Abstract
Staphylococcus capitis is a coagulase-negative staphylococcus that has been described primarily as causing bloodstream infections in neonatal intensive care units (NICUs), but has also recently been described in prosthetic joint infections (PJIs). The multidrug-resistant S. capitis subsp. urealyticus clone NRCS-A, comprising three sublineages, is prevalent in NICUs across the world, but its impact on other patient groups such as those suffering from PJIs or among adults planned for arthroplasty is unknown. Genome sequencing and subsequent analysis were performed on a Swedish collection of PJI isolates (n = 21), nasal commensals from patients planned to undergo arthroplasty (n = 20), NICU blood isolates (n = 9), operating theatre air isolates (n = 4), and reference strains (n = 2), in conjunction with an international strain collection (n = 248). The NRCS-A Outbreak sublineage containing the composite type V SCCmec-SCCcad/ars/cop element was present in PJIs across three Swedish hospitals. However, it was not found among nasal carrier strains, where the less virulent S. capitis subsp. capitis was most prevalent. The presence of the NRCS-A Outbreak clone in adult patients with PJIs demonstrates that dissemination occurs beyond NICUs. As this clone has several properties which facilitate invasive infections in patients with medical implants or immunosuppression, such as biofilm forming ability and multidrug resistance including heterogeneous glycopeptide-intermediate susceptibility, further research is needed to understand the reservoirs and distribution of this hospital-associated pathogen.
Subject terms: Bacterial genetics, Clinical microbiology, Infectious diseases, Bacterial infection
Introduction
Prosthetic joint infection (PJI) is a dreaded complication of arthroplasty, resulting in considerable suffering for the patient and increased costs for healthcare providers1,2. Since the incidence of PJIs appears to be increasing1,3, there is a need for efforts to improve our knowledge in this field regarding prevention, diagnosis, and treatment4. Staphylococci are the predominant cause of PJIs. Staphylococcus aureus is the most common, followed by Staphylococcus epidermidis and Staphylococcus capitis5, with the latter consisting of two subspecies: subsp. capitis and subsp. urealyticus. These three staphylococci differ regarding the presence of virulence factors and multidrug resistance (MDR), as methicillin and rifampin resistance are far less prevalent in S. aureus and S. capitis than in S. epidermidis6–8. Despite this, recent publications have raised concerns about the outcome after debridement, antibiotics, and implant retention (DAIR) in PJIs caused by S. aureus6,8,9. There are only few clinical reports on bone and joint infections caused by S. capitis10,11, and the clinical characteristics of PJIs caused by S. capitis have only recently been described. One study showed that 70% of infections were cured following DAIR, and the all-cause 12-month mortality was ≤ 5%7. It has been suggested that there are differences in biofilm formation and prevalence of MDR between the two S. capitis subspecies12.
Most reports on S. capitis focus on its ability to cause late-onset sepsis (LOS) in newborns at neonatal intensive care units (NICUs)13. In particular, the NRCS-A clone is found worldwide in NICUs14,15. Wirth et al.16 described the differences between Basal S. capitis-strains and the NRCS-A clone and explored the evolution and genetic characteristics behind the success of this clone in NICUs. In that recent study, three sublineages of NRCS-A: Proto-Outbreak 1 (POB1), Proto-Outbreak 2 (POB2), and Outbreak were defined, and of these the methicillin-resistant, heterogeneous glycopeptide-intermediate S. capitis (hGISC) Outbreak sublineage dominated in NICUs. Its genetic trait characteristics include tarFIJL, involved in production of wall teichoic acids (WTA) that are important in biofilm formation, attachment to biomaterials, and protection against cell damage (e.g. glycopeptide resistance)17,18; nsr (nisin resistance), which has been suggested to be involved in gut colonization preceding LOS among neonates19; and a type V SCCmec-SCCcad/ars/cop element (V-NRCS-A) including a type III-A CRISPR element. Recent years have seen an increasing amount of available S. capitis genome data. However, as most of these isolates are either associated with the NICU or insufficiently described, no conclusions can be drawn regarding the presence of the NRCS-A clone either in PJIs or in the community.
The aim of the present study was to investigate the genetic relatedness and diversity among S. capitis isolated from PJIs compared to commensal and neonatal isolates in relation to the NRCS-A clone.
Results
Genome sequencing and phylogenetic analysis
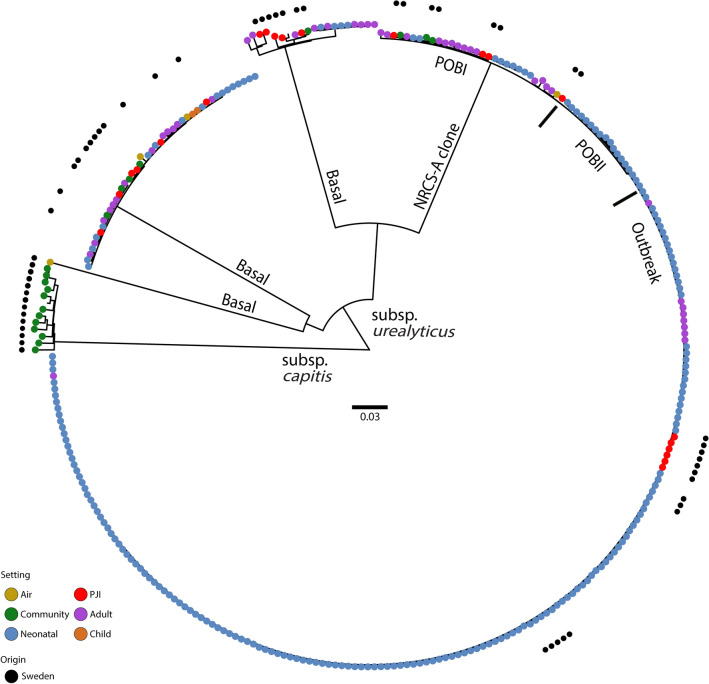
The obtained Illumina sequencing data from the 56 Swedish isolates were assembled into draft genomes with an average sequencing depth of 172 (all > 42 fold), and with between 45 and 357 contigs (average 141). The genome size varied between 2.3 to 2.6 Mb. Using the raw sequencing data of the Swedish isolates with sequence data from the international collection, 82,969 SNPs were obtained in a core genome of ~ 1.8 Mb (72%) which reduced to 37,970 SNPs after removing recombinant regions. In contrast to the nine Swedish NICU strains, which clustered exclusively with the international NRCS-A Outbreak sublineage, PJI isolates were intermingled throughout all previously defined clades including the Outbreak sublineage (Fig. 1). Also present was a highly distinct clade containing nasal commensals only. These isolates were generally antibiotic susceptible; however, three of them also unexpectedly harboured an nsr gene variant.
Figure 1.
Midpoint-rooted maximum-likelihood phylogeny of 305 S. capitis isolates based on 37,970 SNPs after purging of recombination. The Swedish isolates are represented by black dots. The colours in the main circle describe the setting where isolates were retrieved: yellow = air, green = community, blue = neonatal, red = PJI, purple = adult (unspecified location), brown = child (unspecified location). The subspecies differentiation of S. capitis is presented, as are the sublineages of S. capitis subsp. urealyticus. POBI proto-outbreak 1. POBII proto-outbreak 2. Scale bar indicates substitutions per site.
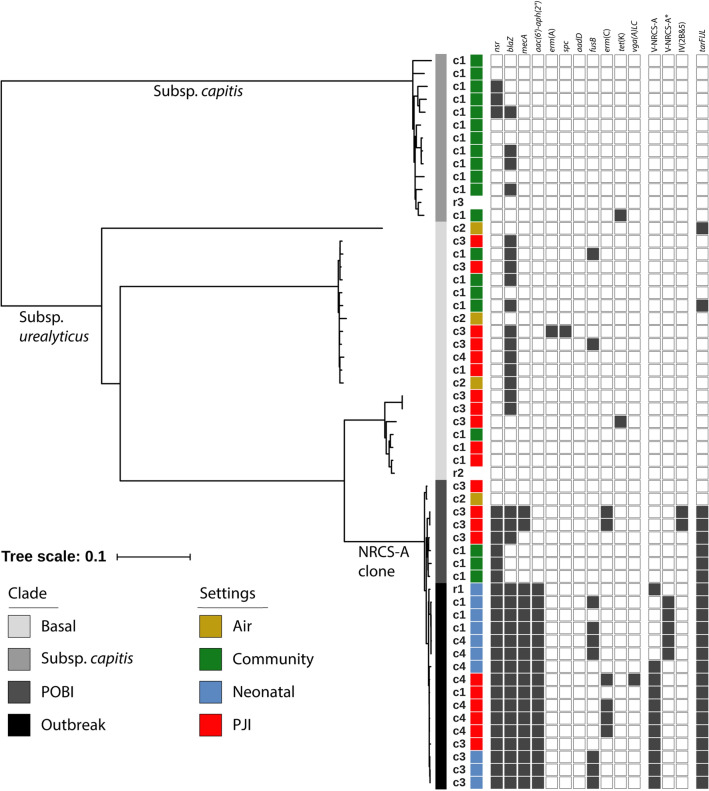
The Swedish-only phylogeny, based on 29,811 purged SNPs obtained from an initial 79,018 SNPs identified in a ~ 1.9 Mb (75%) core genome, revealed the presence of three distinct clades (Fig. 2). The uppermost clade (subsp. capitis) was distinctly separated from the other two clades. This clade included the CCUG 35173 S. capitis subsp. capitis reference strain as well as most of the commensal isolates. The middle clade (Basal lineage) was more diverse and included commensals, PJI isolates, operating theatre air isolates, and the CCUG 55892 S. capitis subsp. urealyticus reference strain, but no NICU-associated isolates. The lower clade (NRCS-A, containing the POB1, POB2, and Outbreak sublineages) contained all the NICU-associated isolates, 10 isolates from PJIs, and one isolate from operating theatre air. All 18 mecA-positive isolates were part of the NRCS-A clade. The composite type V SCCmec-SCCcad/ars/cop element was found in 11 out of 18 Swedish mecA positive isolates, including six from PJIs located in the Outbreak sublineage. Five isolates, all from NICUs in two of the participating centres, had a partial deletion of the element (including the ccrA1 and ccrB3 genes) marked as V-NRCS-A* in Fig. 2. In addition, two isolates carried SCCmec type IV(2B&5).
Figure 2.
Midpoint-rooted maximum-likelihood phylogeny of 56 S. capitis isolates and presence of resistance genes based on a 75% core genome. Different centres are identified as c1–c4 and reference isolates named r1 (NRCS-A prototype strain CR01), r2 (CCUG 55892), and r3 (CCUG 35173). All isolates except r1 were isolated in Sweden. The settings where all Swedish strains were isolated are presented in colour: yellow = air, green = community, blue = neonatal, red = PJI, and white = no data. From c1 was included nasal isolates (n = 20), PJI isolates (n = 4) and NICU isolates (n = 3), from c2 operating theatre air (n = 4), from c3 PJI isolates (n = 12) and NICU isolates (n = 3) and from c4 PJI isolates (n = 5) and NICU isolates (n = 3). The phylogeny highlighted the subsp. capitis, Basal, and NRCS-A clade sublineages. Black blocks represent presence of genes mediating antibiotic resistance and SCCmec type.
The 29 genes previously associated with the NRCS-A clade16 were also mostly found in the NRCS-A clone, but two genes found in the SCCmec composite element (CR01_v3_0458 and CR01_v3_0459) were also found in two isolates in the subsp. capitis clade and two isolates in the Basal clade.
The nsr gene was present in all but two POB1 isolates in the NRCS-A clade, together with an additional three isolates in the subsp. capitis clade. However, the homology to the previously described NRCS-A nsr gene was 99.77% for those three isolates, and further analysis revealed four non-synonymous changes, one resulting in a premature stop codon. All isolates in the NRCS-A clade with the exception of two POB1 isolates, but also two isolates in the Basal clade carried tarFIJL genes. Within the NRCS-A clade, seven of the ten PJI isolates were hGISC, and all seven were tarFIJL-positive, compared to the Basal clade where one of the 12 PJI isolates was hGISC and none were tarFIJL-positive (p = 0.002, Fisher’s exact test). Further clinical and phenotypical data on the NRCS-A Outbreak sublineage PJI isolates are presented in Table 1.
Table 1.
Clinical data for the PJI NRCS-A Outbreak isolates.
| Centre | Infection type | Year of surgery | Year of diagnosis | MDR | hGISC | Biofilm CRA/MTP |
|---|---|---|---|---|---|---|
| c3 | Chronic, polymicrobial | 2001 | 2010 | − | + | + /− |
| c4 | Chronic, monomicrobial | 2009 | 2010 | + | + | + / + |
| c4 | Chronic, monomicrobial | 2011 | 2011 | + | − | + /− |
| c4 | Early, polymicrobial | 2011 | 2011 | + | + | + /− |
| c1 | Early, polymicrobial | 2011 | 2011 | − | + | + / + |
| c4 | Early, monomicrobial | 2012 | 2012 | + | + | + /− |
MDR multi-drug resistant isolate, hGISC heterogeneous glycopeptide intermediate S. capitis, CRA Congo red agar, MTP microtitre plate assay.
Bacterial subspecies
In silico analysis of the 16S rRNA gene did not discriminate between the two subspecies. All Swedish isolates in the subsp. capitis clade were identified as S. capitis subsp. capitis based on urease activity and maltose fermentation tests, including reference strain CCUG 35173. Among the isolates in the Basal and NRCS-A clades, 16/43 (37%) isolates (including the reference strain CCUG 55892) were urease-negative/maltose-positive while the remaining 27 (63%) were urease-positive/maltose-positive. These results were consistent on re-analysis, and urease-negative strains were scattered across the phylogeny (see Supplementary Fig. S1 online), indicating unreliable performance of the urease activity test within one subspecies. Thus, the maltose-positive isolates were interpreted as subsp. urealyticus regardless of the urease activity.
Discussion
Here we have demonstrated that the S. capitis NRCS-A Outbreak clone is not solely restricted to NICU-associated sepsis, but also occurs in adult PJIs in all three investigated Swedish regions. The NRCS-A clone has been shown capable of causing outbreaks in NICUs worldwide, but it is not currently known whether these cases in orthopaedic implant surgery represent spillover from NICUs, or a more widespread in-hospital dissemination than previously reported. However, the temporal distribution indicates that an outbreak situation of the kind seen in NICUs is presently unlikely.
The major specific genetic features that have been described for this clone in NICUs are a type V SCCmec-SCCcad/ars/cop, alteration of WTAs through tarFIJL, and nisin resistance16. When revisiting clinical and phenotypic data7, MDR (including methicillin resistance and hGISC) and biofilm production were common among the NRCS-A PJI Outbreak isolates. Virulence factors, such as biofilm formation, immune evasion, and antibiotic resistance, have an impact on pathogenesis and treatment strategies in PJIs, and the NRCS-A Outbreak clone contains all characteristics required for a successful PJI pathogen.
The nsr gene was present in all isolates in the NRCS-A Outbreak clade, as well as the composite type V SCCmec-SCCcad/ars/cop element. However, the presence of SCCmec type IV in two Proto-Outbreak isolates showed at least two independent acquisitions of SCCmec. In PJIs, methicillin resistance mediates a lack of susceptibility to first-line prophylaxis (i.e. cefazolin or cloxacillin), and hGISC mediates reduced susceptibility to first-line treatment in methicillin-resistant coagulase-negative staphylococci. Several functions have been proposed for WTA in S. aureus, including interaction with biomaterials and receptors (e.g. mediating adherence to epithelial and endothelial cells, attachment to biomaterials, and biofilm formation) and protection against cell damage (e.g. resistance to vancomycin and lysozyme)17,18. Interestingly, the presence of tarFIJL was significantly associated with hGISC expression when comparing the PJI isolates in the Basal clade to those in the NRCS-A clade. Formation of biofilm is crucial in adherence to surfaces, both for persistence in the environment, which is implied to be of importance in the NICU15, and in the pathogenesis of PJIs. Nisin resistance, however, may possibly be beneficial for survival in the gut among neonates19, but there is no obvious connection between nisin resistance and pathogenesis of PJIs. Thus, nisin resistance may simply be a fortuitous passenger in a virulent nosocomial strain residing on surfaces in the NICU, with potential for nosocomial spread. Further environmental sampling from hospital surfaces outside the NICU is required to determine potential reservoirs for persistence of nosocomial S. capitis strains, which could improve preventive measures against the devastating infections PJIs constitute.
Nasal colonization with S. aureus has been described as a risk factor for surgical site infections such as PJIs20, and nasal and PJI strains are phylogenetically similar8. However, a discrepancy between the antibiotic susceptibility and sequence types among commensal and PJI isolates of S. epidermidis indicates that the nares are colonized with different strains from those causing PJIs21,22. The majority of the nasal isolates in the present study belonged to antibiotic susceptible subsp. capitis, and lack of several of the virulence genes found in the NRCS-A clade, thus indicating that strains with lower virulence are prevalent in the community. Still, although commensal isolates were diverse and consisted of both subspecies, the NRCS-A Outbreak sublineage was not found in nares. Thus, based on this collection of isolates, nasal colonization does not seem to be a major source for nosocomial infections by the NRCS-A clone.
Subtyping for differentiation between the two subspecies is generally not performed in clinical practice. When comparing the WGS-based clustering with phenotypic assays, urease activity proved unreliable; all the subsp. capitis isolates and 37% of the subsp. urealyticus were negative, which is in contrast to data from Bannerman et al.23, where > 90% of subsp. urealyticus were positive. However, the maltose fermentation test alone could discriminate between the two subspecies in all tested isolates. While subsp. urealyticus apparently can truly act both as commensal and as pathogen, the pathogenic potential of subsp. capitis is uncertain. If future research confirms the presence of clades with different disease-causing potential in PJIs, determining which clade a clinical isolate belongs to may help discriminate commensals from pathogens, as subsp. capitis seems to have lower pathogenic potential than subsp. urealyticus.
Limitations of the present study include the small cohort size; however, the identification of NRCS-A strains in PJIs in all three investigated centres despite the limited cohort size is alarming. Additionally, no data were available regarding prior healthcare contact of nasal carriers of subsp. urealyticus, particularly the POB1 sublineage. Future research focusing on nasal colonization in subjects with diverse and known backgrounds may shed further light on nasal carriage of different subspecies/clones of S. capitis.
In conclusion, the NRCS-A clone is not exclusive to NICUs, but is also able to cause serious infections, such as PJIs, in adults. Further research is needed to fully understand reservoirs and distribution among patients at risk for nosocomial opportunistic infections, including immunocompromised patients and those with medical implants.
Methods
Bacterial isolates
Whole-genome sequencing (WGS) was performed on 54 S. capitis isolates from three adjacent Swedish regions: Värmland, Örebro, and Östergötland, encompassing approximately one million inhabitants. The clinical and demographic characteristics of the PJI isolates (n = 21) have been reported previously7. Briefly, these were isolated from tissue biopsies taken during reoperations or revisions of infected prosthetic joints between 2005 and 2014. Nasal isolates (n = 20) were obtained prior to hospital admission, at first outpatient clinic visit during 2017–2018 from patients planned for elective hip or knee replacement surgery. No clinical data were available for these patients. Three isolates from epidemiologically unrelated cases of S. capitis-bacteraemia in the NICU were selected from each of the participating regions during 2014–2016 (n = 9). As the primary aim was to determine whether the MDR NRCS-A clone was present in the NICUs, MDR strains were randomly selected if more than three isolates were available. No clinical data were collected for these patients, so it was not known whether LOS was present. Isolates from operating theatre air (n = 4), collected in 2011–2012 in the adjacent region of Västmanland24 were also included. All isolates were determined to species level using MALDI-TOF MS (Microflex LT and Biotyper 3.1; Bruker Daltonics, Bremen, Germany). Also included were published genomic data from an international collection of 250 isolates16 available at the Sequence Read Archive (https://www.ncbi.nlm.nih.gov/sra) BioProject number PRJNA493527; two of these were excluded after quality assessment. Additionally, subspecies reference isolates CCUG 35173 (S. capitis subsp. capitis) and CCUG 55892 (S. capitis subsp. urealyticus) obtained from the University of Gothenburg Culture Collection (http://www.ccug.se) were genome sequenced and included.
Genome sequencing and phylogenetic analysis
Genomic DNA was purified using the QIAGEN Blood and Tissue Kit (Qiagen). A sequencing library was produced using a Nextera XT kit (Illumina) according to the manufacturer’s instructions, followed by paired-end sequencing using 300- or 500-cycle kits on a MiSeq or NextSeq instrument (Illumina), respectively. The resulting datasets are available from the SRA under BioProject number PRJEB35698. Genome sequences were de novo assembled using SPAdes v3.11.125 with default parameters.
To examine their ability to discriminate between S. capitis subsp. capitis and subsp. urealyticus, subspecies relations were investigated using in silico analysis of 16S rRNA genes, as well as urease activity and maltose fermentation tests23 using the ID32 STAPH system (bioMérieux, Marcy l’Etoile, France) according to the manufacturer’s instructions.
Single nucleotide polymorphisms (SNPs) were identified using NASP v1.0.026. BWA-MEM was used to align Illumina reads from individual isolates against the chromosome of S. capitis isolate CR01 (GenBank accession number LN866849). Positions with ≤ 10-fold sequencing depth and/or < 90% unambiguous variant calls were removed using GATK after positions within duplicated or repetitive regions of the reference genome were masked using NUCmer. Two SNP-based analyses were performed, one for the Swedish-only collection (n = 56) and one including the additional 248 isolates. For both analyses, recombinant regions were removed using Gubbins v.2.3.427. Phylogenetic trees of all isolates were constructed using the maximum-likelihood approach in PhyML v3.3 with the GTR substitution model and 100 bootstrap replicates28. The phylogenies were visualized using iTOL (https://itol.embl.de).
Resistance genes were detected from the assembled draft genes with ABRicate (https://github.com/tseemann/abricate) using the ResFinder (cge.cbs.dtu.dk/services/ResFinder/) database. In addition, the presence of 29 previously identified genes associated with the Outbreak/Proto-Outbreak strains16, including the nsr gene encoding nisin resistance and a cell wall teichoic-acid associated gene cluster (tarFIJL), were examined using a BLASTN search against the assembled genomes.
For the mecA-positive Swedish isolates, the SCCmec elements were identified using SCCmecFinder29 with minimum 40% coverage and 80% identity. In addition, reads were mapped towards the composite SCCmec element described by Martins Simoes et al. (GenBank accession number KF049201)30.
Ethics approval
Access to clinical data (reference: 2014/418) and the collection of commensal isolates (reference: 2012/092) were approved by the Regional Ethical Review Board of Uppsala.
Consent for publication
Not applicable.
Supplementary Information
Acknowledgements
The authors would like to thank Olov Svartström for assistance in sequencing and participating in the start-up of this project, and Emeli Månsson for providing the air isolates.
Abbreviations
- DAIR
Debridement, antibiotics, and implant retention
- hGISC
Heterogeneous glycopeptide-intermediate S. capitis
- LOS
Late-onset sepsis (in neonates)
- MDR
Multidrug resistance
- NICUs
Neonatal intensive care units
- PJIs
Prosthetic joint infections
- POB1
Proto-outbreak 1
- POB2
Proto-outbreak 2
- WGS
Whole-genome sequencing
- WTA
Wall teichoic acids
Author contributions
S.T., B.S., M.S., S.B., Å.N.A., and B.H. contributed to the design of the work, with additional input from P.M.S., T.W., and M.B. S.T. collected the medical and bacteriological data. B.S. and B.H. performed the microbiological analysis. B.H., S.B., and M.S. performed the genome sequencing, and S.B. and M.S. performed the bioinformatic analyses. S.T. wrote the manuscript, and B.S., M.S., S.B., Å.N.A., and M.B. made critical revisions. All authors have read and approved the final manuscript.
Funding
Open Access funding provided by Örebro University. Open Access funding provided by Örebro University. This work was supported by grants from the research committee of Värmland County Council, Sweden (grant numbers LIVFOU-644591, LIVFOU-736151, LIVFOU84251, LIVFOU-776591, and LIVFOU-834801), from the research committee of Östergötland County Council, Sweden (grant number LIO-447091), from Örebro University, Sweden (ORU 1.3.1-01273/2015), and from the Foundation for Medical Research at Örebro University Hospital (Nyckelfonden OLL-502241).
Data availability
The datasets generated and analysed during the current study are available from the SRA under BioProject number PRJEB35698.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Bo Söderquist and Marc Stegger.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-020-79225-x.
References
- 1.Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27(8 Suppl):61-5 e1. doi: 10.1016/j.arth.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 2.Kasina P, Enocson A, Lindgren V, Lapidus LJ. Patient claims in prosthetic hip infections: A comparison of nationwide incidence in Sweden and patient insurance data. Acta Orthop. 2018;89(4):394–398. doi: 10.1080/17453674.2018.1477708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindgren V, Gordon M, Wretenberg P, Kärrholm J, Garellick G. Deep infection after total hip replacement: A method for national incidence surveillance. Infect. Control Hosp. Epidemiol. 2014;35(12):1491–1496. doi: 10.1086/678600. [DOI] [PubMed] [Google Scholar]
- 4.Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet. 2016;387(10016):386–394. doi: 10.1016/S0140-6736(14)61798-0. [DOI] [PubMed] [Google Scholar]
- 5.Peel TN, Cole NC, Dylla BL, Patel R. Matrix-assisted laser desorption ionization time of flight mass spectrometry and diagnostic testing for prosthetic joint infection in the clinical microbiology laboratory. Diagn. Microbiol. Infect. Dis. 2015;81(3):163–168. doi: 10.1016/j.diagmicrobio.2014.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Tevell S, Claesson C, Hellmark B, Söderquist B, Nilsdotter-Augustinsson A. Heterogeneous glycopeptide intermediate Staphylococcus epidermidis isolated from prosthetic joint infections. Eur. J. Clin. Microbiol. Infect. Dis. 2014;33(6):911–917. doi: 10.1007/s10096-013-2025-3. [DOI] [PubMed] [Google Scholar]
- 7.Tevell S, Hellmark B, Nilsdotter-Augustinsson A, Söderquist B. Staphylococcus capitis isolated from prosthetic joint infections. Eur. J. Clin. Microbiol. Infect. Dis. 2017;36(1):115–122. doi: 10.1007/s10096-016-2777-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wildeman P, Tevell S, Eriksson C, Campillay Lagos A, Söderquist B, Stenmark B. Genomic caractherization and outcome of prosthetic joint infections caused by Staphylococcus aureus. Sci. Rep. 2020;10:5938. doi: 10.1038/s41598-020-62751-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lowik CAM, Jutte PC, Tornero E, Ploegmakers JJW, Knobben BAS, de Vries AJ, et al. Predicting failure in early acute prosthetic joint infection treated with debridement, antibiotics, and implant retention: External validation of the KLIC score. J. Arthroplasty. 2018;33(8):2582–2587. doi: 10.1016/j.arth.2018.03.041. [DOI] [PubMed] [Google Scholar]
- 10.Bianco C, Arena F, Rossetti B, Tordini G, Migliorini L, Galluzzi P, et al. First report of spondylodiscitis due to vancomycin heteroresistant Staphylococcus capitis in immunocompetent host. J. Infect. Chemother. 2014;20(10):639–642. doi: 10.1016/j.jiac.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Brooks, D., Thomas, V., Snowden, J. Staphylococcus capitis osteomyelitis: Case report. Glob. Pediatr. Health.6, 2333794X19833736 (2019). [DOI] [PMC free article] [PubMed]
- 12.Cui B, Smooker PM, Rouch DA, Daley AJ, Deighton MA. Differences between two clinical Staphylococcus capitis subspecies as revealed by biofilm, antibiotic resistance, and pulsed-field gel electrophoresis profiling. J. Clin. Microbiol. 2013;51(1):9–14. doi: 10.1128/JCM.05124-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rasigade JP, Raulin O, Picaud JC, Tellini C, Bes M, Grando J, et al. Methicillin-resistant Staphylococcus capitis with reduced vancomycin susceptibility causes late-onset sepsis in intensive care neonates. PLoS ONE. 2012;7(2):e31548. doi: 10.1371/journal.pone.0031548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Butin M, Rasigade JP, Martins-Simoes P, Meugnier H, Lemriss H, Goering RV, et al. Wide geographical dissemination of the multiresistant Staphylococcus capitis NRCS-A clone in neonatal intensive-care units. Clin. Microbiol. Infect. 2016;22(1):46–52. doi: 10.1016/j.cmi.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Carter GP, Ussher JE, Da Silva AG, Baines SL, Heffernan H, Riley TV, et al. Genomic analysis of multiresistant Staphylococcus capitis associated with neonatal sepsis. Antimicrob. Agents Chemother. 2018;62(11):e00898–e918. doi: 10.1128/AAC.00898-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wirth T, Bergot M, Rasigade J, Pichon B, Barbier M, Martins-Simoes P, et al. Niche specialization and spread of Staphylococcus capitis involved in neonatal sepsis. Nat. Microbiol. 2020;5:735–745. doi: 10.1038/s41564-020-0676-2. [DOI] [PubMed] [Google Scholar]
- 17.Xia G, Kohler T, Peschel A. The wall teichoic acid and lipoteichoic acid polymers of Staphylococcus aureus. Int. J. Med. Microbiol. 2010;300(2–3):148–154. doi: 10.1016/j.ijmm.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Gerlach D, Guo Y, De Castro C, Kim S-H, Schlatterer K, Xu F-F, et al. Methicillin-resistant Staphylococcus aureus alters cell wall glycosylation to evade immunity. Nature. 2018;563(7733):705–709. doi: 10.1038/s41586-018-0730-x. [DOI] [PubMed] [Google Scholar]
- 19.Simoes PM, Lemriss H, Dumont Y, Lemriss S, Rasigade JP, Assant-Trouillet S, et al. Single-molecule sequencing (PacBio) of the Staphylococcus capitis NRCS-A clone reveals the basis of multidrug resistance and adaptation to the neonatal intensive care unit environment. Front. Microbiol. 2016;7:1991. doi: 10.3389/fmicb.2016.01991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levy PY, Ollivier M, Drancourt M, Raoult D, Argenson JN. Relation between nasal carriage of Staphylococcus aureus and surgical site infection in orthopedic surgery: The role of nasal contamination. A systematic literature review and meta-analysis. Orthop. Traumatol. Surg. Res. 2013;99(6):645–651. doi: 10.1016/j.otsr.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 21.Salih L, Tevell S, Månsson E, Nilsdotter-Augustinsson A, Hellmark B, Söderquist B. Staphylococcus epidermidis isolates from nares and prosthetic joint infections are mupirocin susceptible. J. Bone Jt. Infect. 2018;3(1):1–4. doi: 10.7150/jbji.22459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hellmark B, Söderquist B, Unemo M, Nilsdotter-Augustinsson A. Comparison of Staphylococcus epidermidis isolated from prosthetic joint infections and commensal isolates in regard to antibiotic susceptibility, agr type, biofilm production, and epidemiology. Int. J. Med. Microbiol. 2013;303(1):32–39. doi: 10.1016/j.ijmm.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Bannerman TL, Kloos WE. Staphylococcus capitis subsp. ureolyticus subsp. nov. from human skin. Int. J. Syst. Bacteriol.41(1), 144–147 (1991). [DOI] [PubMed]
- 24.Månsson E, Hellmark B, Sundqvist M, Söderquist B. Sequence types of Staphylococcus epidermidis associated with prosthetic joint infections are not present in the laminar airflow during prosthetic joint surgery. APMIS. 2015;123(7):589–595. doi: 10.1111/apm.12392. [DOI] [PubMed] [Google Scholar]
- 25.Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012;19(5):455–477. doi: 10.1089/cmb.2012.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sahl JW, Lemmer D, Travis J, Schupp JM, Gillece JD, Aziz M, et al. NASP: An accurate, rapid method for the identification of SNPs in WGS datasets that supports flexible input and output formats. Microb. Genom. 2016;2(8):e000074. doi: 10.1099/mgen.0.000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Croucher NJ, Page AJ, Connor TR, Delaney AJ, Keane JA, Bentley SD, et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 2015;43(3):e15. doi: 10.1093/nar/gku1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guindon S, Dufayard JF, Lefort V, Anisimova M, Hordijk W, Gascuel O. New algorithms and methods to estimate maximum-likelihood phylogenies: Assessing the performance of PhyML 3.0. Syst. Biol. 2010;59(3):307–321. doi: 10.1093/sysbio/syq010. [DOI] [PubMed] [Google Scholar]
- 29.Kaya H, Hasman H, Larsen J, Stegger M, Johannesen TB, Allesoe RL, et al. SCCmecFinder, a web-based tool for typing of staphylococcal cassette chromosome mec in Staphylococcus aureus using whole-genome sequence data. mSphere. 2018;3(1):e00612-17. doi: 10.1128/mSphere.00612-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martins Simoes P, Rasigade JP, Lemriss H, Butin M, Ginevra C, Lemriss S, et al. Characterization of a novel composite staphylococcal cassette chromosome mec (SCCmec-SCCcad/ars/cop) in the neonatal sepsis-associated Staphylococcus capitis pulsotype NRCS-A. Antimicrob. Agents Chemother. 2013;57(12):6354–6357. doi: 10.1128/AAC.01576-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analysed during the current study are available from the SRA under BioProject number PRJEB35698.