Abstract
Background
The most recent global pandemic of COVID-19 has been creating multidimensional damages, including a detrimental impact on the mental health status of individuals. Medical students, a vulnerable cross-section of the population, may have perceived a myriad of psychological stressors during this crisis in the background of their prevailing stressful academic pressure and preexisting higher psychological and mental health issue.
Objective
To determine the prevalence of anxiety and depressive symptoms and to elucidate the psychological impact of COVID-19 pandemic on Bangladeshi medical students.
Method
A cross-sectional study design was utilized to conduct this survey. The online survey including demographic questions, COVID-19 related questions, and the Hospital Anxiety and Depression Scale (HADS; higher scores on the subscales indicate higher levels of depressive and anxiety symptoms), was completed by 425 Bangladeshi medical students. Collected data were statistically analyzed by using SPSS (version 25.0) software.
Result
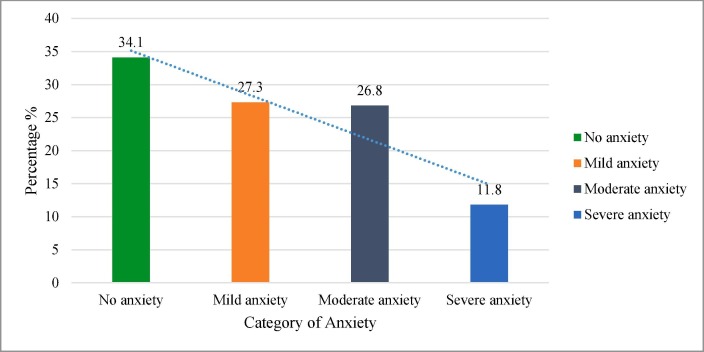
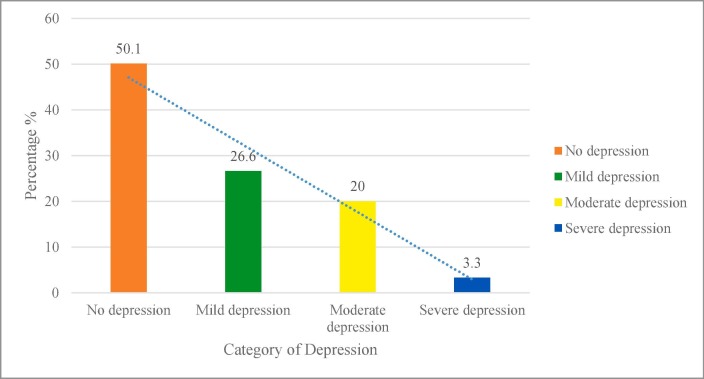
The HADS anxiety subscale revealed that 65.9% of the medical students had different levels of anxiety, ranging from mild (27.3%), moderate (26.8%), and severe (11.8%). As per HADS depression subscale, 49.9% of the medical students had varying degrees of depressive symptoms, with 3.3% of the participants had suffered from severe depressive symptoms. Female students had a relatively more anxiety and depressive symptoms when compared with males. The students, who were severely tensed of getting infected by the virus, were at higher risk of suffering from anxiety (3.5-fold) and depressive (2.7-fold) symptoms, when compared with no/minimally stressed students. Besides, fear of getting assaulted or humiliated on the way to hospital or home, not to be able to give maximum concentration on study after COVID-19 pandemic, students’ present emotional status (agitation), had statistically significant higher risk of anxiety.
Conclusion
A substantial proportion of Bangladeshi medical students are experiencing pandemic-related adverse psychological impact. Poor mental health conditions of these vulnerable medical students pose important threat to their potential contribution in future health care. Thus, medical colleges and health authorities should focus on addressing their psychological needs and formulate effective strategies to ameliorate medical students’ mental health status, particularly during any infectious disease outbreak.
Keywords: COVID-19, Depressive symptoms, Anxiety, Medical students, Bangladesh
1. Background
The grievous impact of any epidemic and/or pandemic on the mental health status of individuals is not unknown. Evidence on this statement has documented in the literature base, where negative psychological consequences were reported among diverse population group during various infectious disease outbreak, such as severe acute respiratory syndrome (SARS) in 2003 (Hawryluck et al., 2004, Maunder et al., 2003, Peng et al., 2010), novel influenza A (HIN1) in 2009 (Matsuishi et al., 2012, Taha et al., 2014), and 2014 Middle East Respiratory Syndrome (MERS) (Al-Rabiaah et al., 2020). Following SARS and MERS outbreak, the most recent COVID-19 global pandemic caused by SARS COV-2, a coronavirus belongs to the same Betacoronavirus genus as SARS and MERS (Guo et al., 2020), is of no exception in creating multidimensional damages, including a detrimental impact on mental health. Currently (as of June 3, 2020) COVID-19 has spread to 216 countries with a total of 6,416, 828 confirmed cases, claimed the lives of 382,867 people (Organization, 2020), and this statistic is proportionately increasing gradually which will create a wreaking havoc on economical, social and psychological aspects of residents living in the affected countries.
It is clear that the volatile existence and ambiguity of COVID-19 has induced major adverse psychological effects and subsequently driven the population to suffer depression, anxiety and post-traumatic stress disorder (Bao et al., 2020, Zandifar and Badrfam, 2020). Mandatory quarantine and lockdown in different countries across the world have put people going through substantially higher number of mental distress and when a near one is affected by COVID-19, then the mental condition of people deteriorate in bad manner. In addition to this, lack in knowledge of coping strategies terrified the common people in the worst manner (Mazza et al., 2020, Roma et al., 2020). Studies have reported disproportionately higher psychological distress among the frontline staffs who were involved in the direct patient care during this crisis (Chen et al., 2020, Greenberg et al., 2020). However, the adverse mental health implications of public especially women, children, adolescents, students, patients, and older adults cannot be overlooked (Cao et al., 2020, Liu et al., 2020, Yang et al., 2020; J. Zhang et al., 2020). While students are deemed as a vulnerable cross-section of population who may experience an unprecedented psychological impact of the pandemic such as higher levels of stress, anxiety and depression (Lee, 2020, Tee et al., 2020; C. Wang et al., 2020), medical students may have perceived a myriad of psychological stressors compared to their counterparts enrolled in other undergraduate and graduate programs. Medical students’ distress is contributed by their prevailing stressful academic pressure and preexisting higher psychological and mental health issues (Pereira, Barbosa, de Rezende, & Damiano, 2015).
The notion of having significantly higher mood disorders, anxiety disorders, suicidal ideation, and psychological distress among medical students to that of other postsecondary graduates has already been proved in a Canadian cross-sectional survey (Maser, Danilewitz, Guérin, Findlay, & Frank, 2019). Moreover, recent studies conducted among the medical students in their clinical years clearly stated the considerable ambivalence between the concerning threat of this virus and their overwhelming sense of duty and desire to contribute to the health services (James, 2020, Samuthpongtorn and Pongpirul, 2020, Ullah and Amin, 2020). Cumulatively, along with other existential stressors, this conflict can trigger psychological trauma of medical students who are already predisposed to a stressful lifestyle.
Unlike students of other background, medical students face differential obstacles like lack of adequate time, higher tests and examinations along with detachment from family, and other societal factors make the medical students more prone to poorer mental health status, according to a study in Bangladeshi context (Sadiq et al., 2019). Moreover, different incidents of attack towards healthcare professionals around the world as well as fear of assault in Bangladesh among physicians during this pandemic, might initiate the fear of assault/humiliation among the medical students (Hasan et al., 2020, McKay et al., 2020). According to a recent study, the prevalence of poor mental health status among Bangladeshi medical students is 33.5%. Particularly, depression was found in 38.9% of medical students in varying degrees, while 17.6% of students had suicidal tendency or attempted suicide at least once during their studentship (Hasan et al., 2020). All these alarming statistics call for an assessment of how the global pandemic is further affecting the mental health of medical students in this country and find out their coping strategies.
This paper aimed to determine the prevalence of anxiety and depressive symptoms and to elucidate the psychological impact of COVID-19 pandemic on Bangladeshi medical students by utilizing the Hospital Anxiety and Depression Scale (HADS) (Zigmond & Snaith, 1983). Although very few studies have been published concerning the mental health sufferings of Bangladeshi citizens (Anwar et al., 2020, Banna et al., 2020, Mamun and Griffiths, 2020, Shammi et al., 2020), to best of our knowledge, no studies have been conducted to date investigating the mental health status of Bangladeshi medical students during this pandemic.
2. Methods
2.1. Study design and participants
A cross sectional design was used. The survey was conducted between April 21 and May 10, 2020, when the government imposed social distancing policies due to the pandemic, during its initial phase in the country. The Bangladeshi medical students who were enrolled in any medical colleges, can read and understand English, and be living in Bangladesh at the time of the COVID-19 were eligible for the study. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Declaration of Helsinki. All procedures involving human participants were approved by the Ethical Review Committee, Shaheed Suhrawardy Dhaka, Bangladesh (ShSMC/Ethical/2020/12).
Sample size was calculated from prevalence estimate using following formula: , where n = number of samples; z = 1.96 for 95% confidence level (CI), p = “best guess” for prevalence and d = precision of the prevalence estimate. However, a recent study by Khan et al. reported that the 33.3% of the students had anxiety and 46.92% had mild to extremely severe depressive symptoms during COVID-19 pandemic in Bangladesh (Khan et al., 2020). We assumed that the psychological problems might be 50% among the current medical students of Bangladesh and provided that 384 samples would be enough for the present study. Assuming a 10% non-response rate, we calculated the sample size as 425.
2.2. Data collection tool
Data were collected using a structured online questionnaire created in Google form. The questionnaire had three parts: (i) demographic questions (gender, age, and marital status), (ii) COVID19-related questions (tested positive for COVID-19, media usage, home supplies, obstacles/humiliation etc.), and (iii) Hospital Anxiety and Depression Scale (HADS). HADS is a fourteen-item scale of seven items each for anxiety and depression. The ranking for each object varies from zero to three. The subscale level > 8 suggests anxiety or depression (Rishi et al., 2017). The HADS scale, designed initially to use in hospital setting only, was validated for using in the community and primary care setting (Snaith, 2003).
2.3. Data collection method
We used both convenient and snowball sampling method to recruit participants. An online survey along with the e-consent form was posted on closed social media (Facebook) groups of current medical students of Bangladesh and open request was placed by the team of investigators to fill up the form. Additionally, five volunteers from different medical institutions were employed to circulate the survey among their academic networks in addition to regular posting in above mentioned social media groups. They were instructed to be inclusive, open & circulate it periodically for a maximum reach. Email addresses of the interested participants were collected for sending them proper clarification upon request and obtaining informed consent for the reliability of the data. The study was conducted following the Checklist for Reporting Results of Internet ESurveys (CHERRIES) guidelines (Eysenbach, 2004).
2.4. Statistical analysis
All statistical analyses were carried out using SPSS (version 25.0). Frequency distribution with percentage was used to present categorical variables. Chi-square (χ2) test was used to explore the association between the study variables. Furthermore, both bivariate and multiple logistic regression models were used to find out the predictors of depressive and anxiety symptoms among Bangladeshi medical students during COVID-19 pandemic. Statistical significance level was set at p-value < 0.05 and 95% confidence interval (CI).
3. Results
Among the 425 medical students, a majority were females (62.4% [n = 265]). The students’ age ranged from 18 to 28 years, with a mean of 22 ± 1.81 years. Students were categorized into two age groups; 18–23 years and 24–28 years. The rationale behind this was to distinguish the undergraduate and post-graduate medical students and to assess if the level of anxiety and depression differs between these two groups. The prevalence and severity of anxiety among the students are shown in Fig. 1 . We found varying degrees of anxiety symptoms, including severe (11.8%), moderate (26.8%), and mild (27.3%) anxiety symptoms. The prevalence and severity of depressive symptoms are shown in Fig. 2 . Data showed varying degrees of depressive symptoms, ranging from mild (26.6%), moderately severe (20%), and severely severe (3.3%).
Fig. 1.
Prevalence and severity of anxiety among medical students during COVID-19 in Bangladesh.
Fig. 2.
Prevalence and severity of depressive symptoms among medical students during COVID-19 situation in Bangladesh.
3.1. Factors related to anxiety symptoms
Our study demonstrated that females (67.9%) suffered relatively more from anxiety symptoms than males (62.5%) (Table 1 ). The students, who were worried about getting infected by COVID-19, had more anxiety. Students with severe tension of getting COVID-19 had the highest percentage (79.6%) suffered from anxiety disorders, and the students of moderate level of tension also had a significantly higher percentage (59.9%) of anxiety disorders (p < 0.001). Almost similar findings (p = 0.001) were found in case of anxiety among the students who were worried about their family members of getting COVID-19. We also found that the students who thought of positive impact of COVID-19 situation on their life, had less anxiety than those who did not (p = 0.044). Furthermore, ‘having fear (p < 0.001) of getting assaulted or humiliated on the way to hospital or home’, ‘being agitated (p < 0.001) more easily during COVID-19 time than before’, and ‘felt agitated (p < 0.001) against human contact during the initial wave of COVID-19′ were found to be significant predictors of students’ anxiety.
Table 1.
Association between study variables and anxiety and depressive symptoms.
| Variables | Total (%) |
Anxiety |
χ2 value (p value) |
Depression |
χ2 value (p value) | |||
|---|---|---|---|---|---|---|---|---|
| No (% in row) | Yes (% in row) | No (% in row) | Yes (% in row) | |||||
| Demographic factors | ||||||||
| Age | ||||||||
| 18–23 years | 330 (77.6) | 120 (36.4) | 210 (63.6) | 3.31 (0.069) | 171 (51.8) | 159 (48.2) | 1.71 (0.191) |
|
| 24–28 years | 95 (22.4) | 25 (26.3) | 70 (73.7) | 42 (44.2) | 53 (55.8) | |||
| Gender | ||||||||
| Male | 160 (37.6) | 60 (37.5) | 100 (62.5) | 1.31 (0.253) | 91 (56.9) | 69 (43.1) | 4.69 (0.030)* | |
| Female | 265 (62.4) | 85 (32.1) | 180 (67.9) | 122 (46.0) | 143 (54.0) | |||
| Marital status | ||||||||
| Unmarried | 414 (97.4) | 142 (34.3) | 272 (65.7) | 0.24 (0.756) | 207 (50.0) | 207 (50.0) | 0.09 (1.000) | |
| Married | 11 (2.6) | 3 (27.3) | 8 (72.7) | 6 (54.5) | 5 (45.5) | |||
| Health and COVID-19 related factors | ||||||||
| Receiving treatment for mental health problems | ||||||||
| N/A | 362 (85.2) | 126 (34.8) | 236 (65.2) | 0.77 (0.725) | 187 (51.7) | 175 (48.3) | 3.27 (0.188) | |
| No | 52 (12.2) | 15 (28.8) | 37 (71.2) | 23 (44.2) | 29 (55.8) | |||
| Yes | 11 (2.6) | 4 (36.4) | 7 (63.6) | 3 (27.3) | 8 (72.7) | |||
| Previously taken treatment or support for mental health problems | ||||||||
| N/A | 349 (82.1) | 118 (33.8) | 231 (66.2) | 1.00 (0.953) | 179 (51.3) | 170 (48.7) | 4.16 (0.125) | |
| No | 50 (11.8) | 18 (36.0) | 32 (64.0) | 26 (52.0) | 24 (48.0) | |||
| Yes | 26 (6.1) | 9 (34.6) | 17 (65.4) | 8 (30.8) | 18 (69.2) | |||
| Receiving treatment for other diseases | ||||||||
| None | 390 (91.8) | 139 (35.6) | 251 (64.4) | 5.06 (0.167) | 198 (50.8) | 192 (49.2) | 1.41 (0.736) | |
| Chronic NCDs | 17 (4.0) | 4 (23.5) | 13 (76.5) | 8 (47.1) | 9 (52.9) | |||
| Lung disease | 14 (3.3) | 2 (14.3) | 12 (85.7) | 6 (42.9) | 8 (57.1) | |||
| Other Infectious diseases | 4 (0.9) | 0 (0.0) | 4 (100.0) | 1 (25.0) | 3 (75.0) | |||
| Experienced symptoms of COVID-19 | ||||||||
| Yes | 14 (3.3) | 4 (28.6) | 10 (71.4) | 0.22 (0.934) | 9 (64.3) | 5 (35.7) | 1.16 (0.602) | |
| No | 389 (91.5) | 134 (34.4) | 255 (65.6) | 193 (49.6) | 196 (50.4) | |||
| Maybe | 22 (5.2) | 7 (31.8) | 15 (68.2) | 11 (50.0) | 11 (50.0) | |||
| Ready to deal a COVID-19 positive patient | ||||||||
| Yes | 127 (29.9) | 48 (37.8) | 79 (62.2) | 1.09 (0.297) | 64 (50.4) | 63 (49.6) | 0.01 (0.941) | |
| N/A, No | 298 (70.1) | 97 (32.6) | 201 (67.4) | 149 (50.0) | 149 (50.0) | |||
| Tension of getting infected by COVID-19 | ||||||||
| No/minimal | 83 (19.5) | 37 (44.6) | 46 (55.4) | 21.21 (<0.001)** | 50 (60.2) | 33 (39.8) | 8.78 (0.012)* | |
| Moderate | 185 (43.5) | 76 (41.1) | 109 (58.9) | 98 (53.0) | 87 (47.0) | |||
| Severe | 157 (36.9) | 32 (20.4) | 125 (79.6) | 65 (41.4) | 92 (58.6) | |||
| Tensed about family members of being infected by COVID-19 | ||||||||
| No/minimal | 50 (11.8) | 20 (40.0) | 30 (60.0) | 14.35 (0.001)** | 27 (54.0) | 23 (46.0) | 3.30 (0.192) | |
| Moderate | 102 (24.0) | 49 (48.0) | 53 (52.0) | 58 (56.9) | 44 (43.1) | |||
| Severe | 273 (64.2) | 76 (27.8) | 197 (72.2) | 128 (46.9) | 145 (53.1) | |||
| Number of times check the daily news /updates | ||||||||
| ≤3 times | 214 (50.4) | 79 (36.9) | 135 (63.1) | 1.50 (0.220) | 112 (52.3) | 102 (47.7) | 0.85 (0.357) | |
| ≥4 times | 211 (49.6) | 66 (31.3) | 145 (68.7) | 101 (47.9) | 110 (52.1) | |||
| Find difficult to stay away from media (TV / Newspaper etc.) | ||||||||
| No | 126 (29.6) | 49 (38.9) | 77 (61.1) | 4.16 (0.125) | 63 (50.0) | 63 (50.0) | 1.95 (0.377) | |
| I am not sure | 62 (14.6) | 25 (40.3) | 37 (59.7) | 36 (58.1) | 26 (41.9) | |||
| Yes | 237 (55.8) | 71 (30.0) | 166 (70.0) | 114 (48.1) | 123 (51.9) | |||
| Source of news | ||||||||
| TV news (Online on Fb page, YouTube/Offline) | 291 (68.5) | 105 (36.1) | 186 (63.9) | 4.87 (0.087) | 145 (49.8) | 146 (50.2) | 2.65 (0.265) | |
| Social Media | 80 (18.8) | 19 (23.8) | 61 (76.3) | 36 (45.0) | 44 (55.0) | |||
| National/Int. news websites /Newspaper (Online/offline) | 54 (12.7) | 21 (38.9) | 33 (61.1) | 32 (59.3) | 22 (40.7) | |||
| Think COVID-19 situation has had any positive outcome or impact on life | ||||||||
| Yes | 133 (31.3) | 50 (37.6) | 83 (62.4) | 6.24 (0.044)* | 79 (59.4) | 54 (40.6) | 10.00 (<0.01)** | |
| No | 139 (32.7) | 36 (25.9) | 103 (74.1) | 56 (40.3) | 83 (59.7) | |||
| Maybe | 153 (36.0) | 59 (38.6) | 94 (61.4) | 78 (51.0) | 75 (49.0) | |||
| Have enough supplies of food in home for family to feed on | ||||||||
| Yes | 248 (58.4) | 90 (36.3) | 158 (63.7) | 3.21 (0.200) | 134 (54.0) | 114 (46.0) | 4.34 (0.114) | |
| No | 55 (12.9) | 13 (23.6) | 42 (76.4) | 22 (40.0) | 33 (60.0) | |||
| Maybe | 122 (28.7) | 42 (34.4) | 80 (65.6) | 57 (46.7) | 65 (53.3) | |||
| Fear of getting assaulted /humiliated on the way to hospital or home | ||||||||
| Yes | 88 (20.7) | 16 (18.2) | 72 (81.8) | 12.54 (<0.001)** | 40 (45.5) | 48 (54.5) | 0.97 (0.326) | |
| Not at all or N/A | 337 (79.3) | 129 (38.3) | 208 (61.7) | 173 (51.3) | 164 (48.7) | |||
| Able to give your maximum concentration on study after the pandemic | ||||||||
| No/minimal | 101 (23.8) | 31 (30.7) | 70 (69.3) | 8.56 (0.014)* | 49 (48.5) | 52 (51.5) | 2.64 (0.268) | |
| May be | 176 (41.4) | 50 (28.4) | 126 (71.6) | 82 (46.6) | 94 (53.4) | |||
| Yes | 148 (34.8) | 64 (43.2) | 84 (56.8) | 82 (55.4) | 66 (44.6) | |||
| Being agitated more easily than usually were | ||||||||
| Yes | 143 (33.6) | 22 (15.4) | 121 (84.6) | 38.63 (<0.001)** | 53 (37.1) | 90 (62.9) | 17.32 (<0.001)** | |
| Maybe | 114 (26.8) | 41 (36.0) | 73 (64.0) | 58 (50.9) | 56 (49.1) | |||
| No | 168 (39.5) | 82 (48.8) | 86 (51.2) | 102 (60.7) | 66 (39.3) | |||
| How is human contact making you feel? | ||||||||
| No change, like before | 180 (42.4) | 89 (49.4) | 91 (50.6) | 35.15 (<0.001)** | 106 (58.9) | 74 (41.1) | 15.62 (<0.001)** | |
| Agitated | 188 (44.2) | 38 (20.2) | 150 (79.8) | 74 (39.4) | 114 (60.6) | |||
| Better than before | 57 (13.4) | 18 (31.6) | 39 (68.4) | 33 (57.9) | 24 (42.1) | |||
Multivariate regression analysis reveals that female medical students had suffered more anxiety (1.6 times, 95% CI: 0.99–2.61) than males (Table 2 ). The students, who were severely (3.5-fold, 95% CI: 1.56–8.06) or moderately (1.5-fold, 95% CI: 0.72–3.14) tensed to contract SAR-CoV-2 infection, were at higher risk of suffering from anxiety, when compared with no/minimally tensed students. Students with fear of getting assaulted or humiliated on the way to hospital or home had 2.37 times (95% CI: 1.22–4.62) more likely to suffer from anxiety. Similarly, students who reported suboptimal study concentration after COVID-19 pandemic were 1.80 times (95% CI: 0.97–3.34) more likely to suffer from anxiety. Furthermore, students who agitated more easily during the COVID-19 period than before had 3.27 times (95% CI: 1.75–6.12) more likely to suffer from anxiety.
Table 2.
Odds of binary logistic regression of predictive study variables with anxiety and depressive symptoms among medical students in Bangladesh.
| Variables |
Anxiety |
Depression |
|||||||
|---|---|---|---|---|---|---|---|---|---|
|
Unadjusted estimates |
Adjusted estimates |
Unadjusted estimates |
Adjusted estimates |
||||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Age | |||||||||
| 24–28 years | 1.60 (0.96–2.66) | 0.070 | 1.54 (0.85–2.79) | 0.159 | 1.36 (0.86–2.15) | 0.192 | 1.33 (0.80–2.19) | 0.273 | |
| 18–23 years | 1.00 | 1.00 | |||||||
| Gender | |||||||||
| Female | 1.27 (0.84–1.92) | 0.254 | 1.60 (0.99–2.61) | 0.057* | 1.55 (1.04–2.30) | 0.031* | 1.78 (1.16–2.75) | <0.01** | |
| Male | 1.00 | 1.00 | |||||||
| Tension of getting infected by COVID-19 | |||||||||
| Severe | 3.14 (1.76–5.62) | <0.001** | 3.54 (1.56–8.06) | <0.01** | 2.15 (1.25–3.69) | <0.01** | 2.75 (1.27–5.96) | 0.010* | |
| Moderate | 1.15 (0.68–1.95) | 0.592 | 1.50 (0.72–3.14) | 0.279 | 1.35 (0.80–2.28) | 0.269 | 1.96 (0.94–4.06) | 0.073 | |
| No/minimal | 1.00 | 1.00 | |||||||
| Tension of getting family members infected by COVID-19 | |||||||||
| Severe | 1.73 (0.93–3.23) | 0.086 | 0.78 (0.32–1.91) | 0.586 | 1.33 (0.73–2.44) | 0.356 | 0.59 (0.25–1.41) | 0.236 | |
| Moderate | 0.72 (0.36–1.43) | 0.350 | 0.47 (0.19–1.21) | 0.119 | 0.89 (0.45–1.76) | 0.738 | 0.54 (0.22–1.33) | 0.181 | |
| No/minimal | 1.00 | 1.00 | |||||||
| COVID-19 situation has had any positive outcome or impact on life | |||||||||
| No | 1.72 (1.03–2.89) | 0.039* | 1.44 (0.79–2.63) | 0.229 | 2.17 (1.34–3.52) | <0.01** | 1.96 (1.17–3.29) | 0.011* | |
| Maybe | 0.96 (0.60–1.55) | 0.866 | 1.09 (0.62–1.91) | 0.768 | 1.41 (0.88–2.25) | 0.154 | 1.53 (0.92–2.54) | 0.104 | |
| Yes | 1.00 | 1.00 | |||||||
| Fear of getting assaulted /humiliated on the way to hospital or home | |||||||||
| Yes | 2.79 (1.56–5.01) | 0.001** | 2.37 (1.22–4.62) | 0.011* | 1.27 (0.79–2.03) | 0.326 | 1.09 (0.65–1.85) | 0.738 | |
| Not at all or N/A | 1.00 | 1.00 | |||||||
| Able to give maximum concentration on study after the pandemic | |||||||||
| No/minimal | 1.72 (1.01–2.93) | 0.046* | 1.80 (0.97–3.34) | 0.061 | 1.32 (0.79–2.19) | 0.285 | 1.23 (0.71–2.14) | 0.467 | |
| May be | 1.92 (1.21–3.05) | <0.01** | 2.11 (1.25–3.59) | <0.01** | 1.42 (0.92–2.21) | 0.114 | 1.39 (0.87–2.22) | 0.165 | |
| Yes | 1.00 | 1.00 | |||||||
| Are you agitated more easily than you usually were? | |||||||||
| Yes | 5.24 (3.04–9.05) | <0.001** | 3.27 (1.75–6.12) | <0.001** | 2.62 (1.66–4.16) | <0.001** | 1.97 (1.17–3.33) | 0.011* | |
| Maybe | 1.70 (1.04–2.78) | 0.033* | 1.46 (0.84–2.53) | 0.176 | 1.49 (0.92–2.41) | 0.102 | 1.43 (0.85–2.39) | 0.178 | |
| No | 1.00 | 1.00 | |||||||
| How is human contact making you feel? | |||||||||
| Agitated | 3.86 (2.44–6.12) | <0.001** | 2.72 (1.58–4.66) | <0.001** | 2.21 (1.45–3.35) | <0.001** | 1.71 (1.06–2.74) | 0.027* | |
| Better than before | 2.12 (1.13–3.98) | 0.020* | 2.04 (1.01–4.11) | 0.046* | 1.04 (0.57–1.91) | 0.894 | 0.88 (0.46–1.66) | 0.685 | |
| No change, like before | 1.00 | 1.00 | |||||||
3.2. Factors related to depressive symptoms
HADS depression subscale demonstrated that females (54%) suffered significantly (p = 0.03) more depressive symptoms than males (43.1%) (Table 1). The students who reported tension of getting COVID-19 had depressive symptoms. Students with severe tension of getting COVID-19 had the highest percentage (58.6%) suffered from depressive symptoms, and the students of moderate level of tension also had a significantly higher percentage (47%) of depressive symptoms (p = 0.012). We also found that the students who thought of positive impact of COVID-19 situation on their life, had fewer depressive symptoms than those who did not (40.6% vs 59.7%; p < 0.01). Depressive symptoms were found higher (p < 0.001) among the students (60.6%) who felt agitated against human contact during the initial lockdown of COVID-19. We also found that the students who agitated more easily during the COVID-19 time than before were with more depression symptoms (62.9%; p < 0.001).
Multivariate regression analysis revealed that female students were 1.8 times (95% CI: 1.16–2.75) more likely to suffer from depressive symptoms than their male counterparts (Table 2). The students who had severe and moderate tension of getting COVID-19 were 2.75 times (95% CI: 1.27–5.96) and 1.96 times (95% CI: 0.94–4.06) more likely to suffer from depressive symptoms than those with no or minimal tension. Furthermore, students who agitated more easily during the COVID-19 time than before had 1.97 times (95% CI: 1.17–3.33) more likely to suffer from depression.
4. Discussion
Medical students are susceptible to increased psychological distress compared to their contemporaries, particularly due the intensive academic curriculum (Hill, Goicochea, & Merlo, 2018). A recent meta-analysis encompassing studies of medical students estimated the global prevalence of anxiety by pooling data from 69 studies, and reported 33.8% of medical students are afflicted with anxiety worldwide, where Asian and Middle Eastern students were found to have a higher prevalence (Quek et al., 2019). COVID-19 pandemic aggravates this existing stress level much more than usual (O'Byrne, 2020). Utilizing a validated research instrument- Hospital Anxiety and Depression Scale (HADS), the present study aimed to elucidate the prevalence and factors associated with anxiety and depression symptoms among Bangladeshi medical students amidst COVID-19 pandemic. To our knowledge, this is the first study to investigate the mental health of medical students in Bangladeshi context during this pandemic.
This study demonstrated the prevalence of anxiety (65.9%) in varying degrees among Bangladeshi medical students, indicating 27.3%, 26.8%, and 11.8% students were afflicted with mild, moderate, and severe anxiety respectively during this pandemic. Depressive symptoms was comparatively prevalent to a lower extent (49.9%), where 26.6% of students scored 8–10, as having symptoms of mild depressive symptoms in HADS sub-scale. These findings are in line with another contemporary Bangladeshi study that found 63.6% and 62.9% of university students were anxious and having depressive symptoms respectively by using the DASS-21 questionnaire (Islam et al., 2020). Surprisingly, study findings of Islam et al., (2020) challenged our assumption of higher depression and anxiety prevalence in medical students; however, it is possible that COVID-19 will have a similar psychological impact on all university students. Alternatively, usage of different scales while measuring anxiety and depression level may cause variance in the study findings. In comparison to another study that estimated prevalence of depression in Bangladeshi medical students prior to the onset of pandemic, found 38.9% of students experienced depressive symptoms which is significantly lower what we found in this study (Hasan et al., 2020). This suggests a detrimental impact of COVID-19 on mental health status of medical students.
Several studies have taken place in different parts of the globe concentrating on the prevalence of psychological distress among university students during this pandemic; however, less attention has been given to medical students. The study by Cao et al. (2020) reported an overall 24.9% students in Changzhi medical college had experienced anxiety, of which, majority of the students (21.3) had mild anxiety symptoms (Cao et al., 2020). Similar results have been mentioned in another Chinese survey, with 22.1% of medical students were found to be afflicted with anxiety and 35.5% were in a state of depression (Liu et al., 2020). Alternatively, a Brazilian study applied Generalized Anxiety Disorder scale (GAD-7) and Patient Health Questionnaire (PHQ-9) and found high prevalence of moderate (46.17%) to severe (64.41%) symptoms of anxiety and depression among medical students (Sartorao Filho et al., 2020). GAD-7 scale was used in all of the above-mentioned studies; however, the disproportionate higher level of anxiety (almost doubled in Brazilian study) may be explained by the adoption of early stage integrated psychological crisis interventions targeting general population, including students, following novel corona virus outbreak in China (Li et al., 2020).
According to our findings, levels of anxiety and depression were higher amongst female medical students than male medical students, which is in compliance with the previous epidemiological research and meta-analysis (Baxter et al., 2013, Iqbal et al., 2015, Kulsoom and Afsar, 2015, Moutinho et al., 2017, Sartorao Filho and Rodrigues, 2020). However, no statistically significant association between gender and psychological distress was observed in several other studies (Cao et al., 2020; Liu et al., 2020, Quek et al., 2019).
Our study investigated the association of several novel factors with the status of anxiety and depression symptoms of medical students. For instance, students who were severely tensed of getting COVID-19 had 3.54- and 2.75-folds higher risk of suffering from anxiety and depressive symptoms respectively, compared to no/minimally tensed individuals, which is not surprising in current pandemic. Besides, evidence from Wang et al. (2020) study confirmed the association of higher DASS anxiety subscale score with higher perceived likelihood of contracting COVID-19 in general population (Cuiyan Wang et al., 2020). However, unlike other studies, worry about transmitting the virus to the family members were not found statistically significant in our study. Logistic regression showed that, students those perceived no positive impact of this pandemic in their lives were more likely to experience anxiety and depression.
Social support was found to be inversely related to medical students’ anxiety (Cao et al., 2020). In Bangladesh, however, healthcare professionals are becoming the victims of rampant ill-treatment by the society, and often being evicted from their residences by their landlords for the fear of transmitting infection to the society. Our study reported fear of getting assaulted/humiliated on the way to hospital or home were significantly correlated with a higher level of anxiety (p < 0.05). A very recent British study has confirmed the immense significance of perceived social support in reducing level of anxiety and depression, as well as improved quality of life (White & Van Der Boor, 2020). Thus, provision of effective social supports is paramount in lowering psychological stress during this global crisis.
Results from the regression analysis pointed out, students who become more agitated presently and those feel agitated while contacting to human experience elevated anxiety and depression symptoms. Agitation may have been caused by disruption of the study, newer study methods, delay in academic activities, home quarantine, and absence of interpersonal communications with peers (Cao et al., 2020, Xiao, 2020). Interventions targeting these insurmountable predisposing psychological factors of COVID-19 related anxiety and depression symptoms amongst medical students should be adopted by medical college authorities and policy makers.
4.1. Limitations of the study
Our study has several limitations. Convenient sampling method and the nature of the survey (internet-based) limits the generalizability of the survey results by generating selection bias. However, during rapidly evolving infectious disease outbreaks, an online survey could produce robust results by engaging a nationally representative population group on a specific topic of interest (Geldsetzer, 2020). Several socio-demographic and behavioral variables, such as living area, family income, living with family or alone, year of study, smoking, and substance use, were not included in the questionnaire, which may confound the study findings. However, we incorporated several unique factors, such as being worried about themselves or family members regarding getting COVID-19, their perceived feeling of any positive impact of this pandemic, impact on their study in post-pandemic period, and their current emotional status (considering being agitated), those were not delineated in other studies. Additionally, data interpretation should be done with caution, because anxiety and depression symptoms level were determined by self-reported data and subjected to response bias. Besides, pre-pandemic data is not available among this sample. Therefore, ambiguity remains if anxiety and depression are actually caused by COVID-19. Furthermore, present study only highlights but does not provide in depth information regarding preventive measures and coping strategies, which is warranted in future studies. Nonetheless, causality cannot be established due to the cross-sectional study design.
4.2. Public health implication
Despite these limitations, this study has some public health implications too. Although anxiety and depressive symptoms possess debilitating psychological impact on medical students, these mostly have garnered less attention, and are often being undiscovered and untreated in Bangladeshi context. Medical students will command the future healthcare profession; any imposed psychological threat due to changes in learning environment, restructuration of examination system, home quarantine, economic instability, and perception of not having any positive reflection of this pandemic in their lives, would unwittingly exploit their willingness to serving the nation in upcoming days. Moreover, the notion of experiencing post-traumatic stress disorder (PTSD) cannot be disregarded, which may have dire consequences for both future doctors and their patients. A study by Low et al. (2019) reported that medical and surgical resident physicians had high prevalence of burnout which suggests designing and implementing potential interventions to support future physicians to protect their mental health and well-being (Low et al., 2019).
Considering the public health implications of sound mental health status of Bangladeshi medical students, resources on how to combat pandemic-related anxiety and depression should be promoted among students. Apart from that, respective class teachers can perform primary screening, and support should be given to those who encounter moderate to severe depression and anxiety. Medical college authorities should ensure optimal alternative learning environment to continue the provision of education for every medical student. In addition, mindfulness-based therapy (Ho, Chee, & Ho, 2020) and internet cognitive behavioral therapy to treat insomnia and stress of medical students can be useful (Soh, Ho, Ho, & Tam, 2020; Zhang & Ho, 2017). Although many of the preventive measures may be perceived unachievable in Bangladeshi socio-demographic context, interventions on mitigating medical student’s psychological distress should be enforced in order to avert serious consequences in this limited resource health systems.
5. Conclusion
In conclusion, this cross-sectional study provides the baseline information on the prevalence of anxiety and depressive symptoms among Bangladeshi medical students during COVID-19 global pandemic. A substantial proportion of medical students are experiencing pandemic-induced adverse psychological impact. Given the vulnerability of medical students towards poor mental health conditions & their potential contribution in future health systems, medical colleges and health authorities should focus on addressing their psychological needs and formulate effective strategies to ameliorate medical students’ mental health status, particularly during any infectious disease outbreak.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to express their gratitude to Jannatul Ferdous, Sakib Hasan, Iftekhar Ahmed Sakib, Lubana Nasreen Tushi, Syed Ramiz Ahnaf, Al Hasnat Turab, Faria Islam Ria, Sajibur Rahman and Md Asifur Rahman for their support in collecting data. They would also like to thank all the participants for their spontaneous and voluntary participation in the study.
References
- Al-Rabiaah A., Temsah M.-H., Al-Eyadhy A.A., Hasan G.M., Al-Zamil F., Al-Subaie S.…Somily A.M. Middle east respiratory syndrome-corona virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. Journal of Infection and Public Health. 2020;13(5):687–691. doi: 10.1016/j.jiph.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anwar S., Nasrullah M., Hosen M.J. COVID-19 and Bangladesh: Challenges and how to address them. Frontiers in public health. 2020;8:154. doi: 10.3389/fpubh.2020.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banna M.H.A., Sayeed A., Kundu S., Christopher E., Hasan M.T., Begum M.R.…Khan M.S.I. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: A nationwide cross-sectional study. International Journal of Environmental Health Research. 2020;1–12 doi: 10.1080/09603123.2020.1802409. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: Address mental health care to empower society. The Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter A.J., Scott K.M., Vos T., Whiteford H.A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychological Medicine. 2013;43(5):897–910. doi: 10.1017/S003329171200147X. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L.…Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet. Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenbach G. Improving the quality of web surveys: The checklist for reporting results of internet e-surveys (CHERRIES) Journal of Medical Internet Research. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geldsetzer P. Use of rapid online surveys to assess people's perceptions during infectious disease outbreaks: A cross-sectional survey on COVID-19. J Med Internet Res. 2020;22(4) doi: 10.2196/18790. e18790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368 doi: 10.1136/bmj.m1211. m1211. [DOI] [PubMed] [Google Scholar]
- Guo Y.-R., Cao Q.-D., Hong Z.-S., Tan Y.-Y., Chen S.-D., Jin H.-J.…Yan Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Medical Research. 2020;7(1):11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan M.T., Hossain S., Gupta R.D., Podder V., Mowri N.A., Ghosh A.…Islam N. Depression, sleeping pattern, and suicidal ideation among medical students in Bangladesh: A cross-sectional pilot study. Journal of Public Health. 2020 doi: 10.1007/s10389-020-01304-0. [DOI] [Google Scholar]
- Hasan, M. T., Hossain, S., Safa, F., Anjum, A., Khan, A. H., Koly, K. N., . . . Thornicroft, G. (2020). Prevalence of anxiety and depressive symptoms among physicians during the COVID-19 pandemic in Bangladesh: a cross-sectional study. medRxiv. doi:10.1101/2020.12.08.20245829. [DOI] [PMC free article] [PubMed]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill M.R., Goicochea S., Merlo L.J. In their own words: Stressors facing medical students in the millennial generation. Medical Education Online. 2018;23(1):1530558. doi: 10.1080/10872981.2018.1530558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap. 2020;49(3):155–160. [PubMed] [Google Scholar]
- Iqbal S., Gupta S., Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. The Indian Journal of Medical Research. 2015;141(3):354–357. doi: 10.4103/0971-5916.156571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam, M., Sujan, S. H., Tasnim, R., Sikder, T., Potenza, M. N., & , & Van Os, J. (2020). Psychological responses during the COVID-19 outbreak among university students in Bangladesh. . doi:https://doi.org/10.31234/osf.io/cndz7. [DOI] [PMC free article] [PubMed]
- James A.R. Rapid Response: Mental health consequences of covid-19: Impact on medical students. BMJ. 2020;369 doi: 10.1136/bmj.m1515. [DOI] [Google Scholar]
- Khan A.H., Sultana S., Hossain S., Hasan M.T., Ahmed H.U., Sikder T. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. Journal of Affective Disorders. 2020 doi: 10.1016/j.jad.2020.07.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulsoom B., Afsar N.A. Stress, anxiety, and depression among medical students in a multiethnic setting. Neuropsychiatric Disease and Treatment. 2015;11:1713–1722. doi: 10.2147/ndt.S83577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. The Lancet Child & Adolescent Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Yang Y., Liu Z.-H., Zhao Y.-J., Zhang Q., Zhang L.…Xiang Y.-T. Progression of mental health services during the COVID-19 outbreak in China. International Journal of Biological Sciences. 2020;16(10):1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhu Q., Fan W., Makamure J., Zheng C., Wang J. Online mental health survey in a medical college in China during the COVID-19 outbreak. Frontiers in Psychiatry. 2020;11:459. doi: 10.3389/fpsyt.2020.00459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. The Lancet Child & Adolescent Health. 2020;4(5):347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low Z.X., Yeo K.A., Sharma V.K., Leung G.K., McIntyre R.S., Guerrero A.…Ho R.C. Prevalence of burnout in medical and surgical residents: A meta-analysis. International Journal of Environmental Research and Public Health. 2019;16(9) doi: 10.3390/ijerph16091479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Griffiths M.D. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian Journal of Psychiatry. 2020;51:102073. doi: 10.1016/j.ajp.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maser B., Danilewitz M., Guérin E., Findlay L., Frank E. Medical student psychological distress and mental illness relative to the general population: A Canadian cross-sectional survey. Academic Medicine. 2019;94(11):1781–1791. doi: 10.1097/acm.0000000000002958. [DOI] [PubMed] [Google Scholar]
- Matsuishi K., Kawazoe A., Imai H., Ito A., Mouri K., Kitamura N.…Mita T. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry and Clinical Neurosciences. 2012;66(4):353–360. doi: 10.1111/j.1440-1819.2012.02336.x. [DOI] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M.…Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Canadian Medical Association Journal. 2003;168(10):1245–1251. https://www.cmaj.ca/content/cmaj/168/10/1245.full.pdf Retrieved from. [PMC free article] [PubMed] [Google Scholar]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A Nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health. 2020;17(9) doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D., Heisler M., Mishori R., Catton H., Kloiber O. Attacks against health-care personnel must stop, especially as the world fights COVID-19. Lancet. 2020;395(10239):1743–1745. doi: 10.1016/s0140-6736(20)31191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moutinho, I. L., Maddalena, N. C., Roland, R. K., Lucchetti, A. L., Tibiriçá, S. H., Ezequiel, O. D., & Lucchetti, G. (2017). Depression, stress and anxiety in medical students: A cross-sectional comparison between students from different semesters. Rev Assoc Med Bras (1992), 63(1), 21-28. doi:10.1590/1806-9282.63.01.21. [DOI] [PubMed]
- O'Byrne, L. (2020). Medical students and COVID-19: the need for pandemic preparedness. Journal of Medical Ethics, medethics-2020-106353. doi:10.1136/medethics-2020-106353. [DOI] [PMC free article] [PubMed]
- Organization, W. H. (2020). Coronavirus disease (COVID-19) pandemic. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019?gclid=CjwKCAjwt-L2BRA_EiwAacX32WTycoV90M932Q8eyiWnJ_n0atJPDQ7rrPjXy2W2COs3aJB-BFZbFxoC4qsQAvD_BwE.
- Peng E.-Y.-C., Lee M.-B., Tsai S.-T., Yang C.-C., Morisky D.E., Tsai L.-T.…Lyu S.-Y. Population-based post-crisis psychological distress: An example from the SARS outbreak in Taiwan. Journal of the Formosan Medical Association = Taiwan yi zhi. 2010;109(7):524–532. doi: 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira M.A.D., Barbosa M.A., de Rezende J.C., Damiano R.F. Medical student stress: An elective course as a possibility of help. BMC Research Notes. 2015;8(1):430. doi: 10.1186/s13104-015-1399-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quek T.-T.-C., Tam W.-W.-S., Tran B.X., Zhang M., Zhang Z., Ho C.-S.-H., Ho R.-C.-M. The global prevalence of anxiety among medical students: A meta-analysis. International Journal of Environmental Research and Public Health. 2019;16(15):2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rishi P., Rishi E., Maitray A., Agarwal A., Nair S., Gopalakrishnan S. Hospital anxiety and depression scale assessment of 100 patients before and after using low vision care: A prospective study in a tertiary eye-care setting. Indian Journal of Ophthalmology. 2017;65(11):1203–1208. doi: 10.4103/ijo.IJO_436_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roma P., Monaro M., Colasanti M., Ricci E., Biondi S., Di Domenico A.…Mazza C. A 2-month follow-up study of psychological distress among Italian people during the COVID-19 lockdown. International Journal of Environmental Research and Public Health. 2020;17(21) doi: 10.3390/ijerph17218180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadiq M.S., Morshed N.M., Rahman W., Chowdhury N.F., Arafat S., Mullick M.S.I. Depression, anxiety, stress among postgraduate medical residents: A cross sectional observation in Bangladesh. Iran J Psychiatry. 2019;14(3):192–197. [PMC free article] [PubMed] [Google Scholar]
- Samuthpongtorn C., Pongpirul K. Medical students in low- and middle-income countries and COVID-19 pandemic. International Journal of Medical Students. 2020;8(1):79–81. doi: 10.5195/ijms.2020.533. [DOI] [Google Scholar]
- Sartorao Filho, C. I., Rodrigues, W. C. d. L. V., Beauchamp de Castro, R., Marcal, A. A., Pavelqueires, S., Takano, L., …, Sartorao Neto, C. I. (2020). Impact of covid-19 pandemic on mental health of medical students:A cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv, 2020.2006.2024.20138925. doi:10.1101/2020.06.24.20138925.
- Shammi M., Bodrud-Doza M., Towfiqul Islam A.R.M., Rahman M.M. COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: A case from Bangladesh. Heliyon. 2020;6(5) doi: 10.1016/j.heliyon.2020.e04063. e04063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snaith R.P. The hospital anxiety and depression scale. Health and Quality of Life Outcomes. 2003;1(1):29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh H.L., Ho R.C., Ho C.S., Tam W.W. Efficacy of digital cognitive behavioural therapy for insomnia: A meta-analysis of randomised controlled trials. Sleep Medicine. 2020;75:315–325. doi: 10.1016/j.sleep.2020.08.020. [DOI] [PubMed] [Google Scholar]
- Taha S.A., Matheson K., Anisman H. H1N1 was not all that scary: Uncertainty and stressor appraisals predict anxiety related to a coming viral threat. Stress Health. 2014;30(2):149–157. doi: 10.1002/smi.2505. [DOI] [PubMed] [Google Scholar]
- Tee M.L., Tee C.A., Anlacan J.P., Aligam K.J.G., Reyes P.W.C., Kuruchittham V., Ho R.C. Psychological impact of COVID-19 pandemic in the Philippines. Journal of Affective Disorders. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullah R., Amin S. The psychological impact of COVID-19 on medical students [Letter] Psychiatry Research. 2020;288:113020. doi: 10.1016/j.psychres.2020.113020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White R.G., Van Der Boor C. Impact of the COVID-19 pandemic and initial period of lockdown on the mental health and well-being of adults in the UK. BJPsych Open. 2020;6(5):e90. doi: 10.1192/bjo.2020.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig. 2020;17(2):175–176. doi: 10.30773/pi.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Li W., Zhang Q., Zhang L., Cheung T., Xiang Y.T. Mental health services for older adults in China during the COVID-19 outbreak. The Lancet. Psychiatry. 2020;7(4) doi: 10.1016/s2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.101990. 101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain, Behavior, and Immunity. 2020;S0889–1591(0820):30535–130533. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M.W., Ho R.C. Moodle: The cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technology and Health Care. 2017;25(1):163–165. doi: 10.3233/thc-161261. [DOI] [PubMed] [Google Scholar]
- Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatrica Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]