Abstract
Context
Accurate prognostic understanding is associated with increased advance care planning, symptom control, and patient autonomy in oncology. The impact of prognostic understanding on patients’ health and prognostic information preferences (HIPs) is unknown and has important implications for healthcare communication.
Objectives
The present study: 1) characterized the HIPs of patients with advanced cancer; 2) examined differences in HIPs between patients with varying curability beliefs and; 3) identified differences in the characteristics and psychological well-being of patients with varying curability beliefs.
Methods
This cross-sectional study utilized a secondary data analysis of baseline data (prerandomization) for patients enrolled in a large randomized, controlled psychotherapy trial. 206 participants were recruited from outpatient clinics at a single facility. Inclusion criteria: ≥18 years old, English-speaking, stage-IV solid tumor cancer, Distress Thermometer score ≥4.
Results
Most participants preferred as many details as possible about their cancer, treatment (69.4%, n=143), and likely outcome of their disease (72.3%, n=149). Most participants accurately described their cancer as unlikely curable or incurable (62.6%, n=129). There were no significant differences in HIPs based on level of prognostic understanding. Poorer prognostic understanding was associated with religiosity and better quality of life and existential well-being.
Conclusion
In the present study, prognostic understanding (i.e., curability beliefs) was not associated with HIPs. Therefore, oncology clinicians must evaluate patients’ interest and preferences for receiving information. Future research should further clarify preferences for the framing and content of prognostic information from providers and improve the measurement of prognostic understanding to facilitate patient-centered end of life care.
Keywords: Prognosis, Communication, Neoplasms, Attitude to Death, Patient Preference
Introduction
Research regarding prognostic understanding in patients with advanced cancer has garnered increasing attention in palliative care.1 A growing number of studies document the positive association between accurate prognostic understanding and increased advance care planning,2–5 symptom control, and patient autonomy.1–8 Accurate prognostic understanding has also been associated with decreased hospital admissions and fewer aggressive life-prolonging interventions at end-of-life.4–6,8 However, many patients over-estimate their life expectancy and/or the likely outcome of their disease, with up to 75% of patients demonstrating poor prognostic understanding.1 This is often a result of patients’ underestimation of the severity of their disease and overestimation of its treatability and their life expectancy.1,9 Moreover, there is no “gold standard” for measuring prognostic understanding, further complicating research and clinical practice in this area.1,9
Although there is increasing recognition of the importance of accurate prognostic understanding, and in particular, its relationship to medical care,10 research on patient preferences for prognostic information, or health information preferences more generally (HIPs), is still understudied.1,5,11 Specifically, while frank discussions of cancer and its treatment have grown less stigmatized, there are no established best practices for communicating prognostic information in a way that is responsive to patients’ needs and preferences. Moreover, these needs and preferences may change throughout the cancer continuum (i.e., as the disease and/or treatment progresses). A systematic review of the literature concluded that patients with advanced cancer tended to prefer prognostic information, but that even with this information, a significant subset wanted their clinicians to “leave room for hope,” or to acknowledge the uncertainty around the anticipated outcome of the disease.5 The term “open door prognosis” has been aptly used to characterize these communication preferences.5,12
The relationship between accurate prognostic understanding and psychological well-being also remains equivocal. Many studies have found accurate prognostic understanding to be associated with greater quality of life and spiritual well-being,4,6–7,13 as well as decreased anxiety and psychological distress.4–6,8,14–15 However, some have identified the opposite relationship, with accurate prognostic understanding being associated with increased depression and anxiety and decreased quality of life.16–17 Indeed, many patients (and clinicians) refer to the open door prognosis as a technique to “keep hope alive.” Despite this, patients have typically identified increased hope, control, trust, coping and satisfaction with care as potential benefits of increased prognostic understanding.5
Additional research is needed to better understand the potential differences in HIPs between patients with advanced cancer who categorize their disease as incurable compared to those who identify their illness as curable. This research would help address the impact of improved communication around prognostic information and specifically, whether or not information delivery should be tailored based on an individual’s level of prognostic understanding. Thus, the purpose of the present study was to: 1) characterize the HIPs of patients with advanced cancer; 2) examine differences in the HIPs of patients with varying curability beliefs; and 3) identify differences in the characteristics and psychological well-being of patients with varying curability beliefs.
Method
Patients with advanced cancer (N=206) were recruited from outpatient oncology clinics between March of 2011 and March of 2016 to participate in a randomized controlled trial (RCT) comparing two psychotherapies and usual care.18 Participants wereat least 18 years old, English speaking, and had stage IV solid tumor cancer or other cancer diagnoses with poor prognosis (e.g., locally advanced but unresectable cancer, confirmed in electronic medical record (EMR)). Prospective participants were screened using the Distress Thermometer,19 and only those who indicated at least moderate distress (≥4) were included. Exclusion criteria were the presence of significant cognitive impairment or psychotic symptoms (based on clinician assessment). Potential participants were informed of the study risks and benefits and provided written informed consent. The study was approved by the Institutional Review Boards of MSK and Fordham University. The full study from which the current data are derived is registered at clinicaltrials.gov (#NCT01323309).
Participants were administered a series of questionnaires prior to beginning treatment, including the FACIT Spiritual Well-Being Scale (FACIT-SP),20 the Life Attitude Profile-Revised (LAP-R),21 the McGill Quality of Life Questionnaire (MQOL),22 the Hospital Anxiety and Depression Scale (HADS),23 the Hopelessness Assessment in Illness questionnaire (HAI),24 and the Schedule of Attitudes toward Hastened Death (SAHD).25 Several months after the study began, a pre-treatment Health Information Preferences (HIP) questionnaire was added to elicit information preferences, satisfaction, and participant awareness of their prognosis. The items comprising this measure are drawn from the Prognosis and Treatment Perceptions Questionnaire (PTPQ), which has been validated and undergone cognitive interviewing with patients with metastatic cancer (see Table 2 for a list of individual items).11, Prognostic awareness was based on responses to the question “How would you describe your current disease status?”, with response options curable, likely curable, unlikely curable, and incurable.
Table 2.
Participant Health Information Preferences
| Information Preference | n (%) |
|---|---|
| Details of information about your diagnosis and treatment | |
| I prefer not to hear a lot of details | 11 (5.3) |
| I want to hear details only in certain situations | 46 (22.3) |
| I want to hear as many details as possible in all situations | 143 (69.4) |
| Missing | 6 (2.9) |
| Importance of knowing your prognosis | |
| Extremely important | 89 (43.2) |
| Very important | 60 (29.1) |
| Somewhat important | 26 (12.6) |
| A little important | 19 (9.2) |
| Not at all important | 7 (3.4) |
| Missing | 5 (2.4) |
| Satisfaction with amount of information about your prognosis | |
| I wish I had more information about my prognosis | 75 (36.4) |
| I now have about the right amount of information | 118 (57.3) |
| I wish I had less information about my prognosis | 9 (4.4) |
| Missing | 4 (1.9) |
| Quality of information about your prognosis | |
| Excellent | 77 (37.4) |
| Good | 63 (30.6) |
| Satisfactory | 45 (21.8) |
| Fair | 15 (7.3) |
| Poor | 1 (0.5) |
| Missing | 5 (2.4) |
| Description of your current disease status | |
| Curable | 22 (10.7) |
| Likely curable | 39 (18.9) |
| Unlikely curable | 63 (30.6) |
| Incurable | 66 (32.0) |
| Missing | 16 (7.8) |
| Current feeling about your disease status | |
| Mostly at peace | 25 (12.1) |
| Somewhat at peace | 28 (13.6) |
| Neutral | 33 (16.0) |
| Somewhat distressed | 89 (43.2) |
| Very distressed | 28 (13.6) |
| Missing | 3 (1.5) |
Note. Items listed reflect the items included on the Health Information Preferences (HIP) Questionnaire.
Spearman rank correlation coefficients (rs) were computed to examine the strength of the relationships between study variables. Chi-square tests of association were utilized to examine potential demographic differences between participants who described their illness as curable or likely curable compared to those who considered their illness likely incurable or incurable. This dichotomizing approach has been consistently utilized in this line of research as method to gauge prognostic understanding.11 Independent samples t-tests evaluated differences between these two groups (curable versus incurable) on psychosocial outcomes. Cohen’s d is reported as an indicator of effect size. All analyses were conducted in SPSS version 25.26 An alpha level of .05 was set for all statistical tests. Missing data was minimal across study variables and pairwise deletion was utilized across analyses.
Results
Participant Characteristics
Participants were predominately female (73.8%; n=152) and ranged in age from 25 to 82 years old (M=59.1, SD=10.9; Table 1). Most participants were white (79.1%; n=163) and 7.8% (n=16) identified as Hispanic. The majority were partnered (69.4%; n=143) and had a college and/or graduate education (72.3%; n=151). The most common cancer diagnoses were gynecological (23.9%; n=49), pancreatic (15.5%; n=32), and lung (14.6%; n=30). The majority of participants were undergoing chemotherapy at the time of participation (71.8%; n=148).
Table 1.
Participant Characteristics
| Characteristic | M (SD) | n (%) |
|---|---|---|
| Age | 59.28 (10.9) | |
| Sex | ||
| Male | 54 (26.2) | |
| Female | 152 (73.8) | |
| Race | ||
| Caucasian | 163 (79.1) | |
| African American | 23 (11.2) | |
| Asian | 7 (3.4) | |
| American Indian/Alaskan Native | 1 (0.5) | |
| Other/unknown | 12 (5.8) | |
| Ethnicity | ||
| Hispanic/Latino | 16 (7.8) | |
| Not Hispanic/Latino | 188 (91.3) | |
| Other/Unknown | 2 (1.0) | |
| Identify as Religious | ||
| Not at all | 81 (39.3) | |
| Somewhat | 65 (31.6) | |
| Yes, very much | 58 (28.2) | |
| Not provided | 2 (1.0) | |
| Marital Status | ||
| Single | 31 (15.0) | |
| Married/living with partner | 128 (62.1) | |
| Widowed | 21 (10.2) | |
| Separated/divorced | 26 (12.6) | |
| Highest Education | ||
| High school | 24 (11.7) | |
| Some college | 31 (15.0) | |
| College or greater | 151 (73.3) | |
| Cancer Diagnosis | ||
| Breast | 26 (12.6) | |
| Colon/rectum | 27 (13.1) | |
| Genitourinary | 4 (1.9) | |
| Lung/bronchus | 30 (14.6) | |
| Pancreas | 32 (15.5) | |
| Stomach | 10 (4.9) | |
| Ovary | 37 (18.0) | |
| Uterine cervix/corpus | 12 (5.8) | |
| Other | 14 (6.8) | |
| Status of Chemotherapy | ||
| Within last 3 months | 29 (14.1) | |
| Currently | 148 (71.8) | |
| Upcoming | 4 (1.9) | |
| Missing | 25 (12.1) |
Health Information Preferences (HIPs)
Nearly three quarters (69.4%, n=143) of participants indicated a preference for as many details as possible about their cancer and its treatment, while only 5.3% (n=11) preferred not to hear a lot of details (Table 2). Similarly, 72.3% (n=149) of participants stated that it was very or extremely important to them to know about the likely outcome of their cancer and its treatment (i.e., prognosis), with only 12.6% (n=26) stating that prognostic information was only a little or not at all important to them. Satisfaction with cancer-related information varied across the sample, with over one third of participants stating they wished they had more information about their prognosis (36.4%, n=75), and 57.3% (n=118) reported feeling they had about the right amount. Nevertheless, most participants described the quality of the information about prognosis that they had received as satisfactory or better (89.8%, n=185).
Disease Curability Beliefs
Most participants described their cancer as unlikely curable or incurable (62.6%, n=129), indicating a generally accurate understanding of their prognosis. Similarly, over half of participants (56.8%, n=117) were somewhat or very distressed about their disease status. Chi-square analyses revealed significant demographic differences between those who identified their disease as incurable/unlikely curable versus curable/likely curable. While there were no significant differences observed between racial groups, Hispanic participants were significantly more likely to identify their disease as curable or likely curable compared to non-Hispanic participants (71.4% vs. 28.6%, X2 (2, N=190)=13.05, p=.0015). Significantly more participants who identified as having unlikely curable or incurable disease were significantly more likely to describe themselves as not at all religious compared to those in the curable/likely curable group (80.3% vs. 19.7%, X2 (2, N=188)=8.83, p=.012).
HIPs did not differ between curability belief groups (i.e., at the item-level). Preferences for prognostic information, as well as satisfaction with the amount and quality of information one had regarding prognosis, did not vary significantly between groups. Similarly, there were no significant differences between groups in how important they felt prognostic information was.
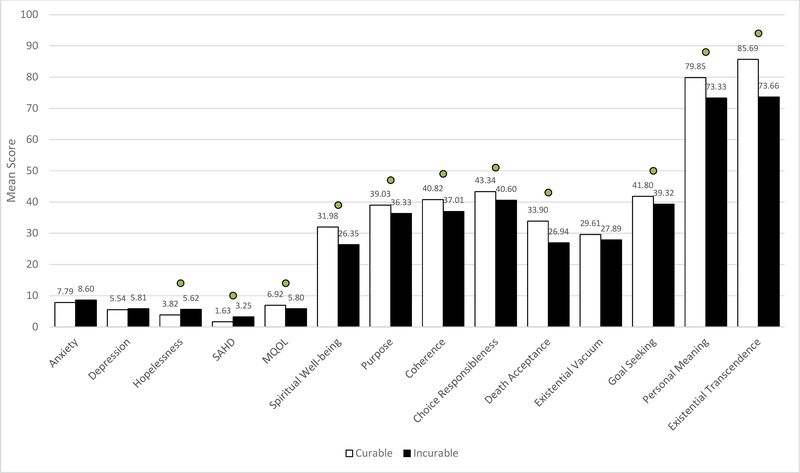
Independent samples t-tests revealed that several psychosocial variables differed significantly between curability groups. For example, participants who identified as curable/likely curable endorsed better psychological quality of life (MQOL: d=0.45, t(187)=2.90, p=.004) and spiritual well-being (FACIT: d=0.64, t(188)=4.09, p=.0001), and obtained higher scores on 7 out of 8 subscales of the LAP-R, including Death Acceptance (d=0.60, t(188)=3.78, p=.0002; Figure 1). Those who identified as unlikely curable/incurable endorsed greater hopelessness (HAI: d=0.57, t(188)=-3.61, p=.0004) and desire for hastened death (SAHD: d=0.64, t(187)=-3.81, p=.0002). There were no significant differences in depression (HADS-D: d=0.08 t(188)=0.53, p=.60) or anxiety (HADS-A: d=0.21, t(188)=-1.33, p=.19) between disease curability belief groups.
Figure 1. Psychological wellbeing and quality of life across curability groups.
Note. Means marked with a circle indicate statistically significant differences at ≤.05. Anxiety and Depression (HADS-A and HADSD subscales); Hopelessness (HAI); SAHD=Desire for Hastened Death; MQOL=Psychological Quality of Life; Meaning and Faith (FACIT-SP); Purpose, Coherence, Choice Responsibleness, Death Acceptance, Existential Vacuum, Goal Seeking, Personal Meaning, and Existential Transcendence (subscales of the LAP-R).
Discussion
The current study sought to characterize the prognostic health information preferences (HIPs) of patients with advanced cancer and to identify potential differences in HIPs and psychological well-being between those who identify as having curable or incurable cancer. The majority of participants in the current study expressed interest in having as much information as possible about their cancer, its treatment, and the likely outcome of their disease. Specifically, prognostic information was rated as very or extremely important by over 70% of participants. Although most participants reported that the quality of the prognostic information they had been given was satisfactory or better, nearly one third of the sample stated they wished they had more information about their prognosis. These observations are consistent with previous findings in patients with earlier stages of disease.11
A number of significant associations were observed between HIPs and distress, including the negative association between distress related to disease status and satisfaction with the quality of prognostic information they had received. Distress may drive some patients to seek out as much information as possible about their illness, as they may equate information with a sense of control, especially during periods of prognostic uncertainty. Conversely, it is also possible that patients who are dissatisfied with the information their provider has communicated, or who interpret a lack of sufficient information as indicating a poor prognosis, might have greater distress about the state of their illness. Patient distress may also impact physician communication patterns, as clinicians may limit the information they share if they perceive the patient as highly distressed. Therefore, while the direction of this relationship cannot be determined based on the current correlational analyses, it is likely influenced by patient, clinician, and disease characteristics.
Although all patients in this study had advanced, and likely incurable disease (i.e., verified in EMR), more than one quarter (29.6%) described their disease as curable or likely curable. This subgroup would be considered to have less prognostic understanding than those who characterized their illness as unlikely curable or incurable. Notably, however, patient preferences for prognostic information, and satisfaction with the amount and quality of prognostic information did not differ between these two groups. This suggests that those with less prognostic understanding were not necessarily avoidant of prognostic information. Instead, it highlights the importance of patient-centered prognostic communication. Oncology clinicians must evaluate their patients’ level of interest and preferences for receiving information without making assumptions.11–12,27–29
Those participants with less prognostic understanding were more likely to describe themselves as religious. It is possible that having more salient religious beliefs counters identifying one’s disease as “incurable.” For example, a belief that God controls the outcome of the disease or miracles can change the course of an illness may deter the patient from perceiving their illness as incurable. Although they did not evaluate prognostic understanding, Balboni and colleagues30,31 found that among patients with advanced cancer, higher levels of religiosity were associated with less advanced care planning, more aggressive treatment, and a greater likelihood of dying in the ICU.
Finally, across several psychological and quality of life variables, those participants with greater prognostic understanding reported worse quality of life and spiritual well-being, and higher levels of hopelessness and desire for hastened death. The absence of differences in depression and anxiety between the two groups diverges from several past studies. For example, Chochinov et al.13 found that, among patients with cancer in their final weeks of life, depression was three times higher in those who did not acknowledge their prognosis compared to those with partial or complete knowledge. This could also be due to measurement differences, as the current study did not use a diagnostic interview, but rather a screening measure for depression. Similarly, a restricted range of depression scores, which tended to be low, could also account for no observed relationship between depression and prognostic understanding. Notably, these findings highlight the resiliency of many patients facing an advanced cancer diagnosis, as despite distress, most are not depressed, and most still desire more information about their disease.
Limitations and Future Directions
Several sampling limitations restrict the generalizability of the present findings. First, the sample was relatively homogenous ethnically, racially, and socioeconomically. Therefore, there was limited power to examine some of the potential demographic differences in health information preferences and curability beliefs. This is an important ongoing area of research and warrants closer consideration in future studies involving patients at the end of life. Similarly, as the current paper represents secondary data analysis from a primary RCT, the requirement that all participants endorse at least moderate distress and express interest in receiving psychotherapy may have impacted study results. For example, patients who express interest in psychotherapy may desire more information related to their prognosis that patients who decline the opportunity to participate in psychotherapy. The responses and relationships reported, therefore, may not represent the potential full range of responses that might be observed in a more general sample.
There may also be semantic and other measurement considerations that make obtaining a patient’s accurate prognostic understanding challenging, as this construct can be interpreted in several ways. Even in the presence of adequate prognostic understanding, the term “curable” may be interpreted by patients in a way that does not only reflect medical prognosis. The HIP questionnaire utilized in the current study might be interpreted by patients in ways that were not anticipated. Therefore, further research should address whether there are better methods for measuring this construct.32 Similarly, clinicians themselves often have a challenging time accurately prognosticating and this can create even more clinical ambiguity.33 Finally, it is also possible that these findings were impacted by selection bias, as participants were drawn from a single comprehensive cancer care institution where patients often travel from great distances to receive state-of-the-art care. Thus, this setting may over-represent patients who are open to talking about their disease and desire as much treatment-related information as possible.
Due to the cross-sectional design and limitations of the health information preferences questionnaire, only preliminary interpretations about the observed relationships can be made. However, future research should determine whether there are nuanced differences in patient preferences for the framing and content (versus quality and amount) of prognostic information received from providers based on one’s prognostic understanding. Finally, accurate measurement of prognostic understanding should be a priority in palliative care, as it will enhance the ability of clinicians to navigate these complexities and accurately tailor communication to meet patients’ unique needs throughout the illness trajectory, thus facilitating more efficient and patient-centered care at the end of life.
Supplementary Material
Key Message.
This article describes a cross-sectional evaluation of the previously unstudied relationship between curability beliefs (i.e. prognostic understanding), health information preferences, and psychological functioning among patients with advanced cancer. The results indicate that there are no significant differences in health information preferences based on prognostic understanding.
Disclosures and Acknowledgements
The entire study team reports support from grants from the National Cancer Institute during the conduct of the study and/or preparation of the manuscript.
This research was supported with funding from the National Cancer Institute: R01CA128134, T32CA009461, and P30CA008748.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Applebaum AJ, Kolva E A, Kulikowski JR, et al. Conceptualizing prognostic awareness in advanced cancer: A systematic review. J Health Psychol. 2014; 19(9):1103–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradley EH, Hallemeier AG, Fried TR, et al. Documentation of discussions about prognosis with terminally ill patients. Am J Med. 2001; 111(3):218–223. [DOI] [PubMed] [Google Scholar]
- 3.Mack JW, Nilsson M, Balboni T, et al. Peace, equanimity, and acceptance in the cancer experience (PEACE): Validation of a scale to assess acceptance and struggle with terminal illness. Cancer. 2008; 112(11):2509–2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008; 300(14):1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Innes S, Payne S. Advanced cancer patients’ prognostic information preferences: A review. Palliat Med. 2009; 23(1):29–39. [DOI] [PubMed] [Google Scholar]
- 6.Justo Roll I, Simms V, Harding R. Multidimensional problems among advanced cancer patients in Cuba: Awareness of diagnosis is associated with better patient status. J Pain Symptom Manage. 2009; 37(3):325–330. [DOI] [PubMed] [Google Scholar]
- 7.Leung K, Chiu T, Chen C. The influence of awareness of terminal condition on spiritual well-being in terminal cancer patients. J Pain Symptom Manage. 2006; 31(5): 449–456. [DOI] [PubMed] [Google Scholar]
- 8.Thompson GN, Chochinov HM, Wilson KG, et al. Prognostic acceptance and the well-being of patients receiving palliative care for cancer. J Clin Oncol. 2009; 27(34):5757–5762. [DOI] [PubMed] [Google Scholar]
- 9.Chen CH, Kuo SC, Tang ST. Current status of accurate prognostic awareness in advanced/terminally ill cancer patients: Systematic review and meta-regression analysis. Palliat Med. 2017; 31(5):406–418. [DOI] [PubMed] [Google Scholar]
- 10.Diamond EL, Prigerson HG, Correa DC, et al. Prognostic awareness, prognostic communication, and cognitive function in patients with malignant glioma. Neuro Oncol. 2017; 19(11):1532–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Jawahri A, Traeger L, Park ER, et al. Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer. 2014; 120(2):278–85. [DOI] [PubMed] [Google Scholar]
- 12.Johnson M, Tod AM, Brummell S, Collins K. Prognostic communication in cancer: a critical interpretive synthesis of the literature. Eur J Oncol Nurs. 2015; 19(5):554–67. [DOI] [PubMed] [Google Scholar]
- 13.Chochinov HM, Tataryn DJ, Wilson KG, Ennis M, Lander S. Prognostic a wareness and the terminally ill. Psychosomatics. 2000; 41(6):500–504. [DOI] [PubMed] [Google Scholar]
- 14.Kutner JS, Steiner JF, Corbett KK, Jahnigen DW, Barton PL. Information needs in terminal illness. Soc Sci Med. 1999; 48(10):1341–1352. [DOI] [PubMed] [Google Scholar]
- 15.Helft PR, Hlubocky F, Wen M, Daugherty CK. Associations among awareness of prognosis, hopefulness, and coping in patients with advanced cancer participating in phase I clinical trials. Support Care Cancer. 2003; 11(10):644–651. [DOI] [PubMed] [Google Scholar]
- 16.Shin JA, El-Jawahri A, Parkes A, Schleicher SM, Knight HP, Temel JS. Quality of life, mood, and prognostic understanding in patients with metastatic breast cancer. J Palliat Med. 2016; 19(9):863–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nipp RD, Greer JA, El-Jawahri A, et al. Coping and prognostic awareness in patients with advanced cancer. J Clin Oncol. 2017; 35(22):2551–2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Breitbart W, Pessin H, Rosenfeld B, et al. Individual meaning-centered psychotherapy for the treatment of psychological distress: A randomized controlled trial in patients with advanced cancer. Cancer. 2018; 124(15):3231–3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer. 1998; 82(10):1904–8. [DOI] [PubMed] [Google Scholar]
- 20.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med. 2002; 24(1):49–58. [DOI] [PubMed] [Google Scholar]
- 21.Reker GT. The Life Attitude Profile-Revised:(LAP-R). Peterborough, Ontario, Canada: Student Psychologists Press; 2001. [Google Scholar]
- 22.Cohen SR, Sawatzky R, Russell LB, Shahidi J, Heyland DK, Gadermann AM. Measuring the quality of life of people at the end of life: The McGill Quality of Life Questionnaire– Revised. Palliat Med. 2017; 31(2):120–9. [DOI] [PubMed] [Google Scholar]
- 23.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–70. [DOI] [PubMed] [Google Scholar]
- 24.Rosenfeld B, Pessin H, Lewis C, et al. Assessing hopelessness in terminally ill cancer patients: Development of the Hopelessness Assessment in Illness Questionnaire. Psychol Assess. 2011; 23(2):325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosenfeld B, Breitbart W, Galietta M, et al. The schedule of attitudes toward hastened death: Measuring desire for death in terminally ill cancer patients. Cancer. 2000; 88(12):2868–75. [DOI] [PubMed] [Google Scholar]
- 26.IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0 [software]. Armonk, NY: IBM Corp. [Google Scholar]
- 27.Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007; 34(1):81–93. [DOI] [PubMed] [Google Scholar]
- 28.Bernacki RE, Block SD. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994–2003. [DOI] [PubMed] [Google Scholar]
- 29.Smith CB, Phillips T, Smith TJ. Using the new ASCO clinical practice guideline for palliative care concurrent with oncology care using the TEAM approach. Am Soc Clin Oncol Educ Book. 2017; 37:714–23. [DOI] [PubMed] [Google Scholar]
- 30.Balboni TA, Balboni M, Enzinger AC, et al. Provision of spiritual support to patients with advanced cancer by religious communities and associations with medical care at the end of life. JAMA Intern Med. 2013; 173(12):1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010; 28(3):445–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Masterson MP, Applebaum AJ, Buda K, Reisch S, Rosenfeld B. Don’t Shoot the Messenger: Experiences of delivering prognostic information in the context of advanced cancer. Am J Hosp Palliat Care. 2018; 35(12):1526–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lamont EB, Christakis NA. Complexities in prognostication in advanced cancer: To help them live their lives the way they want to. JAMA. 2003;290(1):98–104. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.