Abstract
Context:
Psychological distress is associated with adverse health outcomes in serious illness and magnified among patients of low socioeconomic status. Aspects of one’s culture, such as religion and spirituality, can influence these patients’ coping response to distress. Advanced chronic kidney disease (CKD) is a serious illness that disproportionately affects patients of low socioeconomic status, but a theory-based understanding of this group’s lived experience of CKD is lacking.
Objectives:
We explored the cognitions, emotions, and coping behaviors of patients with CKD with emphasis on those of low socioeconomic status. We further inquired into any influences of religion or spirituality.
Methods:
We interviewed 50 English or Spanish-speaking adults with advanced CKD from three medical centers in Nashville, Tennessee. Analyses occurred with 1) isolation of themes; 2) development of a coding system; and 3) creation of a conceptual framework using an inductive-deductive approach.
Results:
Median age was 65 years old, median annual income was $17,500 per year, and 48% of participants had not progressed beyond high school. Key beliefs (awareness of mortality, lack of control) influenced patients’ emotions (existential distress in the form of death anxiety, prognostic uncertainty, hopelessness) and coping behaviors (acceptance, avoidance, emotion regulation via spirituality, seeking social support via a religious community).
Conclusions:
Individuals with advanced CKD and low socioeconomic status lack control over disease progression, experience death anxiety and existential distress, and emphasize spirituality to cope. Our study identifies novel components for a psychotherapeutic intervention for patients with advanced CKD at high risk for adverse health outcomes.
Keywords: qualitative, socioeconomic disadvantage, kidney, existential distress
Introduction
Psychological distress, which occurs when the cognitive, emotional, and behavioral resources to adapt to stress are exceeded, is prevalent in serious illness.1,2 Individuals with serious illness and limited socioeconomic resources, defined as having a low annual income, financial instability, or poor educational attainment, experience higher rates of psychological distress as compared to those with adequate resources.3 Advanced chronic kidney disease (CKD) is a serious illness that disproportionately affects those with limited socioeconomic resources, but psychological adaptation to distress remains poorly investigated in this group.4 Most existing studies use quantitative surveys that only include depressive symptoms, focus on patients who have already become dialysis-dependent, exclude those who are economically disadvantaged and from diverse cultural backgrounds, and do not ground analyses in psychological theory.5–7 Aspects of culture, such as religious or spiritual beliefs, have been shown to strongly influence how individuals of low socioeconomic status cope with psychological distress.8–10 Yet, these areas have not been sufficiently explored in patients living with advanced CKD.
Cognitive behavioral interventions reduce psychological distress by challenging distressing beliefs, or cognitions, and improving emotion regulation to facilitate adapting coping responses to a perceived threat.11 Evidence supports the use of tailored psychotherapeutic interventions to treat psychological distress in individuals with heart disease and malignancy, but there is a paucity of theoretical models to inform these interventions in CKD.12 Furthermore, patients with advanced CKD of all backgrounds continue to report that they have unmet psychosocial needs.13
Burdensome cognitive representations, distressing emotional reactions, or maladaptive coping responses to advanced CKD have not been identified in subgroups at highest risk for adverse outcomes, and meaningful targets for psychotherapeutic interventions to decrease psychological distress and improve health outcomes in this group remain undefined. This study represents a first step toward meeting this need by exploring the cognitive, emotional, and behavioral response to adapting to life with advanced CKD among individuals with low socioeconomic status from diverse cultural backgrounds with special inquiry into any emotion regulation facilitated by religious or spiritual beliefs.
Materials and Methods
Study Design and Sample
Semi-structured interviews of 50 adults from Vanderbilt University Medical Center, Meharry Medical College, and the Siloam Health Center in Nashville, Tennessee were conducted. Individuals were eligible if they were English or Spanish speaking, above the age of 18, able to consent, and had Stage 4-5 CKD (estimated glomerular filtration rate of <30 mL/min/1.73m2) as documented in the medical record. Participants receiving dialysis, with a kidney transplant, or with dementia were excluded. The study was approved by Institutional Review Boards or study committees at each site.
Qualitative Interviews
We adhered to the Consolidated Criteria for reporting Qualitative Research (COREQ) guidelines to ensure the rigor of our qualitative methods (Supplementary File 1).14 The principal investigator (DN) developed a semi-structured interview guide informed by validated, cross-cultural communication frameworks in health psychology, the Kleinman Explanatory Model of Illness and Leventhal’s Common-Sense Model of Self-Regulation.15–16 According to these frameworks, adaptation to an illness is informed by perceptions of its intrusiveness, controllability, and consequences. Questions were not copied verbatim from these frameworks and remained broad and open-ended to allow for participants to respond in their own words. The interview guide and consent forms were written in English and Spanish. Interview questions were pilot tested for comprehension and clarity in a community engagement studio of six patients who met study inclusion criteria.17 Two questions identified as vague or uncomfortable were removed. Participants unanimously agreed on adequacy of study compensation ($40 per interview) and the relevance of the study to their daily lives. The final version was agreed upon by all investigators (Supplementary File 2).
The principal investigator used purposive sampling to ensure that an adequate sample of participants of low socioeconomic strata and from diverse cultural and religious backgrounds were included, within the limitations of geography. Participants were recruited based on zip code, insurance status, and the following self-reported characteristics: race, educational attainment, annual income, and religious affiliation. Recruitment was done via telephone from electronic medical record review or in-person in clinic waiting rooms. Four participants who were initially approached refused due to scheduling issues, resulting in a total of 50 participants who were ultimately interviewed.
Interviews were conducted in-person by investigators with formal training in qualitative research (DN and KB). Neither investigator had any prior relationship with the participants, and participants were aware of the investigators’ professions (researchers in nephrology and health psychology, respectively). Research bias was minimized in the following ways: neither investigator had any expectations regarding the results, and the study used investigators with different, unrelated professions. Interviews occurred between November 2018 and February 2019 at each site, ranged from 30 to 90 minutes, were conducted in English or Spanish according to participant preference, and were audio-recorded on a secure device in real time. Spanish interviews were translated into English in real time using an on-site translator. Only the interviewer and participant were present, no notes were taken, and no repeat interviews were conducted. Interviews were conducted until thematic saturation was achieved (N = 50 participants), meaning that after 50 interviews, no new themes were generated from participant quotations.18 Audio recordings were transcribed using an IRB-approved professional transcription service (http://rev.com). Transcripts were offered to participants, but all declined.
Coding and Data Analysis
Analyses occurred in real-time as ongoing interviews were conducted. Using an iterative, inductive and deductive approach as has been described in the literature, DN and KB coded quotations from the interviews onto a framework (Supplementary File 3).19–20 Inductively, content from participant quotations was used to identify themes and subthemes for the coding system from three initial transcripts. Deductively, the researchers reviewed literature on psychological distress and adaptation to illness to name and divide themes and subthemes.1,9–11
Coding was managed using a Microsoft Excel spreadsheet template developed by the Vanderbilt University Qualitative Research Core. Once the first three transcripts were coded independently and agreement was established, each subsequent transcript was coded by both investigators. Transcripts were analyzed in English using quotations that were input into the Statistical Package for the Social Sciences software (version 25) which was used to manipulate text and sort the data.21
Results
Table 1 lists the demographic, clinical, and sociocultural characteristics of participants. The median age of participants was 65 years old. There were similar numbers of participants across the following demographic characteristics: gender, marital status, race, and area of residence (urban vs. rural). Though this information had been documented by nephrologists in clinic visit notes, sixteen participants could not name the cause of their CKD. Median annual income was under $17,500 per year, and 48% of participants had not progressed beyond a high school education. ‘Low income’ and ‘very low income’ are defined by the United States Department of Housing and Urban Development as ‘less than or equal to 80%’ or ‘less than or equal to 50%’ of the median family income of the area, respectively.22–23 The interquartile range of income reported by participants qualities as ‘low income,’ and the median income of our participants falls into the ‘very low income’ range.
Table 1:
Demographic and sociocultural characteristics of participants (N = 50)
| Age in years (Median [IQR]) | 65 [53 – 72] | |
| Gender | Male (28) Female (22) |
|
| Marital status | Married (22) Single (11) Widowed (10) Divorced (6) In a relationship (1) |
|
| Self-identified race | White (24) Black or African American (21) American Indian or Alaska Native (1) |
|
| Ethnicity | Hispanic or Latino (4) Not Hispanic or Latino (46) |
|
| Annual income (Median [IQR]) | $17,500 [$11,000 – 40,000] | |
| Highest educational attainment | ≤ High school (24) Associate degree (4) ≥ College (15) Post-graduate degree (7) |
|
| Health insurance status | Some insurance (35) No insurance (15) |
|
| Years in nephrology care (Median [IQR]) | 4 [2 – 10] | |
| Number of medical comorbidities (Median [IQR]) | 3 [2 – 4] | |
| Cause of chronic kidney disease | Patient did not know** (16) Diabetes (14) Medication side effects (8) Hereditary genetic disease (4) Hypertension (2) Infection (2) Malignancy (2) Congenital defect (1) Sequelae of pregnancy (1) |
|
| Kidney transplant eligibility | Patient did not know** (10) Yes (22) No (18) |
|
| Religious affiliation | Christian (29) - Baptist (13) - Non-denominational (5) - Church of Christ (3) - East Orthodox (2) - Evangelical (2) - Roman Catholic (1) - Methodist (1) - Protestant (1) - Pentecostal (1) - Quaker (1) |
Jewish (8) Jehovah’s Witness (4) Muslim (3) Buddhist (1) Mormon (1) Spiritual (1) Not religious or spiritual (2) |
| Country of origin | United States (42) Mexico (3) Serbia (2) Sudan (1) Nigeria (1) Ethiopia (1) |
|
| Area of residence | Urban (30) Rural (20) |
|
known in electronic medical record
Abbreviations: IQR = interquartile range
Across demographic and sociocultural characteristics, we identified three major themes and ten subthemes of patients’ cognitive, emotional, and behavioral response to advanced CKD. No themes distinguished individuals based on demographic, cultural, or clinical characteristics, including race, ethnicity, religion, residential area, and cause of CKD. Figure 1 is a conceptual framework of the interrelationships between themes, and Table 2 lists themes and subthemes with corresponding illustrative quotes. As existing literature supports that the cognitive, emotional and behavioral response to an illness threat often occurs simultaneously and bidirectionally, a non-linear framework best fit our data.24 Exemplar quotes from each theme and subtheme are below.
Figure 1:
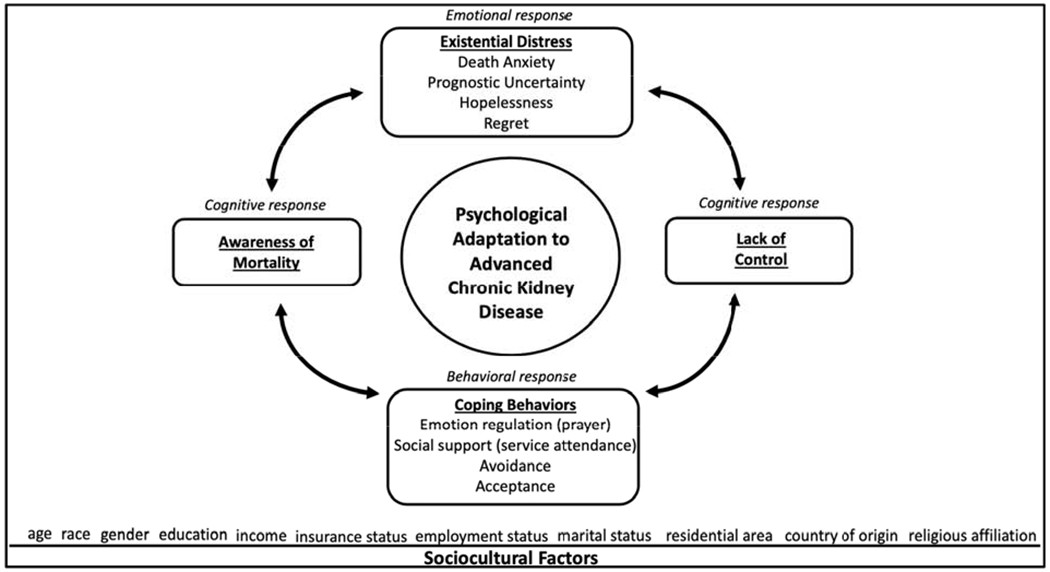
Psychological adaptation to advanced chronic kidney disease: a conceptual framework
↔ indicates hypothesized bidirectional relationship
Table 2:
Themes, subthemes, and corresponding illustrative quotes
| Theme | Subtheme | Illustrative quotes |
|---|---|---|
| Cognitive response to CKD | Awareness of mortality |
“It’s a chronic, fatal disease. It diminishes my ability to do things. Sometimes I’m functional, sometimes I’m not.” (P14) “My mother was on dialysis for three or four years, and it was really hard on her. She lived at the hospital. She’s talked about how people would die and bleed out, and how some people would get horribly bad cramps and be crying and screaming.” (P16) “I have a certain length to my freedom. I know that my days are numbered.” (P18) “To me, it’s like a death sentence.” (P23) “It’s like hitting a brick wall. ” (P35) “There is an expiration date on all of us.” (P16) “It’s going to get worse until you die.” (P42) |
| Lack of control | “You can’t do anything about it and sooner or later, that’s it.” (P46) “I can’t control the deterioration of my kidneys.” (P26) “I don’t think there’s anything. There’s nothing that can be done.” (P33) |
|
|
Emotional response to CKD Existential distress |
Death anxiety |
“I get antsy. I get nervous. I can’t eat because I’m so worried about what’s going to happen next. It’s been a rough road.” (P23) “I’m stressed about it, because I know it could be very fatal. I know folks that died on the machine. I know people have died when their other organs started failing.” (P24) “Well, the worst thing about having kidney disease is it will kill you.” (P39) |
| Prognostic uncertainty |
“I don’t know if I’m going to live.” (P49) “You can’t really forget it if you have chronic kidney disease because you never know what’s going to happen next.” (P34) “You know I feel like I may just be biding my time.” (P50) |
|
| Hopelessness |
“I know I’m going to die if I don’t go on the machine. But if I go on the machine, I may only live two or three months. I’m going to die anyhow. I’d rather take the few months.” (P34) “If you just sit and think about it, it makes you more depressed on a regular basis.” (P42) |
|
| Regret |
“I could have taken better care of myself earlier and controlled my blood pressure. I did develop high blood pressure 30-some odd years ago and at times didn’t take care of it.” (P15) “I could have done a lot of things - going to the doctor earlier, taking medication for high blood pressure, which I didn’t. I never took care of myself like I should’ve. I know I’m at fault.” (P28) |
|
|
Behavioral response to CKD Coping behaviors |
Emotion regulation (prayer, mindfulness) |
“My faith helps me with everything in life, because I’m not scared of dying.” (P6) “If your time comes, it comes. And if the doctor can’t help you, he can’t help you. And then, you just pray that you go to heaven… pray for a reunion.” (P33) “I pray about my kidneys. I know He’s got the power. I’ll say a prayer every night. Then, I thank Him for letting me live long enough to see my babies grow up to be old enough to take care of themselves.” (P48) “Praying gives me hope, faith, courage, and strength.” (P5) “For me, it’s a matter of praying. Inside, I feel hopeless when it comes to this disease. When I let it out, I don’t feel I’m a burden to those around me. At least I can get it off my chest.” (P3) “God answers my prayers. He understands. He gives me courage.” (P49) |
|
Seeking social support (religious service attendance) |
“Our faith group are really supportive of us and helped us cope with the day to day tragedies.” (P30) “Religious groups are a very strong source of support.” (P19) |
|
| Avoidance |
“I haven’t gotten there yet, I don’t want to think that far ahead.” (P40) “Actually, that would probably stress me out more. I try not to think about it.” (P6) “The less I think about it, the better. Otherwise, I would be stressed all the time.” (P20) “I try to think about something else, what we’re going to do this weekend, what we’re going to eat, things like that.” (P2) |
|
| Acceptance |
“I’ve got to bear with it. I’ve got to do everything I can to keep the kidney disease from getting worse than what it is. I try to do exactly what I’m supposed to.” (P26) “I don’t worry about it. I don’t dwell on it. I don’t let it control my life.” (P31) “It’s something that I’ve just got to live with.” (P29) |
Abbreviations: CKD = chronic kidney disease
Cognitive response to CKD
Awareness of mortality
When asked about the meaning and impact of CKD on daily life, participants viewed the disease as life-threatening and life-limiting. Participants emphasized the cognitive burden of being constantly reminded of impending death and viewed CKD as more psychologically burdensome than other illnesses. Participants described the uncertainty of having CKD, its asymptomatic nature, and the perceived inevitability of disease progression.
“It’s always threatening you, cutting short your time. Every day it reminds you. You can’t forget if you have kidney disease because you never know what’s going to happen.” (P34)
“Heart disease is no big deal. Worst case scenario, you get a pacemaker. For the kidneys, if you don’t keep following up with it, you may not wake up one day. You may not know that you’re toxic.” (P35)
“A cold is a cold. It’s not as bad as kidney disease. A cold can get worse, or it can get better. But kidney disease… it’s not going to get any better.” (P31)
Lack of control
Participants continued to emphasize feeling helpless, vulnerable, and powerless in the face of CKD and expressed a lack of control over disease prevention and treatment. Progression to death or dialysis was viewed as inevitable because of a lack of medications to improve or reverse kidney disease.
“I don’t have control over the creatinine. If I have another illness, it will affect my kidneys one way or the other.” (P17)
“There is nothing. There is no medication that’s going to enhance kidney function. If it’s damaged, it’s damaged.” (P33)
“I feel very vulnerable. I don’t feel in control of anything.” (P35)
“The more I think that I may have to undergo dialysis, the more helpless I feel.” (P46)
Emotional response to CKD
Death anxiety and prognostic uncertainty
In response to living with what was perceived as a life-limiting illness, participants moved beyond depressive symptoms to describe fear, anxiety, uncertainty, hopelessness, and regret. Prognostic uncertainty related to the severity of kidney disease was particularly distressing, and participants expressed feeling fear and anxiety as a result of this uncertainty.
“That worries me more than anything. Dialysis is just two, three, four years away from death. I don’t see a future.” (P32)
“The prognosis of kidney disease is very stressful for me.” (P10)
“It’s scary because of the ‘not knowing.’ How do I live the rest of my life with this disease? What shouldn’t I do?” (P31)
Hopelessness and regret
Many participants described hopelessness in the face of impending dialysis and conveyed regret from missed opportunities in disease self-management. Participants expressed a desire to improve self-management but felt ill-equipped to do so. One participant admitted to having had prior suicidal thoughts as a result of regret.
“They told me, ‘It’ll never get better. All we can do is keep it from getting worse.’ I was surprised when I heard that… there isn’t any hope.” (P24)
“I have screwed up all of my life. This will make a good novel for you. I have screwed up all my life. I’ve had a lot of potential. I always intended to do something. I still have a chance to… but if I’m laid up and sickly, I can’t do it…” (P46)
“Kidney disease catches up from when you were a child. What’s that thing they say? ‘What you put in the wash will come out in the rinse?’ I was raised in the country, so we ate a lot of syrup, jelly. Now, I’m 53. Some days, I get depressed. Some days, I’ve wanted to go to sleep and not wake up.” (P42)
Behavioral response to CKD
Coping behaviors – avoidance and acceptance
Participants used various strategies to cope with the psychological stressors associated with advanced CKD. Many avoided thinking about the topic entirely and hoped that the disease would resolve itself on its own. Others accepted the presence of the CKD in their daily lives.
“I hope it will go away. I’ll click my heels and the kidney disease will go away.” (P5)
“Fixating on something you’ve got no control over doesn’t help. What can you do to change the situation? If there’s nothing, fretting over it is not going to improve it in any way, shape, or form.” (P30)
“You play the hand that you’ve been dealt. If fate has determined that this is what it is, then you accept it.” (P36)
Coping behaviors – emotion regulation and social support via spirituality and religion
Participants also used emotion regulation to cope with advanced CKD by turning to their spiritual beliefs or using mindfulness techniques. Many sought social support via engaging with their religious community. Spiritual coping was strongly emphasized by all individuals who had attained a high school education or less or reported an annual income of under $25,000. Three individuals who reported an annual income of over $100,000 also emphasized turning to spiritual beliefs to cope. Prayer was a means to effectively adapt to life with a serious illness and resulted in courage, comfort, and hope.
“Being able to cope helps. Being able to control your mind is very important.” (P25)
“Our church and congregation are close. I have friends who support me and will visit if I’m hospitalized.” (P13)
“I’m not scared of dying. Praying gives me hope. Even if I died tomorrow, there is a future for me.” (P22)
“I’m able to put into perspective that kidney disease is not a death sentence. It’s an opportunity for me to reexamine and do as much as I can on this side of my life.” (P34)
Discussion
We found that across racial, ethnic, and sociocultural characteristics, patients consider advanced CKD to be life-limiting; lack a sense of control over disease progression; experience death anxiety, prognostic uncertainty, and existential distress; and respond with acceptance, avoidance, turning to spiritual beliefs, or engaging with a religious community to adapt. Preoccupation with and fear of death are newly recognized sources of psychological distress in patients living with CKD. Additionally, our patients’ emphasis on spiritual coping provides new insights into the supportive care needs of individuals with advanced CKD and limited socioeconomic resources.
Depressive symptoms are the most frequently described form of psychopathology in patients with kidney disease. Furthermore, the few existing studies that move beyond depressive symptoms to further explore the illness experience of CKD focus on patients at earlier stages along their disease continuum, use quantitative surveys such that coping behaviors influenced by religion or spirituality are unable to be deeply explored, and do not include the perspectives of individuals of low socioeconomic status despite this group being disproportionately affected by CKD.4–6,13 Our qualitative study design allowed for the exploration of a more complex range of emotions. A strong awareness of death, or mortality salience, is prevalent in those with living with serious illness, and this awareness often coexists with anxiety related to impending demise.25 In cross-sectional analyses of patients with breast, gastrointestinal, genitourinary, lung, or endocrine malignancies, death anxiety was more frequently reported by those with a greater physical symptom burden, those with children under the age of 18, and those who expressed depressive symptoms or prognostic uncertainty.26
A qualitative analysis describing the illness experience of undocumented immigrants with end-stage kidney disease (ESKD) revealed the presence of death anxiety among study participants.27 In a recent study of adults with CKD and their caregivers, being confronted with death was identified as a patient and caregiver priority. To our knowledge, this is the only other study that has described this concept in CKD.28 Our participants’ negative experiences related to peers who died while receiving hemodialysis may have significantly contributed to their own fears of impending death, but empirical data on several key aspects of death anxiety in CKD are lacking. It remains unknown whether death anxiety is worse among individuals with CKD who are ineligible for a transplant, who have a greater physical symptom burden, or whether similar emotions occur in those at even earlier stages of kidney disease. It also remains to be determined if death anxiety worsens perceptions of depression or contributes to difficulty in treating depression in patients with CKD.
Prognostic uncertainty was particularly distressing to individuals in our study. Similar findings have been demonstrated in other studies of patients with kidney disease and other serious illnesses. In a qualitative analysis of young adults receiving chronic dialysis or who had received a kidney transplant, prognostic uncertainty emerged as a patient and caregiver-prioritized outcome.29 In a study of patients with advanced malignancy, prognostic uncertainty was significantly associated with greater psychological distress and poorer perceptions of health-related quality of life.30 In addition to expressing distress related to prognostic uncertainty, many participants in our study could not name the cause of their disease or whether they were eligible for a transplant. While it has been established that CKD awareness in the general population is low, it is concerning that many participants in our study could not name the cause of their disease or their transplant status despite having been in nephrology care for a median of four years.31 These findings point to the importance of assessing kidney disease-specific knowledge and clearly communicating information regarding estimates of disease progression to prevent prognostic uncertainty in individuals with advanced CKD.32–33
Death anxiety, prognostic uncertainty, hopelessness, and feeling a decreased sense of control, all emphasized by our study participants, are core components of a multi-dimensional construct known in health psychology as existential distress. Defined as emotional turmoil in the face of imminent death, existential distress threatens individuals’ personal, physical, and spiritual identities.34 Often a result of living with a life-limiting illness, existential distress can cause individuals to feel isolated, lack a sense of purpose, and question their life’s meaning. Existential distress is best documented in individuals who live with or have survived a malignancy, and researchers have begun to identify and quantify the impact of existential distress on health outcomes. High levels of existential distress are associated with a greater frequency of depressive symptoms and an increased tendency for suicidal behavior in those living with malignancy.35–36 Pinpointing individuals at highest risk for existential distress as well as identifying factors to facilitate psychological adaptation are currently research priorities in serious illness care.37
Participants in our study turned to several coping behaviors, ranging from acceptance to avoidance, to adapt to living with advanced CKD, but for many, turning to spiritual beliefs was most meaningful. Spirituality, or having a relationship with the sacred in order to give life meaning, improves psychological adaptation to serious illness, and even more so for those with fewer social and economic resources.38–39 The awareness of death and existential distress emphasized by participants in our study may explain why so many turned to their spiritual beliefs to cope, as spiritual well-being has been linked to improvements in death anxiety. In a cross-sectional analysis of 190 patients with advanced malignancy, spiritual well-being was associated with decreased death anxiety, and in a sample of community-dwelling older adults receiving hospice care, spirituality, as opposed to adhering to a specific religious faith, was linked to decreased anxiety at the end of life.40
The hope, comfort, courage, and life meaning that participants derived from spiritual coping in our study deserve close attention. According to terror management theory, death anxiety occurs when an individual becomes strongly aware of his or her own mortality. As a result, individuals engage in coping behaviors to allay these fears, including denial, avoidance, or turning to religion or spirituality to find meaning in life.41 Similar to the needs expressed by our participants, individuals with both non-dialysis and dialysis-dependent CKD in another study expressed a strong need to find hope and meaning in the face of their illness.42 That study included mostly white participants at a university-affiliated medical center, and demographics did not predict participants’ desire for spiritual support. This suggests individuals with advanced CKD may benefit from a psychosocial and spiritual assessment regardless of demographics.
Patients with kidney disease who report higher levels of spirituality experience fewer depressive symptoms, greater resilience, improved health-related quality of life, and, in one analysis, increased survival.43–47 Psychotherapeutic interventions rooted in principles of spirituality improve psychological adaptation to serious illness, particularly among cancer survivors. Meaning-Centered Psychotherapy-- an intervention consisting of renegotiating life goals, learning how to cope with loss, making peace with missed opportunities, and accepting uncertainty related to death and dying-- decreased depressive symptoms and improved perceptions of meaning in life in a randomized controlled trial of 147 cancer survivors.48 Six, group-based sessions of Acceptance and Commitment Psychotherapy, which uses mindfulness and acceptance of intrusive thoughts to increase psychological flexibility, reduced avoidant coping, anxiety, depression, and fear of cancer recurrence in a pilot randomized controlled trial of breast cancer survivors.49 An ongoing cognitive existential intervention targets death anxiety and existential distress to decrease fear of cancer recurrence in women who have survived breast or gynecological malignancy.50 Results from these studies suggest that psychotherapeutic interventions may be feasible in and applicable to person-centered CKD care, though existing models of care delivery do not yet allow for their seamless implementation and update.
This study has limitations to acknowledge. Views expressed largely represent individuals in one geographic location, though findings may remain generalizable to other regions. The median age of our cohort was 65. While this is representative of the fastest-growing CKD population in the United States, we cannot draw conclusions related to psychological adaptation in younger individuals.51 Though on-site translators were available to translate interview responses for Spanish-speaking participants, some aspects of their responses may have been lost in translation to English. Though this was not the purpose of our study, we did not ask probing questions related to patients’ reactions to transplant ineligibility or specific sources of financial distress that may have affected CKD self-management. These questions would have provided insight into external and environmental drivers of psychological distress in this patient group.
This study amplifies underrecognized psychological stressors experienced by patients with CKD. Furthermore, it advances the methodological rigor of research in this area by providing a novel, theory-based framework of actionable targets to improve psychological adaptation to advanced CKD. Finally, this study illuminates perspectives of individuals who are often underrepresented in clinical research. Our findings provide empiric support for a tailored, psychotherapeutic intervention to reduce psychological distress and improve psychological adaptation for individuals with advanced CKD who are at high risk for adverse health outcomes.
Supplementary Material
Key Message:
This study demonstrates for the first time that individuals with advanced chronic kidney disease (CKD) and economic disadvantage experience death anxiety, existential distress, and emphasize spirituality to cope. It identifies novel targets for a psychotherapeutic intervention to reduce psychological distress and improve health outcomes in this group.
Acknowledgements:
The authors would like to thank the patients at Vanderbilt University Medical Center, Meharry Medical College, and the Siloam Health Center for their interest, participation, and support
Funding:
This work was supported by the following funding sources:
National Institutes of Health (NIH) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) 5T32DK007569-30 to DN
NIH National Center for Advancing Translational Sciences Vanderbilt Institute for Clinical and Translational Research UL1TR002243 to DN
Vanderbilt University Center for Effective Health Communication Pilot Grant to DN
NIH NIDDK 5K23DK114566-02 to EMU
NIH NIDDK 5P30DK114809-03 to KLC
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
Results of this work were shared in oral presentations at the 2019 National Kidney Foundation’s Mid-Atlantic Young Investigator Forum and the Academy of Communication in Healthcare’s 2019 International Conference for Communication in Healthcare.
All authors confirm that they have no conflicts of interest to disclose.
References
- 1.Folkman S Lazarus RS Dunkel-Schetter C, DeLongis A, Gruen A. Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol 1986;50(5): 992–1003. [DOI] [PubMed] [Google Scholar]
- 2.Troy JD, Locke SC, Samsa GP, Feliciano J, Richhariya A, LeBlanc TW: Patient-reported distress in Hodgkin lymphoma across the survivorship continuum. Support Care Cancer 2019;27(7):2453–2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lazzarino AI, Hamer M, Stamatakis E, Steptoe A. Low socioeconomic status and psychological distress as synergistic predictors of mortality from stroke and coronary heart disease. Psychosom Med April 2013; 75(3):311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norris K, Nissenson AR. Race, gender, and socioeconomic disparities in CKD in the United States. J Am Soc Nephrol 2008;19(7):1261–1270. [DOI] [PubMed] [Google Scholar]
- 5.Flythe JE, Dorough A, Narendra JH, Forfang D, Hartwell L, Abdel-Rahman E. Perspectives on symptoms experiences and symptom reporting among individuals on hemodialysis. Nephrol Dial Transplant October 2018;33(10):1842–1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molnar MZ, Streja E, Sumida K, Soohoo M, Ravel VA, Gaipov A, Potukuchi PK, Thomas F, Rhee CM, Lu JL, Kalantar-Zadeh K, Kovesdy CP. Pre-ESRD depression and post-ESRD mortality in patients with advanced CKD transitioning to dialysis. Clin J Am Soc Nephrol September 7 2017;12(9):1428–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rees J, Chilcot J, Donellan W, Soulsby L. Exploring the nature of illness perceptions in people with end-stage kidney disease. J Ren Care March 2018;44(1):19–29. [DOI] [PubMed] [Google Scholar]
- 8.Maliski SL, Connor SE, Williams L, Litwin MS. Faith among low-income African American/Black Men Treated for Prostate Cancer. Cancer Nurs Nov-Dec 2010;33(6):470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wright AW, Yendork JS, Kliewer W. Patterns of spiritual connectedness during adolescence: links to coping and adjustment in low-income urban youth. J Youth Adolesc December 2018;47(12):2608–2624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zavala MW, Maliski SL, Kwan L, Fink A, Litwin MS. Spirituality and quality of life in low-income men with metastatic prostate cancer. Psychooncology July 2009;18(7):753–761. [DOI] [PubMed] [Google Scholar]
- 11.Beck JS. (2011). Cognitive Behavior Therapy: Basics and Beyond (2nd ed), New York, NY: The Guilford Press, 19–20. [Google Scholar]
- 12.Magidson JF, Weisberg RB. Implementing cognitive behavioral therapy in specialty medical settings. Cogn Behav Pract November 2014;24(4):367–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teasdale EJ, Leydon G, Fraser S, Roderick P, Taal MW, Tonkin-Crine S. Patients’ experiences after CKD diagnosis: a meta-ethnographic study and systematic review. Am J Kidney Dis November 2017;70(5):656–665. [DOI] [PubMed] [Google Scholar]
- 14.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care December 2007; 19(6):349–357. [DOI] [PubMed] [Google Scholar]
- 15.Kleinman A Patients and healers in the context of culture: an exploration of the borderland between anthropology, medicine, and psychiatry. Berkeley, CA: University of California Press, 1980. [Google Scholar]
- 16.Leventhal H, Phillips LA, Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med December 2016;39(6):935–946. [DOI] [PubMed] [Google Scholar]
- 17.Joosten YA, Israel TL, Williams NA, Boone LR, Schlundt DG, Mouton CP, Dittus RS, Bernard GR, Wilkins CH. Community engagement studios: a structured approach to obtaining meaningful input from stakeholders to inform research. Acad Med December 2015; 90(12):1646–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saunders B, Sim J, Kingstone T, Baker S, Waterfield J, Bartlam B, Burroughs H, Jinks C. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52(4):1893–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tjora A Qualitative research as a stepwise-deductive induction: a stepwise-deductive inductive approach. London, UK: Routledge, 2018. [Google Scholar]
- 20.Fereday J, Muir-Cochrane E: Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:1–11.20. [Google Scholar]
- 21.International Business Machines (IBM) Corporation. Released 2017 IBM Statistical Package for the Social Sciences (SPSS) Statistics for Windows, Version 25.0 Armonk, NY: IBM Corporation. [Google Scholar]
- 22.United States Department of Housing and Urban Development. Office of Policy Development and Research. Available at: https://www.huduser.gov/portal/datasets/il/fmr98/sect8.html. Accessed on June 25, 2020.
- 23.United States Census Bureau. Quick Facts: Nashville-Davidson. Available at: https://www.census.gov/quickfacts/fact/table/nashvilledavidsonbalancetennessee/INC110218. Accessed on June 25, 2020.
- 24.Groves MS, Muskin PR. Psychological response to illness The American psychiatric publishing textbook of psychosomatic medicine, Washington, DC: American Psychiatric Publishing, Inc, 2005. [Google Scholar]
- 25.Iverach L, Menzies RG, Menzies RE. Death anxiety and its role in psychopathology: reviewing the status of a transdiagnostic construct. Clin Psychol Review November 2014; 34(7):580–593. [DOI] [PubMed] [Google Scholar]
- 26.Neel C, Lo C, Rydall A, Hales S, Rodin G. Determinants of death anxiety in patients with advanced cancer. BMJ Support Palliat Care December 2015;5(4):73–380. [DOI] [PubMed] [Google Scholar]
- 27.Cervantes L, Fischer S, Berlinger N, Zabalaga M, Camacho C, Linas S, Ortega D. The illness experience of undocumented immigrants with end-stage renal disease. JAMA Intern Med April 2017;177(4):529–535. [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez AM, Gutman T, Lopez-Vargas P, Anumudu S, Arce CM, Craig JC, Dunn L, Eckardt K, Harris T, Levey AS, Lightstone L, Scholes-Robertson N, Shen JI, Teixeira-Pinto A, Wheeler DC, White D, Wilkie M, Jadoul M, Winkelmayer WC, Tong A. Am J Kidney Dis May 31 2020; S0272-6386(20):30719–30728. [DOI] [PubMed] [Google Scholar]
- 29.Hanson CS, Gutman T, Craig JC, Bernays S, Raman G, Zhang Y, James LJ, Ralph AF, Ju A, Manera KE, Teixeira-Pinto A, Viecelli AK, Alexander SI, Blydt-Hansen TD, Dionne J, McTaggart S, Michael M, Walker A, Carter S, Wenderfer SE, Winkelmayer WC, Bockenhauer D, Dart A, Eddy AA, Furth SL, Gipson DS, Goldstein SL, Groothoff J, Samuel S, Sinha A, Webb NJA, Yap HK, Zappitelli M, Currier H, Tong A. Identifying important outcomes for young people with CKD and their caregivers: a nominal group technique study. Am J Kidney Dis July 2019;74(1): 82–94. [DOI] [PubMed] [Google Scholar]
- 30.Gramling R, Stanek S, Han PKJ, Duberstein P, Quill TE, Temel JS, Alexander SC, Anderson WG, Ladwig S, Norton SA. Distress due to prognostic uncertainty in palliative care: frequency, distribution, and outcomes among hospitalized patients with advanced cancer. J Palliat Med March 2018; 21(3):315–321. [DOI] [PubMed] [Google Scholar]
- 31.Tuot DS, Zhu Y, Velasquez A, Espinoza J, Mendez CD, Banerjee T, Hsu CY, Powe NR. Variation in patients’ awareness of CKD according to how they are asked. Clin J Am Soc Nephrol September 7 2016;11(9):1566–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizler TA, Cavanaugh KL. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int December 2011;80(12):1344–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tangri N, Stevens LA Griffith J, Tighiouart H, Djurdjev O, Naimark D, Levin A, Levey AS. A predictive model for progression of chronic kidney disease to kidney failure. JAMA 2011. 305(15):1553–1559. [DOI] [PubMed] [Google Scholar]
- 34.Kissanw DW. Psychospiritual and existential distress: the challenge for palliative care. Aust Fam Physician November 2000; 29(11):1022–1025. [PubMed] [Google Scholar]
- 35.Behling S, Kissane DW. Existential distress in cancer: alleviating suffering from fundamental loss and change. Psychooncology November 2018; 27(11):2525–2530. [DOI] [PubMed] [Google Scholar]
- 36.Breitbart W, Rosenfeld B, Pessin H, Kaim M, Funesti-Esch J, Galietta M, Nelson CJ, Brescia R. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA December 2000. 284(22):2907–2911. [DOI] [PubMed] [Google Scholar]
- 37.Cherny NI, Coyle N, Foley KM. Suffering in the advanced cancer patient: a definition and taxonomy. J Palliat Care 1994. 10(2):57–70. [PubMed] [Google Scholar]
- 38.Soleimani MA, Bahrami N, Zarabadi-Pour S, Motalebi SA, Parker A, Chan YH. Predictors of death anxiety among patients with heart disease. Death Stud 2020. 44(3):160–167. [DOI] [PubMed] [Google Scholar]
- 39.Byrne CM, Morgan DD. Patterns of religiosity, death anxiety, and hope in a population of community-dwelling palliative care patients in New Zealand – what gives hope if religion can’t? Am J Hosp Palliat Care 2020. 37(5):377–384. [DOI] [PubMed] [Google Scholar]
- 40.Taghiabadi M, Kavosi A, Mirhafez SR, Keshvari M, Mehrabi T. The association between death anxiety with spiritual experiences and life satisfaction in elderly people. Electron Physician March 2017; 9(3): 3980–3985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pyszczynski T, Greenberg J, Solomon S. A dual-process model of defense against conscious and unconscious death-related thoughts: an extension of terror management theory. Psychol Rev. 1999;106(4): 835–845. [DOI] [PubMed] [Google Scholar]
- 42.Davison SN, Jhangri GS. Existential and supportive care needs among patients with chronic kidney disease. J Pain Symptom Manage December 2010; 40(6):838–843. [DOI] [PubMed] [Google Scholar]
- 43.Pham TA, Beasley CM, Gagliardi JP, Koenig HG, Stanifer JW. Spirituality, coping, and resilience among rural residents living with chronic kidney disease. J Relig Health August 7. doi: 10.1007/s10943-019-00892-w, 2019. [DOI] [PubMed] [Google Scholar]
- 44.Al-Ghabeesh SH, Alshraifeen AA, Saifan AR, Bashayreh IH, Alnuami KM, Masalha HA. Spirituality in the lives of patients with end-stage renal disease: a systematic review. J Relig Health December 2018;57(6):2461–2477. [DOI] [PubMed] [Google Scholar]
- 45.Davison SN, Jhangri GS The relationship between spirituality, psychosocial adjustment to illness, and health-related quality of life in patients with advanced chronic kidney disease. J Pain Symptom Manage February 2013; 45(2):170–178. [DOI] [PubMed] [Google Scholar]
- 46.Elliott BA, Gessert CE, Larson P, Russ TE. Religious beliefs and practices in end-stage renal disease: implications for clinicians. J Pain Symptom Manage September 2012;44(3): 400–409. [DOI] [PubMed] [Google Scholar]
- 47.Spinale J, Cohen SD, Khetpal P, Peterson RA, Clougherty B, Puchalski CM, Patel SS, Kimmel P. Spirituality, social support, and survival in hemodialysis patients. Clin J Am Soc Nephrol November 2008; 3(6):1620–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van der Spek N, Vos J, Van Uden-Kraan CF, Breitbart W, Cuijpers P, Holtmaat K, Witte BI, Tollenaar RAEM, Verdonck-de Leeuw IM. Efficacy of meaning-centered group psychotherapy for cancer survivors: a randomized controlled trial. Psychol Med August 2017; 47(11): 1990–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johns SA, Stutz PV, Talib TL, Cohee AA, Back-Coon KA, Brown LF, Wilhelm LR, Monahan PO, LaPradd ML, Champion VL, Miller KD, Giesler RB. Acceptance and commitment therapy for breast cancer survivors with fear of cancer recurrence: a 3-arm pilot randomized controlled trial. Cancer Jan 2020; 126(1):211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maheu C, Lebel S, Courbasson C, Lefebvre M, Singh M, Bernstein LJ, Muraca L, Benea A, Jolicoeur L, Harris C, Ramanakumar AV, Ferguson S, Sidani S. Protocol of a randomized controlled trial of the fear of recurrence therapy (FORT) intervention for women with breast or gynecological cancer. BMC Cancer April 15 2016;16:291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chronic Kidney Disease in the United States. Centers for Disease Control and Prevention. Available from: https://www.cdc.gov/kidneydisease/publications-resources/2019-national-facts.html. Accessed February 28, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


