Abstract
Objective:
The DSM’s disruptive mood dysregulation disorder (DMDD), characterized by severe, chronic irritability, currently excludes children <6 years. However, capitalizing on a burgeoning developmental science base to differentiate clinically salient irritability in young children may enable earlier identification. Our objective was to advance an empirically-derived framework for early childhood DMDD (EC-DMDD) by (1) modeling and validating DMDD patterns in early childhood and (2) generating clinically informative, optimized behaviors with thresholds.
Method:
Data (N=425) were from three longitudinal assessments of the MAPS Study, spanning preschool (Ms=4.7 and 5.5 years) to early school age (M=6.8 years). The Multidimensional Assessment Profile of Disruptive Behavior (MAP-DB) Temper Loss scale captured irritability, and Family Life Impairment Scale (FLIS) assessed cross-domain impairment at the preschool timepoints and the K-SADS was used to assess clinical status at early school age. Latent transition analyses differentiated children with EC-DMDD from those with low, transient, or non-impairing irritability.
Results:
Developmental patterning of irritability proved important for normal:abnormal differentiation. 27% of children had initially high irritability, but only two-thirds of these were persistently highly irritable. Thus, “false positives” based on a single screen would be substantial. Yet, “false negatives” are low, as <1% with baseline low irritability demonstrated later high irritability. Based on the sequential preschool age time points, 6.7% of children were identified with EC-DMDD, characterized by persistent irritability with pervasive impairment, similar to prevalence at older ages. Specific behaviors included low frustration tolerance; dysregulated, developmentally unexpectable tantrums; and sustained irritable mood, which sensitively (.85–.96) and specifically (.80–.91) identified EC-DMDD. EC-DMDD predicted irritability-related syndromes (DMDD, ODD) at early school-age better than downward extension of DSM DMDD criteria to preschool age.
Conclusion:
These findings provide empirical thresholds for preschool-age clinical identification of DMDD patterns. The results lay the foundation for validation of DMDD in early childhood and inform revision of DSM criteria.
Keywords: disruptive mood dysregulation disorder, DSM, nosology, early childhood, irritability
Introduction
Irritability reflects a relative dispositional tendency to respond to frustration with temper tantrums/outbursts (i.e., phasic expressions) and/or to experience chronic/prolonged angry mood states (i.e., tonic irritability).1, 2 Disruptive mood dysregulation disorder (DMDD) in DSM-5 represents a major advance to encapsulate severe, impairing, chronic irritability in a single syndrome.3 DSM-5 includes more developmental considerations than its predecessors, yet due to a lack of a science base when the DMDD diagnosis was being developed, and in keeping with conventions that clinical differentiation in young children is more unreliable due to the prevalence of normative misbehavior during this period,4 children <6 years are excluded from DMDD. This age exclusion is of particular concern, given the widely recognized importance of neurodevelopmental characterization and prevention at the earliest phase of the clinical sequence,5 as well as the predictive utility of early irritability for lifespan mental disorder.2, 6–8 Moreover, early childhood tantrums are a prominent parental concern to health professionals9 and are associated with significant impairment.10
Recent advances in measurement science that enable psychometric, clinical, and neural differentiation of normal vs. abnormal patterns of irritability at preschool ages warrants reconsideration of excluding children <6 years from DMDD.2, 10–12 Our prior work has demonstrated that normative irritability is distinguishable from impairing, pathological irritability in early childhood when the irritability is frequent, dysregulated, and occurs in developmentally unexpectable contexts.2, 10, 13–18 Corollary neural abnormalities have also been demonstrated in young children.2, 19
Preliminary evidence supports the validity of DSM-5 DMDD criteria in early childhood when employing slightly higher thresholds than for older children using the PAPA.10, 20–22 While promising, those thresholds merely “downwardly extend” current symptom thresholds, rather than determining the optimal behaviors and thresholds for sensitive and specific characterization during this age period. In addition, current DSM-5 DMDD criteria for children emphasizes extreme mood and outbursts and very high frequency thresholds at a single assessment time point (Table S1, available online);3 yet, this is adevelopmental, particularly as tantrums are ubiquitous in early childhood, and thresholds were not empirically derived.3, 13 Empirically deriving clinical parameters using developmentally sensitive measures is crucial for normal:abnormal differentiation in early childhood, a period marked by rapid growth and change.15, 23
Here, we take this work a step further via a novel developmental measurement science approach; this study is the first to empirically derive optimized criteria for early childhood DMDD (EC-DMDD), using data-driven analyses with multiple longitudinal assessments and developmentally-specified characterization of irritable behaviors in young children. Although MAPS (Multidimensional Assessment of Preschoolers Study) was not designed a priori to validate EC-DMDD, and secondary data analyses are inherently constrained,24 we here capitalize on this existing, early childhood sample with rich, longitudinal characterization of irritability as a first step towards generating empirical parameters for an EC-DMDD profile.
Because of the substantial variation in preschool age misbehavior and rapid change in self-regulation capacity across early childhood,23 and evidence from our prior work in this sample indicating substantial intra-individual instability,15 we here test our hypothesis that requiring both longitudinal stability as well as pervasive impairment, i.e., impairment in multiple domains of functioning,10 will ensure that the transient elevations in irritability common to this developmental period will not be identified as false positives and thus will most validly represent EC-DMDD.2, 15 Moreover, we derive an empirically supported, optimized set of criteria (i.e., pinpointing the irritable behaviors that best differentiate atypical patterns at this age period) to describe the EC-DMDD profile and facilitate translation to clinical application. This additional step addresses a pressing need for studies to directly enable clinical application by providing parsimonious item sets that can be feasibly administered in the clinic and behavior-level thresholds for clinical decision-making. Finally, as methodologic advances in characterization of irritability have not yet been applied within a pragmatic measurement framework,25, 26 we also synthesize findings to illustrate how a practical tool/algorithm structured for clinical utility may be generated. Thus, our aims are to: (1) derive and validate a stable pattern of dysregulated, impairing irritability in early childhood by (1a) identifying the EC-DMDD profile and (1b) characterizing the predictive validity of the EC-DMDD profile; and (2) generate clinically informative, optimized behaviors with thresholds towards clinical utility.
Method
Participants
The present study utilizes data from three time points in the Multidimensional Assessment of Preschoolers (MAPS)15 longitudinal study (N=425), spanning preschool to early school age (T1: mean age=4.66 years, SD=.85; T2: mean=5.45 years, SD=.91; T3: mean=6.83 years, SD=.85), clinically enriched for psychopathology risk via oversampling for child disruptive behavior and domestic violence.15 n=425 children at T1 and n=403 at T2 had irritability data, and n=388 had impairment data at both T1 and T2; analyses used available data (n=425 for latent class analysis with best practices for imputation, see Supplement 1, available online; n=388 for other analyses involving impairment, see Analytic Plan below). Data from 306 of the original 425 families who participated in a reassessment visit at early school age (T3) and had complete diagnostic data were included for follow-up of traditional DSM diagnoses at early school age. Children who did (n=306) vs. did not participate in the early school age visit (n=119) were similar in poverty status (χ2=0.46, df=1, p=.50), race/ethnicity (χ2=3.65, df=3, p=.31), and baseline levels of irritability (t423=1.36, p=.18), but were more likely to be boys (χ 2=4.09, df=1, p=.043). Boys and girls did not differ in irritability at baseline (t423=0.84, p=.404), but there was a marginally significant trend for children in the “poor” group to have slightly higher baseline irritability (t423=1.93, p=.055). Additionally, an omnibus ANOVA showed overall differences among race/ethnicity groups on baseline irritability (F3,421=2.85, p=.037), although no post-hoc between-group comparisons were significant (all ps>.05, corrected). Subsequent predictive validity analyses controlled for poverty, race/ethnicity, and child sex. Participant characteristics are provided in Table 1.
Table 1.
Participant Demographics
| 425 | 26 | 362 | ||||||
|---|---|---|---|---|---|---|---|---|
| 4.66 | .85 | 4.76 | .81 | 4.63 | .86 | 0.775 | 386 | 0.439 |
| 217 | 51.1% | 8 | 30.8% | 192 | 53.0% | 4.82 | 1 | 0.028 |
| 212 | 49.9% | 15 | 57.7% | 186 | 51.4% | 1.12 | 3 | 0.772 |
| 127 | 29.9% | 8 | 30.8% | 107 | 29.6% | |||
| 79 | 18.6% | 3 | 11.5% | 63 | 17.4% | |||
| 7 | 1.6% | 0 | 0.0% | 6 | 1.7% | |||
| 209 | 49.2% | 17 | 65.4% | 179 | 49.4% | 2.47 | 1 | 0.116 |
Note: Mean age with standard deviation (SD). For all other categories, number of participants and percentage of total, in parentheses, shown. n=425 children at T1 and n=403 at T2 had irritability data, and n=388 had impairment data at both T1 and T2 (early childhood disruptive mood dysregulation disorder [EC-DMDD] profile analyses required irritability and impairment data). T1 = timepoint 1; T2 = timepoint 2.
Measures
Irritability
The Temper Loss scale of the Multidimensional Assessment Profile of Disruptive Behavior (MAP-DB)15, which has excellent psychometric properties and validity,13 was administered at both preschool time points (T1, T2) to assess irritability in the past month. The 22 Temper Loss items comprise a range of irritable behavior, encompassing tantrums and mood, from mild, “normative” misbehaviors to rare, severe, “atypical” behaviors in young children. These are rated on an objective frequency scale, which has the advantage of generating frequency severity thresholds that can be translated to symptom cut-offs.2 As described below, we utilized the MAP-DB Temper Loss factor for the latent transition analysis to define groups and the individual items for the frequency cutoffs for specific behaviors.
Impairment
The Family Life Impairment Scale (FLIS27), which has been validated in both clinical and nonclinical early childhood samples,28 was administered at T1 and T2 to assess whether children’s emotions and behavior were currently interfering with functioning in three domains: the child’s functioning, interactions with their family, or childcare (Cronbach’s α=.63–.81).15 Cross-domain impairment was defined as endorsing impairment in two or more FLIS domains based on our prior work.10
DSM-based assessment of DMDD at preschool age
To test the predictive utility of our empirically-based parameters for an EC-DMDD profile relative to preschool modified DSM DMDD criteria (previously validated21), DMDD status based on DSM criteria (excluding the >6 years of age requirement and using prior studies’ higher frequency threshold (i.e., “every day”, to prevent over-identification,22 vs. 3 days/week as in DSM-5)21 was ascertained at T1 using the Preschool Age Psychiatric Assessment (PAPA29), an interview with the parent, with the last 3 months as the primary period of recall. Inter-rater reliability was monitored on 20% of interviews, with κ ranging from .83–1.00 across PAPA diagnoses.
Clinical status at early school age
To evaluate predictive validity of the EC-DMDD profile, the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL)30 was administered to parents at early school age to assess clinical status at this age (“present diagnoses” = beginning or continuing through the last 6 months) for all DSM-5 diagnoses that include irritability in the criteria15 (i.e., major depressive/persistent depressive, attention deficit hyperactivity, and generalized anxiety disorders) and disruptive mood dysregulation and oppositional defiant (ODD) disorders, whose core feature is irritability. Subclinical and clinical cases for each diagnosis were combined in analyses, as our objective was to capture children with elevated symptoms across a risk spectrum. Inter-rater reliability was κ=.79–1.0. Of note, to capture developmental expression of symptoms, developmentally-appropriate interview methods were used, i.e., the PAPA at preschool age and the K-SADS at early school age.
Analytic Plan
We generated parameters for EC-DMDD by first identifying and validating a pattern that reflects DMDD phenomenology in early childhood, then narrowing down the behavior set to those that are the most clinically informative and defining clinical cutoffs for those behaviors.
Step 1: Model and validate a stable pattern of dysregulated, impairing irritability in early childhood
1a: Identify EC-DMDD profile
We conceptualized EC-DMDD a priori as children with persistent, elevated irritability with persistent, pervasive impairment across the two timepoints. To identify elevated irritability sustained over time, we used a latent transition analysis, based on the Temper Loss factor, across the two preschool time points (T1, T2). Latent transition analysis defines classes at each time point, then groups individuals by how they change (or fail to change) from class to class over time. The best-fitting model (i.e., which/how many classes) is determined through fit indices (Akaike and Bayesian Information Criteria; AIC, BIC). This approach is advantageous because it is a data-driven method that allows the persistently severely irritable groups to emerge (i.e., being in the elevated irritability group(s) consistently over time).
1b: Predictive validity of EC-DMDD profile
We evaluated predictive validity of the EC-DMDD profile for early school age DSM diagnoses using logistic regression with EC-DMDD group membership as the predictor. The outcome variables were the presence (vs. absence) of DMDD/ODD (combined due to the high overlap in irritability phenotype as the primary feature of both; all but one youth with DMDD also met criteria for ODD) or other irritability-related disorders at the T3 follow-up. We also contrasted predictive utility of the EC-DMDD profile to assessment at only one time point or single-domain impairment, as well as compared to DSM-based DMDD criteria. In addition, we tested the predictive validity of EC-DMDD for early school age DMDD/ODD above and beyond other preschool-age irritability-related diagnoses (ODD, major depressive disorder, dysthymia, depressive disorder not otherwise specified, attention deficit hyperactivity disorder, or generalized anxiety disorder) as well as diagnoses (all but DMDD, ODD) at school-age. We moreover tested whether EC-DMDD prediction was specific to irritability rather than the headstrong/hurtful dimension of ODD31 by including both in a logistic regression. All analyses controlled for sociodemographic variables (poverty, race/ethnicity, and child sex).
Step 2: Generate clinically informative, optimized behaviors with thresholds
Next, we derived optimized criteria for EC-DMDD by identifying the most parsimonious set of behaviors and the frequency thresholds at which these behaviors are clinically informative. To do this, we conducted receiver operator characteristic (ROC) analyses to test the sensitivity and specificity of each Temper Loss item (i.e., the specific behaviors) at T1 and T2, with the EC-DMDD profile (identified in Step 1) as the classification variable. Informative items had area under the curve (AUC)≥.80 and sensitivity≥.80 and/or specificity≥.80.32 We utilized Youden’s index to identify frequency cut points with maximal sensitivity and specificity.33 (See Supplement 1, available online, for additional details). Finally, to illustrate how our empirical approach generating an optimized behavior set and cutoffs could be pragmatically applied, we organized the optimized behaviors/cutoffs into an algorithm and tested sensitivity and specificity of this practical tool to identify EC-DMDD.
Results
Step 1: Model and validate a stable pattern of dysregulated, impairing irritability in early childhood
1a: Identify EC-DMDD profile
All fit indices indicated that a latent transition model with 3 levels at the first time point and 2 levels at the second time point fit the data best (Table S2, available online). This reflected six longitudinal classes, including one class with moderately high irritability at T1 and T2 (ModHi-ModHi, 16.5%, n=70) and another class with extremely high irritability at T1 and moderately high irritability at T2 (VeryHi-ModHi, 1.6%, n=7) (Figure 1). As both of these classes represent patterns of relatively elevated, persistent irritability, children in these two classes were combined (“persistent, elevated irritability group”, 18.1%, n=77). Children in the remaining four classes displayed other longitudinal patterns of irritability (82.9%, n=348; Supplement 1, available online; Figure 1). 37.7% of the children in the persistent, elevated irritability group (i.e., n=26 of the 69 with both impairment and irritability data) showed cross-domain impairment at both T1 and T2 (persistent, pervasive impairment) (Table 2). Thus, 26 children (6.7% overall, of the 388 with impairment and irritability data) were identified as having the EC-DMDD profile, i.e., persistent, elevated irritability with persistent, pervasive impairment (Table S3, available online).
Figure 1. Classes Based on Irritability Changes Over Time.
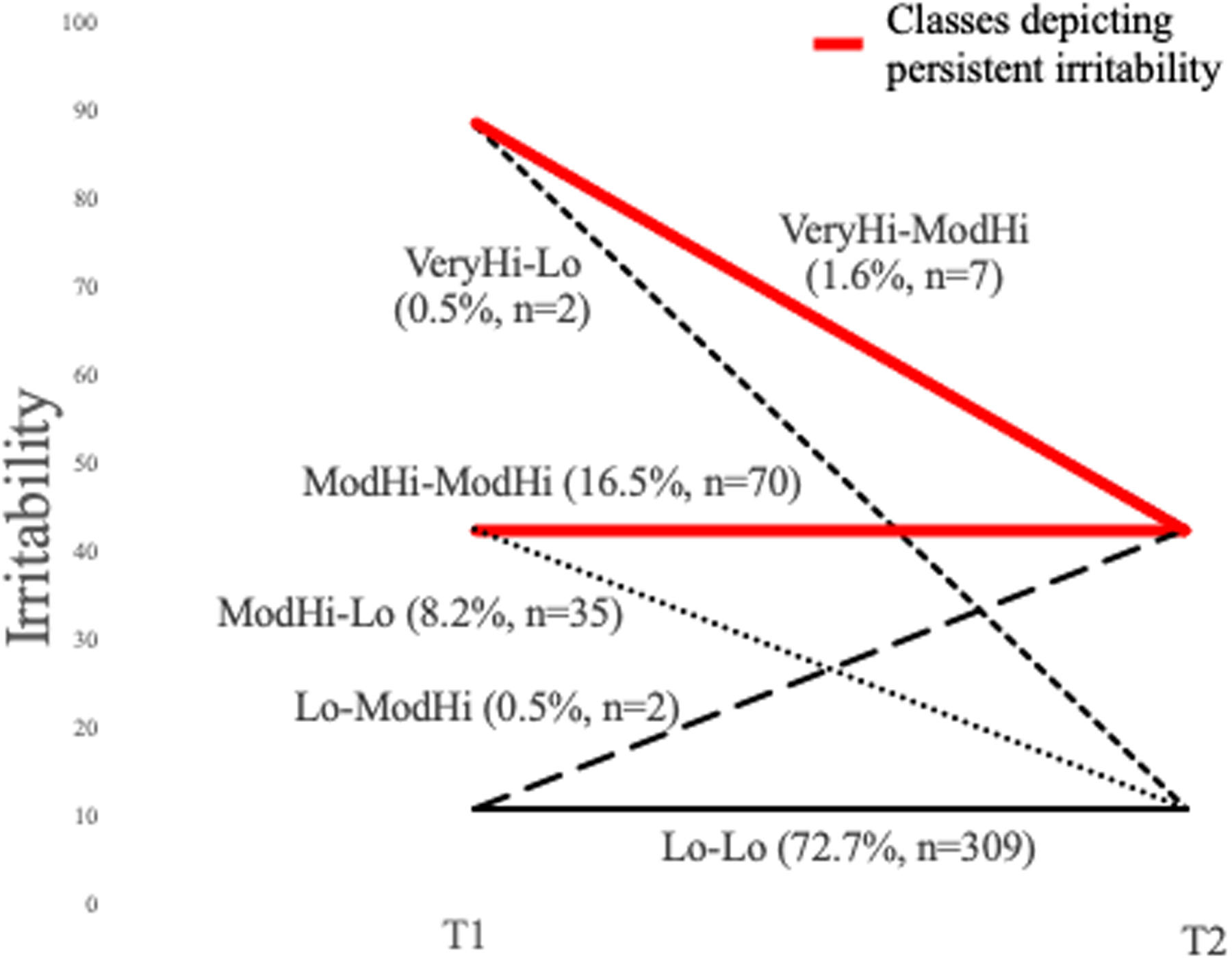
Note: Latent transition analysis identified 6 classes of individuals based on how they moved from group to group over time. T1=time point 1, T2=time point 2, Lo=low irritability, ModHi=moderately high irritability, VeryHi=very high irritability.
Table 2.
Proportion of Latent Transition Irritability Groups With Impairment Patterns
| Persistently Elevated Irritability Groups | Low or Transient Irritability Groups | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ModHi-ModHi | VeryHi-ModHi | Total | Lo-Lo | Lo-ModHi | ModHi-Lo | VeryHi-Lo | ||||||||
| N in each group | 70 | 7 | 77 | 309 | 2 | 35 | 2 | |||||||
| Never impaired | 22 | 31% | 1 | 14% | 23 | 30% | 92 | 30% | 0 | 0% | 6 | 17% | 0 | 0% |
| Cross-domain impairment at 1 time point | 18 | 26% | 2 | 29% | 20 | 26% | 75 | 24% | 2 | 100% | 10 | 29% | 2 | 100% |
| Impairment at 2 time points (but not cross-domain) | 44 | 63% | 4 | 57% | 48 | 62% | 94 | 30% | 0 | 0% | 16 | 46% | 1 | 50% |
| Cross-domain impairment at both time points | 24 | 34% | 2 | 29% | 26 | 34% | 23 | 7% | 0 | 0% | 7 | 20% | 0 | 0% |
Note: Children with persistently elevated irritability and pervasive (ie, cross-domain) impairment at both time points were identified with early childhood disruptive mood dysregulation disorder.
1b: Predictive validity of EC-DMDD profile
Children with the EC-DMDD profile were at significantly higher risk in early school age for DSM disorders in which irritability is a core feature (DMDD, ODD) relative to children without the EC-DMDD profile. Specifically, children with an EC-DMDD pattern at preschool age were more than 11 times more likely to have an irritability-related disorder at early school age (OR=11.52, p<.001) (Table 3, Table S4, available online). This association between EC-DMDD and school-age DMDD/ODD remained significant after controlling for all other disorders at both baseline and school-age (OR=4.69, p=.017) (Tables S4 and S5, available online). In addition, the EC-DMDD profile more strongly predicts early school age DMDD/ODD relative to traditional DSM-based DMDD criteria derived from the PAPA at preschool age (incremental Nagelkerke R2=0.082, χ2=16.99, df=1, p<.001). The elevated irritability with assessment at only one time point (i.e., T1), with single-domain impairment at one time point, or single-domain impairment at both time points remained significantly but less strongly predictive of early school-age DMDD/ODD relative to the derived EC-DMDD profile (ORs=6.01–9.36 vs. 11.52), which had cross-domain impairment and elevated irritability at both time points (Table 3). This suggests that heightened stringency, to account for normative developmental variation, and pervasive impairment will reduce the concern about false positives, which has been a major impediment to application of early childhood diagnoses to date. Of note, to further bolster this approach, we demonstrate that EC-DMDD relates to the irritability dimension of ODD (OR=1.96, p=.020), but not ODD’s headstrong/hurtful dimension (OR=1.38, p=.395). Lastly, the EC-DMDD profile additionally predicts other DSM disorders that include irritability-related features (Table 4).
Table 3.
Odds of Developing Disruptive Mood Dysregulation Disorder (DMDD) or Oppositional Defiant Disorder (ODD) in Early School Age Based on Early Childhood (EC) DMDD Profile Defined With 1 vs. 2 Time Points and Single- vs. Cross-domain Impairment
| DMDD or ODD in Early School Age | ||||
|---|---|---|---|---|
| 95% CI | ||||
| Adjusted Odds Ratio | Lower Bound | Upper Bound | p | |
| Irritable behaviors over 2 time points, and Cross-domain impairment over 2 time points | 11.521 | 4.132 | 32.119 | <.001 |
| Irritable behaviors at 1 time point, and Cross-domain impairment at 1 time point | 9.361 | 3.753 | 23.346 | <.001 |
| Irritable behaviors over 2 time points, and At least single-domain impairment over 2 time points | 6.007 | 2.983 | 12.096 | <.001 |
| Irritable behaviors at 1 time point, and At least single-domain impairment at 1 time point | 6.276 | 3.361 | 11.721 | <.001 |
Note: Compared to assessment at 1 time point and/or single-domain impairment, using assessment at 2 time points and cross-domain impairment yields the highest odds ratio (although not significantly so). Odds ratios adjusted for child’s sex, race/ethnicity, poverty status, and baseline age.
Table 4.
Early Childhood Disruptive Mood Dysregulation Disorder (EC-DMDD) Diagnosis Predicts DMDD in Early School Age and Other DSM Disorders that Feature Irritability
| 95% CI | |||||
|---|---|---|---|---|---|
| Adjusted Odds Ratio | Lower bound | Upper Bound | p | Proportion of EC-DMDD with school-age diagnosis | |
| Disruptive Mood Dysregulation Disorder | 7.148 | 1.465 | 34.868 | 0.015 | (3 of 19) |
| Oppositional Defiant Disorder | 8.990 | 3.359 | 24.058 | <.001 | (14 of 21) |
| Major Depressive Disorder or Persistent Depressive Disorder | 10.550 | 2.478 | 44.922 | 0.001 | (4 of 21) |
| Attention Deficit Hyperactivity Disorder | 4.627 | 1.535 | 13.948 | 0.007 | (6 of 21) |
| Generalized Anxiety Disorder | 6.110 | 1.855 | 20.121 | 0.003 | (5 of 21) |
| Any of the above (excluding DMDD) | 6.801 | 2.493 | 18.553 | <.001 | (15 of 21) |
Note: Odds ratios adjusted for child’s sex, race/ethnicity, poverty status, and baseline age.
Step 2: Generate clinically informative, optimized behaviors with thresholds for clinical utility
ROC analyses for each of the Temper Loss items classifying EC-DMDD indicated that six items at the first time point passed our classification accuracy threshold of AUC≥.80 (Tables S6 and S7, available online). These included tantrum and mood indicators indicative of dysregulation (i.e., become angry quickly, keep on having tantrum, get extremely angry), tantrums occurring in developmentally unexpectable contexts (e.g., tantrum for no reason, with other adults), and low frustration tolerance (i.e., easily frustrated). Consistent with prior work showing that normative items are associated with severity only at higher frequencies,13 irritability indicators that are normative misbehaviors had higher frequency cutpoints (e.g., frustrated easily, 1–3 days/week) than atypical items (e.g., tantrum for no reason, monthly). All five items were highly sensitive (.85–.96) and were thus retained as informative, although specificity values were somewhat lower (.55–.72) at baseline. This lower specificity means that these T1 items alone would over-identify DMDD.
At the second time point, ROC analyses indicated 5 items with both AUC≥.80 and specificity≥.80 (range: .80–91). These items were thus retained as informative items (Tables S6 and S7, available online). Sensitivity values ranged from .69–.85. Frustrated easily was the only item from the first time point that was retained at the second time point, with a cutoff at very high frequency (4–6 days/week). High frequencies of tantrums and irritable mood (≥1–3 days/week) specifically identified the EC-DMDD profile, as did the presence of dysregulated tantrums (e.g., break/destroy during tantrum). The optimized item set with these cutoffs, combined into an illustrative algorithm (Supplement 1, available online), sensitively (85%) and specifically (88%) identifies children in the EC-DMDD group.
Discussion
Empirically derived recommendations for EC-DMDD criteria
Our findings provide a foundation for a developmental nosology for EC-DMDD (Table S8) as well as an agenda for future research (Table S9). As a first step towards a more developmentally-based, dimensional approach to DMDD, these findings provide firm grounding for earlier identification. Importantly, using developmentally-sensitive expressions of irritability, accounting for developmental change, and requiring that irritability be pervasively impairing was the crux of normal:abnormal differentiation. Table S8 illustrates potential clinical application of these findings in a DSM context, and Supplement 1, available online, contains an algorithm for an EC-DMDD scale based on the findings. For practical purposes, we here used an approach aligned with current categorical decision-making. However, as it is now widely recognized that psychopathologic patterns are more dynamic and less discrete than the bounds of current nosological systems,34 our long-term objective is to apply this developmental-empirical approach to generate a dimensional risk spectrum, which may encompass several currently discrete irritability categories (i.e., DMDD, ODD), and enable tailored prevention at earlier phases of the clinical risk sequence (Table S9). Moreover, whereas the advantages of this empirically-derived approach for syndrome parameters is most apparent during this early-childhood period, which has proved so challenging for clinical differentiation, our results provide a model for empirically-derived, developmentally sensitive clinical identification that could potentially be applied across the lifespan.
Implications
These findings bolster prior work demonstrating that integrating developmental and clinical science, particularly through longitudinal assessments during this early childhood period marked by change, enables earlier identification of clinical syndromes that overlap with normative misbehavior that is typically transient or milder.18 Strikingly, <1% of children initially low in irritability at the first time point worsen over time, consistent with prior work,23 indicating that heterogeneity in developmental irritability patterns emanates largely from children at the mid-high points along the dimensional spectrum.15, 23 The use of repeated assessments optimizes accuracy of clinical identification, with the initial assessment acting as a screener, sensitively identifying children with potentially clinically significant irritability, as well as those for whom follow-up screening is not needed. The second assessment filters out the subset of initially flagged children whose heightened irritability was transient, within this early childhood period. In addition, our findings support that cross-domain impairment, i.e., pervasive difficulty, yields better predictive validity for the EC-DMDD profile than impairment in a single domain. Again, this highlights the need for developmentally-specified approaches to reduce the rate of false positives in this early childhood period where tantrums are very common13, 35, 36 but do not typically impair functioning in a sustained manner.15 Importantly, these assessments consisted of relatively brief parent surveys which could be administered online and made even more efficient via computer adaptive testing (CAT).37, 38 Future research on the number and spacing of assessments needed, as well as longer term prognostication, will be important for further refinement. This should include extension to infancy, where there is emergent evidence that normal:abnormal differentiation is also possible within developmental context.38, 39
Our developmentally-based psychometric approach also pinpointed particular features of irritability most informative for early clinical identification. For example, DSM-5 requires “mood [that is] persistently irritable or angry,” (i.e., tonic irritability) yet this description relies on subjective judgment without empirical anchoring. Our data suggest that for preschoolers, the most clinically informative features of irritable mood are rapid escalation (get extremely angry, become angry quickly) and difficulty recovering (difficulty calming down), sustained over two repeated assessments. Similarly, the DSM-5’s criterion “tantrums inconsistent with developmental level” (i.e., phasic irritability) is left to subjective judgment, which would be especially challenging for clinicians when >80% of preschoolers tantrum regularly.13 More objective features we found to be clinically informative were tantrums that occur in unexpectable contexts (with non-parental adults, for no reason) and are dysregulated (break/destroy, tantrum until exhausted). Also in contrast to DSM-5, we found that tantrum features that may be relevant for older children (e.g., “verbal rages”/“yell angrily at someone” and “physical aggression toward people”/“hit, bite, or kick during a tantrum”) were not especially informative for EC-DMDD, compared to other behavioral expressions of irritability. Of special importance is the centrality of low frustration tolerance (frustrated easily) for clinical identification, the only behavior sensitive and specific at both time-points for EC-DMDD. This is a “normative misbehavior” (i.e., present in the majority of preschoolers)2 and is not typically considered clinically informative. That is, current DMDD nosology focuses on more extreme behavioral expressions (outbursts and chronic irritable mood). Our finding highlights the importance of “bottom up” approaches not constrained to behaviors from extant nosology typically derived from older youths or adults, and also expanding phenomenology beyond consideration of extreme behaviors. Low frustration tolerance, identified here and previously as a strong predictor of impairment,10 may be important as a necessary (but not sufficient) substrate of irritability related disorders, i.e., a core problem that may underlie dysregulated behavioral expressions of irritability, and will be important to consider in an empirically-based classification system. Overall, employing empirically identified features of irritability that enable efficient normal:abnormal differentiation, as demonstrated here in young children, will improve precision and provide sturdy data-based parameters to guide clinicians. Predictive utility of the EC-DMDD profile also suggests that clinical approaches that account for heterogeneity and change in early childhood provide a reliable and meaningful way to address high levels of normative variation during this age period, that have so long impeded clinical applications in young children.
Frequency thresholds of the EC-DMDD items varied based on the normative vs. pathognomonic nature of the behavior in question.18 When normative misbehaviors (i.e. that most young children do) were present (e.g., frustrated easily, have a tantrum), these were clinically salient only when occurring with high regularity. Thus, screening without empirically determined frequency thresholds would contribute to false positives. By contrast, for severe pathognomonic items such as developmentally unexpectable or destructive/dysregulated tantrums (which most children never do), merely the presence of these behaviors, even rarely, was clinically significant. Our findings that EC-DMDD patterns encompass both elevated frequencies of normative misbehaviors and uncommon, highly dysregulated, severe behaviors suggests careful attention to the nature and frequency of behavior is key for developmentally-sensitive differentiation of clinical irritability in young children. In particular, the DSM nosologic focus on frequent, extreme behaviors is likely to create false negatives for preschool-age children with DMDD syndromes. This conundrum has impeded application of clinical nosologies to early childhood,40 yet exclusion of young children from DMDD constrains earlier identification and prevention at this period of heightened neuroplasticity.41 The generation of empirical thresholds for young children may thus prevent future nosologic approaches from “missing the boat.”
The current findings and recommendations must be considered within the context of their limitations. First, all measures were derived from maternal report; thus, shared method variance is a possibility, particularly for the predictive validity analyses. The use of direct, observational assessments and other informants will reduce this source of bias in future studies,42 as will incorporating biomarkers (e.g., neural profiles) to improve precision of clinical identification.43
Second, our preschool assessments were separated by approximately 9 months. This was useful for establishing the need for repeated assessments for children who present with elevated irritability. However, the time span is a methodologic artifact of the MAPS dataset. Future research in real world settings should determine the shortest possible interval between assessments to reliably establish persistence, which would enable quicker clinical decision-making and corollary preventive services.
Fourth, although we have a reasonably sized, clinically enriched sample (n=425), the number of children identified with the EC-DMDD profile was relatively small (n=26) and thus contributed to large confidence intervals for predictive validity, though this is consistent with prevalence in older children.44, 45 In addition, because boys were predominant in the EC-DMDD group, and moreover in those who went on to develop DMDD, the small number of girls with EC-DMDD at greatest risk for DMDD limits the generalizability of the findings for girls in particular. Replication and extension in large, population-based samples with closely spaced irritability assessments will be necessary and would also benefit from using irritability-specific impairment measures such as the recently developed Early Childhood Irritability-Related Impairment Interview (E-CRI46). This future work should elucidate individual differences in profiles and their clinical implications, including whether the derived parameters differ in boys vs. girls, children at the extreme vs. mid-level of the irritability spectrum, younger vs. older preschoolers and for examining the role of (dys)regulating home environments for more precise identification of those young children whose irritability declines over time.
The present study provides foundational evidence for empirically derived parameters for an early childhood DMDD profile, which is currently precluded in DSM-5. Here, we build on the burgeoning body of literature that has emerged since DSM-5, which suggests that the neurodevelopmental basis of these syndromes begins in early life and that establishing onset at school age “misses the boat” for the earliest expression of these syndromes.2 Such a category is necessary to capture young children in need of intervention, which could not only provide relief from chronic, severe irritability in preschool age but also potentially prevent the ensuing clinical cascade to chronic psychopathology, including a range of irritability-related disorders over time.2, 11, 47
Supplementary Material
Acknowledgments
This study was supported by National Institutes of Health/National Institute of Mental Health grants R01MH082830, R01MH107652, 2U01MH082830, U01MH090301 to Dr. Wakschlag and a Brain and Behavior Research Foundation NARSAD Young Investigator Award (26802) to Dr. Wiggins.
The authors thank Daniel S. Pine, MD, of the National Institute of Mental Health, Intramural Research Program, for his advice on the manuscript, Ryne Estabrook, PhD, of the University of Illinois at Chicago, and James Burns, MS, of Northwestern University, for statistical input, Kimberly McCarthy, MSW, of the University of Connecticut, for data management, and Erica Anderson, PhD, of Northwestern University, for oversight of clinical measurements. The authors are grateful to Lea Dougherty, PhD, of the University of Maryland, for her algorithm to assess disruptive mood dysregulation disorder in the Preschool Age Psychiatric Assessment.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Wiggins, Briggs-Gowan, Brotman, Leibenluft, and Wakschlag have reported no biomedical financial interests or potential conflicts of interest.
References
- 1.Brotman MA, Kircanski K, Stringaris A, Pine DS, Leibenluft E. Irritability in Youths: A Translational Model. Am J Psychiatry. June 1 2017;174(6):520–532. [DOI] [PubMed] [Google Scholar]
- 2.Wakschlag LS, Perlman SB, Blair RJ, Leibenluft E, Briggs-Gowan MJ, Pine DS. The Neurodevelopmental Basis of Early Childhood Disruptive Behavior: Irritable and Callous Phenotypes as Exemplars. Am J Psychiatry. February 1 2018;175(2):114–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Association AP. Diagnostic and statistical manual of mental disorders. 5 ed. Washington, DC: 2013. [Google Scholar]
- 4.Keenan K, Wakschlag LS. Can a valid diagnosis of disruptive behavior disorder be made in preschool children? Am J Psychiatry. March 2002;159(3):351–358. [DOI] [PubMed] [Google Scholar]
- 5.Casey BJ, Oliveri ME, Insel T. A Neurodevelopmental Perspective on the Research Domain Criteria (RDoC) Framework. Biological psychiatry. September 1 2014;76(5):350–353. [DOI] [PubMed] [Google Scholar]
- 6.Copeland WE, Brotman MA, Costello EJ. Normative Irritability in Youth: Developmental Findings From the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. August 2015;54(8):635–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. September 2009;166(9):1048–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dougherty LR, Smith VC, Bufferd SJ, Kessel E, Carlson GA, Klein DN. Preschool irritability predicts child psychopathology, functional impairment, and service use at age nine. J Child Psychol Psychiatry. September 2015;56(9):999–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheldrick RC, Neger EN, Perrin EC. Concerns about development, behavior, and learning among parents seeking pediatric care. J Dev Behav Pediatr. February 2012;33(2):156–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiggins JL, Briggs-Gowan MJ, Estabrook R, et al. Identifying Clinically Significant Irritability in Early Childhood. J Am Acad Child Adolesc Psychiatry. March 2018;57(3):191–199 e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dougherty LR, Leppert KA, Merwin SM, Smith VC, Bufferd SJ, Kushner MR. Advances and directions in preschool mental health research. Child Development Perspective. 2015;6(2):1–6. [Google Scholar]
- 12.Grabell AS, Li Y, Barker JW, Wakschlag LS, Huppert TJ, Perlman SB. Evidence of Non-Linear Associations between Frustration-Related Prefrontal Cortex Activation and the Normal:Abnormal Spectrum of Irritability in Young Children. J Abnorm Child Psychol. January 2018;46(1):137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wakschlag LS, Choi SW, Carter AS, et al. Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology. J Child Psychol Psychiatry. November 2012;53(11):1099–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perlman SB, Jones BM, Wakschlag LS, Axelson D, Birmaher B, Phillips ML. Neural substrates of child irritability in typically developing and psychiatric populations. Dev Cogn Neurosci. August 2015;14:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wakschlag LS, Estabrook R, Petitclerc A, et al. Clinical Implications of a Dimensional Approach: The Normal:Abnormal Spectrum of Early Irritability. J Am Acad Child Adolesc Psychiatry. August 2015;54(8):626–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petitclerc A, Briggs-Gowan MJ, Estabrook R, et al. Contextual variation in young children’s observed disruptive behavior on the DB-DOS: implications for early identification. J Child Psychol Psychiatry. September 2015;56(9):1008–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carlson GA, Danzig AP, Dougherty LR, Bufferd SJ, Klein DN. Loss of Temper and Irritability: The Relationship to Tantrums in a Community and Clinical Sample. J Child Adolesc Psychopharmacol. March 2016;26(2):114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wakschlag LS, Tolan PH, Leventhal BL. Research Review: ‘Ain’t misbehavin’: Towards a developmentally-specified nosology for preschool disruptive behavior. J Child Psychol Psychiatry. January 2010;51(1):3–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dougherty LR, Schwartz KTG, Kryza-Lacombe M, Weisberg J, Spechler PA, Wiggins JL. Preschool- and School-Age Irritability Predict Reward-Related Brain Function. J Am Acad Child Adolesc Psychiatry. June 2018;57(6):407–417 e402. [DOI] [PubMed] [Google Scholar]
- 20.Kessel EM, Dougherty LR, Kujawa A, Hajcak G, Carlson GA, Klein DN. Longitudinal Associations Between Preschool Disruptive Mood Dysregulation Disorder Symptoms and Neural Reactivity to Monetary Reward During Preadolescence. J Child Adolesc Psychopharmacol. March 2016;26(2):131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dougherty LR, Smith VC, Bufferd SJ, et al. DSM-5 disruptive mood dysregulation disorder: correlates and predictors in young children. Psychol Med. August 2014;44(11):2339–2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Copeland WE, Angold A, Costello EJ, Egger H. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. February 2013;170(2):173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wiggins JL, Mitchell C, Stringaris A, Leibenluft E. Developmental trajectories of irritability and bidirectional associations with maternal depression. J Am Acad Child Adolesc Psychiatry. November 2014;53(11):1191–1205, 1205 e1191–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wakschlag LS, Henry DB, Tolan PH, Carter AS, Burns JL, Briggs-Gowan MJ. Putting theory to the test: modeling a multidimensional, developmentally-based approach to preschool disruptive behavior. J Am Acad Child Adolesc Psychiatry. June 2012;51(6):593–604 e594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wakschlag LS, Roberts MY, Flynn RM, et al. Future Directions for Early Childhood Prevention of Mental Disorders: A Road Map to Mental Health, Earlier. J Clin Child Adolesc Psychol. May-Jun 2019;48(3):539–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glasgow RE. What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Educ Behav. June 2013;40(3):257–265. [DOI] [PubMed] [Google Scholar]
- 27.Mian ND, Soto TW, Briggs-Gowan MJ, Carter AS. The Family Life Impairment Scale: Factor Structure and Clinical Utility with Young Children. J Clin Child Adolesc Psychol. May 2 2018:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mian ND, Soto TW, Briggs-Gowan MJ, Carter AS. The Family Life Impairment Scale: Factor Structure and Clinical Utility with Young Children. J Clin Child Adolesc Psychol. 2018;47(sup1):S530–S541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Egger HL, Angold A. The preschool age psychiatric assessment (PAPA): A structured parent interview for diagnosing psychiatric disorders in preschool children. In: DelCarmen-Wiggins R, Carter AS, eds. Handbook of Infant and Toddler Mental Health Assessment. New York: Oxford University Press; 2004:223–243. [Google Scholar]
- 30.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. July 1997;36(7):980–988. [DOI] [PubMed] [Google Scholar]
- 31.Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent Irritability: Phenotypic Associations and Genetic Links With Depressed Mood. American Journal of Psychiatry. 2012;169(1):47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Committee on Children with Disabilities −. Developmental surveillance and screening of infants and young children. Pediatrics. July 2001;108(1):192–196. [DOI] [PubMed] [Google Scholar]
- 33.Lopez-Raton M, Cadarso-Suarez C, Rodriguez-Alvarez MX, Gude-Sampedro F. OptimalCutpoints: An R Package for Selecting Optimal Cutpoints in Diagnostic Tests. J Stat Softw. October 2014;61(8):1–36. [Google Scholar]
- 34.Casey BJ, Oliveri ME, Insel T. A neurodevelopmental perspective on the research domain criteria (RDoC) framework. Biol Psychiatry. September 1 2014;76(5):350–353. [DOI] [PubMed] [Google Scholar]
- 35.Bufferd SJ, Dougherty LR, Olino TM. Mapping the Frequency and Severity of Depressive Behaviors in Preschool-Aged Children. Child Psychiatry Hum Dev. December 2017;48(6):934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leppert KA, Bufferd SJ, Olino TM, Dougherty LR. A Daily Diary Analysis of Preschool Depressive Behaviors: Prospective Associations and Moderators Across 14 Days. J Abnorm Child Psychol. September 2019;47(9):1547–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gibbons RD, Weiss DJ, Frank E, Kupfer D. Computerized Adaptive Diagnosis and Testing of Mental Health Disorders. Annu Rev Clin Psychol. 2016;12:83–104. [DOI] [PubMed] [Google Scholar]
- 38.Wakschlag LS, Roberts M, Flynn R, et al. Future directions for early childhood prevention of mental disorders: A roadmap to Mental Health, Earlier. Journal of Clinical Child & Adolescent Psychology. 2019, 48(3), 539–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolke D, Rizzo P, Woods S. Persistent infant crying and hyperactivity problems in middle childhood. Pediatrics. June 2002;109(6):1054–1060. [DOI] [PubMed] [Google Scholar]
- 40.Wakschlag LS, Leventhal B, Thomas B. Disruptive behavior disorders & ADHD in preschool children: Characterizing heterotypic continuities for a developmentally informed nosology for DSM-5. In: Narrow W, First M, Sirovatka P, Regier D, eds. Age and gender considerations in psychiatric diagnosis: A research agenda for DSM-5. Arlington, VA: American Psychiatric Association; 2007:243–258. [Google Scholar]
- 41.Luby JL. Dispelling the “they’ll grow out of it” myth: implications for intervention. Am J Psychiatry. November 2012;169(11):1127–1129. [DOI] [PubMed] [Google Scholar]
- 42.Wakschlag LS, Briggs-Gowan MJ, Hill C, et al. Observational Assessment of Preschool Disruptive Behavior, Part II: validity of the Disruptive Behavior Diagnostic Observation Schedule (DB-DOS). J Am Acad Child Adolesc Psychiatry. June 2008;47(6):632–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bosl WJ, Tager-Flusberg H, Nelson CA. EEG Analytics for Early Detection of Autism Spectrum Disorder: A data-driven approach. Sci Rep. May 1 2018;8(1):6828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. November 1 2006;60(9):991–997. [DOI] [PubMed] [Google Scholar]
- 45.Mayes SD, Mathiowetz C, Kokotovich C, et al. Stability of Disruptive Mood Dysregulation Disorder Symptoms (Irritable-Angry Mood and Temper Outbursts) Throughout Childhood and Adolescence in a General Population Sample. J Abnorm Child Psychol. November 2015;43(8):1543–1549. [DOI] [PubMed] [Google Scholar]
- 46.Wakschlag LS, Krogh-Jespersen S, Estabrook CR, et al. The Early Childhood Irritability-Related Impairment Interview (E-CRI): A novel method for assessing young children’s developmentally-impairing irritability. under review. [DOI] [PMC free article] [PubMed]
- 47.Weiss B, Weisz JR, Politano M, Carey M, Nelson WM, Finch AJ. Relations among self-reported depressive symptoms in clinic-referred children versus adolescents. J Abnorm Psychol. August 1992;101(3):391–397. [DOI] [PubMed] [Google Scholar]
- 48.McCartney K, Burchinal MR, Bub KL. Best practices in quantitative methods for developmentalists. Monogr Soc Res Child Dev. 2006;71(3):1–145. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


