Abstract
Acute treatment of Generalized Anxiety Disorder often requires 3 months or more of care in order to optimize response. As part of an exploratory grant we have previously demonstrated that six weeks of twice-weekly Swedish Massage Therapy (SMT) was more effective than an active control in decreasing Hamilton Anxiety Rating Scale Scores (HAM-A). An additional goal of this project was to determine if an additional six weeks of twice-weekly SMT led to greater clinical and statistical benefit. We found that HAM-A scores did continue to decrease with an additional six weeks of therapy but that the greatest benefit occurred during the first versus the second 12 sessions (−9.91 vs. −3.09, t=2.21; df=10; p=0.052). These preliminary findings suggest that the majority of benefit in symptom reduction occurs in the first six weeks and that six weeks of twice-weekly SMT may be sufficient for the majority of patients.
Keywords: Swedish Massage, Generalized Anxiety Disorder, Dose, Anxiety, Treatment
1. Introduction
Generalized Anxiety Disorder (GAD) has a prevalence rate of 5.8% and is characterized by a constellation of both physical and psychological symptoms.1–3 Relief from anxiety and stress are two of the most common reasons people seek out complementary and alternative medicine (CAM) treatments4–6, with massage as one of the most frequently employed therapies for anxiety.1, 7 In fact, 43% of participants in the Coordinated Anxiety Learning and Management study endorsed using some form of CAM.8 As a secondary outcome, anxiety symptoms decreased in multiple studies on the efficacy of massage for medical disorders (see9 for review) including therapeutic effects in infants who were pre-term, cocaine-exposed, HIV-exposed and full-term10–12; decreased pain and anxiety associated with childbirth, labor, severe burns, the post-operative period, juvenile rheumatoid arthritis, fibromyalgia, lower back pain, and migraine headaches13–20; and decreased anxiety and depression associated with multiple sclerosis21 and spinal cord injuries22, 23. Previous meta-analyses suggest that massage is a useful intervention for people with problems with anxiety, fatigue, muscle tension, muscle soreness, and headaches.9 To date there has been one case series and two randomized controlled trials of massage for GAD.24, 25 The case series reported that patients with GAD benefited from Swedish Massage therapy (SMT).24 However, the trial by Sherman and colleagues25 in a mixed population of medicated and unmedicated participants employing approximately weekly sessions versus a non-intervention control condition, did not demonstrate any benefit for massage therapy. More recently, we performed a randomized, singly masked, six-week monotherapy trial of twice-weekly SMT versus a light touch control (LT) condition for participants with GAD, with outcomes evaluated by masked raters.26 This trial demonstrated significant improvements in ratings of anxiety and depression for the group receiving SMT. The exploratory goal of this study was to gather preliminary data employing the Hamilton Rating Scale for Anxiety (HAM-A) comparing the first six weeks of twice-weekly SMT from the clinical trial (12 sessions) with a second six weeks of twice-weekly SMT (for a total of 24 sessions). The aim was to determine if there was a significant added value to continuing therapy for the 24 total sessions delivered over three months.
2. Methods
2.1. Trial Design and Participants
The trial design and participants for the initial 6 weeks of the study are fully described in Rapaport et al., 2016 and briefly below.26 The study was a randomized, single-masked, two-arm clinical trial comparing six weeks of twice-weekly SMT vs. LT as monotherapy for GAD. It was conducted at the Mood and Anxiety Disorders Program of Emory University in Atlanta, Georgia, between March of 2012 and May of 2013. Forty-seven participants with GAD were recruited from the surrounding community by means of flyers, referrals, and word of mouth and signed written informed consent. The Emory Institutional Review Board approved the study protocol.
Participants had to be medically healthy as demonstrated by a normal medical history and physical exam, meet criteria for a primary diagnosis of current GAD as determined by a structured clinical interview for DSM-IV (SCID),27 and have a HAM-A28 total score >14 in order to enter the acute randomized trial. The HAM-A was chosen as the only assessment of anxiety because 1) it has validated subscales for both psychic anxiety and somatic anxiety, and 2) we wanted to minimize the assessment burden on participants. Participants were permitted to have comorbid but secondary major depressive disorder, dysthymic disorder, or another anxiety disorder except obsessive compulsive disorder. Exclusion criteria included current suicidal ideation, schizophrenia, bipolar disorder, borderline personality disorder, illicit drug use, current psychotropic medication use, current participation in psychotherapy, pregnancy, shift work, current dieting, active medical problems, excessive regular use of alcohol (more than two 5 -oz glasses of wine or equivalents/day), or a history of binge drinking (more than seven drinks/24 hour period) within the last six months.
For inclusion in this analysis, the participants had to complete the twelve SMT sessions in the randomized clinical trial and agree to participate for an additional six weeks of twice-weekly SMT. Three of the 14 eligible participants declined to participate in this open extension phase, two because of conflicts with their job and one because of complications after a car accident. The three participants who discontinued after six weeks of SMT were similar to the 11 who continued SMT in terms of mean age and baseline HAM-A, and they had an identical mean score (10.0) at the six-week point. All 11 participants who began the second period of SMT completed the full six weeks.
2.2. Interventions
SMT treatment occurred between 12:00 PM – 6:00 PM. Prior to the start of each visit participants were asked about changes in health or pregnancy status, use of prescription or over -the-counter medication, illicit substance use, and any new life events
The 45 minute SMT sessions were performed by licensed massage therapists from the Atlanta School of Massage, who adhered to a script that standardized their interactions with participants and followed a manualized treatment protocol29 performed at pressure level 1 on the Massage Therapy Pressure Scale.30 The room was dimly lit and a sound machine was used to mask ambient noise. The participant was draped with a sheet and in a prone position on a massage table, the therapist worked slowly down the body from the shoulders to the feet. The participant then turned over to the supine position and the therapist continued the protocol from the feet back up to the shoulders. SMT techniques included effleurage (slow, rhythmic, continuous stroking), petrissage (slow, rhythmic kneading of underlying muscles), and tapotement (various forms of percussive touching/tapping). Quality control was maintained by review of audio taped sessions, quarterly reliability sessions, weekly discussion of issues arising during intervention sessions, periodic spot checks of SMT protocol adherence, as well as feedback from participants about consistency across therapists.29, 31
2.3. Outcome Assessment
At baseline prior to the initiation of the randomized masked trial, the HAM-A was performed and this rating serves as the pre-treatment measure of anxiety. The HAM-A performed at the end of visit 12 serves as both the end-point for assessment of change during the first 12-session period and the baseline value for comparison of change during the additional 12 sessions of SMT. After all visits, the study psychiatrist conducted a HAM-A interview and assessed the participant for suicidality. The HAM-A consists of 14 items scored 0–4 (range 0–56).
2.4. Statistical Approach
A repeated measures t-test was employed to evaluate within-participant change in HAM-A during six and twelve weeks of SMT, as well as to compare change in HAM-A scores during the first vs. second six-week period.
3. Results
All eleven participants who started the second six weeks of SMT completed the entire 24 sessions. Mean HAM-A scores dropped from 19.91 (2.17 SD) at baseline, to 10.00 (5.80 SD) at week 6 (t=6.31, DF 10, p<0.0001), to 6.91 (3.11 SD) by week 12 (t=6.13, DF 10, p<0.0001) (Figure 2A). The majority of improvement on HAM-A scores occurred in the first six weeks during the single masked trial: mean change of −9.91 (5.20 SD) compared to −3.09 (5.61 SD) in the second six weeks, a difference that approached the level of statistical significance (t=2.21, DF 10, p=0.052) (Figure 2B). This small reduction in the HAM-A does not meet the criteria for a clinically meaningful change based on our group and others definition of a clinically meaningful change.
Figure 2.
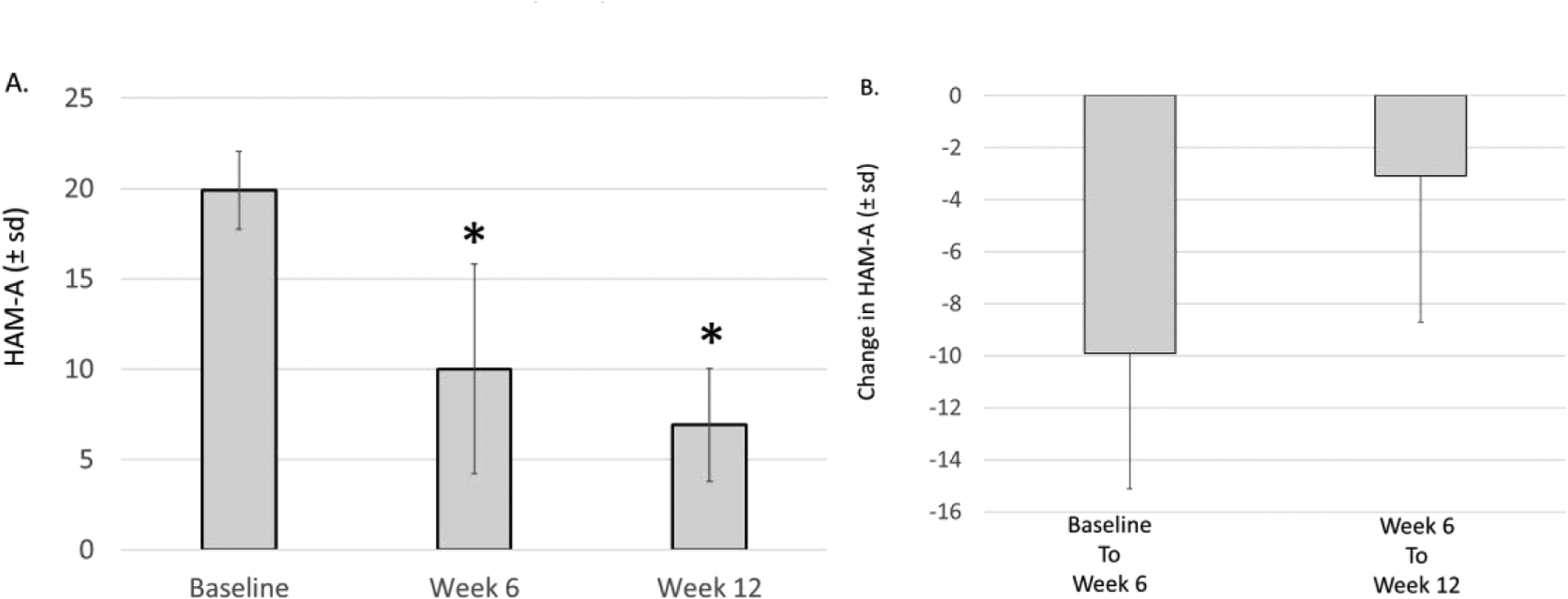
HAM-A ratings in participants undergoing Swedish massage therapy as monotherapy treatment of generalized anxiety disorder (GAD). A) HAM-A at baseline, week 6 (after 12 sessions of SMT), and week 12 (after 24 sessions of SMT). Data are mean ± standard deviation (SD). * p<0.0001. B) Change in HAM-A from baseline to week 6, and from week 6 to week 12. Data are mean ± standard deviation (SD).
4. Discussion
GAD is a common, chronic and debilitating condition.32 People with GAD have increased sympathetic nervous system (SNS) activity (as evidenced by heightened heart rate and skin conductance) as well as decreased parasympathetic nervous system (PNS) activity (as evidenced by lower heart rate variability).33, 34 Further, basal activity of the amygdala, an integral part of the neural circuit that controls peripheral targets of stress response (i.e., SNS and PNS) through the hypothalamus35 is elevated in those with GAD. Worry and GAD are also associated with altered reactivity to stressors. In particular, greater levels of SNS arousal immediately pre-stressor predicts a lesser increase in sympathetic adrenergic activity in response to a stressor36, 37. Thus, increased basal physiological arousal (reflecting a state of pre-stressor worry) may explain dampened physiological reactivity to the stressor in GAD. Although both pharmacological and psychotherapeutic approaches are available, the response and remission rates are inadequate and leave many individuals with ongoing symptoms and impairment.38–42 Other challenges include societal and individual feelings of stigma, which frequently lead patients suffering from GAD to suffer without seeking help. In addition, many individuals prefer a somatic treatment like massage over either medication or psychotherapy.
Our previous work with patients suffering from GAD demonstrates that carefully manualized SMT produces a clinically and statistically significant reduction in measures of anxiety, general distress and depression, superior to an active control condition, LT.26 The current study assessed the impact of twelve additional sessions of SMT on the overall change in anxiety. These data need to be viewed as preliminary and require replication in a larger study because our sample is small and only includes those participants from the acute treatment trial who elected to continue for an additional six weeks of twice-weekly massage. In addition, the lack of a comparison group is a weakness of the study. Although continued improvement occurred over the additional twelve sessions of SMT, 71% of the total improvement occurred during the first twelve sessions. This suggests that a time limited intervention with twice-weekly SMT for six weeks may be sufficient acute treatment for many individuals with GAD. At a time when massage therapy is frequently a non-reimbursed expense, it is important to ascertain the quantity of care that provides sufficient treatment for most patients. Such information will empower patients to make a more informed decision about employing this treatment approach
5. Conclusions
In conclusion, this preliminary analysis suggests that participants who continued with SMT for a second twelve sessions did continue to experience less anxiety as measured by the HAM-A. Yet the amount of improvement was clinically and statistically greater during the first twelve sessions. Thus, six weeks of twice-weekly SMT may be sufficient for most individuals with GAD.
Figure 1.
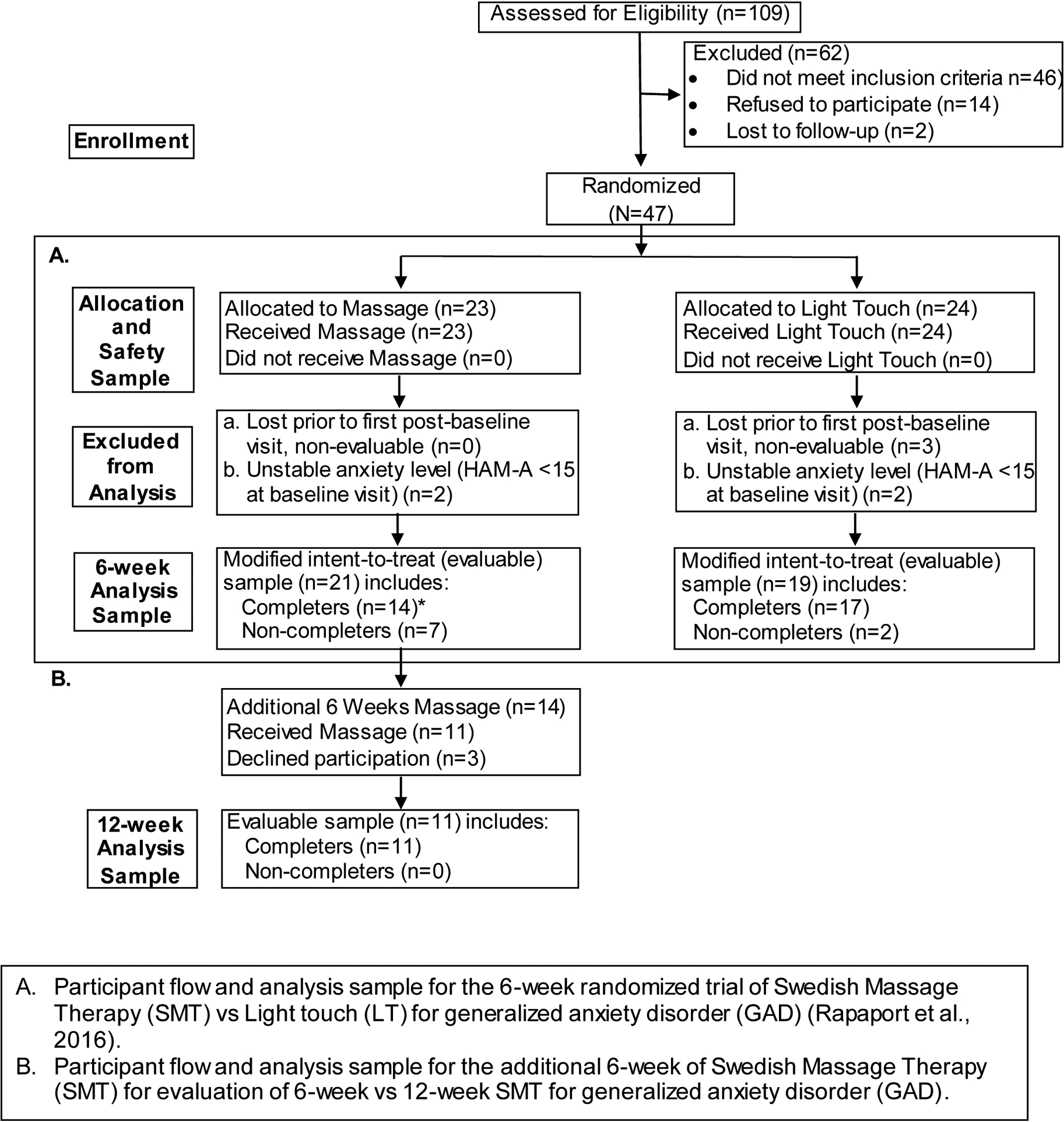
CONSORT Statement Diagram of Participant Flow: 6- vs 12-weeks of Swedish Massage for Generalized Anxiety Disorder.
ACKNOWLEDGMENTS:
The authors would like to acknowledge and thank the Staff of the Atlanta School of Massage Leticia Allen, Lovelace Linares, and Aaron Gunn as well as the research massage therapists: Dedric Carroll, Laureen Dietrick, Grace Prior, and Brittney Turner. Sherry Edwards served as an outstanding coordinator for this trial. This study could not have been performed without their partnership.
FUNDING SOURCE:
The study was funded by grant R21AT004208 from the National Institutes of Health to Dr. Rapaport. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. Drs. Rapaport and Schettler had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
PREVIOUS PRESENTATION: The material is original research, has not been previously published, and is not currently submitted for publication elsewhere. The primary outcomes of the study (6-week data) have been published in the Journal of Clinical Psychiatry (2016). Some of the preliminary analyses of these data were presented at the 2014 ACNP meeting, Phoenix, Arizona, USA.
Conflict of Interest
Dr. Rapaport has provided consulting services to PAX, Inc (unpaid) and has been funded by the NIH.
Dr. Schettler works part-time both as Senior Research Associate in the Department of Psychiatry and Behavioral Sciences at the Emory University School of Medicine, Atlanta, Georgia; as well as Principal Statistician in the Department of Psychiatry of the School of Medicine at the University of California, San Diego. Dr. Schettler has been funded by the NIH. She has no other direct or indirect affiliations or financial interests in connection with the contents of this paper.
Ms. Larson is an employee of the Atlanta School of Massage.
Dr. Dunlop has research support from Acadia, Compass Pathways, Intra-Cellular Therapies, Janssen, National Institute of Mental Health, Sage Therapeutics, and Takeda. He has served on the scientific advisory board of Greenwich Biosciences, Myriad Neuroscience, and Otsuka, and as a consultant to Aptinyx and Sophren Therapeutics.
Dr. Rakofsky has received research funding from Takeda, AstraZeneca and Novartis.
Dr. Kinkead has received research funding from NIH, PCORI and the Brain and Behavior Research Foundation.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 2.Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA. 1994;272(22):1741–1748. [DOI] [PubMed] [Google Scholar]
- 3.Wittchen HU, Kessler RC, Beesdo K, Krause P, Hofler M, Hoyer J. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry. 2002;63 Suppl 8:24–34. [PubMed] [Google Scholar]
- 4.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United states, 2007. Hyattsville, MD: National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- 5.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, Kessler RC. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA: Journal of the American Medical Association. 1998;280(18):1569–1575. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328(4):246–252. [DOI] [PubMed] [Google Scholar]
- 7.Cherkin DC, Deyo RA, Sherman KJ, Hart LG, Street JH, Hrbek A, Davis RB, Cramer E, Milliman B, Booker J, Mootz R, Barassi J, Kahn JR, Kaptchuk TJ, Eisenberg DM. Characteristics of visits to licensed acupuncturists, chiropractors, massage therapists, and naturopathic physicians. J Am Board Fam Pract. 2002;15(6):463–472. [PubMed] [Google Scholar]
- 8.Bystritsky A, Hovav S, Sherbourne C, Stein MB, Rose RD, Campbell-Sills L, Golinelli D, Sullivan G, Craske MG, Roy-Byrne PP. Use of complementary and alternative medicine in a large sample of anxiety patients. Psychosomatics. 2012;53(3):266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moyer CA, Rounds J, Hannum JW. A meta-analysis of massage therapy research. Psychol Bull. 2004;130(1):3–18. [DOI] [PubMed] [Google Scholar]
- 10.Field T, Diego M, Cullen C, Hernandez-Reif M, Sunshine W, Douglas S. Fibromyalgia pain and substance P decrease and sleep improves after massage therapy. J Clin Rheumatol. 2002;8(2):72–76. [DOI] [PubMed] [Google Scholar]
- 11.Scafidi F, Field T. Massage therapy improves behavior in neonates born to HIV-positive mothers. J Pediatr Psychol. 1996;21(6):889–897. [DOI] [PubMed] [Google Scholar]
- 12.Field T, Morrow C, Valdeon C, Larson S, Kuhn C, Schanberg S. Massage reduces anxiety in child and adolescent psychiatric patients. J Am Acad Child Adolesc Psychiatry. 1992;31(1):125–131. [DOI] [PubMed] [Google Scholar]
- 13.Field T, Hernandez-Reif M, Seligman S, Krasnegor J, Sunshine W, Rivas-Chacon R, Schanberg S, Kuhn C. Juvenile rheumatoid arthritis: benefits from massage therapy. J Pediatr Psychol. 1997;22(5):607–617. [DOI] [PubMed] [Google Scholar]
- 14.Field T, Hernandez-Reif M, Taylor S, Quintino O, Burman I. Labor pain is reduced by massage therapy. J Psychosom Obstet Gynaecol. 1997;18(4):286–291. [DOI] [PubMed] [Google Scholar]
- 15.Field T, Peck M, Krugman S, Tuchel T, Schanberg S, Kuhn C, Burman I. Burn injuries benefit from massage therapy. J Burn Care Rehabil. 1998;19(3):241–244. [DOI] [PubMed] [Google Scholar]
- 16.Field T Early interventions for infants of depressed mothers. Pediatrics. 1998;102(5 Suppl E):1305–1310. [PubMed] [Google Scholar]
- 17.Hernandez-Reif M, Dieter J, Field T, Swerdlow B, Diego M. Migraine headaches are reduced by massage therapy. Journal of Bodywork and Movement Therapies. 1998;96:1–11. [Google Scholar]
- 18.Nixon N, Teschendorff J, Finney JW, Karnilowicz W. Expanding the nursing repertory: The effective of massage in postoperative pain. Australian Journal of Advance Nursing 1997;14:21–26. [PubMed] [Google Scholar]
- 19.Puustjärvi K, Airaksinen O, Pontinen PJ. The effects of massage in patients with chronic tension headache. Acupunct Electrother Res. 1990;15(2):159–162. [DOI] [PubMed] [Google Scholar]
- 20.Sunshine W, Field TM, Quintino O, Fierro K, Kuhn C, Burman I, Schanberg S. Fibromyalgia benefits from massage therapy and transcutaneous electrical stimulation. J Clin Rheumatol. 1996;2(1):18–22. [DOI] [PubMed] [Google Scholar]
- 21.Hernandez-Reif M, Field T, Theakston H. Multiple sclerosis patients benefit from massage therapy. Journal of Bodywork and Movement Therapies. 1998;2:168–174. [Google Scholar]
- 22.Diego MA, Field T, Hernandez-Reif M, Hart S, Brucker B, Field T, Burman I. Spinal cord patients benefit from massage therapy. Int J Neurosci. 2002;112(2):133–142. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan SJ, Williams LR, Seaborne DE, Morelli M. Effects of massage on alpha motoneuron excitability. Phys Ther. 1991;71(8):555–560. [DOI] [PubMed] [Google Scholar]
- 24.Billhult A, Maatta S. Light pressure massage for patients with severe anxiety. Complement Ther Clin Pract. 2009;15(2):96–101. [DOI] [PubMed] [Google Scholar]
- 25.Sherman KJ, Ludman EJ, Cook AJ, Hawkes RJ, Roy-Byrne PP, Bentley S, Brooks MZ, Cherkin DC. Effectiveness of therapeutic massage for generalized anxiety disorder: a randomized controlled trial. Depress Anxiety. 2010;27(5):441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rapaport MH, Schettler P, Larson ER, Edwards SA, Dunlop BW, Rakofsky JJ, Kinkead B. Acute Swedish massage monotherapy successfully remediates symptoms of generalized anxiety disorder: A proof-of-concept, randomized controlled study. J Clin Psychiatry. 2016;77(7):e883–891. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Frances A, Pincus HA. DSM-IV handbook of differential diagnosis. 1st Edition ed Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- 28.Hamilton M The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. [DOI] [PubMed] [Google Scholar]
- 29.Larson ER, Kinkead B, Edwards SA, Schettler PJ, Dunlop BW, Rakofsky JJ, Rapaport MH. Model structure for protocol adherence utilizing a manualized therapeutic massage intervention. J Complement Integr Med. 2018;16(2). [DOI] [PubMed] [Google Scholar]
- 30.Walton T Medical Conditions and Massage Therapy: A Decision Tree Approach. Lippincott WIlliams & Wilkins, Philadelphia: 2011. [Google Scholar]
- 31.Larson E Commentary on Operationalizing Partnership Between a Traditional Research Institution and a Massage School. Int J Ther Massage Bodywork. 2018;11(4):32–38. [PMC free article] [PubMed] [Google Scholar]
- 32.Keller MB. The long-term clinical course of generalized anxiety disorder. J Clin Psychiatry. 2002;63 Suppl 8:11–16. [PubMed] [Google Scholar]
- 33.Newman MG, Llera SJ, Erickson TM, Przeworski A, Castonguay LG. Worry and generalized anxiety disorder: a review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annu Rev Clin Psychol. 2013;9:275–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pittig A, Arch JJ, Lam CW, Craske MG. Heart rate and heart rate variability in panic, social anxiety, obsessive-compulsive, and generalized anxiety disorders at baseline and in response to relaxation and hyperventilation. Int J Psychophysiol. 2013;87(1):19–27. [DOI] [PubMed] [Google Scholar]
- 35.Davis M, Falls WA, Campeau S, Kim M. Fear-potentiated startle: A neural and pharmacological analysis. Behav Brain Res. 1993;58(1–2):175–198. [DOI] [PubMed] [Google Scholar]
- 36.Llera SJ, Newman MG. Effects of worry on physiological and subjective reactivity to emotional stimuli in generalized anxiety disorder and nonanxious control participants. Emotion. 2010;10(5):640–650. [DOI] [PubMed] [Google Scholar]
- 37.Fisher AJ, Newman MG. Heart rate and autonomic response to stress after experimental induction of worry versus relaxation in healthy, high-worry, and generalized anxiety disorder individuals. Biol Psychol. 2013;93(1):65–74. [DOI] [PubMed] [Google Scholar]
- 38.Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, Andersson G. Psychological treatment of generalized anxiety disorder: a meta-analysis. Clin Psychol Rev. 2014;34(2):130–140. [DOI] [PubMed] [Google Scholar]
- 39.Pollack MH. Refractory generalized anxiety disorder. J Clin Psychiatry. 2009;70 Suppl 2:32–38. [DOI] [PubMed] [Google Scholar]
- 40.Rickels K, Rynn M. Pharmacotherapy of generalized anxiety disorder. J Clin Psychiatry. 2002;63 Suppl 14:9–16. [PubMed] [Google Scholar]
- 41.Szkodny LE, Newman MG, Goldfried MR. Clinical experiences in conducting empirically supported treatments for generalized anxiety disorder. Behav Ther. 2014;45(1):7–20. [DOI] [PubMed] [Google Scholar]
- 42.Tyrer P, Baldwin D. Generalised anxiety disorder. Lancet. 2006;368(9553):2156–2166. [DOI] [PubMed] [Google Scholar]


