Abstract
Objective: During the outbreak of the COVID-19 epidemic in China, breast cancer (BC) patients and healthcare workers faced several challenges, resulting in great psychological stress. We measured the psychological status of BC patients and female nurses and compared the severity within the two groups at the peak time-point of the COVID-19 outbreak.
Methods: A total of 207 BC patients and 684 female nurses were recruited from Wuhan. They completed an anonymous questionnaire online using the most popular social media software in China, WeChat. The psychological status of BC patients and of female nurses was measured using the Chinese versions of the 9-item Patient Health Questionnaire (PHQ-9), the 7-item Generalized Anxiety Disorder scale (GAD-7), the 7-item Insomnia Severity Index (ISI), and the 22-item Impact of Event Scale-Revised (IES-R) for evaluation of post-traumatic stress disorder (PTSD). The differences between the two groups were analyzed.
Results: The scores of BC patients and frontline female nurses for the four scales were significantly higher than those of non-frontline female nurses (P < 0.001). There were similar scores between BC patients and frontline female nurses for PHQ-9, GAD-7, and IES-R (P = 0.789, P = 0.101, P = 0.158, respectively). Notably, the scores of BC patients for ISI were significantly higher than those of the frontline female nurses (P = 0.016). A considerable proportion of BC patients reported symptoms of depression (106/207, 51.2%), anxiety (130/207, 62.8%), insomnia (106/207, 51.2%), and PTSD (73/207, 35.5%), which was more severe than that of female nurses.
Conclusions: BC patients experienced great psychological pressure during the COVID-19 outbreak. The incidents of symptomatic anxiety, depression, sleep disorders, and PTSD were significantly comparable to that of frontline female nurses, and episodes of insomnia among BC participants were more serious than for frontline female nurses.
Keywords: breast cancer, female nurses, COVID-19, anxiety, depression, insomnia, post-traumatic stress disorder
Introduction
Since the end of 2019, a novel coronavirus, COVID-19, caused by the virus SARS-CoV-2, began to spread in Wuhan, China. This new disease, defined as the Coronavirus Disease 2019 (COVID-19) by the World Health Organization (WHO) on 11 February 2020, spread all over the world (1, 2). The Chinese government placed a lockdown on the epicenter city of Wuhan and quickly conducted powerful and effective measures to fight the pandemic.
All healthcare workers joined in and fought against the pandemic without hesitation. During the initial phase of the pandemic, healthcare workers faced great challenges, such as limited information about COVID-19 and effective drugs, rapidly increasing numbers of patients, and limited resources and protective supplies. At the same time, the non-COVID-19 patients had to discontinue or delay their normal therapy owing to the lockdown policies, limited medical resources, and the predicted increased risk of infection, especially for patients with cancer. Therefore, the outbreak of COVID-19 led to significant increases in the psychological burden of healthcare workers and patients with cancer, especially those with breast cancer (BC).
Our recent investigation showed that healthcare workers suffered great psychological pressure during the COVID-19 pandemic, especially frontline nurses (3). In addition, we evaluated the effects of the pandemic on the psychological status of breast cancer (BC) patients (4). However, there are few comparisons of the psychological status between different groups in the literature. Therefore, in this study, we focused on the severity of psychological problems in BC patients and compared them with that of female nurses in the epicenter of the pandemic, in Wuhan, China. We measured the psychological status of BC patients and nurses at the peak point of the COVID-19 outbreak by using the Generalized Anxiety Disorder Questionnaire (GAD-7), Patient Health Questionnaire (PHQ-9), Insomnia Severity Index (ISI), and Impact of Events Scale-Revised (IES-R) for PTSD evaluation.
Methods
Patients
BC patients from the epicenter of COVID-19 in China, Wuhan Hubei Province, were enrolled in this survey study. Female nurses from a tertiary hospital in Wuhan were selected as the control group. The study was sponsored by the Renmin Hospital of Wuhan University. All enrolled patients and nurses signed a digital informed consent form before accessing the questionnaire online. The questionnaire was designed to include demographic characteristics and four validated psychological assessment scales. The clinical features and current treatments were additionally recorded for patients with BC. The four scales included the Generalized Anxiety Disorder Questionnaire (GAD-7), Patient Health Questionnaire (PHQ-9), Insomnia Severity Index (ISI), and Impact of Events Scale-Revised (IES-R). All participants were asked to answer the questionnaire online by using the most popular social media software in China, Wechat. We issued the questionnaire in the WeChat groups from February 1 to 19, 2020, when the daily number of confirmed cases was at its peak. The daily pandemic curve showed that the number of reported cases increased rapidly after January 10, reaching the pandemic peak on February 5, after which point it declined slowly (5).
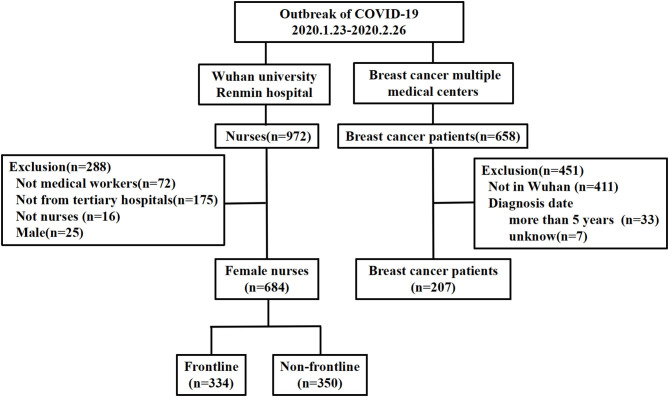
Participants who completed the entire questionnaire in <5 min or more than 60 min were excluded. BC patients whose date of diagnosis was before 2015 and male nurses were excluded. After the evaluation of questionnaires for eligibility, 891 participants were enrolled for analysis, including 207 BC patients and 684 female nurses. The female nurses were divided into a frontline and a non-frontline group. The nurses from the emergency department, fever clinics, or the medical unit for COVID-19 patients were identified as frontline nurses, and the others were non-frontline nurses. The flowchart of patient and nurse selection is shown in Figure 1. This study protocol was approved by the Institutional Ethics Committee of Renmin Hospital of Wuhan University.
Figure 1.
Flowchart of the recruitment of the patients and nurses.
Psychological Status Evaluation
We used four questionnaire scales to evaluate the psychological status of BC patients and nurses during the epidemic, including the PHQ-9, GAD-7, ISI, and IES-R. The validity and reliability of depression on the PHQ-9 scale (6, 7) and generalized anxiety on the GAD-7 scale (8, 9) have been demonstrated previously. The PHQ-9 with nine items and the GAD-7 with seven items were rated from 0 (“almost never”) to 3 (“almost always”). Based on the scores obtained on these scales, the severity of anxiety or depression for participants was divided into normal (0–4), mild (5–9), moderate (10–14), and severe (>15). The respondents whose scores were higher than 4 in PHQ-9 or GAD-7 were thought to have depressive or anxiety symptoms.
The ISI (10) is a seven-item instrument for insomnia assessment utilizing a 5-point Likert scale (0–4, not at all to extremely). The insomnia status was divided into no sleep difficulties (0–7), mild (8–14), moderate (15–21), and severe insomnia (22–28). The respondents whose scores were higher than 7 in ISI were thought to have sleep problems.
The IES-R scale (11) was used to assess Post-traumatic Stress Disorder (PTSD) symptoms based on DSM-IV criteria. Each item was rated using a five-point Likert scale ranging from 0 (not at all) to 4 (very much), for a total score ranging from 0 to 88. Participants with a score of more than 34 were defined as having PTSD.
Statistical Analysis
All statistical analyses were carried out using IBM SPSS Statistics (Version 26.0). One-way ANOVA, independent-samples T-test, and Chi-square-test were used to compare differences in the psychological status of BC patients and female nurses, based on the PHQ-9, GAD-7, ISI, and IES-R. A corresponding 95% confidence interval (CI) was calculated, and the statistical significance level was set at P < 0.05.
Results
Characteristics of BC Patients and Female Nurses in Wuhan
A total of 207 BC patients were collected in this study, including 113 cases (54.6%) within 1 year of their BC diagnosis. The majority of the patients were married (81.2%), younger than 55 years old (72.0%), had no bachelor's or higher degree (66.2%), and earned an annual income of < $15,000 (154/207; 74.9%). Most of the patients identified themselves as having presented with a good or average physical condition in the past. There were 73.4% of participants with early-stage BC disease, 59.9% who reported a history of prior breast surgery (194/207; 93.7%), and 79.7% who were advised to undergo BC treatment during COVID-19. The baseline characteristics of the BC patients are shown in Table 1.
Table 1.
The baseline characteristics of breast cancer patients and nurses in Wuhan.
| No. (207) | % | ||
|---|---|---|---|
| Age (years) | <40 | 43 | 20.8 |
| 40–55 | 106 | 51.2 | |
| >55 | 58 | 28.0 | |
| Highest level of education | Elementary school or less | 10 | 4.8 |
| Middle school | 36 | 17.4 | |
| High school | 91 | 44.0 | |
| Bachelor's degree or higher | 70 | 33.8 | |
| Marital status | Unmarried | 15 | 7.2 |
| Married | 168 | 81.2 | |
| Divorced/widowed | 24 | 11.6 | |
| Annual income (US dollars) | < $7500 | 91 | 44.0 |
| $7500–$15,000 | 64 | 30.9 | |
| $15,000–$43,000 | 46 | 22.2 | |
| >$43,000 | 6 | 2.9 | |
| General health condition by self-identification | Well | 74 | 35.7 |
| Average | 78 | 37.7 | |
| Poor | 55 | 26.6 | |
| Someone infected with COVID-19 around breast cancer patients | Yes | 24 | 11.6 |
| No | 18 | 8.7 | |
| N/A | 165 | 79.7 | |
| Breast cancer diagnosis time | Within 1 year | 113 | 54.6 |
| More than 1 year | 94 | 45.4 | |
| Breast cancer stage | Early | 124 | 59.9 |
| Advanced | 40 | 19.3 | |
| Unknown | 43 | 20.8 | |
| Molecular subtype of breast cancer | TNBC | 36 | 17.4 |
| Luminal | 55 | 26.7 | |
| HER2 | 68 | 32.8 | |
| Unknown | 48 | 23.1 | |
| History of breast cancer surgery | Yes | 194 | 93.7 |
| No | 13 | 6.3 | |
| Recommend anti-cancer therapy | Yes | 165 | 79.7 |
| No | 42 | 20.3 | |
| Discontinued anticancer therapy | Endocrine therapy | 103 | 53.4 |
| Targeted therapy | 30 | 15.5 | |
| Chemotherapy | 47 | 24.4 | |
| Radiotherapy | 5 | 2.6 | |
| Traditional Chinese medicine | 8 | 4.1 |
N/A, Not provided or not available.
A total of 684 questionnaires completed by female nurses were received. Three hundred and thirty-four (48.4%) were from the frontline. Most of the nurses had a college education (96.9%) and identified themselves as being in good or average health (96.8%) in the past. The majority of nurses (86.4%) were <40 years old. More than half of the nurses were married (53.2%). Nurses with a primary professional title constituted 57.9% and 58.3% felt uncertain about fighting against the pandemic. The baseline characteristics of the nurses are shown in Table 2.
Table 2.
The characteristics of female nurses in Wuhan during the outbreak.
| Female nurses N = 684 | Frontline female nurses N = 334 | Non-frontline nurses N = 350 | |||||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Age/years | 18–25 | 171 | 25.0 | 87 | 26.0 | 84 | 24.0 |
| 26–30 | 236 | 34.5 | 115 | 34.4 | 121 | 34.6 | |
| 30–40 | 184 | 26.9 | 102 | 30.5 | 82 | 23.4 | |
| >40 | 93 | 13.6 | 30 | 9.0 | 63 | 18.0 | |
| Marital status | Unmarried | 310 | 45.3 | 163 | 48.8 | 147 | 42.0 |
| Married | 364 | 53.2 | 166 | 49.7 | 198 | 56.6 | |
| Divorced or widowed | 10 | 1.5 | 5 | 1.5 | 5 | 1.4 | |
| Highest level of education | Junior college degree | 4 | 0.6 | 2 | 0.6 | 2 | 0.6 |
| Bachelor's degree | 648 | 94.7 | 321 | 96.1 | 330 | 94.2 | |
| Master's degree or higher | 32 | 4.7 | 11 | 3.3 | 18 | 5.2 | |
| Professional title | None | 94 | 13.7 | 46 | 13.8 | 48 | 13.7 |
| Primary | 396 | 57.9 | 204 | 61.6 | 192 | 54.9 | |
| Junior | 185 | 27.0 | 79 | 23.7 | 106 | 30.3 | |
| Senior | 9 | 1.3 | 5 | 1.5 | 4 | 1.1 | |
| Change of physical condition by self-identification | Similar | 477 | 69.7 | 214 | 64.1 | 263 | 75.1 |
| Worse | 207 | 30.3 | 120 | 35.9 | 87 | 24.9 | |
| Uncertainty of fighting against the epidemic | Yes | 399 | 58.3 | 211 | 63.2 | 188 | 53.7 |
| No | 285 | 41.7 | 123 | 36.8 | 162 | 46.3 | |
The Scores of BC Patients and Female Nurses in the Four Scales
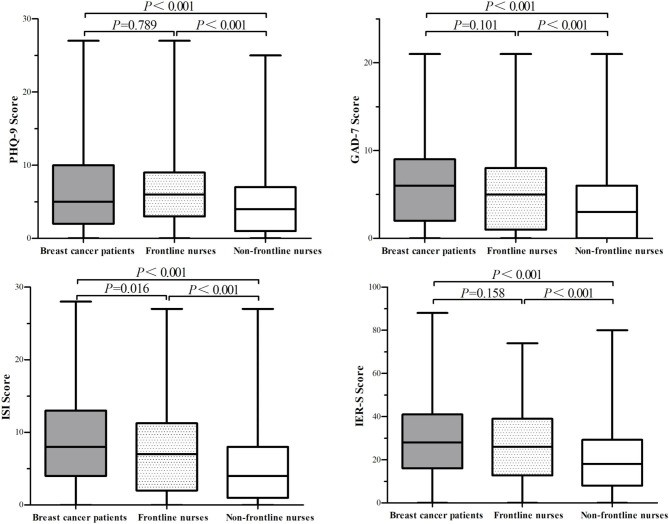
The scores of the BC patients in PHQ-9, GAD-7, ISI, and IES-R were 6.56 ± 6.044, 6.30 ± 4.879, 8.99 ± 6.359, and 29.12 ± 17.656 respectively; the scores of the frontline female nurses in PHQ-9, GAD-7, ISI, and IES-R were 6.68 ± 5.378, 6.53 ± 4.946, 7.77 ± 6.221, and 27.05 ± 17.377 respectively; the scores of the non-frontline female nurses in PHQ-9, GAD-7, ISI, and IES-R were 4.53 ± 4.305, 3.92 ± 4.127, 5.33 ± 4.378, and 20.08 ± 15.021 respectively. The psychological scores of the BC patients, frontline female nurses, and non-frontline female nurses for the four questionnaires are shown in Figure 2. Scores from the four scales administered to the BC patients were all significantly higher than for the scores of female nurses on the PHQ-9, GAD-7, ISI, and IES-R (P = 0.035, P < 0.0001, P < 0.0001, and P < 0.0001, respectively). The scores of BC patients and those of the frontline female nurses for the four scales were significantly higher than those of non-frontline female nurses (P < 0.001). There were similar scores between BC patients and frontline female nurses for PHQ-9, GAD-7, and IES-R (P = 0.789, P = 0.101, P = 0.158, respectively). Notably, the scores of BC patients on the ISI were significantly higher than those of frontline nurses (P = 0.016).
Figure 2.
The scores of the breast cancer patients, frontline nurses, and non-frontline nurses in PHQ-9, GAD-7, ISI, and IES-R. PHQ-9, Patient Health Questionnaire; GAD-7, Generalized Anxiety Disorder Questionnaire; ISI, Insomnia Severity Index; IES-R, Impact of Events Scale-Revised.
The Proportion of Psychological Problems Identified on the Four Scales for BC Patients and Female Nurses
The proportions of psychological problems identified on the four scales in BC patients and female nurses are shown in Table 3. More than half of BC patients and frontline female nurses revealed incidents of depression and anxiety. The scores associated with these factors were significantly higher than those of the non-frontline female nurses. The sleep problems for BC patients and frontline female nurses were significantly higher than those of the non-frontline female nurses. More than one-third of BC patients and frontline female nurses endured a significantly higher proportion of PTSD symptoms than did the non-frontline female nurses.
Table 3.
The abnormal proportion of four scales in nurses and breast cancer patients.
| Frontline nurses N = 334 | Non-frontline nurses N = 350 | Breast cancer patients N = 207 | ||||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | P-value | ||
| PHQ-9 | Normal | 132 | 39.5 | 190 | 54.3 | 101 | 48.8 | 0.001 |
| Abnormal | 202 | 60.5 | 160 | 45.7 | 106 | 51.2 | ||
| GAD-7 | Normal | 148 | 44.3 | 213 | 60.9 | 77 | 37.2 | <0.001 |
| Abnormal | 186 | 55.7 | 137 | 39.1 | 130 | 62.8 | ||
| ISI | Normal | 180 | 53.9 | 245 | 70.0 | 101 | 48.8 | <0.001 |
| Abnormal | 154 | 46.1 | 105 | 30.0 | 106 | 51.2 | ||
| IER-S | Normal | 223 | 66.8 | 284 | 81.1 | 134 | 64.7 | <0.001 |
| Abnormal | 111 | 33.2 | 66 | 18.9 | 73 | 35.3 | ||
P-value was calculated using the Chi-square-test.
PHQ-9, Patient Health Questionnaire; GAD-7, Generalized Anxiety Disorder Questionnaire; ISI, Insomnia Severity Index; IES-R, Impact of Events Scale-Revised.
Discussion
During the COVID-19 outbreak, rapidly rising numbers of infected cases put both the local healthcare system and the citizens in Wuhan, as the epicenter of COVID-19 in China, under tremendous stress. The Chinese government quickly took powerful and effective measures to fight against the COVID-19 pandemic, such as the lockdown of Wuhan city, integration of personal and medical resources, and the construction of Fangcang shelter hospitals (12). Under this unique circumstance, patients with cancer and healthcare workers experienced significant mental stress. In this study, we focused on the psychological status of BC patients and female nurses in Wuhan city at the peak time-point of the COVID-19 outbreak. Our survey showed that more than half of BC patients had symptoms of depression, anxiety, and insomnia, and over one-third of BC patients endured distress. The proportion of psychological problems in BC patients was comparable to that of frontline female nurses.
Because of limited medical resources, a higher risk of infection with COVID-19, and the possibility of experiencing worse outcomes after infection, the BC patients had to delay or discontinue their planned anti-cancer treatments, increasing the psychological pressure on these individuals. Our study showed that more than half of BC patients suffered from depression (51.2%), anxiety (62.8%), and sleep problems (51.2%), and over one-third of BC patients experienced PTSD symptoms (35.3%). These proportions of psychological problems were higher than those from previous reports in normal situations. BC patients already have a lot of psychological stress as a result of the diagnosis and treatment of the tumor in their bodies. Recent systematic studies have summarized the prevalence of psychological problems in BC patients (13, 14). The results showed that nearly one-third (32.2%) of BC patients experienced depression (13) and nearly 10% of patients (9.6%) had PTSD (14). However, the prevalence of depression, anxiety, insomnia, and PTSD displayed great discrepancies from previous studies (13–17), partly due to the utilization of different definitions, measurements, populations, and the timing of assessments. Therefore, we compared the severity of the psychological problems of BC patients with those of female nurses in the same place and during the same period of the pandemic.
In the face of COVID-19, healthcare workers have taken an active part in fighting the pandemic, regardless of their own safety. Many health care workers suffered great psychological pressure during the outbreak of the pandemic. Many studies have shown that healthcare workers, especially nurses, endured significantly high psychological problems during the outbreak of SARS or MERS (18–21). In our recent study, we assessed the magnitude of mental health outcomes and associated factors among 1,257 healthcare workers for COVID-19 patients in multiple regions of China (3). The results showed that a considerable proportion of healthcare workers reported experiencing symptoms of depression, anxiety, insomnia, and distress. This was especially true for frontline female nurses from the epicenter, Wuhan. We accordingly deduced that frontline female nurses in Wuhan are under the most severe psychological pressure. In this survey, more than half of frontline female nurses suffered from depression (202/334, 60.5%) and anxiety (186/334, 55.7%), and over one-third of female nurses experienced sleep problems (154/334, 46.1%) and PTSD (111/334, 33.2%). The proportions of symptomatic depression, anxiety, insomnia, and PTSD in frontline female nurses were significantly higher than those in non-frontline female nurses. However, our results showed that BC cancer patients were under psychological pressure comparable to that of the frontline female nurses at the peak of the COVID-19 outbreak in Wuhan, China. This is the first report offering a direct comparison of psychological status between patients and nurses during the pandemic. BC patients, in fact, were found to suffer worse symptoms of insomnia than female frontline nurses. These results indicate that more attention should be paid to the psychological problems experienced by BC patients and that more effective intervention measures need to be taken during future epidemics.
There were significant differences in age, marital status, and levels of education between the BC patients and female nurses. They were all women living in Wuhan, who had to go to hospitals while being at a greater risk of infection with COVID-19. Nurses are at the forefront of fighting the pandemic, and their psychological state easily attracts public attention. By comparing the psychological status of BC patients with that of nurses, we were able to obtain a greater understanding of the psychological state of the BC patients. It is important to pay attention to the psychological status of people with chronic illnesses during the outbreak of a pandemic.
During the outbreak, a number of modifications to standard treatment paradigms were implemented for BC patients. However, in addition to obtaining support through online or offline services from professional health care workers (22), necessities from social volunteers, BC patients also need to receive more support from their families. This is crucial because most remained at home during the pandemic. Several reports have demonstrated the importance of family support for patients. A prospective study with a long-term follow-up for patients showed that family support was associated with both low levels of, and quick improvement from, depression (23). For BC patients aged more than 55 years, family support from adult children might decrease their levels of anxiety and depression (24). Kamen et al. (25) showed that family support was related to less severe insomnia at baseline in BC patients. Additionally, one previous study demonstrated that family support could avoid or alleviate certain mood difficulties in BC patients in the Chinese population (26). Therefore, people need to be educated regarding the importance of providing support for BC family members, especially during epidemic outbreaks.
We acknowledge some shortcomings in our study. First, our study is a cross-sectional study that only extracts data from one point in time. The changes in the psychological status of BC patients should be investigated at different periods of the pandemic. Second, the sample size of BC patients was small. Third, the direct comparison of psychological pressures between BC patients and nurses might not be appropriate because of different influencing factors in the two distinct groups. However, our findings indicated that when BC patients were forced to delay or discontinue treatment due to the pandemic, their psychological pressures increased greatly. The differences in psychological status among other populations, such as the normal population, BC patients more recently diagnosed from other areas, and patients with other chronic diseases, should be evaluated in future. Moreover, effective measures for alleviating the psychological pressures of BC patients, both during and after the pandemic, should be investigated.
Conclusions
In summary, our study showed that BC patients were under great psychological pressure as compared to frontline female nurses in the COVID-19 epicenter, Wuhan, China. BC patients suffered worse incidents of insomnia than frontline female nurses who treated COVID-19 patients. These results indicate that effective measures should be taken to alleviate the psychological problems of BC patients during pandemics. The importance of family support in relieving psychological stress in these patients is also emphasized.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Ethics Committee of Renmin Hospital of Wuhan University. The ethics committee waived the requirement of written informed consent for participation.
Author Contributions
QC: validation, formal analysis, writing—original draft, and visualization. ZC: conceptualization, methodology, validation, formal analysis, resources, data curation, and supervision. ZL: methodology, project administration, and funding acquisition. JL: formal analysis and investigation. SS: investigation, resources, and project administration. CC and GW: conceptualization, writing-review and editing, visualization, supervision, and funding acquisition. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Footnotes
Funding. This research was supported by grants from the Fundamental Research Funds for the Central Universities (2042019kf0229), Medical Science Advancement Program of Wuhan University (TFLC2018001), the National Key R&D Program of China (2018YFC1314600), and the Chinese Society of Clinical Oncology (CSCO) Foundation (No: Y-SY201901-0189).
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO WHO Virtual Press Conference on COVID-19. Available online at: https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2 (accessed March 11, 2020).
- 3.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, Cesar Augusto SM, Feng H, Wang L, Zhang P, Xu Y, et al. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clin Breast Cancer. (2020) 20:E651–62. 10.1016/j.clbc.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team . The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. (2020) 41:145–51. 10.3760/cma.j.issn.0254-6450.2020.02.003 [DOI] [PubMed] [Google Scholar]
- 6.Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the patient health questionnaire (PHQ-9). J Affect Disord. (2004) 81:61–6. 10.1016/S0165-0327(03)00198-8 [DOI] [PubMed] [Google Scholar]
- 7.Cameron IM, Crawford JR, Lawton K, Reid IC. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract. (2008) 58:32–6. 10.3399/bjgp08X263794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swinson RP. The GAD-7 scale was accurate for diagnosing generalised anxiety disorder. Evid Based Med. (2006) 11:184. 10.1136/ebm.11.6.184 [DOI] [PubMed] [Google Scholar]
- 9.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 10.Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep (Basel). (2011) 34:601–8. 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale—revised. Behav Res Ther. (2003) 41:1489–96. 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- 12.Chen SC, Zhang ZJ, Yang JT, Wang J, Zhai XH, Bärnighausen T, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. (2020) 395:1305–14. 10.1016/S0140-6736(20)30744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pilevarzadeh M, Amirshahi M, Afsargharehbagh R, Rafiemanesh H, Hashemi SM, Balouchi A. Global prevalence of depression among breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. (2019) 176:519–33. 10.1007/s10549-019-05271-3 [DOI] [PubMed] [Google Scholar]
- 14.Wu X, Wang J, Cofie R, Kaminga AC, Liu A. Prevalence of posttraumatic stress disorder among breast cancer patients: a meta-analysis. Iran J Public Health. (2016) 45:1533–44. [PMC free article] [PubMed] [Google Scholar]
- 15.Tsaras K, Papathanasiou IV, Mitsi D, Veneti A, Kelesi M, Zyga S, et al. Assessment of depression and anxiety in breast cancer patients: prevalence and associated factors. Asian Pac J Cancer Prev. (2018) 19:1661–9. 10.22034/APJCP.2018.19.6.1661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fleming L, Randell K, Stewart E, Espie CA, Morrison DS, Lawless C, et al. Insomnia in breast cancer: a prospective observational study. Sleep. (2019) 42:zsy245. 10.1177/2047487312460020 [DOI] [PubMed] [Google Scholar]
- 17.Mehnert A, Brähler E, Faller H, Härter M, Keller M, Schulz H, et al. Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol. (2014) 32:3540–6. 10.1200/JCO.2014.56.0086 [DOI] [PubMed] [Google Scholar]
- 18.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci. (2004) 359:1117–25. 10.1098/rstb.2004.1483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. (2004) 170:793–8. 10.1503/cmaj.1031077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oh N, Hong N, Ryu DH, Bae SG, Kam S, Kim KY. Exploring nursing intention, stress, and professionalism in response to infectious disease emergencies: the experience of local public hospital nurses during the 2015 MERS outbreak in South Korea. Asian Nurs Res (Korean Soc Nurs Sci). (2017) 11:230–6. 10.1016/j.anr.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JS, Lee EH, Park NR, Choi YH. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: a cross-sectional study. Arch Psychiatr Nurs. (2018) 32:2–6. 10.1016/j.apnu.2017.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu BL, Ma F, Wang JN, Fan Y, Mo HN, Xu BH. Health management of breast cancer patients outside the hospital during the outbreak of 2019 novel coronavirus disease. Zhonghua Zhong Liu Za Zhi. (2020) 42:E002. 10.3760/cma.j.cn112152-20200221-00110 [DOI] [PubMed] [Google Scholar]
- 23.Kamen C, Cosgrove V, McKellar J, Cronkite R, Moos R. Family support and depressive symptoms: a 23-year follow-up. J Clin Psychol. (2011) 67:215–23. 10.1002/jclp.20765 [DOI] [PubMed] [Google Scholar]
- 24.Maly RC, Umezawa Y, Leake B, Silliman RA. Mental health outcomes in older women with breast cancer: impact of perceived family support and adjustment. Psycho-oncology. (2005) 14:535–45. 10.1002/pon.869 [DOI] [PubMed] [Google Scholar]
- 25.Kamen C, Garland SN, Heckler CE, Peoples AR, Kleckner IR, Cole CL, et al. Social support, insomnia, and adherence to cognitive behavioral therapy for insomnia after cancer treatment. Behav Sleep Med. (2019) 17:70–80. 10.1080/15402002.2016.1276019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Su JA, Yeh DC, Chang CC, Lin TC, Lai CH, Hu PY, et al. Depression and family support in breast cancer patients. Neuropsychiatr Dis Treat. (2017) 13:2389–96. 10.2147/NDT.S135624 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.