Abstract
Background
A population-based study would be useful to identify the association between chronic kidney disease (CKD) or acute kidney injury (AKI) and prognosis of coronavirus disease 2019 (COVID-19) patients.
Methods
This retrospective study utilized the claim data from Korea. Patients who underwent COVID-19 testing and were confirmed to be positive were included and divided into the following three groups based on the presence of CKD or requirement of maintenance dialysis: Non-CKD (participants without CKD), non-dialysis CKD (ND-CKD), and dialysis-dependent CKD (DD-CKD) patients. We collected data on the development of severe clinical outcomes and death during follow-up. Severe clinical outcomes were defined as the use of inotropics, conventional oxygen therapy, high-flow nasal cannula, mechanical ventilation, or extracorporeal membrane oxygenation and the development of AKI, cardiac arrest, myocardial infarction, or acute heart failure after the diagnosis of COVID-19. AKI was defined as the initiation of renal replacement therapy after the diagnosis of COVID-19 in patients not requiring maintenance dialysis. Death was evaluated according to survival at the end of follow-up.
Results
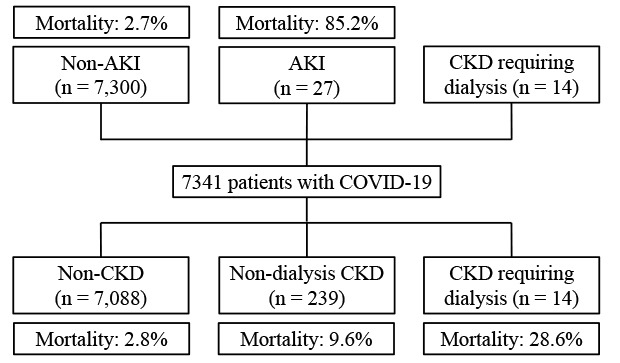
Altogether, 7,341 patients were included. The median duration of data collection was 19 (interquartile range, 11–28) days. On multivariate analyses, odds ratio (OR) for severe clinical outcomes in the ND-CKD group was 0.88 (95% confidence interval [CI], 0.64–1.20; P = 0.422) compared to the Non-CKD group. The DD-CKD group had ORs of 7.32 (95% CI, 2.14–33.90; P = 0.004) and 8.32 (95% CI, 2.37–39.21; P = 0.002) compared to the Non-CKD and ND-CKD groups, respectively. Hazard ratio (HR) for death in the ND-CKD group was 0.79 (95% CI, 0.49–1.26; P = 0.318) compared to the Non-CKD group. The DD-CKD group had HRs of 2.96 (95% CI, 1.09–8.06; P = 0.033) and 3.77 (95% CI, 1.29–11.06; P = 0.016) compared to the Non-CKD and ND-CKD groups, respectively. DD-CKD alone was associated with severe clinical outcomes and higher mortality. There was no significant difference in frequency of severe clinical outcomes or mortality rates between the Non-CKD and ND-CKD groups. In patients not requiring maintenance dialysis, AKI was associated with old age, male sex, and high Charlson's comorbidity index score but not with the presence of CKD. HRs for patients with AKI were 11.26 (95% CI, 7.26–17.45; P < 0.001) compared to those for patients without AKI in the multivariate analysis. AKI was associated with severe clinical outcomes and patient survival, rather than underlying CKD.
Conclusion
CKD requiring dialysis is associated with severe clinical outcomes and mortality in patients with COVID-19; however, the development of AKI is more strongly associated with severe clinical outcomes and mortality.
Keywords: Coronavirus Disease, Mortality, Chronic Kidney Disease, Acute Kidney Injury, Prognosis
Graphical Abstract
INTRODUCTION
Coronavirus disease (COVID-19) is a major global pandemic. As of 15th December 2020, a total of 39,402 patients were diagnosed with COVID-19 in Korea.1 The Korea Disease Control and Prevention Agency reported a COVID-19-related mortality of approximately 1.35% in South Korea. Favorable prognosis and rapid infectivity are important aspects of COVID-19. Several prognostic factors have been reported from previous studies, and ongoing studies may also be focused on the prognostic factors for COVID-19.
Chronic kidney disease (CKD) and acute kidney injury (AKI) are important health problems, and some studies have previously evaluated the association between these disorders and mortality in COVID-19 patients. Chen et al.2 compared the prevalence of pre-existing CKD and serum creatinine levels at the time of admission between deceased COVID-19 patients and surviving COVID-19 patients. They showed that, although the prevalence of CKD was not significantly different between the two groups, the deceased COVID-19 patients had higher serum creatinine levels at the time of admission. Other studies have evaluated the association between CKD and prognosis of COVID-19 patients.3,4,5,6 A meta-analysis showed a positive association between CKD and severity of COVID-19; however, all included studies individually reported a weak statistical association between the two, and most studies were conducted in the Chinese population.7 End-stage renal disease requiring maintenance dialysis is an advance stage of CKD and is also associated with poor prognosis of COVID-19 patients. Valeri et al.8 evaluated 59 patients on maintenance dialysis and reported a high mortality in dialysis patients.
Guan et al.3 evaluated 1,099 patients and showed that the incidence of AKI was 0.5% in all COVID-19 patients and 0.8% in COVID-19 patients requiring continuous renal replacement therapy. However, Chan et al.9 evaluated 3,235 hospitalized patients in USA and showed that the incidence of AKI was 46%; 20% of these patients required dialysis and showed a positive association between AKI and COVID-19 prognosis.
Many clinicians suggest that CKD and AKI are well-known risk factors for mortality in COVID-19 patients, but most previous studies on the association between CKD or AKI and clinical outcomes of COVID-19 patients were performed using limited cohorts, such as studies involving patients from a single center or those utilizing multicenteric data from regional hospitals.2,4,5,6,8,9 In addition, some studies did not compare between CKD patients with and without maintenance dialysis. Owing to these limitations of previous studies, further investigations are needed to identify the definite association between CKD and AKI, or CKD or AKI and COVID-19 prognosis. A population-based study would be useful to identify the association between CKD with or without maintenance dialysis or AKI and clinical outcomes of COVID-19 patients. The aim of the present study was to evaluate the association between CKD or AKI and clinical outcomes of COVID-19 patients using a population-based dataset.
METHODS
Data source
This retrospective study utilized the claims data from the Health Insurance Review & Assessment Service (HIRA) of Korea. The Korean national healthcare system and the Medical Aid program cover nearly all the population residing in South Korea. The HIRA, as a government-affiliated organization, collects nearly all information on patient's diagnosis and past medical or procedural data. The HIRA contained data of all patients diagnosed with COVID-19 from February 1, 2020, and May 15, 2020.10 They merged the data with the claims data during the last 3 years from January 1, 2017 to May 15, 2020. They provided the merged data after anonymization and de-identification. Patients who underwent COVID-19 testing and were confirmed to be positive were included, and those aged < 18 years were excluded.
Follow-up and outcomes
The index date of the last follow-up was May 15, 2020. Baseline characteristics evaluated included age, sex, Charlson's comorbidity index (CCI), and the time of diagnosis of COVID-19. After the diagnosis of COVID-19, we recorded the follow-up duration; time of death as the end of follow-up; the use of inotropics, conventional oxygen therapy, high-flow nasal cannula (HFNC), mechanical ventilation (MV), or extracorporeal membrane oxygenation (ECMO); and the development of AKI, cardiac arrest, myocardial infarction (MI), or acute heart failure.
Definitions of variables
Diseases, including COVID-19, were defined using the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10). COVID-19 patients were defined using diagnostic codes for COVID-19 (B342, B972, Z208, Z290, U18, U181, Z038, Z115, U071, or U072). Briefly, claims for COVID-19-related testing were made using a special code (MT043, national disaster fundholding 3/02), and reimbursement for confirmed cases were claimed based on B342, B972, Z208, Z290, U18, U181, Z038, Z115, U071, or U072 (B342, coronavirus infection in unspecified area; B972, coronavirus as the cause of the diseases in other chapters; Z208, contact with and suspected exposure to other communicable diseases; Z290, isolation; U18, tentative designation or emergency use of a new disease in Korea; U181, novel coronavirus infection; Z038, observation for other suspected diseases and conditions; Z115, special screening examination for other viral diseases; U071, COVID-19, virus identified; and U072, COVID-19, virus not identified). The HIRA has a list of patients with both MT043 code and any of these ICD-10 codes and the Korea Disease Control and Prevention Agency has a list of confirmed patients. The HIRA merged two lists.
The presence of comorbidities at 1 year prior to the diagnosis of COVID-19 was recorded and defined using ICD-10 codes proposed by Quan et al.11,12 Finally, the CCI score without age factor was calculated. During follow-up, the clinical outcomes, except death, were defined using Electronic Data Interchange or ICD codes from the HIRA (M0040 for conventional oxygen therapy; M0046 for HFNC; M5850 or M5857–M5860 for MV; O1901–O1904 for ECMO; O7020 for hemodialysis; O7031–O7035 or O7051–O7055 for continuous renal replacement therapy [CRRT]; O7061, O7062, O7071, or O7072 for peritoneal dialysis; I46, M5873–M5877, or M5880 for cardiac arrest; I21, I22, I252, M655x–M657x, OA631x–OA639x, OB631x–OB639x, OA641x, OA642x, OA647x, O0161x–O0171x, or O1641x–O1647x for MI; and I110, I130, I132, I255, I420, I425, I428, I429, I43, or I50 for acute heart failure). The use of inotropics was defined as the use of norepinephrine, epinephrine, vasopressin, dopamine, or dobutamine after the confirmed diagnosis of COVID-19.
Participants were divided into the following three groups based on the presence of CKD or requirement of maintenance dialysis: Non-CKD (participants without CKD), ND-CKD (non-dialysis CKD patients), and DD-CKD (dialysis dependent CKD patients). CKD patients were defined as those with ICD codes for N03, N05, N165, N18, N19, N250, I12, I13, Z490, Z491, Z492, Z940, Z992, E102, E112, E132, E142, or T861 at 1 year prior to the diagnosis of COVID-19. Patients with DD-CKD were defined as CKD patients with Electronic Data Interchange codes for dialysis over the last 3 months before the diagnosis of COVID-19 (O7020 for hemodialysis and O7061, O7062, O7071, O7072, or the drug codes for peritoneal dialysis solutions for peritoneal dialysis). AKI was defined as the initiation of hemodialysis, CRRT, or peritoneal dialysis after the diagnosis of COVID-19 in patients not requiring maintenance dialysis. The presence of severe clinical outcomes was defined as having one or more of the following conditions: the use of inotropics, conventional oxygen therapy, HFNC, MV, or ECMO, and the development of AKI, cardiac arrest, MI, or acute heart failure. Death was evaluated according to survival at the index date of the last follow-up.
Statistical analyses
Data were analyzed using SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC, USA). Categorical variables are expressed as number and percentage, and continuous variables are expressed as mean ± standard deviation. The Pearson χ2 test or Fisher's exact test was used to analyze categorical variables. For continuous variables, the means were compared using the Student's t-test or one-way analysis of variance, followed by Bonferroni's post-hoc comparison. The survival estimates were calculated using Kaplan-Meier curve and Cox regression analyses. P values for the comparison of survival curves were determined by the log-rank test. Multivariate Cox regression analyses were adjusted for age, sex, CCI score, and hypertension. In addition, logistic regression analyses were performed to evaluate the independent variables for clinical outcomes. The results of logistic regression were presented as odds ratio (OR) and 95% confidence interval (CI). Multivariate Cox regression analyses were also adjusted for age, sex, CCI score, and hypertension. P < 0.05 was considered to be statistically significant.
Ethics statement
The study was approved by the Institutional Review Board (IRB) of Yeungnam University Medical Center (IRB No: YUMC 2020-04-069). The board waived the need for obtaining patients' informed consent. The study was conducted in accordance with guidelines of the Declaration of Helsinki.
RESULTS
Clinical characteristics of the participants
The number of patients who underwent laboratory test for COVID-19 was 234,427. Among these, 7,590 patients (3.2%) were diagnosed with COVID-19. Participants aged < 18 years (n = 249) were excluded. Finally, 7,341 patients were included. The Non-CKD, ND-CKD, and DD-CKD groups consisted of 7,088 (96.5%), 239 (3.3%), and 14 (0.2%) patients, respectively (Table 1). The time interval from disease onset to final follow-up was 1-96 days. All patients in the DD-CKD group underwent maintenance hemodialysis. The CCI scores of the Non-CKD, ND-CKD, and DD-CKD groups were 1.2 ± 1.7, 5.4 ± 2.4, and 5.2 ± 2.2, respectively (P < 0.001). The mean age of patients in the Non-CKD, ND-CKD, and DD-CKD groups was 46.5 ± 18.9, 63.0 ± 14.8, and 59.6 ± 14.5 years, respectively (P < 0.001). Patients in the ND-CKD and DD-CKD groups showed higher frequencies of comorbidities than those in the Non-CKD group.
Table 1. Baseline characteristics of participants.
| Characteristics | Total (n = 7,341) | Non-CKD (n = 7,088) | ND-CKD (n = 239) | DD-CKD (n =14) | P value |
|---|---|---|---|---|---|
| Sex, male | 4,371 (59.5) | 4,241 (59.8) | 122 (51.0) | 8 (57.1) | 0.024 |
| Age, yr | 47.1 ± 19.0 | 46.5 ± 18.9 | 63.0 ± 14.8a | 59.6 ± 14.5a | < 0.001 |
| Follow-up duration, day | 20.8 ± 13.1 | 20.7 ± 13.0 | 24.5 ± 14.8a | 22.7 ± 15.6a | < 0.001 |
| Myocardial infarction | 97 (1.3) | 78 (1.1) | 19 (8.0) | 0 | < 0.001 |
| Congestive heart failure | 297 (4.0) | 247 (3.5) | 45 (18.8) | 5 (35.7) | < 0.001 |
| Peripheral vascular disease | 573 (7.8) | 516 (7.3) | 54 (22.6) | 3 (21.4) | < 0.001 |
| Cerebrovascular disease | 522 (7.1) | 470 (6.6) | 48 (20.1) | 4 (28.6) | < 0.001 |
| Dementia | 443 (6.0) | 410 (5.8) | 33 (13.8) | 0 | < 0.001 |
| Chronic pulmonary disease | 1,676 (22.8) | 1,586 (22.4) | 84 (35.2) | 6 (42.9) | < 0.001 |
| Connective tissue disease | 268 (3.7) | 241 (3.4) | 27 (11.3) | 0 | < 0.001 |
| Peptic ulcer disease | 1,102 (15.0) | 1,041 (14.7) | 58 (24.3) | 3 (21.4) | < 0.001 |
| Mild liver disease | 1,545 (21.0) | 1,384 (19.53) | 156 (65.3) | 5 (35.7) | < 0.001 |
| Diabetes mellitus | 1,230 (16.8) | 1,033 (14.6) | 190 (79.5) | 7 (50) | < 0.001 |
| Hemiplegia | 100 (1.4) | 95 (1.3) | 4 (1.7) | 1 (7.1) | 0.159 |
| Any malignancy | 359 (4.9) | 330 (4.7) | 28 (11.7) | 1 (7.1) | < 0.001 |
| Moderate to severe liver disease | 9 (0.1) | 7 (0.1) | 2 (0.8) | 0 | 0.006 |
| Metastatic tumor | 33 (0.4) | 29 (0.4) | 4 (1.7) | 0 | 0.016 |
| Acquired immune deficiency syndrome | 5 (0.1) | 4 (0.1) | 1 (0.4) | 0 | 0.108 |
| Hypertension | 1,572 (21.4) | 1,400 (19.8) | 159 (66.5) | 13 (92.9) | < 0.001 |
Data are expressed as number (%) for categorical variables and mean ± standard deviation for continuous variables. The P values were assessed using one-way analysis of variance, followed by Bonferroni's post hoc test for continuous variables and Pearson χ2 test or Fisher exact test for categorical variables.
Non-CKD = non-chronic kidney disease, ND-CKD = non-dialysis-chronic kidney disease, DD-CKD = dialysis dependent chronic kidney disease.
aP < 0.05 vs. Non-CKD group.
Severe clinical outcomes in COVID-19 patients
The number of the patients who had severe clinical outcomes was 1,266 (17.9%) in Non-CKD, 90 (37.7%) in ND-CKD, and 11 (78.6%) in DD-CKD groups, respectively (P < 0.001). Univariate logistic regression analyses showed that for severe clinical outcomes, the ND-CKD group had an OR of 2.78 (95% CI, 2.12–3.63; P < 0.001) compared to the Non-CKD group. The DD-CKD group had ORs of 16.82 (95% CI, 5.26–74.62; P < 0.001) and 6.06 (95% CI, 1.84–27.36; P = 0.007) compared to the Non-CKD and ND-CKD groups, respectively. Multivariate analyses showed that the ND-CKD group had an OR of 0.88 (95% CI, 0.64–1.20; P = 0.422) compared to the Non-CKD group. The DD-CKD group had ORs of 7.32 (95% CI, 2.14–33.90; P = 0.004) and 8.32 (95% CI, 2.37–39.21; P = 0.002) compared to the Non-CKD and ND-CKD groups, respectively.
The proportion of the patients who required the use of inotropics, conventional oxygen therapy, HFNC, MV, or ECMO, or were diagnosed with cardiac arrest or acute heart failure was greater in the DD-CKD group than in the other groups (Table 2). Multivariate logistic regression analyses showed that a higher proportion of patients in the DD-CKD group required the use of inotropics, conventional oxygen therapy, or MV than those in the other groups (Supplementary Table 1). Furthermore, a higher proportion of patients in the DD-CKD group required ECMO than those in ND-CKD group. ND-CKD or DD-CKD was not independently associated with cardiac arrest, MI, and acute heart failure during follow-up.
Table 2. Clinical outcomes according to groups.
| Clinical outcomes | Total (n = 7,341) | Non-CKD (n = 7,088) | ND-CKD (n = 239) | DD-CKD (n = 14) | P value |
|---|---|---|---|---|---|
| Acute kidney injury | 27 (0.37) | 24 (0.34) | 3 (1.26) | - | 0.021 |
| Inotropics use | 187 (2.5) | 170 (2.4) | 12 (5.0) | 5 (35.7) | < 0.001 |
| Conventional oxygen therapy | 909 (12.4) | 827 (1.6) | 74 (31.0) | 8 (57.1) | < 0.001 |
| High flow nasal cannula | 182 (2.5) | 165 (2.3) | 13 (5.4) | 4 (28.6) | < 0.001 |
| Mechanical ventilation | 127 (1.7) | 114 (1.6) | 9 (3.8) | 4 (28.6) | < 0.001 |
| ECMO | 21 (0.3) | 19 (0.3) | 1 (0.4) | 1 (7.1) | < 0.001 |
| Cardiac arrest | 43 (0.6) | 37 (0.5) | 5 (2.1) | 1 (7.1) | < 0.001 |
| Myocardial infarction | 257 (3.5) | 239 (3.4) | 17 (7.1) | 1 (7.1) | 0.006 |
| Acute heart failure | 382 (5.2) | 361 (5.1) | 19 (8.0) | 2 (14.3) | 0.046 |
The data are expressed as the number (%).
ECMO = extracorporeal membrane oxygenation, Non-CKD = non-chronic kidney disease, ND-CKD = non-dialysis-chronic kidney disease, DD-CKD = dialysis dependent chronic kidney disease.
AKI developed in 24 (0.3%) and 3 (1.3%) patients in the Non-CKD and ND-CKD groups, respectively (P = 0.021). The number of patients who underwent CRRT was 24 in Non-CKD, 3 in ND-CKD, and 3 in DD-CKD groups, respectively. All AKI patients in the Non-CKD and ND-CKD groups underwent CRRT, and 3 patients in the DD-CKD group were shifted to CRRT during follow-up. Multivariate logistic regression analyses revealed that old age, male sex, and high CCI score were associated with the development of AKI (Supplementary Table 2). The presence of CKD as an underlying comorbidity was not associated with the development of AKI during follow-up. Supplementary Table 3 shows that the development of AKI during follow-up was associated with a higher risk of use of inotropics, conventional oxygen therapy, HFNC, MV, or ECMO or the development of cardiac arrest or acute heart failure.
Patient survival
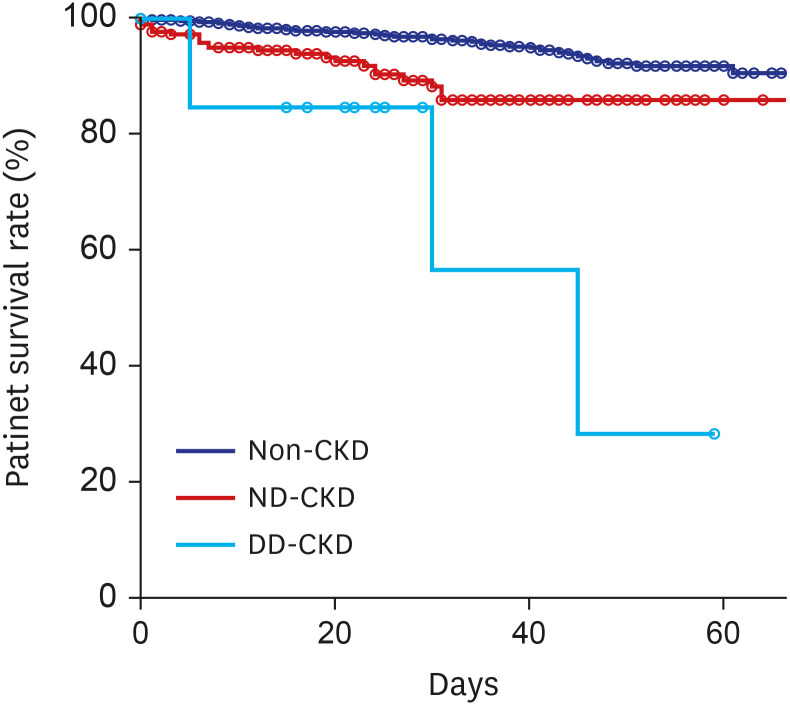
During follow-up, a total of 227 (3.1%) patients died. The number of deaths during follow-up in the Non-CKD, ND-CKD, and DD-CKD groups were 200 (2.8%), 23 (9.6%), and 4 (28.6%), respectively (P < 0.001). Kaplan-Meier curves showed that CKD was significantly associated with mortality in COVID-19 patients (P < 0.001 for Non-CKD vs. ND-CKD and P = 0.001 for ND-CKD vs. DD-CKD) (Fig. 1). Multivariate Cox regression analysis showed that the DD-CKD group had a higher mortality risk than the other groups (Table 3). However, the differences in the mortality risk between the Non-CKD and ND-CKD groups were not significant.
Fig. 1. Kaplan-Meier survival curves of the CKD groups. Blue, red, and skyblue lines reveal survival graphs of the Non-CKD, ND-CKD, and DD-CKD groups, respectively. Circle reveals a censored point. The 20-day survival rates were 97.6%, 92.4%, and 84.6% for the Non-CKD, ND-CKD, and DD-CKD groups, respectively (P < 0.001). The 40-day survival rates were 94.7%, 85.7%, and 56.4% for the CON, ND-CKD, and DD-CKD groups, respectively.
CKD = chronic kidney disease, Non-CKD = non-chronic kidney disease, ND-CKD = non-dialysis-chronic kidney disease, DD-CKD = chronic kidney disease requiring dialysis.
Table 3. Cox regression analysis of survival according to variables.
| Variables | Univariate | Multivariate | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| Age per increase 1 yr | 1.11 (1.10–1.12) | < 0.001 | 1.10 (1.09–1.11) | < 0.001 | |
| Sex, ref: male | 0.61 (0.47–0.79) | < 0.001 | 0.48 (0.37–0.63) | < 0.001 | |
| CCI score | 1.35 (1.30–1.39) | < 0.001 | 1.15 (1.09–1.21) | < 0.001 | |
| Hypertension | 8.32 (6.21–11.16) | < 0.001 | 1.37 (0.99–1.90) | 0.057 | |
| CKD group | |||||
| ND-CKD, ref: Non-CKD | 2.87 (1.86–4.42) | < 0.001 | 0.79 (0.49–1.26) | 0.318 | |
| DD-CKD, ref: Non-CKD | 9.38 (3.49–25.26) | < 0.001 | 2.96 (1.09–8.06) | 0.033 | |
| DD-CKD, ref: ND-CKD | 3.27 (1.13–9.47) | 0.029 | 3.77 (1.29–11.06) | 0.016 | |
Multivariate analysis was adjusted for age, sex, CCI score, hypertension, and CKD groups.
CCI = Charlson's comorbidity index, HR = hazard ratio, CI = confidence interval, Non-CKD = non-chronic kidney disease, ND-CKD = non-dialysis-chronic kidney disease, DD-CKD = dialysis dependent chronic kidney disease.
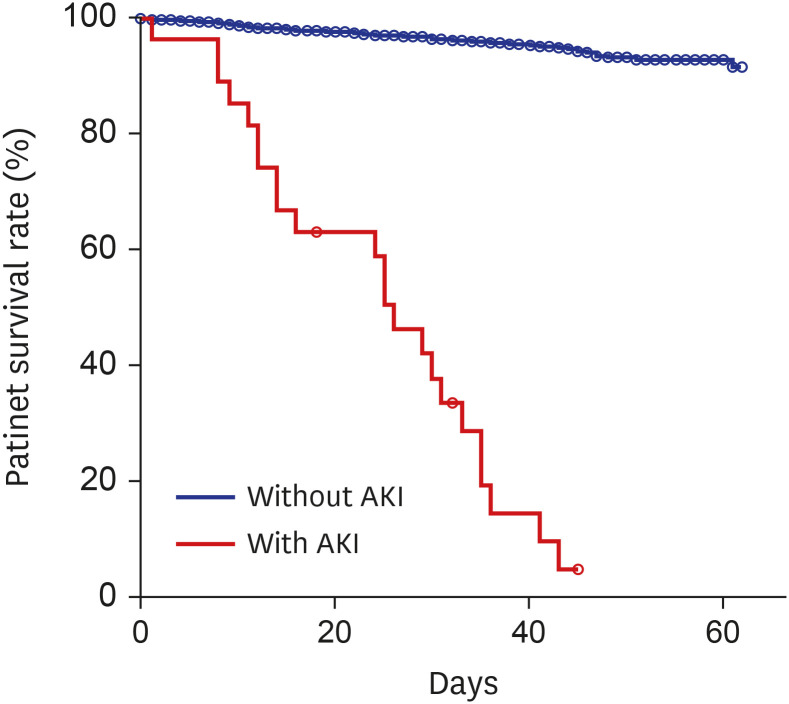
During follow-up, 200 (2.7%) and 23 (85.2%) patients without and with AKI died, respectively (P < 0.001). The 20-day survival rates of patients without and with AKI were 97.6% and 63.0%, respectively (Fig. 2), and the 40-day survival rates were 95.2% and 14.4%, respectively.
Fig. 2. Kaplan-Meier survival curves of the AKI groups. Blue and red lines reveal the survival graph of patients without and with AKI, respectively. Circle reveals a censored point.
AKI = acute kidney injury.
We performed additional survival analyses involving patients not requiring maintenance dialysis. Cox regression analysis showed that the HRs for patients with AKI were 11.26 (95% CI, 7.26–17.45; P < 0.001) compared to those for patients without AKI in the multivariate analysis (Supplementary Table 4). Supplementary Fig. 1 shows a forest plot of the association between CKD or AKI and mortality according to subgroups in patients not requiring maintenance dialysis. The number of patients not requiring maintenance dialysis was 7,327 and 223 deaths occurred in these patients. The number of patients aged ≤ 60 and > 60 years were 5,459 and 1,868, respectively; of these, 19 and 204 patients died, respectively. There were 2,964 male and 4,363 female patients; of these, 120 and 103 patients died, respectively. The number of patients with and without diabetes mellitus and those with and without hypertension was 1,223 and 6,104 and 1,559 and 5,768, respectively; of these, 115 and 108, and 161 and 62 patients died, respectively. Subgroup analyses for age (≤ 60 vs. > 60 years), sex, diabetes mellitus, and hypertension showed that the development of AKI during follow-up was associated with higher mortality, rather than the prevalent CKD as an underlying comorbidity (Supplementary Fig. 1).
DISCUSSION
Our population-based study showed that DD-CKD alone was associated with severe clinical outcomes and higher mortality. There was no significant difference in the frequency of severe clinical outcomes or mortality rate between the Non-CKD and ND-CKD groups. In patients not requiring maintenance dialysis, AKI was associated with old age, male sex, and high CCI score but not with the presence of CKD. AKI was associated with severe clinical outcomes and patient survival, rather than underlying CKD. For each outcome among the severe clinical outcomes, most variables showed similar trends.
A meta-analysis in a Chinese population showed a positive, although weak, association between CKD and the severity of COVID-19.7 Recent studies using a large sample size from USA or UK showed that the presence of CKD was significantly associated with adverse outcomes.9,13,14 Although there has been no data regarding the association between these two variables, CKD patients are reported to exhibit immunity dysfunction, which may be associated with more severe lung injury.15 Advanced CKD might be associated with higher adverse outcomes than early-stage CKD. Dialysis patients may be prone to higher risk of adverse outcomes among CKD patients. Valeri et al.8 reported a mortality rate of 31% among 59 dialysis patients. A study on 36 hemodialysis patients showed that the mortality rate was 30.5%.16
In our study, DD-CKD was associated with higher adverse outcomes than Non-CKD and ND-CKD, but there were no significant differences in the frequency of adverse outcomes between the Non-CKD and ND-CKD groups. The non-significant association between these two groups may be attributed to our definition of CKD. The estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2 is the widely accepted definition of CKD.17 Flythe et al.18 compared the prognosis between non-dialysis CKD patients with eGFR < 60 mL/min/1.73 m2, dialysis-dependent CKD patients, and patients with eGFR ≥ 60 mL/min/1.73 m2 and showed that patients with dialysis-dependent CKD had the poorest outcomes, where those with eGFR ≥ 60 mL/min/1.73 m2 had the best outcomes. Williamson et al.19 utilized a more detailed classification method and showed that non-dialysis CKD patients with eGFR < 30 mL/min/1.73 m2 had poorer outcomes than those with eGFR 30–60 mL/min/1.73 m2. eGFR < 60 mL/min/1.73 m2 is generally associated with an increased risk of CKD complications, and the prognosis of early-stage CKD patients with eGFR 60–90 mL/min/1.73 m2 may be similar to that of individuals with a normal renal function. In our study, CKD was defined using the ICD-10 codes, which include both early-stage and advanced CKD. Although we did not determine the accurate number of patients depending on their CKD stage, except for those with end-stage renal disease, a large proportion of patients in the ND-CKD group may be suffering from early-stage CKD. Non-association of clinical outcomes and survival between Non-CKD and ND-CKD groups in our study could be attributed to the inaccurate definition of ND-CKD. However, there were few studies on the prognosis of patients with eGFR 60–90 mL/min/1.73 m2. Further studies with accurate CKD staging could help in identifying the difference in clinical outcomes among patients with varying severities of CKD.
In COVID-19 patients, AKI might develop via a direct cytopathic effect of renal cells or indirect effects caused by virus-induced immunological damages or cytokines.20,21,22,23 Su et al.20 evaluated the postmortem renal pathology and showed evidences for virus infection in podocytes and tubular epithelial cells by immunostaining or electron microscopy. Previous studies have shown a positive association between AKI and poor prognosis of COVID-19 patients.2,6,9,21,22,23,24,25,26 Lim et al.24 investigated the clinical outcomes according to the AKI stage and found that patients with severe AKI with serum creatinine levels ≥ 300% or those requiring dialysis had higher mortality than those without AKI or with mild AKI. Hirsch et al.22 evaluated 5,449 hospitalized patients and showed that 37% of the patients developed AKI. They also revealed that the mortality rate of AKI patients requiring dialysis was 55.1%, and the use of MV was greater in patients with AKI than in those without AKI. Recently, a meta-analysis of 10 studies showed that the incidence of AKI in deceased or surviving patients was 52% and 7%, respectively.27
The association between AKI and adverse outcomes of COVID-19 patients could be attributed to several factors. First, AKI could be caused by direct invasion of severe acute respiratory syndrome coronavirus 2 and it is assumed that AKI can be considered as an indicator of more severe systemic infection with the involvement of other organs beyond the lungs. Second, AKI could develop by indirect effects of shock, hypoxia, or inflammatory cytokines, which were closely associated with patient survival. Third, AKI is associated with abnormal volume status and uremic condition. These factors can lead to various adverse outcomes, such as pulmonary edema or uncontrolled infection.
Our study showed that AKI was more closely associated with adverse outcomes than CKD, even though DD-CKD had more severe adverse outcomes than Non-CKD or ND-CKD. Our results may be in line with those from Petrilli et al.'s13 prospective cohort study involving 5,279 patients, which reported that underlying comorbidities were predictors of admission to hospital and, to a lesser extent, of the severity of disease. Impairment of oxygen or markers of inflammation on disease onset was more significantly associated with severity of disease or mortality than underlying comorbidities. In our study, DD-CKD alone was modestly associated with adverse outcome. Development of AKI during follow-up could be a direct/indirect indicator of the severity of COVID-19. AKI, per se, or as an indicator of disease severity, was strongly associated with adverse outcomes in COVID-19 patients in our study. In addition, the presence of CKD was not associated with the development of AKI in COVID-19 patients, which might be attributed to two factors. First, patients in the ND-CKD group might have, at most, early-stage CKD. Second, the severity of disease, per se, including systemic inflammation/infection, was more strongly associated with the development of AKI than the presence of CKD.
Diabetes mellitus is an important comorbidity associated with the prognosis of COVID-19 patients. CCI includes the scores of patients with diabetes mellitus. The addition of diabetes mellitus as a covariate may be associated with a statistical error. However, our study included data from our subgroup analyses of patients with and without diabetes mellitus, and the data showed a similar trend with those obtained when analyzing the whole patient cohort. In addition, multivariate models of our data did not include some variables, such as the use of inotropics, MV, or ECMO. The use of inotropics, MV, or ECMO may be highly associated with the development of AKI or mortality, as shown in Supplementary Table 3 (e.g., all patients with AKI used inotropics). In addition, we had a small number of patients in the DD-CKD group or those with AKI. Considering the small sample size of the DD-CKD group or patients with AKI and the highly deviated distribution among variables, the addition of these variables to the multivariate models may lead to biased results or influence the statistical significance of other variables. Therefore, we decided to exclude these variables from the multivariate model.
Our study had several limitations. First, we used health insurance claims with Electronic Data Interchange or ICD codes from HIRA. Therefore, our study did not include laboratory or clinical data. The dataset had a possibility of overcoding or undercoding, which might lead to discrepancies between the relevant code and the actual condition. In our study, AKI was defined as a requirement of dialysis due to the absence of data on serum creatinine levels or urine output. We did not evaluate the grade of AKI, and the AKI cases in our study included only severe AKI cases requiring dialysis. In addition, CKD was defined using the ICD codes, and we did not identify the CKD stage. Less extent of advanced CKD might be responsible for non-association with clinical outcomes between Non-CKD and ND-CKD groups. The AKI/CKD stage using laboratory or clinical findings could be helpful in identifying its association with clinical outcomes according to the AKI/CKD stages. Second, the follow-up period was relatively short, and the dataset did not include data of patients who did not claim for health insurance despite changes in the intervention and/or death. Therefore, we suggest that multi-center or registry studies with a larger sample population using more accurate laboratory or clinical data, such as serum creatinine levels, must be conducted.
In conclusion, CKD requiring maintenance dialysis is associated with adverse outcomes and mortality in COVID-19 patients; however, the development of AKI is more strongly associated with adverse outcomes and mortality.
ACKNOWLEDGMENTS
The authors appreciate healthcare professionals dedicated to treating COVID-19 patients in Korea, and the Ministry of Health and Welfare and the Health Insurance Review & Assessment Service of Korea for sharing invaluable national health insurance claims data in a prompt manner.
Footnotes
Funding: This work was supported by the 2020 Yeungnam University Medical Center COVID-19 Research Grant.
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Kang SH, Kim SW, Do JY.
- Data curation: Kang SH, Kim AY, Cho KH, Park JW.
- Formal analysis: Kang SH, Kim AY.
- Funding acquisition: Do JY.
- Methodology: Kim SW.
- Project administration: Kang SH.
- Software: Kim SW.
- Validation: Do JY.
- Visualization: Kang SH, Do JY.
- Writing - original draft: Kang SH, Do JY.
- Writing - review & editing: Kang SH, Do JY.
SUPPLEMENTARY MATERIALS
Logistic regression analysis of clinical outcomes according to variables
Logistic regression analysis of risk of acute kidney injury according to variables
Clinical outcomes according to the development of acute kidney injury in patients without maintenance dialysis
Cox regression analysis of survival according to variables in patients without maintenance dialysis
Forest plots of the association between CKD or AKI and mortality in patients without maintenance dialysis (A) Forest plot of the association between CKD and mortality according to subgroups in patients without maintenance dialysis. (B) Forest plot of the association between AKI and mortality according to subgroups in patients without maintenance dialysis. Adjustment according to age, sex, Charlson's comorbidity index score, and hypertension.
References
- 1.Korea Disease Control and Prevention Agency. The updates on COVID-19 in Korea as of 15 December. [Updated 2020]. [Accessed December 15, 2020]. http://www.kdca.go.kr/board/board.es?mid=a30402000000&bid=0030.
- 2.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020;71(15):762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi Y, Yu X, Zhao H, Wang H, Zhao R, Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108. doi: 10.1186/s13054-020-2833-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang X, Fang X, Cai Z, Wu X, Gao X, Min J, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 Patients: a systemic review and meta-analysis. Research (Wash D C) 2020;2020:2402961. doi: 10.34133/2020/2402961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valeri AM, Robbins-Juarez SY, Stevens JS, Ahn W, Rao MK, Radhakrishnan J, et al. Presentation and outcomes of patients with ESKD and COVID-19. J Am Soc Nephrol. 2020;31(7):1409–1415. doi: 10.1681/ASN.2020040470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan L, Chaudhary K, Saha A, Chauhan K, Vaid A, Baweja M, et al. Acute kidney injury in hospitalized patients with COVID-19. medRxiv. [Updated 2020]. [Accessed July 7, 2020]. https://www.medrxiv.org/content/10.1101/2020.05.04.20090944v1.
- 10.Ministry of Health and Welfare, Health Insurance Review & Assessment Service. #opendata4covid19. [Updated 2020]. [Accessed July 3, 2020]. https://hira-covid19.net.
- 11.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 13.Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamada T, Mikami T, Chopra N, Miyashita H, Chernyavsky S, Miyashita S. Patients with chronic kidney disease have a poorer prognosis of coronavirus disease 2019 (COVID-19): an experience in New York City. Int Urol Nephrol. 2020;52(7):1405–1406. doi: 10.1007/s11255-020-02494-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goicoechea M, Sánchez Cámara LA, Macías N, Muñoz de Morales A, Rojas ÁG, Bascuñana A, et al. COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int. 2020;98(1):27–34. doi: 10.1016/j.kint.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2005;67(6):2089–2100. doi: 10.1111/j.1523-1755.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- 18.Flythe JE, Assimon MM, Tugman MJ, Chang EH, Gupta S, Shah J, et al. Characteristics and outcomes of individuals with pre-existing kidney disease and COVID-19 admitted to intensive care units in the United States. Am J Kidney Dis. doi: 10.1053/j.ajkd.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219–227. doi: 10.1016/j.kint.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hirsch JS, Ng JH, Ross DW, Sharma P, Shah HH, Barnett RL, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020;98(1):209–218. doi: 10.1016/j.kint.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim JH, Park SH, Jeon Y, Cho JH, Jung HY, Choi JY, et al. Fatal outcomes of COVID-19 in patients with severe acute kidney injury. J Clin Med. 2020;9(6):E1718. doi: 10.3390/jcm9061718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y, Lu X, Li Y, Chen H, Chen T, Su N, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201(11):1430–1434. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brienza N, Puntillo F, Romagnoli S, Tritapepe L. acute kidney injury in coronavirus disease 2019 infected patients: a meta-analytic study. Blood Purif. 2020;2:1–7. doi: 10.1159/000509274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Logistic regression analysis of clinical outcomes according to variables
Logistic regression analysis of risk of acute kidney injury according to variables
Clinical outcomes according to the development of acute kidney injury in patients without maintenance dialysis
Cox regression analysis of survival according to variables in patients without maintenance dialysis
Forest plots of the association between CKD or AKI and mortality in patients without maintenance dialysis (A) Forest plot of the association between CKD and mortality according to subgroups in patients without maintenance dialysis. (B) Forest plot of the association between AKI and mortality according to subgroups in patients without maintenance dialysis. Adjustment according to age, sex, Charlson's comorbidity index score, and hypertension.