays from both groups, anticoagulation regimens used in those individuals and their associated complications (e.g. major bleeding, thrombosis, death). Ischemic complications were typically associated with platelet hyperactivity (MA-AA/ADP > 50 mm), even sometimes in the face of antiplatelet administration (medication nonresponders). Mild increases in MA-AA/ADP (> 60 mm) were associated with increased need for MV, whereas isolated thrombotic complications such as deep vein thrombosis (DVT), venothrombo-emboli (VTE), or ischemic strokes were seen with MA-AA/ADP greater than 70 mm. Platelets were often noted to rise during the time of clinical deterioration and worsening hypoxemia. Extreme thrombocytosis (> 500,000/µL) was not uniformly associated with worse outcomes, but rather, complications did parallel platelet hyperactivity (MA-AA/ADP > 50 mm).
TABLE 3.
Thromboelastography Variables in Patients With Severe Thrombotic and Hemorrhagic Complications, as Well as Death
| Patient | Complications | Thromboelastography With Platelet Mapping Variables | Inflammatory Markers | Anticoagulation Medications | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Platelet Count (100,000/μL) | d-dimer | C-Reactive Protein | Ferritin | Antifactor | Antiplatelet | |||||||||
| Reaction Time | Alpha Angle | MA | MA-Arachidonic Acid | MA-Adenosine Diphosphate | Activator F | Percent of Lysis at 30 min | ||||||||
| Ischemic complications | ||||||||||||||
| A | PE | 5.4 | 66.3 | 64 | 65 | 69.0 | 10.9 | 3 | 211 | 27.1 | 1.68 | 316 | None | None |
| B | PE | 5.5 | 72.7 | 76 | 74 | 73.7 | 22.0 | 4 | 364 | > 30 | 20.7 | 240 | Rivaroxaban 15 mg | None |
| C | PE | 4.8 | 78.7 | 77 | 81 | 79.3 | 23.9 | 10 | 457 | 1.03 | 4.83 | NA | None | None |
| D | PE | 3.4 | 72.0 | 70 | 77 | 75.9 | 28.0 | 0 | 434 | 5.9 | 6.45 | 1,245 | Enoxaparin 60 mg BID | None |
| E | PE and bilateral deep vein thrombosis | 3.8 | 78.5 | 76 | 78 | 78.6 | 24.0 | 1 | 306 | 5.61 | 11.4 | 387 | Enoxaparin 60 mg BID | None |
| F | Ischemic CVA | 3.2 | 79.2 | 79 | 75 | 81.4 | NA | 0 | 587 | 1.5 | 1.31 | 1,088 | None | Aspirin 81 mg |
| G | Ischemic CVA | 4.8 | 77.0 | 73 | 73 | 50.6 | 19.0 | 2 | 535 | NA | NA | 608 | None | Clopidogrel 75 mg |
| Ha | Hemorrhagic, ischemic CVA | 9.8 | 78.3 | 86 | 87 | 87.3 | 42.8 | 0 | 528 | 2.8 | 12.3 | 787 | None | Aspirin 81 mg/clopidogrel 75 mg |
| Bleeding complications | ||||||||||||||
| Ia | Gl bleed, death | 9.2 | 63.0 | 62 | 49 | 46.8 | 33.8 | 0 | 43 | > 30 | 11.1 | 1,054 | None | None |
| Ha | Hemorrhagic, ischemic CVA | 9.8 | 78.3 | 86 | 87 | 87.3 | 42.8 | 0 | 528 | 2.8 | 12.3 | 787 | None | Aspirin 81 mg/clopidogrel 75 mg |
| Death | ||||||||||||||
| Ia | GI bleed, death | 9.2 | 63.0 | 62 | 49 | 46.8 | 33.8 | 0 | 43 | > 30 | 11.1 | 1,054 | None | None |
| J | Death | 12.6 | 53.4 | 52 | 10 | 47.2 | 7.0 | 0 | 162 | 4.76 | < 0.29 | 608 | Enoxaparin 100 BID | None |
| K | Death | 40.5 | 4.2 | 10 | 35 | 43.3 | 10.0 | 0 | 93 | > 30 | 20.6 | 752 | Enoxaparin 30 QD | None |
| L | Death | 21.6 | 17.3 | 39 | 31 | 28.0 | 27.3 | 0 | 128 | 4.85 | 9.49 | 826 | Enoxaparin 40 BID | Aspirin 81 mg |
| M | Death | 5.8 | 78.3 | 82 | 43.1 | 48.0 | 40 | 19 | 469 | 21.6 | 8.7 | 1,728 | Enoxaparin 90 BID | Aspirin 81 mg |
| N | Death | 3.7 | 77.2 | 76 | 53 | 71.1 | 25 | 0 | 273 | 4.1 | 5.9 | 2,078 | Heparin 5,000 BID | None |
| O | Death | 4.1 | 76.2 | 72 | 56 | 71.7 | 31 | 0 | 48 | 4 | 9 | NA | Enoxaparin 30 BID | None |
| P | Death | > 50 | NA | NA | NA | NA | NA | 100 | 489 | 1.97 | 6.32 | 700.5 | Enoxaparin 70 BID | Aspirin 81 mg |
| R | Death | 10.5 | 48.6 | 60 | 51 | 46.7 | 27 | 0 | 61 | 0.76 | 9.17 | 1,173 | Enoxaparin 100 BID | Clopidogrel 75 mg |
| Q | Death | 17.9 | 61.3 | 50 | 11.0 | 11.8 | 11 | 43 | 111 | 8.8 | 3.8 | 16,500 | Enoxaparin 60 QD | Aspirin 81 mg |
BID = twice daily, CVA = cerebrovascular accident, GI = gastrointestinal, MA = maximum amplitude, mg = miligrams, NA = not available, PE = pulmonary embolus, QD = once daily.
aPatients H and I are listed in two categories.
Bleeding complications were related to problems with clot initiation (reaction time [R] > 8 min), often in the setting of full antifactor anticoagulation. When prolonged R was combined with severe platelet hyperactivity (MA-AA/ADP > 80 mm), both ischemic and hemorrhagic complications cooccurred (Table 3, Patient F). However, a minimal increase in platelet function (MA-AA/ADP 50–60 mm) could also be balanced through decreased factor activity (R > 7), preventing complications.
For nonsurvivors, irreversible thrombocytopenia (< 100,000/µL) was an unmistakable sign of deterioration/death (Table 3, Patients I, K, R). When TEG variables were outside of their physiologic norm, death was more likely to occur (R > 10 min; percentage of lysis at 30 min [LY30] > 10%). Prolonged R (Table 3, Patients J, K, L, P, R, Q) or high LY30 (Table 3, Patients M, P, Q) denoted those with severe “hypocoagulability”. Conversely, uncorrected “hypercoagulability” of Patient N with persistently overactive platelets (MA-AA > 70 mm and ADP > 50 mm), early clot initiation (R < 4.5 min), and high activator F was also associated with patient demise.
Thromboelastography-Guided Anticoagulation
Among the 72 patients, who received TEG-guided anticoagulation (antifactor or antiplatelet) management, TEG-PM was typically repeated every 48–72 hours (90% of the time). Correction of TEG variables to R ~6 min and MA-AA/ADP less than 40–55 mm was associated with greatly improved survival, decreased rates of ICU admission, MV, and AKI (Table 2). In addition to proper characterization of coagulopathy, TEG-PM frequently identified antiplatelet nonresponders, requiring dose increase or substitution of medications. Overall, use of TEG-guided antiplatelet medications decreased mortality by 82% (p = 0.0002).
Patients in the non-AG treatment group were more likely to have received full dose antifactor/anticoagulation with heparin or enoxaparin (Table 2). A total of 45 patients (both groups) received full (antifactor) anticoagulation; AG-TEG group followed TEG protocols for escalation and de-escalation of antifactor anticoagulation. Of the nonsurvivors, 12 (42.9%) were in the non-AG treatment group and three (4.2%) in the AG-TEG group, p < 0.0001. Accordingly, the non-AG use of antifactor treatment, without adjustments based on R, was associated with 10.3 times increased risk of mortality (p = 0.0001).
A total of 10 patients with representative TEG-PM, before and after TEG-guided anticoagulation adjustment of anticoagulation medications are listed in Table 4. Increase in antifactor medications allowed for R prolongation in most cases, whereas antiplatelet medications decreased platelet activity (MA-AA/ADP). Of note, patients were often found to have inadequate platelet suppression with aspirin 81 mg alone. If incremental increase in aspirin dosage (162 or 325 mg) failed to show decreases in MA-AA or if MA-ADP remained extremely high (> 70 mm), clopidogrel or ticagrelor was added to the regimen.
TABLE 4.
Algorithm-Guided Treatment Using Antifactor (Heparin, Enoxaparin) and Antiplatelet (Aspirin, Clopidogrel) Medications; Comparison of 10 Before/After Thromboelastography With Platelet Mapping
| Anticoagulation Medications | Thromboelastography With Platelet Mapping Variables | Inflammatory Markers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Antifactor | Antiplatelet | Treatment | Reaction Time | Alpha Angle | MA | MA-Adenosine Diphosphate | MA-Arachidonic Acid | Lysis at 30 Min | Activator F | d-dimer | C-Reactive Protein | Ferritin |
| 1 | Heparin 5,000 BID | None | Initial | 5.0 | 73.8 | 70 | 68 | 70.3 | 0 | 18 | 0.96 | 2.1 | 986 |
| Heparin 5,000 BID | Aspirin 81 mg | Based on TEG | 7.0 | 68.3 | 69 | 67 | 32.5 | 0 | 20 | 1.1 | 3.5 | 1,516 | |
| 2 | None | None | Initial | 3.8 | 80.2 | 79 | 66 | 62.9 | 1 | 19.8 | 2.1 | 12 | 816 |
| Heparin 5,000 BID | Aspirin 81 mg | Based on TEG | 4.2 | 78.1 | 72 | 74 | 31.4 | 3 | 25.1 | 1.7 | 3.1 | 524 | |
| 3 | None | None | Initial | 3.2 | 79.2 | 79 | 75 | 81.4 | 0 | 28 | 1.5 | 17 | 1,089 |
| Heparin 5,000 BID | Aspirin 325 mg | Based on TEG | 4.2 | 77.1 | 77 | 76 | 42.9 | 0 | 28 | 4.3 | 1.3 | 1,256 | |
| 4 | Enoxaparin 40 QD | Aspirin 325 mg | Initial | 5.9 | 76.1 | 80 | 83 | 84.3 | 1 | 26.9 | 1.1 | 2.5 | 990 |
| Enoxaparin 40 BID | Aspirin 81 mg, clopidogrel 75 mg | Based on TEG | 7.1 | 69.7 | 78 | 77 | 62.9 | 0 | 26 | Not available | 1.1 | 829 | |
| 5 | None | None | Initial | 4.6 | 75.3 | 77 | 86 | 78.5 | 0 | 33 | 4.7 | 11 | 1,639 |
| Enoxaparin 100 BID | Aspirin 81 mg | Based on TEG | 7.2 | 66 | 72 | 55 | 57.1 | 0 | 19 | 4.2 | 6.8 | 1,080 | |
| 6 | Heparin 5,000 TID | None | Initial | 7.8 | 78.3 | 86 | 87 | 87.3 | 0 | 43 | 2.8 | 12.3 | 787 |
| Heparin 5,000 TID | Aspirin 81 mg, clopidogrel 75 mg | Based on TEG | 3.8 | 80.4 | 83 | 40 | 58.1 | 0 | 34 | 1.2 | 3.1 | 284 | |
| 7 | Enoxaparin 40 QD | Clopidogrel 75 mg | Initial | 4.7 | 79 | 81 | 76 | 82.9 | 0 | 35 | 1.5 | 15.8 | 206 |
| Enoxaparin 40 QD | Aspirin 81 mg | Based on TEG | 3.3 | 78.9 | 81 | 77 | 40 | 0 | 31 | 3.5 | 4.46 | 150 | |
| 8 | Enoxaparin 40 QD | None | Initial | 4.3 | 74.9 | 69 | 78 | 68.4 | 2 | 16 | 1.89 | 0.29 | 124 |
| Enoxaparin 30 BID | Aspirin 81 mg | Based on TEG | 4.7 | 73.5 | 69 | 68 | 49.3 | 3 | 15 | 1.09 | 0.19 | 91 | |
| 9 | Enoxaparin 100 BID | None | Initial | 5.1 | 74.5 | 71 | 72 | 76.5 | 1 | 19 | 9.3 | 4.2 | 490 |
| Enoxaparin 80 BID | Aspirin 81 mg | Based on TEG | 4.8 | 75.4 | 59 | 38 | 35 | 0 | 17 | 2.96 | 2.3 | 274 | |
| 10 | Enoxaparin 40 QD | None | Initial | 3.7 | 77.2 | 76 | 53 | 71.1 | 0 | 25 | 4.05 | 5.9 | 2,079 |
| Enoxaparin 100 BID | Aspirin 81 mg, clopidogrel 75 mg | Based on TEG | 4.5 | 71.6 | 68 | 34 | 24.7 | 0 | 12 | 11.5 | 3.5 | 2,041 | |
BID = twice daily, MA = maximum amplitude, QD = once daily, R = reaction time, TEG = thromboelastography, TID = three times daily.
DISCUSSION
In this study, TEG-PM is introduced as a more tailored, patient-specific approach to diagnosing COVID-19 coagulation abnormalities. TEG-PM better characterizes and emphasizes the spectrum of coagulopathic disorders and may indeed guide more appropriate, individualized therapies in patients infected with COVID-19.
The experience and results of this study have already led to an ever-increasing number of clinicians at the study’s institution to fully adopt the use of TEG-PM as a way to: 1) better characterize the specific coagulopathy found in any given COVID-19 patient, 2) more accurately delineate the underrecognized platelet contribution to any coagulopathy, and 3) better guide patient-specific anticoagulation management with the hope of improving patient outcomes.
It has been postulated that most signs and symptoms associated with COVID-19 are secondary to a coagulopathy (2, 27). Infected patients of all ages can present with arterial and venous thromboses (DVT and pulmonary emboli) and/or microthrombi causing PF and AKI, myocardial infarctions, ischemic and hemorrhagic strokes, or DIC and death (2, 5, 6, 27, 28). Coagulopathy is reported to carry an 11.5% mortality rate (9). The current study showed a significantly increased risk for MV and AKI in patients whose coagulopathy (as diagnosed by TEG-PM) did not resolve (Table 2) as well as a 7.7-fold increased risk of death (p = 0.0001).
With presenting symptoms and signs being highly variable and complications ranging from thrombotic to hemorrhagic, the diagnosis of coagulopathy remains difficult, yet of paramount importance. Based on our findings and those of others, a “hypercoagulable” state does not define the entire coagulopathic spectrum of COVID-19 (3, 7). Patient H (Table 3) presented with ischemic and hemorrhagic complications and was found to have prolonged R on TEG-PM in a setting of platelet hyperactivity. Overall, hemorrhagic complications were associated with factor inactivity and inability to initiate clot formation (R > 8 min), whereas ischemic complications occurred with platelet hyperactivity (MA-AA/ADP > 50 mm). Others proceeded to DIC and death with extremes of TEG variables (R > 10 min or LY30 > 10%), including primary fibrinolysis, previously noted to carry a 70–100% mortality rate in critically injured patients (29).
Although inflammatory markers and CCTs have been associated with higher risk of coagulopathy in COVID-19 patients, they did not differentiate between coagulopathic and noncoagulopathic patients (9). Counterintuitively, prior studies have reported a 31% frequency of thrombosis in ICU patients when PT/PTT values were elevated (hazard ratio = 4.1) (2). Higher levels of CRP, d-dimer, FDPs, and prolonged PT/PTT were also found in COVID-19 nonsurvivors and among those with worsening respiratory failure, likely reflecting systemic inflammatory response (9, 11, 18). The current study did confirm that higher levels of d-dimer, CRP, and ferritin were associated with increased rates of PF, AKI, and mortality, but also demonstrated no change in PT/PTT/INR variables until demise was imminent (data not shown). In several studies, diagnosis of coagulopathy was only based on CCTs, anti-Xa, and inflammatory markers, rather than TEG (30–32). In this study, most patients received some form of antifactor prophylaxis at admission. However, use of prophylactic and/or therapeutic non-AG antifactor medications as compared to those guided by TEG-PM was associated with a 10.3-fold increased risk of mortality (p = 0.0001). One consideration is that coagulopathy of COVID-19 may include “hypocoagulability”, further exacerbated through administration of anticoagulants. Therefore, TEG guidance regarding antifactor medication administration may identify patients at risk for bleeding and further bridge the gap between survivors and non-survivors.
A small number of studies have reported the use of TEG to identify hypercoagulability in COVID-19 patients, but the specific TEG-PM approach to manage platelets has not been described, despite the known complexities of platelet dysfunction as further demonstrated in this study (12, 22, 27, 33–36). Considering that platelets become hyperactive and have the ability to aggregate faster in COVID-19, TEG-PM appears to be a useful test to more optimally identify and characterize platelet dysfunction and, in turn, guide treatment (14, 36–40). In this study, corrected coagulopathy, largely platelet-related, was associated with what appeared to be markedly improved outcomes, including enhanced likelihood of survival.
Given the sheer volume of patients being diagnosed with COVID-19, it might not be feasible to perform TEG-PM testing in every confirmed COVID-19 patient. But based on these preliminary findings, high-risk patients with respiratory decline or other early organ failure should advisedly receive TEG-PM evaluation and, by all indications, the earlier the better. While use of TEG-PM emphasizes the tailoring of an individualized approach to care, management can be standardized to a large degree through pre-existing algorithms. Based on the preliminary results in this study, TEG-guided treatment appeared to make a significant difference compared with the cases in which TEG variables were not followed (40).
The main limitation of this study is that it remains observational in nature, rather than a randomized controlled trial testing TEG-guided management. Patients were followed prospectively in order to reliably capture all the data and document the clinical decisions regarding TEG-guided medication adjustments. However, the treating clinicians, regardless of their use of the TEG-PM algorithm and/or TTF support, were ultimately responsible for choosing patient’s anticoagulation management. Additionally, during the COVID-19 surge, the overwhelming demand for coagulopathy assessment using TEG-PM required the recruitment and training of multiple TTF teams. Only one team was involved with data-gathering, which may have led to an inadequate or biased sample size, although patients were randomly distributed among the TTF members. Also, although unrecognized confounding variables may have had an impact in this unadjusted exploratory analysis, the non-AG and AG-TEG groups overall appeared to be well-matched based on their demographics and admission criteria as seen in Table 1.
Another study limitation is that our patients were derived from one specific geographical and demographic setting, which is not large enough to represent the overall population of COVID-19 patients nor the many nuances of COVID-19 disease. Consequently, there is a potential selection bias that may limit the applicability of this study more broadly. Nevertheless, the hyper- and hypocoagulable algorithms created by the institutional TTF are of great value as a template and therefore should undergo external validation and additional testing with further evaluation in controlled trials.
CONCLUSIONS
As confirmed by this study, COVID-19 coagulopathy has a multifaceted, chameleon spectrum of coagulopathy with platelet aberrations often playing a large role. Therefore, we recommended that patient-tailored diagnosis/characterization and treatment of COVID-19 coagulopathy should be based on a standardized algorithm employing TEG-PM. Although yet to be confirmed in other settings, the results here suggest that TEG-PM may be a mechanism to improve outcomes for COVID-19 patients, and, most importantly, it may reduce the risk of potential iatrogenic complications through indiscriminate use of anticoagulation medications. Most optimally, anticoagulant treatment should be tailored according to TEG-PM as some coagulopathic patients with COVID-19 are actually “hypocoagulable”, indicating a risk for bleeding, whereas many others have a significant platelet activity dysfunction that creates the “hypercoagulable” state. Some patients do not respond to first-line medications, and therefore, on-going TEG-PM assays and protocols are also indicated to guide the next steps in treatment (40).
ACKNOWLEDGMENTS
The Memorial Health System team expresses its deepest appreciation to the women and men in our healthcare system who continue to take on the inherent and ever-fatiguing risk of serving on the front lines of the severe COVID-19 pandemic in one the world’s busiest epicenters. All of us will be forever indebted to those team members for saving lives and for aiding and providing comfort to those afflicted. The team also sends its deepest sense of compassion and sympathy for those who have lost their loved ones to this deadly virus and hope that our contributions here will benefit future victims of the illness.
Footnotes
The authors have disclosed that they do not have any potential conflicts of interest.
This study was performed at Memorial Regional Hospital.
REFERENCES
- 1.Mortus JR, Manek SE, Brubaker LS, et al. Thromboelastographic results and hypercoagulability syndrome in patients with coronavirus disease 2019 who are critically ill. JAMA Netw Open. 2020; 3:e2011192–e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok F, Kruip M, Van der Meer N, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191:145–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharifi-Razavi A, Karimi N, Rouhani N: COVID-19 and intracerebral haemorrhage: Causative or coincidental? New Microbes New Infect. 2020; 35:100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wichmann D, Sperhake J-P, Lütgehetmann M, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: A prospective cohort study. Ann Int Med. 2020; 173:268–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020; 383:120–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Su H, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020; 98:219–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poyiadji N, Shahin G, Noujaim D, et al. COVID-19–associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020; 296: E119–E120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kitchens CS. Thrombocytopenia and Thrombosis in Disseminated Intravascular Coagulation (DIC). ASH Education Program Book. 2009; 2009(1):240–246. Available at: 10.1182/asheducation-2009.1.240. Accessed October 4, 2020 [DOI] [PubMed] [Google Scholar]
- 9.Tang N, Li D, Wang X, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020; 18:844–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180:934–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ling W: C-reactive protein levels in the early stage of COVID-19. Med Mal Infect. 2020; 50:332–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kay AB, Morris DS, Collingridge DS, et al. Platelet dysfunction on thromboelastogram is associated with severity of blunt traumatic brain injury. Am J Surg. 2019; 218:1134–1137 [DOI] [PubMed] [Google Scholar]
- 13.Wang Z, Li J, Cao Q, et al. Comparison between thromboelastography and conventional coagulation tests in surgical patients with localized prostate cancer. Clin Appl Thromb Hemost. 2018; 24:755–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manne BK, Denorme F, Middleton EA, et al. Platelet gene expression and function in COVID-19 patients. Blood. 2020; 136:1317–1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maatman TK, Jalali F, Feizpour C, et al. Routine venous thromboembolism prophylaxis may be inadequate in the hypercoagulable state of severe coronavirus disease 2019. Crit Care Med. 2020; 48:e783–e790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tapia NM, Chang A, Norman M, et al. TEG-guided resuscitation is superior to standardized MTP resuscitation in massively transfused penetrating trauma patients. J Trauma Acute Care Surg. 2013; 74:378–385 [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez E, Moore EE, Moore HB, et al. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: A pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg. 2016; 263:1051–1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020; 18:1738–1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chau T, Chan Y, Patch D, et al. Thrombelastographic changes and early rebleeding in cirrhotic patients with variceal bleeding. Gut. 1998; 43:267–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Pietri L, Bianchini M, Montalti R, et al. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: A randomized, controlled trial. Hepatology. 2016; 63:566–573 [DOI] [PubMed] [Google Scholar]
- 21.Wright FL, Vogler TO, Moore EE, et al. Fibrinolysis shutdown correlates to thromboembolic events in severe COVID-19 infection. J Am Coll of Surg. 2020; 231:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helms J, Tacquard C, Severac F, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: A multicenter prospective cohort study. Intensive Care Med. 2020; 46:1089–1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liang C, Yang Y, He Z, et al. Comparison between thromboelastography and the conventional coagulation test in detecting effects of antiplatelet agents after endovascular treatments in acute ischemic stroke patients: A STROBE-compliant study. Medicine. 2020; 99:e19447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Quellec S, Bordet J-C, Negrier C, et al. Comparison of current platelet functional tests for the assessment of aspirin and clopidogrel response. Thromb Haemost. 2016; 116:638–650 [DOI] [PubMed] [Google Scholar]
- 25.Chitlur M, Sorensen B, Rivard G, et al. Standardization of thromboelastography: A report from the TEG-ROTEM working group. Haemophilia. 2011; 17:532–537 [DOI] [PubMed] [Google Scholar]
- 26.Bolliger D, Seeberger MD, Tanaka KA. Principles and practice of thromboelastography in clinical coagulation management and transfusion practice. Transfus Med Rev. 2012; 26:1–13 [DOI] [PubMed] [Google Scholar]
- 27.Hartmann J, Murphy M, Dias JD. Viscoelastic hemostatic assays: moving from the laboratory to the site of care—a review of established and emerging technologies. Diagnostics. 2020; 10:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sakamoto Y, Koami H, Miike T: Monitoring the coagulation status of trauma patients with viscoelastic devices. J Intensive Care. 2017; 5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barker EE, Saini A, Gazit AZ, et al. TEG Platelet mapping and impedance aggregometry to predict platelet transfusion during cardiopulmonary bypass in pediatric patients. Front Pediatr. 2019; 7:509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agarwal S, Johnson RI, Kirmani BH. Pre-and post-bypass platelet function testing with multiple electrode aggregometry and TEG platelet mapping in cardiac surgery. J Cardiothorac Vasc Anesth. 2015; 29:1272–1276 [DOI] [PubMed] [Google Scholar]
- 31.Yuriditsky E, Horowitz JM, Merchan C, et al. Thromboelastography profiles of critically ill patients with coronavirus disease 2019. Crit Care Med. 2020; 48:1319–1326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dewitte A, Lepreux S, Villeneuve J, et al. Blood platelets and sepsis pathophysiology: A new therapeutic prospect in critical ill patients? Ann Intensive Care. 2017; 7:115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu X, Li Z, Liu S, et al. Potential therapeutic effects of dipyridamole in the severely ill patients with COVID-19. Acta Pharm Sin B. 2020; 10:1205–1215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Viecca M, Radovanovic D, Forleo GB, et al. Enhanced platelet inhibition treatment improves hypoxemia in patients with severe Covid-19 and hypercoagulability. A case control, proof of concept study. Pharmacol Res. 2020; 158:104950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Song J-C, Wang G, Zhang W, et al. Chinese expert consensus on diagnosis and treatment of coagulation dysfunction in COVID-19. Mil Med Res. 2020; 7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oxley TJ, Mocco J, Majidi S, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020; 382:e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Napolitano LM, Cohen MJ, Cotton BA, et al. Tranexamic acid in trauma: How should we use it? J Trauma Acute Care Surg. 2013; 74:1575–1586 [DOI] [PubMed] [Google Scholar]
- 38.Stattin K, Lipcsey M, Andersson H, et al. Inadequate prophylactic effect of low-molecular weight heparin in critically ill COVID-19 patients. J Crit Care. 2020; 60:249–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flaczyk A, Rosovsky RP, Reed CT, et al. Comparison of published guidelines for management of coagulopathy and thrombosis in critically ill patients with COVID 19: Implications for clinical practice and future investigations. Crit Care. 2020; 24:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nadkarni GN, Lala A, Bagiella E, et al. Anticoagulation, mortality, bleeding and pathology among patients hospitalized with COVID-19: A single health system study. J Am Coll Cardiol. 2020; 76:1815–1826 [DOI] [PMC free article] [PubMed] [Google Scholar]


