Abstract
Objective:
To determine the value of a traditional (easy to implement) group-based intervention program on both static and dynamic postural control in children with Developmental Coordination Disorder (DCD).
Methods:
Sway and stability indices were measured with the Clinical Test of Sensory Integration in Balance (CTSIB) and efficiency of goal-directed movement was measured during a Limits-of-Stability (LoS) task, before and after the intervention program. The intervention involved a total of 10 one-hour group sessions, administered once per week for 10 weeks.
Results:
Results indicated significant group increases in dynamic postural control (p < .05). These results suggest it is possible to improve dynamic postural control in this population. This type of intervention does not require any expensive materials, it is feasible, and easy-to-implement to a group of children.
Conclusion:
We conclude that this simple form of intervention involving fun group activities can significantly improve dynamic postural control in children with DCD.
Keywords: Developmental Coordination Disorder, postural control, balance, intervention, group-based, training, children
Developmental Coordination Disorder (DCD) is defined as a neurodevelopmental, chronic disorder characterized by low motor proficiency, which significantly affects activities of daily living and academic achievement1. Of these, poor balance ability is a major concern, since the combination of postural and motor control are necessary in order to effectively navigate and participate in their environment2. Static postural control is essential in daily activity and commonly evaluated in clinical settings3, however, individuals utilize dynamic control more often in functional tasks. In addition, there is consensus that improving postural control can significantly help with children’s participation and efficiency in several activities4.
While several studies have tested the feasibility and efficiency of postural control training programs in children with DCD5–6, a great deal of concern remains regarding feasibility and cost of programming, and the search for engaging, effective, and easily-implemented intervention programs continues. One possibility to address these concerns is the use of group-based interventions. When comparing gains in motor ability after an 8-week intervention program done individually or as a group, a study found that the gains were similar, and group-based training may be the preferred treatment option due to cost savings7. Another group-based intervention study determined that children with DCD improved motor coordination and physical ability after 8 weeks, and also improved in non-trained tasks such as handwriting8. In addition, a study found that motor skill improvements happened regardless of the group size9. Therefore, group-based interventions enable programs to offer more sessions per child to a larger number of children, without requiring significant additional resources10.
Therefore, the aim of the present study was to test the feasibility and efficiency of a group-based intervention program on static and dynamic postural control of children with DCD. The intervention focused on activities mostly designed to practice postural control in a group setting. Specifically, we measured sway and stability indices of the Clinical Test of Sensory Integration in Balance (CTSIB) and the efficiency of goal-directed movement during a limits-of-stability task (LoS) before and after the intervention program. Our secondary aim was to determine whether scores on the Balance subscale of a motor ability assessment were related to Age or to performance on the CTSIB and LoS tasks. We expected to see improvements in both static and dynamic postural control due to participation in the program, and to find an association between the balance subscales and performance on the tasks.
Method
Participants
Twelve children (11 males, 1 female) between the ages of 7 and 11 years participated in the study. Inclusion criteria for the study involved a diagnosis of DCD (or Dyspraxia, a term that is not used in the DSM-5 but sometimes used in clinical settings) and ages between 7–12 years. Exclusion criteria involved the presence of other diagnoses that could potentially affect the results (e.g., Autism Spectrum Disorders) and participation in sports (during the intervention program). In addition, participants were asked to not participate in any therapy involving motor skills during the program. Table 1 contains characteristics of the participants. We confirmed the DCD diagnosis via the Movement Assessment Battery for Children, 2nd ed. (MABC-2)11 [Criterion A], and a parent-report of functional impact via the Developmental Coordination Disorder Questionnaire (DCDQ)12 [Criterion B]. In addition, parents reported no other medical conditions that excluded the diagnosis of DCD were present in their children [Criterion D]. Criterion C was not formally assessed. The experimental protocol was approved by the Institutional Review Board (IRB) for the ethical treatment of human subjects. Parents signed consent forms, and children provided verbal and written assent.
Table 1.
Participant characteristics
| Participant | Age | Gender | Diagnoses | MABC – Total % | MABC – Bal % |
|---|---|---|---|---|---|
| 1 | 10 | M | DCD, ADHD, Dyslexia | 5 | 2 |
| 2 | 8 | M | DCD, ADHD, OCD | 0.1 | 0.1 |
| 3 | 7 | F | DCD, Dyslexia | 2 | 5 |
| 4 | 9 | M | DCD | 0.1 | 0.1 |
| 5 | 7 | M | DCD, Dysgraphia | 2 | 1 |
| 6 | 8 | M | DCD (Dyspraxia), SPD | 2 | 2 |
| 7 | 7 | M | DCD | 1 | 0.5 |
| 8 | 9 | M | DCD, ADHD | 1 | 1 |
| 9 | 9 | M | DCD, ADHD | 1 | 2 |
| 10 | 11 | M | DCD (Dyspraxia), ADHD | 2 | 2 |
| 11 | 10 | M | DCD | 2 | 9 |
| 12 | 10 | M | DCD, Dysphagia | 0.5 | 5 |
DCD: Developmental Coordination Disorder
ADHD: Attention Deficit Hyperactivity Disorder
OCD: Obsessive Compulsive Disorder
SPD: Sensory Processing Disorder
Measures
During the pre- and post- tests, each participant stood on a force plate embedded in a 21.25 inch wide by 19.00 inch long stationary platform and connected to a 12.1 inch color LCD display with 800×600 resolution (BioSway, Biodex Corp., Shelby, NY). The BioSway collected data about a participant’s Center of Pressure (CoP) during a static and a dynamic postural control task. The static postural control task (CTSIB) involved standing on a platform with feet shoulder-width apart for 30 seconds each with eyes open (EO), eyes closed (EC), and eyes open while the participant’s head was enclosed in a translucent paper dome 36” in diameter (Dome). These measures (e.g., CoP data collected from a force plate) been validated against other common clinical assessments of balance13 and used extensively in other clinical populations.
The dynamic postural control task (LoS) involved standing on a platform with feet shoulder-width apart and moving a user-controlled object on the screen to reach static targets as quickly and accurately as possible. The targets were in 9 locations (8 surrounding the participant’s center position, and one in the middle). The task difficulty was set to easy, meaning that targets were located at 25% of the limit of stability: the posterior target required 2 degrees of angular displacement, the posterior lateral targets required 3 degrees, and all remaining targets required 4 degrees. Each target flashed to cue movement, and the participant’s objective was to lean to reach the target, before returning to center. This task has shown acceptable reliability and construct validity in a prior study with adolescents14.
Procedures
Participants completed the pre- and post-intervention assessments within one week of the beginning and end of the intervention. The group-based motor intervention program involved a total of 10 one-hour sessions administered once per week for 10 weeks. Nine participants attended 100% of the sessions, while three participants missed one session, attending 90% of the program. Two trained professionals in kinesiology delivered the sessions, while several kinesiology students helped the children perform the activities. The sessions required interaction among participants, and focused on activities involving upper-body coordination, postural control, and fine-motor skills. About half (30 min) of the session was dedicated to dynamic postural control activities, and a detailed program was implemented based on developmentally appropriate activities and motor goals for the participants. If a participant was not able to perform one activity, adaptations were made so the activity could be practiced. Examples of postural control intervention activities are described in the Appendix at the end of this article.
Data analysis
CTSIB outcome measures included Stability Index (average excursion from center) and Sway Index (standard deviation of stability index, or how much they sway). We calculated the Sway and Stability Index for each condition of the CTSIB and averaged across the three conditions. The primary outcome measure of the LoS task is the Control Score, a measure of the efficiency of a goal-directed movement. We calculated a Control Score for the LoS task for each target position and averaged across all targets.
A dependent-samples t-test was used to identify differences between pre- and post-intervention performance on all variables of the CTSIB and LoS tasks. In addition, we used a Pearson correlation analysis to determine whether scores on the Balance subscale of the MABC-2 were related to Age or to performance on the CTSIB and LoS tasks.
Results and Discussion
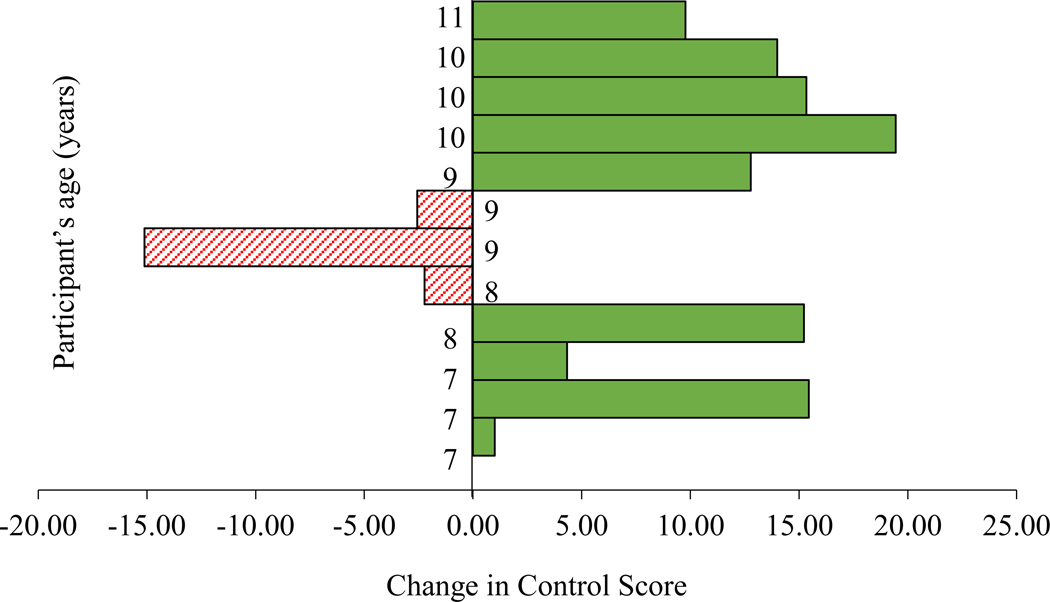
A dependent samples t-test indicated no significant improvements in static postural control as measured by the CTSIB Sway Index, t(11) = −.191, p > .05; or for the CTSIB Stability Index, t(11) = −.607, p > .05, overall or in any of the individual conditions (EO, EC, Dome). However, dynamic postural control as measured by the LoS Control Score improved significantly post-intervention, t(11) = −2.45, p = .03 (Pre-intervention: 31.96±7.15; Post-intervention: 39.25±13.52). Figure 1 depicts the individual pre- and post-intervention Control Scores for the LoS task expressed as change scores (9 participants improved, 3 did not). Treatment-responders’ performance improved 3–37% post-intervention (Mean Change = 26%) with all but one treatment-responder improving 18% or more (Median Change = 30%). Pearson correlation analyses revealed significant correlations between Age and post-intervention with the LoS Control Score (r = .60, p < .05), and between Age and both pre- and post-intervention with the CTSIB Sway Indexes (pre-intervention: r = −.66, p < .05; post-intervention: r = −.66, p < .05). The Balance subscale of the MABC-2 assessment was not significantly associated with Age or performance on the CTSIB or LoS tasks.
Figure 1.
Pre- to post intervention change in Limits-of-Stability Control Score
Using a novel approach to outcome assessment, we determined that the group-based intervention was effective in improving dynamic postural control in this group of children with DCD. These results extend the previous literature, and add to the current body of knowledge by establishing that a simple, traditional, and feasible group-based intervention is effective and potentially a more sustainable type of intervention for this population.
The Limits of Stability task assessed participants’ dynamic postural control skills, or their ability to intentionally shift their center of pressure to move a user-controlled object to a static target. Given that the majority of the tasks in the group-based motor intervention involved dynamic postural control, it is not surprising that we observed improvements in performance on this test post-intervention. Activities targeting dynamic postural control comprised approximately 50% of the program sessions/duration. In contrast, static postural control was not a primary focus of the tasks in the program. While we anticipated that there might be carryover effects of practice with dynamic postural control activities into the domain of static postural control, it appears that for most children, that was not the case. This suggests that motor interventions must work on the specific type of postural control that needs to be improved.
Another aspect of these results is associated with the lack of relationship between the MABC-2 and the LoS scores. In general, most studies that use the MABC-2 as the main assessment for intervention outcomes have detected improvements in motor skills. For example, significant improvements after a Wii-based training program on the Balance scores of the test have been found15. However, the authors noted no transfer effects of the intervention on balance-related skills, which limits the generalization of this effect. Tests that are more adapted to the task-specific training, such as the LoS, can be more sensitive to detect changes especially in the domain of dynamic postural control.
It is important to note that other types of interventions for children with DCD have also shown positive, significant results. However, our results add to the literature by demonstrating that a simple, more “traditional” approach involving fun group activities that engage a child’s balance and also promote interaction with other children can significantly improve dynamic postural control. It is possible that these interventions may be more scalable and accessible, as they demand little resources in comparison to other forms of intervention that require technological or other type of expensive equipment. It is also likely that these interventions are sustainable, and children can enjoy these activities for many years in a row.
These results extend previous work by establishing that it is possible to improve postural control in this population, and most importantly, they demonstrate that easily-implemented, group-based interventions are effective. They also extend previous work by offering a precise, quantifiable approach to evaluating response to treatment using a system that is portable and user-friendly, in contrast to common assessments that rely on subjective observation. The three participants who did not improve in static or dynamic postural control post-intervention were relatively younger (8 and 9 years old), and did not share other clinical features (e.g., co-occurring diagnoses or medication use). We can speculate that participation in group-based interventions require a specific level of executive functioning ability (e.g., goal maintenance, attention) in order for participants to benefit from activities in this type of setting, which comes as a result of development and maturation. This should be tested in future studies, as executive functioning has been determined to be impaired in children with DCD16.
Two important limitations of the present study are the lack of control group, small sample size, and of assessment beyond the post-test to verify long-term retention of improvements in dynamic postural control among treatment-responders. We were also not able to establish whether these improvements transferred to real life skills, or if they were isolated to the LoS task; although, it is worth noting that dynamic postural control has a demonstrated relationship to activities of daily living. In future work, it would be valuable to test response to intervention using both clinical (e.g., MABC-2) or functional (e.g., DCD-Q) measures of postural control in addition to the direct measurements collected in this study.
In conclusion, this brief report indicates improvements in dynamic postural control after a group-based intervention program (measured by the LoS task). These results extend previous findings denoting the potential for improving postural control in children with DCD, and add to the body of literature by demonstrating that a group-based, feasible, and easy-to-implement type of intervention can significantly improve dynamic postural control in this population.
Acknowledgments:
We would like to thank all students and Research Assistants involved in the intervention and data collection. We would also like to thank the families and children for their time and participation.
Funding: National Institutes of Health (KL2-TR001103; K01-MH107774)
Appendix: Activities used for Dynamic Postural Control
| Activity Category | Description |
|---|---|
| Walking |
Balance Maze: Children go through a maze while balancing on various items (domes and pool noodles), then walk heel to toe on taped lines. Balance Tree: Children walk heel to toe along a taped line and place objects at the end of each segment. Heel to Toe Walking: Children are paired into groups and each group walks side by side. Limbo: Children attempt to go under a limbo stick while keeping both feet on the ground. Walk the Line: Children walk along a variety of lines/paths that vary in length and width. Dangerous Paths: Children do an obstacle course that involves walking/balancing on dots, walking heel to toe on a line, and hopping on one foot. |
| Hopping/Skipping |
Zig Zag Hopping: Children try to hop on one foot down a zig zag path. Hop Scotch: Children throw a bean bag onto taped squares in the shape of a traditional hop scotch. Then, they have to hop through the squares and land within the square where the bean bag landed. Rainbow Hop: Children hop or walk across colorful domes that are shaped like a rainbow. Adventure: Children, with a ball between their legs, hop along a path on both feet without dropping the ball. |
| With an Object |
Sit and Stand: Children hold a side of a hula hoop and attempt to sit and stand without letting the hula hoop touch the ground. Jungle Trail: Children attempt to balance a bean bag on their head while walking along a variety of paths (wavy, zig zag, or straight). Worm in Tunnel: Children take turns stepping inside of a hula hoop, squatting, and then pulling the hula hoop over their head. Bean Bag Balance: Children place a bean bag on their foot and try to keep it balanced as they lift their foot into the air in front of their body. One Legged Noodle Pick Up: Children start with a pool noodle on one side of their body and then attempt to balance on one leg while bending over to pick up the noodle. Pin the Tail on the Bunny: Children are semi-blindfolded, spun around 3 times, and then attempt to place a tail on a paper bunny. Marbles and Balance Beam: Children have a spoon in their mouth and balance a marble on the spoon. Then they walk along various lines while keeping the marble on the spoon. Potholes: Children step over, into, and then back over several hula hoops which are positioned horizontally on top of tall orange cones. They attempt to not knock over any of the hula hoops Figure Skating: Children step onto paper plates and slide their feet along a designated path around cones. |
| With a Partner |
Acid River: Children hold hands to make it to the opposite end of the dots/cones. If a child steps into the ‘acid river’, they have to go back and start over. Bean Bag Pass: Children stand on two stepping stones and pass a bean bag to a partner. Group Sit and Stand: Children get in a large circle with their arms locked and attempt to sit and stand as a group without letting go of each other’s arms. Tip Toeing Partners: Each group of two children have to move together, while holding a pool noodle. They are instructed to walk on their toes. One child walks forwards while the second walks backwards. Airlock game: Children have their ankles tied together with a bandana in order to form one long line. One child steps into and then out of a hula hoop causing the child attached to them to follow the same movement. Bean Bag Balance Relay: Children stand next to 2 sets of cones that are staggered across the floor. The first child places a bean bag on their head, walks to the next child without having the bean bag fall. Then the child places the bean bag on the next child’s head. Flower Twister: Children attempt to place their hand(s) and feet on the twister mat according to the directions given (i.e. right foot on pink flower). Lateral Walking: Children are paired into groups and positioned back to back. While walking, they pass a ball to each other by rotating their trunk. |
References
- 1.American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th ed American Psychiatric Association, Washington, DC, 2013. [Google Scholar]
- 2.Miller H, Caçola P, Sherrod G, Bugnariu N. Children with Autism Spectrum Disorder, Developmental Coordination Disorder, and typical development differ in characteristics of dynamic postural control: a preliminary study. Gait Posture. 2019; 67:9–11. doi: 10.1016/j.gaitpost.2018.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pavao SL, Nunes GS, Santos AN, Rocha, NACF. Relationship between static postural control and the level of functional abilities in children with cerebral palsy. Braz J Phys Ther. 2014; 18(4): 300–307. doi: 10.1590/bjpt-rbf.2014.0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smits-Engelsman B, Vinçon S, Blank R, Quadrado VH, Polatajko H, Wilson PH. Evaluating the evidence for motor-based interventions in Developmental Coordination Disorder: A systematic review and meta-analysis. Res Dev Disabil. 2018; 74: 72–102. doi: 10.1016/j.ridd.2018.01.002 [DOI] [PubMed] [Google Scholar]
- 5.Fong SSM, Tsang WWN, Ng GYF. Taekwondo training improves sensory organization and balance control in children with Developmental Coordination Disorder: A randomized controlled trial. Res Dev Disabil. 2012; 33(1):85–95. doi: 10.1016/j.ridd.2011.08.023 [DOI] [PubMed] [Google Scholar]
- 6.Jelsma D, Geuze RH, Mombarg R, Smits-Engelsman BCM. The impact of Wii Fit intervention on dynamic balance control in children with probable Developmental Coordination Disorder and balance problems. Hum Mov Sci. 2014; 33:404–418. doi: 10.1016/j.humov.2013.12.007 [DOI] [PubMed] [Google Scholar]
- 7.Hung WW, Pang MY. Effects of group-based versus individual-based exercise training on motor performance in children with developmental coordination disorder: A randomized controlled pilot study. J Rehabil Med. 2010; 42(2):122–128. doi: 10.2340/16501977-0496 [DOI] [PubMed] [Google Scholar]
- 8.Farhat F, Hsairi I, Baati H, Smits-Engelsman BC, Masmoudi K, Mchirgui R, Triki C, Moalla W. The effect of a motor skills training program in the improvement of practiced and non-practiced tasks performance in children with Developmental Coordination Cisorder (DCD). Hum Mov Sci. 2016; 46:10–22. doi: 10.1016/j.humov.2015.12.001 [DOI] [PubMed] [Google Scholar]
- 9.Caçola P, Romero M, Ibana M, Chuang J. Effects of two distinct group motor skill interventions in psychological and motor skills of children with developmental coordination disorder: a pilot study. Disabil Health J. 2016; 9(1):172–8. doi: 10.1016/j.dhjo.2015.07.007 [DOI] [PubMed] [Google Scholar]
- 10.Caçola P, Ibana M, Romero M, Chuang J. The effectiveness of a group motor skill intervention program in children with Developmental Coordination Disorder: Program duration matters. Internet J Allied Health Sci Pract. 2016; 14(1). [DOI] [PubMed] [Google Scholar]
- 11.Henderson SE, Sugden DA, Barnett AL, editors. Movement assessment battery for children - second edition [MABC-2], 2nd ed London, The Psychological Corporation, 2007. [Google Scholar]
- 12.Wilson BN, Crawford SG, Green D, Roberts G, Aylott A, Kaplan B. Psychometric properties of the revised Developmental Coordination Disorder Questionnaire. Phys Occup Ther Pediatr. 2009; 29:182–202. doi: 10.1080/01942630902784761 [DOI] [PubMed] [Google Scholar]
- 13.Dawson N, Dzurino D, Karleskint M, Tucker J. Examining the reliability, correlation, and validity of commonly used assessment tools to measure balance. Health Sci Rep. 2018; 1:e98. doi: 10.1002/hsr2.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alsalaheen B, Haines J, Yorke A, Broglio SP. Reliability and construct validity of limits of stability test in adolescents using a portable forceplate system. Arch Phys Med Rehabil. 2015; 96(12):2194–2200. doi: 10.1016/j.apmr.2015.08.418 [DOI] [PubMed] [Google Scholar]
- 15.Mombarg R, Jelsma D, Hartman E. Effect of Wii-intervention on balance of children with poor motor performance. Res Dev Disabil. 2013; 34:2996–3003. doi: 10.1016/j.ridd.2013.06.008 [DOI] [PubMed] [Google Scholar]
- 16.Leonard HC, Bernardi M, Hill EL, Henry LA. Executive functioning, motor difficulties, and Developmental Coordination Disorder. Dev Neuropsychol. 2015; 40:201–15. doi: 10.1080/87565641.2014.997933 [DOI] [PubMed] [Google Scholar]