Abstract
COVID-19 pandemic caused a major crisis, affecting and straining health care systems, including some very advanced ones. The pandemic may have also indirectly affected access to health care for patients with other conditions, not related to COVID-19, even in countries not overwhelmed by an outbreak.
We analyzed and compared visits to the emergency room (ER) department during the same calendar period of 2019 and 2020 (from March 1 to March 31 of each year) in our hospital, a medium size, tertiary center, located in the center of Athens, which is not a referral center for COVID-19.
Total ER visits were reduced by 42.3% and the number of those requiring hospitalization by 34.8%. This reduction was driven by lower numbers of visits for low risk, non-specific symptoms and causes. However, there was a significant decrease in admissions for cardiovascular symptoms and complications (chest pain of cardiac origin, acute coronary syndromes, and stroke) by 39.7% and for suspected or confirmed GI hemorrhage by 54.7%. Importantly, number of ER visits for infections remained unchanged, as well as the number of patients that required hospitalization for infection management; only few patients were diagnosed with COVID-19.
During the initial period of the pandemic and lock-down in Greece, there was a major decrease in the patients visiting ER department, including decrease in the numbers of admissions for cardiovascular symptoms and complications. These observations may have implications for the management of non-COVID-19 diseases during the pandemic.
Keywords: acute coronary syndrome, COVID-19, emergency room, resuscitation
What is already known in this subject
During COVD-19 pandemic, overwhelmed health care systems were not able to manage with non-COVID-19 related admissions.
Lock-down measures may have affected patients’ access to health care.
A general observation for a reduction in ER visits during lock-down has been made, but has not been quantified and or assessed in detail, outside regions with heavy outbreaks.
What this study adds
Quantitative and qualitative changes in ER visits have been recorded during lock-down compared to the same calendar period in 2019.
A major reduction in ER visits occurred.
Major reductions in admission for acute coronary syndromes, GI hemorrhage, stroke have been observed compared to the same calendar period in 2019.
In an area not heavily affected by the outbreak, this change could not be explained by an overwhelmed health care system.
Lock-down may have indirectly affected non-COVID-19 patients, potentially increasing risks of adverse outcomes in many diseases.
1. Introduction
Since January 2020, a pandemic due to SARS-CoV-2 virus, causing COVID-19,[1] has affected almost every country in the globe and resulted in a major health crisis. This pandemic has affected the health care systems of several countries, including some with very advanced health care systems. Since COVID-19 became the major focus to allocate health care resources, it was realized that other patients may have also been affected negatively, in an indirect pathway. There has been a widespread perception that visits to emergency room (ER) departments have been reportedly decreased for causes other than suspected COVID-19 and this has been discussed extensively in the news and social media, but without hard data to support further evaluation of this phenomenon. Indeed, there are very few precise reports of the decrease in ER visits and of the qualitative characteristics of those reaching finally to ER. Some reports from Northern Italy indicate a reduction of the number of admissions for acute coronary syndromes (ACS), when compared to a previous period.[2] However, Northern Italy was probably one the most affected areas by COVID-19 in the world. In other countries, including Greece, COVID-19 pandemic was less severe, in terms of cases and associated deaths, but there were still major “lock-down” measures in place, which may have affected the pathway to health care services. In Austria, a country similar in population size with Greece but with a more advanced health care system, which also contained the outbreak, a reduction of admissions for acute coronary syndromes was also observed.[3] However, as of today, there is very little data on the real effect in terms of ER visits and the characteristics of those who reached to an ER department during the pandemic, beyond some data for patients with ACS.[2,3] In order to describe in more detail changes in the volume and type of visits during the COVID-19 pandemic, we compared the ER visits during the same calendar period of 2019 and 2020 in the ER department of our hospital, a medium size, tertiary center, located in the center of Athens which is not a referral center for COVID-19 patients.
2. Methods
We analyzed the records of the visits in the ER department of “Alexandra” hospital. This is a public tertiary hospital, with academic Internal Medicine departments but has no surgical ER department; cases requiring emergency surgical evaluation are assessed in a neighboring hospital. Thus, we assessed only visits in ER department concerning non-surgical causes.
We analyzed the records of the visits in the ER department of the hospital and extracted data regarding age, gender, primary cause for the visit to ER and whether hospitalization was required for further management. We compared the records of ER visits during the same time period of 2019 and of 2020 (from March 1 to March 31). The first measures of social distancing in Greece started at the end of February, with cancellation of mass gatherings (such as the carnival festivities) and then a more generalized “lock-down” followed on March 10th with the closures of schools. However, the first case of COVID-19 in Greece occurred at the end of February 2020 (26 February 2020) and was associated with a visit to Northern Italy; news of the pandemic from Italy were already spreading and had caused concern. We present descriptive data for the 2 calendar periods. For comparisons between different eras for the distribution of diagnoses we used chi-square test in SPPS 24.
3. Results
During the period between March 1 and 31 of 2020, total visits in the ER Department of the hospital were reduced by 42.3% compared to the same calendar period in 2019 (i.e., from 1133 in the previous year to 653 in the same calendar period in 2020) (see Table 1 and Fig. 1). From those who visited ER, 33.2% required further hospitalization, while in the same period in 2019, 29.3% of those who visited the ER were admitted to hospital (P = .09 for rate of hospitalization); however, the number of those that were hospitalized was reduced by 34.8% (217 vs 333 during the 2 calendar periods). The number of patients who required immediate admission to ICU was not significantly different between the 2 periods (25 vs 31, 3.8% and 2.7% of the total visits and 11.5% vs 9.3% of the total in-hospital admissions); 7 patients were dead on arrival to ER in 2020 vs 9 in 2019.
Table 1.
Numbers and distribution of ER visits between 2019 and 2020 and relevant changes.
| 2020n (% of visits in the time period) | 2019n (% of visits in the time period) | Absolute reduction (percent) | |
| Total visits | 653 | 1133 | −42.3% |
| Visits requiring further hospitalization | 217 | 333 | −34.8% |
| Infections (all sites) | 202 (30.9%) | 208 (18.4%) | −2.8% |
| Upper respiratory tract infections | 93 (14.2%) | 77 (6.8%) | +20.7% |
| Lower respiratory tract infection | 33 (5%) | 25 (2.2%) | +32% |
| Other site or non-specified site of infection | 76 (11.6%) | 106 (9.3%) | −28.3% |
| Non-specific GI complaints (nausea, vomiting, abdominal pain) | 102 (15.6%) | 248 (21.9%) | −58.8% |
| Non-specific general complaints (fatigues, back or other non-specific pain, etc) | 24 (3.7%) | 80 (7.1%) | −70% |
| Cancer complication management | 34 (5.2%) | 58 (5.1%) | −41.4% |
| Symptoms of cardiac origin (angina, non-specific chest pain) | 59 (9%) | 93 (8.2%) | −36.6% |
| Acute coronary syndrome | 14 (2.1%) | 20 (1.7%) | −30% |
| Stroke | 6 (0.9%) | 18 (1.5%) | −67% |
| Cardiovascular disease∗ (all pooled) | 79 (12.1% | 131 (11.6%) | −39.7% |
| Arrhythmia/palpitations | 37 (5.6%) | 48 (4.2%) | −23% |
| Heart failure/decompensation | 24 (3.7%) | 35 (3.1%) | −31.4% |
| Syncope/pre-syncope | 13 (2%) | 21 (1.9%) | −38% |
| Uncontrolled hypertension/hypertensive spike | 14 (2.1%) | 40 (3.5%) | −65% |
| GI bleeding (suspected or confirmed) | 24 (3.7%) | 53 (4.7%) | −54.7% |
| “Colitis” of any cause | 1 (0.15%) | 6 (0.5%) | −83% |
Figure 1.
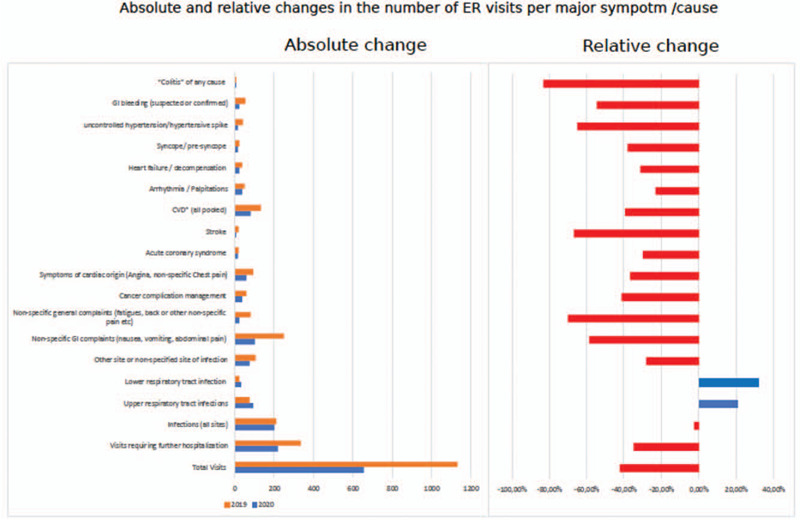
Absolute number of visits and relative change per major/symptom cause in the 2 periods under comparison (1–31st March of 2020 vs same period of 2019).
We further evaluated the characteristics of the individuals who visited ER, such as age, gender, and primary cause for visit (such as symptom/complaint) for visit. We found no significant difference in the gender and age distribution between the 2 calendar periods: the median age of the individuals who visited the ER was 55 in the recent vs 53 years of age in the previous calendar period (P = .328) and the median age of those who were further admitted for hospitalization was 70 vs 72 years (P = .867). There was also no major difference in the distribution of age of those who visited ER: in the recent period, 28.8% vs 31.5% were below 40 years of age, 36.5% vs 31.3% were between 40 and 65 years and 34.7% vs 37% were above the age of 65 years (P = .106). However, among those above the age of 65 who visited the ER, 61.8% required further hospitalization in the 2020 period vs 48.9% in the 2019 period (P = .003); this was not observed in the other age groups.
We then evaluated the major sub-specialty that was involved in the management of the individuals in the ER: visits which required primarily cardiology assessment were reduced by 36.1% (168 in the recent vs 263 in the previous calendar period), those requiring primarily a GI specialist evaluation were reduced by 57% (26 vs 61) while there was a reduction of 43% (459 vs 809) of cases that were evaluated primarily by an Internal Medicine specialist (infections, stroke, non-specific constitutional symptoms, management of cancer complications, etc) (Fig. 1).
In absolute numbers, infections of any site remained similar between the 2 periods (202 vs 208 visits for infection). However, there was a significantly higher proportion of total ER visits in 2020 (30.9% of visits vs 18.4%, P < .001). More specifically, upper respiratory tract infections and related complaints were increased as a reason to visit ER both relatively and in absolute numbers (from 77 to 93 total visits, representing an increase from 6.8% to 14.2% of the ER visits, P < .001); similarly, lower respiratory tract infection and related complaints increased (from 25 to 33 visits, representing an increase from 2.2% to 5.5% of the ER visits, P = .001). ER visits for other types of infections or fever of non-specified primary site decreased from 106 to 76 cases, being 9.3% vs 11.6% of total visits (P = .032) (Fig. 1). Regarding the severity of these infections, 21.7% vs 15.6% required hospitalization (47 vs 52 cases) in the 2020 and 2019 periods, respectively (P = .071). There were no further hospital admissions required for those who visited ER for upper respiratory tract infections and related complaints in the 2020 period (0/93) vs only in 2/77 in the previous year, but more patients with lower respiratory tract infection were admitted in-hospital (24/33 vs 16/25, 72.7% vs 64.8% of visits for this cause). Of patients who presented with fever or respiratory symptoms, 10 were diagnosed with COVID-19 in 2020 (6 with fever and no specific symptoms, 1 with upper respiratory, and 1 with lower respiratory tract symptoms) – all were admitted to referral centers or sent to home isolation, according to the national guidelines at that moment.
Visits for non-specific GI complaints (nausea, vomiting, diarrhea, non-specific abdominal pain, etc) were reduced by 58.8% (102 vs 248 visits, constituting 15.6% vs 21.9% of total visits, P = .001). Further hospitalization was required for 15 vs 23 patients (14.7% and 9.2%, respectively). Other causes with non-specific symptoms (fatigue, non-specific back, or other musculoskeletal pains, etc) were reduced by 70% (24 vs 80 visits, being 3.7% vs 7.1% of total visits in each period respectively, P = .003) and only 3 (12.5%) vs 14 (17.5%) of those required hospitalization.
A population of special concern is cancer patients; visits of cancer patients for management of complications related with their disease or their therapy or terminal care were less in the recent era vs in 2019 (34 vs 58, a 41% reduction) but remained similar as proportion of total visits (5.2% vs 5.1%); a similar proportion that visited ER was hospitalized (27/34 (79.4%) vs 42/58 (72.4%)).
Cardiovascular disease is a major cause of morbidity and mortality; however, during the 2020 period there was a reduction of visits for major cardiovascular events (angina, AMI, stroke) by 39.7% (from 131 to 79 visits, being 11.6% and 12.1% of the ER visits, respectively). More specifically, visits for chest pain of suspected cardiac origin (“angina,” “dyspnea with chest pain,” etc) reduced by 36.5% (there were 59 vs 93 visits, 9% and 8.2% of the visits, respectively) and there was a reduction in the number of acute coronary syndrome (by 30%, from 20 to 14); the number of primary PTCA performed was reduced to 12 from 25 in 2019 (absolute reduction 52%). Admissions for stroke constituted 0.9% and 1% of the visits; however, the absolute number of patients with stroke was reduced by 67% (from 18 in 2019 to 6 admissions in 2020). Other visits requiring a cardiologist consultation, such as for arrhythmia and palpitations (almost in all cases AF) (37 vs 48 admissions, 5.6% and 4.2% of visits, respectively) were reduced by 23%. There was a reduction in the visits due to “heart failure” by 31.4% (24 vs 35, 3.7% and 3.1% of visits, respectively) and further hospitalization was required in 20/24 (83.3%) vs 17/35 (48.6%) (P = .007) patients. Syncope/pre-syncope was also reduced as presenting symptom by 38% (13 vs 21, being 2% and 1.9% of the visits) and 5/13 (38.5%) vs 10/21 (47.6%) (P = .601) were hospitalized. We observed a significant reduction in the visits for “uncontrolled hypertension/hypertensive spike” (by 65%, 14 vs 40, being 2.1% vs 3.5% of total ER visits).
Visits of GI bleeding (suspected or confirmed) were reduced by 54.7%, mostly visits for “melena/suspected upper GI bleeding/lower GI bleeding” (reduced by 59.5% to 19 vs 47 in the previous period, while ER visits for “hematemesis” were similar (5 vs 6 visits respectively); hospitalization was required for 14/19 (73.7%) vs 25/47 (53.2%) (P = .109) (Fig. 1).
4. Discussion
In the current report we observed a major reduction in the ER visits in our hospital during the period when measures of social distancing and country “lock-down” were introduced, from 1st to 31st of March 2020, when compared to the same period in 2019. More specifically, we found a major reduction of 42.3% of the ER visits and of 33.2% in the hospitalizations during these 2 calendar periods. It is important to note that COVID-19 was rather controlled and as of March 31st, 1314 confirmed cases with 49 deaths due to COVID-19 had been reported in Greece. It is important that the hospitals in Greece were not overwhelmed. It is also our experience that there were a lot of empty beds, in contrast to the usual situation during winter and spring, in Greek hospitals.
This reduction needs further analysis as to the qualitative characteristics, and thus we further attempted to scrutinize our data in order to understand this finding. We observed a reduction in ER visits both in cases presenting with probably less “severe,” non-specific symptoms (such as non-specific GI complaints and non-specific general complaints; in the range of a 58–70% reduction) but also in visits which were or could be associated with more “severe” and potentially life threatening conditions. Thus, there was a reduction of almost 40% in those coming to ER for cardiovascular complaints or complications (acute MI, stroke, unstable angina) and a reduction in the number of primary percutaneous angioplasty for ST elevation acute myocardial infarction performed in our hospital by 52%. In addition, a reduction of ∼55% in the admission for suspected GI hemorrhage was also observed. However, there has been no major change in any of the characteristics of the population or in any medical/pharmacological intervention to explain a reduction of this magnitude in cardiovascular disease or GI hemorrhages. Data from several cardiovascular centers in Northern Italy also indicated a significant reduction in the rates of acute coronary syndrome-related hospitalizations during the early days of the COVID-19 outbreak by 26% to 30%[2] but similar data are coming from Austria, which was less severely affected by the pandemic.[3] We believe that the combination of these data form Italy and Austria with our observations should alarm the physicians and the authorities. Avoiding immediate access to health care (as in ER) during an acute cardiovascular syndrome or a hemorrhage may be associated with increased morbidity, poor long-term outcomes, and increased mortality. Hence, in Northern Italy there was a 58% increase in the cases of out-of-hospital cardiac arrests[4] during the pandemic. In our opinion it is probably the fear of reaching to the hospital that probably explains, at least in a major part, our findings, given the fact that the hospitals in Greece (including ours) were not overwhelmed by COVID-19. However, the situation may be quite different in other countries which were hit harder by the outbreak, as shown in the Northern Italy.[2,4] In such areas, overwhelmed hospitals may lack the resources to manage the non-COVID-19 cases in full capacity, as in the pre-pandemic era.
Because there was an awareness of COVID-19 as a respiratory disease,[1,5] we evaluated visits for respiratory symptoms and respiratory infections. The numbers of those who came to ER due to respiratory infections were not different compared to the previous reference period. The severity of those respiratory infections was also rather unchanged, as depicted by the numbers of those who required further hospitalization. Notably, only 10 cases of COVID-19 were diagnosed (1.5% of those that visited ER). This further emphasizes our premise that the reduction in ER visits was not due to an overwhelmed system, flooded with cases of respiratory infections. It is also important that, during the 2 periods, we did not observe a major difference in those who required immediate admission to the ICU (none was COVID-19 related) and also in the number of out-of-hospital deaths admitted to the ER. In any case, we will need additional data to fill in the complete picture of the effects of the pandemic in the non-COVID-19 related morbidity and perhaps mortality, and how may have been affected indirectly by the pandemic.
Our study has certain limitations, as it includes data from a single tertiary academic hospital, which, however, is located in the center of Athens and is a referral center for several diseases in oncology/hematology, cardiology, GI medicine. Importantly, our hospital was not a referral center for COVID-19, so the bias introduced by patients admitted for confirmed or suspected COVID-19 may be significantly less. Also, during the 2 periods that we compared there has been no change in the function or the capacity of the hospital or its departments. Our observations may differ in other countries, with differences in health care systems, or in other cities with differences in size, locations, and number of hospitals, even in Greece. Thus, similar data need to be generated from more countries and hospitals. Our report offers a piece of the data that needs to be collected in order to understand the function of the health care systems, and the perception of the public for the health care system, the hospitals and the services that they can expect during the current pandemic. Combined with data from other countries, with different structure of their health care systems and including hospitals of different capacities may be helpful to design the response to the current and to a future return of the COVID-19 or other pandemic.
In conclusion, a major decrease in the ER visits during the initial and lock-down phase of the COVID-19 pandemic has been observed with a major decrease in admissions for cardiovascular symptoms and complications (cardiac origin chest pain, acute coronary syndromes, stroke) and suspected or confirmed GI hemorrhage. This decrease was not associated with an increase in visits for respiratory infections or COVID-19 cases, indicating that probably fear or other reasons may have discouraged patients to seek medical help, even for potentially severe diseases. These data should be viewed carefully, in combination with similar data which need to be generated from other countries and hospitals, to help the authorities design the next step in the management of the pandemic. These data emphasize the need for the adequate management of non-COVID-19 related diseases and their impact on population health, during the pandemic.
Author contributions
EK performed the analysis and wrote the first draft , KT, EA, KS, IK, CL, SC, SM, CP, EvK, EM, SK, IP, ET, AM collected data and criticality reviewed and revised the manuscript, MAD designed the study, reviewed and revised the manuscript.
Footnotes
Abbreviations: COVID-19 = corona virus disease 2019, GI = Gastrointenstinal.
How to cite this article: Kastritis E, Tsitsimpis K, Anninos E, Stamatelopoulos K, Kanakakis I, Lampropoulos C, Chatzidou S, Michopoulos S, Papamichail C, Kostis E, Manios E, Kontogiannis S, Paraskevaidis I, Terpos E, Mitrakou A, Dimopoulos MA. Significant reduction in the visits to the emergency room department during the COVID-19 pandemic in a tertiary hospital in Greece: Indirect victims of the pandemic?. Medicine. 2020;99:52(e23845).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med 2020;383:88–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Metzler B, Siostrzonek P, Binder RK, et al. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J 2020;41:1852–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Baldi E, Sechi GM, Mare C, et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med 2020;383:496–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]


