Abstract
Background
The COVID‐19 pandemic has impacted spine care around the globe. Much uncertainty remains regarding the immediate and long‐term future of spine care and education in this COVID‐19 era.
Study design
Cross‐sectional, international study of spine surgeons.
Methods
A multi‐dimensional survey was distributed to spine surgeons around the world. A total of 73 questions were asked regarding demographics, COVID‐19 observations, personal impact, effect on education, adoption of telemedicine, and anticipated challenges moving forward. Multivariate analysis was performed to assess factors related to likelihood of future conference attendance, future online education, and changes in surgical indications.
Results
A total of 902 spine surgeons from seven global regions completed the survey. Respondents reported a mean level of overall concern of 3.7 on a scale of one to five. 84.0% reported a decrease in clinical duties, and 67.0% reported a loss in personal income. The 82.5% reported being interested in continuing a high level of online education moving forward. Respondents who personally knew someone who tested positive for COVID‐19 were more likely to be unwilling to attend a medical conference 1 year from now (OR: 0.61, 95% CI: [0.39, 0.95], P = .029). The 20.0% reported they plan to pursue an increased degree of nonoperative measures prior to surgery 1 year from now, and respondents with a spouse at home (OR: 3.55, 95% CI: [1.14, 11.08], P = .029) or who spend a large percentage of their time teaching (OR: 1.45, 95% CI: [1.02, 2.07], P = .040) were more likely to adopt this practice.
Conclusions
The COVID‐19 pandemic has had an adverse effect on surgeon teaching, clinical volume, and personal income. In the future, surgeons with family and those personally affected by COVID‐19 may be more willing to alter surgical indications and change education and conference plans. Anticipating these changes may help the spine community appropriately plan for future challenges.
Keywords: COVID‐19, coronavirus, education, future, guidelines, healthcare, impact, spine

1. INTRODUCTION
The COVID‐19 pandemic has affected both patients and healthcare providers worldwide. At the time of this study's completion, inpatient hospital and intensive care unit demand have far exceeded capacity for many regions. Hospitals have made drastic alterations to care structures, including prioritizing different types of procedures and deferring elective surgeries. 1 , 2 In addition, many spine and orthopedic surgeons have been asked to help provide care outside of their area of expertise, including the emergency department and intensive care unit. 3 , 4 For many, the length of time that these changes will remain in place is unknown, and the pandemic may continue to unfold in stages. 4 , 5 The long‐term repercussions of the pandemic and its effects on healthcare providers are fraught with uncertainty.
As highlighted by Louie et al, spine surgeons around the globe have been affected by these aforementioned changes. 6 Many have experienced diminished clinical productivity, adverse effects on personal income, and travel bans. In some cases, they have even been reassigned to work on the front lines. 3 , 7 Limitations from hospital systems have made it difficult for spine surgeons to effectively treat their patients. Many with myelopathic symptoms, worsening radicular pain, and motor weakness have been forced to struggle through continued conservative treatment. 8 , 9 An understanding of the challenges faced by spine surgeons in this current pandemic and their attitudes towards the future may help to guide resource allocation moving forward. Similarly, embracing positive changes that have resulted from this unique time may stimulate a new age of virtual learning and global collaboration. Thus, the aim of the present study was to elicit the attitudes, stresses, and future anticipations of spine surgeons around the globe as they pertain to patient care and education in response to the COVID‐19 pandemic, and to present tangible plans to address the challenges and concerns as they return to their clinical practices in the postCOVID‐19 era.
2. METHODS
2.1. Survey design and content
A survey, known as the AO Spine COVID‐19 and spine surgeon global impact survey, was developed. The survey panel was composed of five regional Research Chairs of AO Spine, representing seven global regions (Africa, Asia, Australia, Europe, Middle East, North America, and South America/Latin America), as well as long‐standing, experienced spine surgeons who have directed spine fellowship programs, epidemiologists, statisticians, and spine fellows as noted by Louie et al. 6 Question selection was based on a Delphi style for consensus, following several rounds of review before finalization. The multiple‐choice questions included several domains, such as: demographics, COVID‐19 observations, financial impact, and future perceptions.
2.2. Survey distribution
The 73‐item survey was presented in English and distributed via email to the AO Spine membership who agreed to receive surveys (n = 3805). AO Spine is the world's largest society of international spine surgeons (www.aospine.org). The survey recipients were provided 9 days to complete the survey (27 March 2020 to 4 April 2020). Respondents were informed their participation was voluntary, and information gained would be disseminated publicly and in peer‐review journals.
2.3. Statistical analysis
All statistical analysis and data processing were performed using open‐source packages through the Python v3.7 programming language. Survey responses were summarized via collection of raw count data and respective calculation of percentages, means, and standard deviations. Multivariate logistic regression analysis was performed to assess variations in survey responses focusing on patient care/education and included reported interest level in online spine education, likelihood of attending a medical conference in 1 year, and inclination to use increased nonoperative measures prior to surgery in 1 year. Model covariates believed to be relevant to dependent variables of interest based on the opinions of senior co‐authors, and included all collected baseline survey respondent demographics and practice‐specific characteristics. Results of the multivariate models were summarized via calculation of odds ratios (ORs), 95% confidence intervals (CIs), and P‐values. A P‐value <.05 was used to establish statistical significance for all tests.
3. RESULTS
In total, 902 surgeons completed the survey, with an overall response rate of 23.7%. Of the 7 global regions represented, those with the greatest number of responses were Europe (242/881; 27.5%), followed by Asia (213/881; 24.2%) and North America (152/881; 17.3%). Of 91 countries, the majority of survey responses were from the United States (128/902; 14.2%), China (73/902; 8.1%), and Egypt (66/902; 7.3%) (Figure 1 ). More respondents were male (826/881; 93.8%) orthopedic surgeons (637/902; 70.6%), aged 35‐44 years‐old (344/895; 38.4%), and primarily practiced in academic institutions (405/892; 45.4%). Of note, a majority reported having a spouse at home (773/902; 86.5%) and children at home (637/887; 71.8%) (Table 1 ).
FIGURE 1.
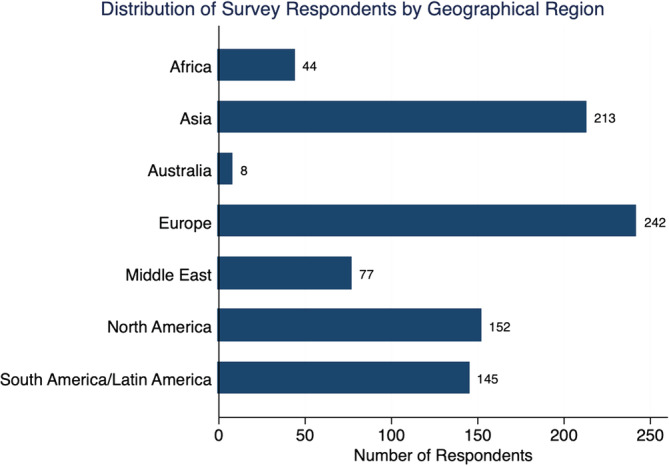
Distribution of survey respondents by geographical region
TABLE 1.
Survey respondent demographics
| Personal demographics | Practice demographics | ||||
|---|---|---|---|---|---|
| # | % | # | % | ||
| Age (Y) | Specialty | ||||
| 25‐34 | 130 | 14.5 | Orthopedics | 637 | 70.6 |
| 35–44 | 344 | 38.4 | Neurosurgery | 246 | 27.3 |
| 45‐54 | 245 | 27.4 | Trauma | 104 | 11.5 |
| 55‐64 | 150 | 16.8 | Pediatric surgery | 17 | 1.9 |
| 65+ | 26 | 2.9 | Other | 35 | 3.9 |
| Sex | Years since training completion | ||||
| Female | 55 | 6.2 | Less than 5 Y | 161 | 25.3 |
| Male | 826 | 93.8 | 5 to 10 Y | 141 | 22.2 |
| Home demographics | 10 to 15 Y | 104 | 16.4 | ||
| Spouse at home | 773 | 86.5 | 15 to 20 Y | 117 | 18.4 |
| Children at home | Over 20 Y | 113 | 17.8 | ||
| 0 | 250 | 28.2 | Practice Type | ||
| 1 | 221 | 24.9 | Academic/Private Combined | 204 | 22.9 |
| 2 | 266 | 30.0 | Academic | 405 | 45.4 |
| 3 | 109 | 12.3 | Private | 144 | 16.1 |
| 4+ | 41 | 4.6 | Public/Local Hospital | 139 | 15.6 |
| Elderly at home | 191 | 21.4 | Practice Breakdown (%) | ||
| Living alone | 63 | 7.1 | % Research | ||
| Geographic region | 0–25 | 731 | 81.9 | ||
| Africa | 44 | 5.0 | 26‐50 | 129 | 14.5 |
| Asia | 213 | 24.2 | 51‐75 | 21 | 2.4 |
| Australia | 8 | 0.9 | 76‐100 | 12 | 1.3 |
| Europe | 242 | 27.5 | % Clinical | ||
| Middle East | 77 | 8.7 | 0–25 | 22 | 2.5 |
| North America | 152 | 17.3 | 26–50 | 87 | 9.7 |
| South America/Latin America | 145 | 16.5 | 51–75 | 194 | 21.7 |
| Exposure to previous pandemics | 76–100 | 590 | 66.1 | ||
| SARS | 98 | 47.1 | % Teaching | ||
| H1N1 (Swine Flu) | 128 | 61.5 | 0–25 | 668 | 74.9 |
| MERS | 17 | 8.2 | 26–50 | 152 | 17.0 |
| Ebola | 15 | 7.2 | 51–75 | 50 | 5.6 |
| Total respondents | 902 | 100 | 76–100 | 22 | 2.5 |
Abbreviations: #, number of respondents/votes, %, percent, SARS, severe acute respiratory syndrome; MERS, Middle East respiratory syndrome.
Respondents reported a moderate‐ to high‐level of overall concern regarding the COVID‐19 outbreak, with a mean score of 3.7 on a scale of one to five. The three most common stressors identified were family health (76.0%), economic concerns (45.7%), and timeline to resume regular clinical practice (44.9%). Hospitals did not have guidelines for dealing with an outbreak for 39.6% of respondents, and 94.7% said that formal guidelines should be developed moving forward.
Furthermore, these concerns matched reported changes in daily clinical practice, income, and anticipations to resume normal elective surgical activity. Time spent performing clinical duties had decreased for 84.0%. At the time of survey completion, 100% of respondents reported that their surgical volume was adversely affected, and 67.1% of respondents stated that over 75.0% of their surgical caseload had been either postponed or canceled. Financially, 67.0% of surgeons reported an expected loss of income (Figure 2), and a majority reported an expected decrease in revenue both personally and for their employer at the time of survey completion. In addition, 48.8% of respondents stated that the timeframe to resume elective surgeries is unknown. Assuming normal operative permission for elective surgery, 64.0% anticipated more than 4 weeks and 26.5% anticipated more than 8 weeks before a return to “baseline” status is possible.
FIGURE 2.
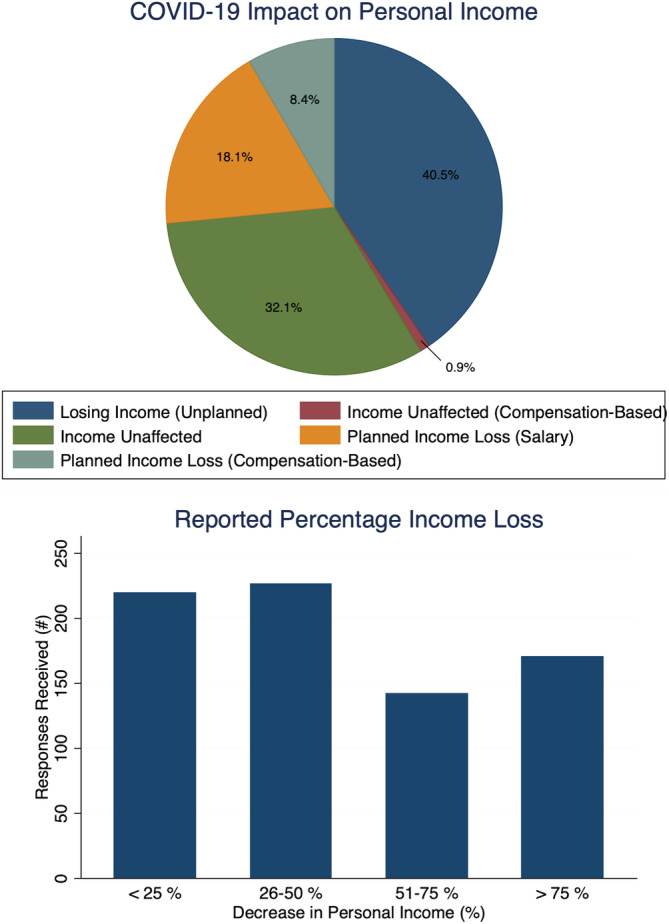
Impact of COVID‐19 pandemic on personal income loss
There is also concern that the presence of the virus may be felt for years to come. When asked how this outbreak will impact patient care 1 year from now, 57.9% said they will have a heightened awareness of hygiene, and 45.8% will increase use of personal protection equipment. Providers may be more hesitant to offer surgical intervention going forward, as 20.0% reported they plan to pursue an increased degree of nonoperative measures prior to surgery and 38.0% will have patients reschedule if they feel sick. Furthermore, when asked if they would attend a scheduled medical conference 1 year from now, 33.7% reported being either unsure or not likely.
Multivariate assessment of anticipated clinical practice changes revealed that respondents are more inclined to pursue nonoperative measures in 1 year if he/she reported having a spouse at home (OR: 3.55, 95% CI: [1.14, 11.08], P = .029) or spent a large percentage of their time teaching (OR:1.45, 95% CI: [1.02, 2.07], P = .040). Conversely, orthopedic respondents (OR: 0.17, 95% CI: [0.01, 0.65], P = .009), North American clinicians (OR: 0.25, 95% CI: [0.01, 0.94], P = .040), and those who did not expect the COVID‐19 pandemic to impact their salary (OR: 0.39, 95% CI: [0.19, 0.81], P = .011) were less likely to implement future nonoperative management (Table 2).
TABLE 2.
Inclination to pursue nonoperative measures in 1 year
| Survey questions | Odds ratio | 95% Confidence interval | P‐value a |
|---|---|---|---|
| Demographics | |||
| Sex | 0.46 | (0.15, 1.44) | .184 |
| Age | 1.15 | (0.74, 1.77) | .534 |
| Number of Children at Home | 0.92 | (0.72, 1.17) | .478 |
| Spouse at home | 3.55 | (1.14, 11.08) | .029 |
| Region | |||
| Asia | 1.66 | (0.52, 5.32) | .393 |
| Australia | 0.30 | (0.02, 3.79) | .355 |
| Europe | 0.93 | (0.28, 3.05) | .901 |
| Middle East | 0.83 | (0.22, 3.19) | .783 |
| North America | 0.25 | (0.07, 0.94) | .040 |
| South/Latin America | 0.64 | (0.19, 2.19) | .473 |
| Specialty | |||
| Orthopedics | 0.17 | (0.05, 0.65) | .009 |
| Neurosurgery | 0.24 | (0.06, 0.92) | .038 |
| Trauma | 0.80 | (0.30, 2.10) | .649 |
| Pediatrics | 0.00 | (<0.00, 1.25 × 10235) | .966 |
| Other | 1.14 | (0.30, 4.36) | .846 |
| Income impact | |||
| No Impact: Compensation‐based income | 4.42 | (0.46, 42.33) | .198 |
| No impact: Salary | 0.39 | (0.19, 0.81) | .011 |
| Reduction: Salary | 0.97 | (0.49, 1.89) | .918 |
| Reduction: Compensation‐based income | 0.90 | (0.35, 2.31) | .832 |
| Practice time allocation | |||
| Clinic | 0.92 | (0.64, 1.32) | .633 |
| Research | 1.21 | (0.73, 2.00) | .460 |
| Teaching | 1.45 | (1.02, 2.07) | .040 |
| Previous outbreak | |||
| SARS | 0.81 | (0.36, 1.80) | .599 |
| H1N1 (Swine Flu) | 1.04 | (0.49, 2.23) | .911 |
| MERS | 3.12 | (0.60, 16.20) | .175 |
| Ebola | 1.63 | (0.25, 10.81) | .612 |
| Recommend precautions for spine surgery | |||
| Recommend against | 1.65 | (0.92, 2.98) | .096 |
| Standard level of caution | 1.00 | (0.50, 1.97) | .991 |
| Not present during intubation/extubation | 0.86 | (0.45, 1.65) | .653 |
| Addition PPE during surgery | 1.71 | (0.92, 3.17) | .089 |
| Other | |||
| Practice type | 0.93 | (0.73, 1.18) | .528 |
| Years since training completion | 0.90 | (0.67, 1.20) | .453 |
| Clinical duties impacted | 1.09 | (0.70, 1.70) | .718 |
| Personal revenue loss expected | 0.98 | (0.75, 1.28) | .868 |
| Currently performing elective cases | 0.66 | (0.33, 1.32) | .242 |
P‐values were calculated using multivariate logistic regression analysis. Bolded values indicate statistical significance at P < .05.
Abbreviations: SARS, severe acute respiratory syndrome, MERS, Middle East respiratory syndrome.
Scholarly activity and in‐person education has been adversely affected, with 66.3% reporting that their research activities had decreased in productivity or completely stopped. Similarly, of respondents with residents and fellows, 85.2% reported that the pandemic has hurt their overall experience. However, there has been a stimulation of telemedicine, web‐based learning, and global collaboration in response to the pandemic. One year from now, 41.8% of respondents anticipated having an increased use of digital options for patient communication. Regarding online spine education, 82.5% reported being either interested or very interested in participating and continuing these efforts. If a centralized web‐based collaboration platform were established, 33.9% said they would be active readers, and 59.8% said they would both read and contribute.
Multivariate analysis of present and future academic activity also demonstrated significant associations with various responses. Clinicians being government mandated to shelter in place (OR: 2.59, CI: [1.14, 5.87], P = .022) or those with practices previously impacted by a prior pandemic (SARS) (OR: 2.49, CI: [1.30, 4.76], P = .006) were significantly more likely to attend medical conferences in 1 year. In contrast, those unlikely to attend reported knowing someone who has tested positive for COVID‐19 (OR: 0.61, CI: [0.39, 0.95], P = .029) (Table 3). Lastly, surgeons reporting larger clinic‐based practices were more likely to express interest in online spine education (OR: 2.56, CI: [1.07, 6.12], P = .034) (Table 4).
TABLE 3.
Likelihood of attending a conference in 1 year
| Survey questions | Odds ratio | 95% Confidence interval | P‐value a |
|---|---|---|---|
| Demographics | |||
| Region | 0.96 | (0.85, 1.09) | .543 |
| Sex | 0.93 | (0.30, 2.90) | .899 |
| Age | 0.92 | (0.71, 1.19) | .518 |
| Children | 1.02 | (0.83, 1.25) | .870 |
| Spouse at home | 1.85 | (0.79, 4.35) | .156 |
| Previous Outbreak | |||
| SARS | 2.48 | (1.30, 4.76) | .006 |
| H1N1 (Swine Flu) | 0.50 | (0.24, 1.01) | .054 |
| MERS | 1.41 | (0.30, 6.51) | .662 |
| Ebola | 0.63 | (0.11, 3.55) | .598 |
| Specialty | |||
| Orthopedics | 1.02 | (0.26, 4.06) | .975 |
| Neurosurgery | 0.89 | (0.22, 3.57) | .871 |
| Trauma | 0.56 | (0.22, 1.43) | .224 |
| Pediatrics | 1.52 | (0.21, 10.97) | .678 |
| Other | 1.10 | (0.29, 4.13) | .891 |
| Practice time allocation | |||
| Clinic | 0.95 | (0.68, 1.33) | .756 |
| Research | 1.41 | (0.90, 2.21) | .139 |
| Teaching | 0.94 | (0.69, 1.29) | .720 |
| Other | |||
| Practice type | 0.85 | (0.66, 1.09) | .195 |
| Years since training completion | 0.98 | (0.83, 1.15) | .767 |
| Personal exposure to COVID‐19 | 0.61 | (0.39, 0.95) | .029 |
| Clinical duties impacted | 1.40 | (1.00, 1.96) | .049 |
| Government mandate to shelter | 2.59 | (1.14, 5.88) | .022 |
| Income impacted | 0.91 | (0.78, 1.07) | .241 |
| Personal revenue loss expected | 0.87 | (0.71, 1.05) | .145 |
| Hospital staff furloughed | 1.03 | (0.71, 1.50) | .876 |
| Negative research impact | 0.91 | (0.77, 1.08) | .259 |
P‐values were calculated using multivariate logistic regression analysis. Bolded values indicate statistical significance at P < .05.
Abbreviations: SARS, severe acute respiratory syndrome, MERS, Middle East respiratory syndrome.
TABLE 4.
Interest in Participating in online spine education
| Survey questions | Odds ratio | 95% Confidence interval b | P‐value a |
|---|---|---|---|
| Demographics | |||
| Sex | 1.00 | (0.07, 15.42) | 1.000 |
| Age | 1.60 | (0.51, 4.98) | .420 |
| Number of children at home | 0.64 | (2.00, 1.10) | .106 |
| Spouse at home | 1.28 | (0.17, 9.88) | .811 |
| Region | |||
| Asia | 6.07 | (0.63, 58.61) | .119 |
| Australia | 2.430 × 103 | (0, inf) | .938 |
| Europe | 2.42 | (0.28, 20.83) | .421 |
| Middle East | 1.27 | (0, inf) | .997 |
| North America | 2.85 | (0.33, 24.72) | .341 |
| South/Latin America | 3.31 | (0.38, 28.99) | .280 |
| Specialty | |||
| Orthopedics | 2.66 | (0.01, 5.32) | .386 |
| Neurosurgery | 4.43 | (0.03, 7.67) | .576 |
| Trauma | 5.69 | (0, inf) | .998 |
| Pediatrics | 6.05 | (0, inf) | .950 |
| Other | 779.61 | (0, inf) | .936 |
| Perceived impact on resident training | |||
| Negative | 3.67 | (0.98, 13.69) | .053 |
| None | 1.18 | (0.19, 7.35) | .861 |
| Positive | 4.49 × 107 | (0, inf) | .997 |
| Practice time allocation | |||
| Clinic | 2.56 | (1.07, 6.12) | .034 |
| Research | 6.83 × 109 | (0, inf) | 1.000 |
| Teaching | 3.54 | (0, inf) | .227 |
| Previous outbreak | |||
| SARS | 0.84 | (0.13, 5.50) | .854 |
| H1N1 | 1.04 | (0.10, 2.45) | .377 |
| MERS | 6.05 × 104 | (0, inf) | .969 |
| Ebola | 6.16 × 103 | (0, inf) | .950 |
| Other | |||
| Government mandate to shelter | 1.33 | (0.46, 6.44) | .417 |
| Inclination to pursue nonoperative measures in 1 y | 0.48 | (0.28, 24.87) | .398 |
| Negative research impact | 1.04 | (0.67, 1.61) | .852 |
| Percentage of clinic performed via telecommunication | 0.97 | (0.631, 1.65) | .934 |
| Practice type | 1.82 | (0.44, 1.13) | .144 |
| Number years since posttraining | 0.79 | (0.40, 1.54) | .478 |
Abbreviations: SARS, severe acute respiratory syndrome, MERS, Middle East respiratory syndrome.
P‐values were calculated using multinominal logistic regression analysis. Bolded values indicate statistical significance at P < .05.
95% Confidence intervals with an upper bound of infinity indicates a failure of convergence, whereby an estimated range for a given odds ratio could not be calculated.
4. DISCUSSION
The findings of the present study suggest that spine surgeon's worldwide share in the concern surrounding the COVID‐19 pandemic. Clinical volume has diminished, daily routines have been altered, and revenues have decreased. There is uncertainty as to what both the immediate and distant future holds. Despite these concerns, there has been a renewed interest in telemedicine, virtual learning, and global collaboration. Guidelines are necessary to help spine surgeons meet the challenges of current and future patient care, in addition to maintaining efforts aimed at education and collaboration (Table 5 ).
TABLE 5.
Anticipated future challenges and tips for spine surgeons
| Immediate challenges |
|
| Future challenges |
|
| Education and collaboration |
|
4.1. Spine care in the future
In regards to spine care moving forward, roughly one in five surgeons reported that they plan to attempt longer courses of conservative care before committing to surgical intervention 1 year from now. This may be reflective of surgeons’ hesitancy to bring patients to the hospital, exposing both patients and care teams to the potential for pathogen transmission. A more likely explanation, however, may be an effort to avoid overwhelming a stressed healthcare system with unplanned hospital or ICU admissions. 10 This practice of attempting a longer course of conservative therapy was more likely to be adopted by those with a spouse at home, likely reflective of an overarching desire to avoid spreading COVID‐19 to the home environment. 11 , 12 Interestingly, this practice was also more likely to be adopted by clinicians who identified as spending a large portion of their time in resident and fellow education, and less likely to be adopted by those who did not expect the pandemic to impact their salary. In addition to minimizing exposure of residents and fellows to COVID‐19, this finding is consistent with the higher likelihood of providers in academic settings receiving a fixed‐salary rather than reimbursement based solely on surgical volume. 13 Regardless, forced consideration of elective surgeries moving forward may help providers to better identify patients that can be treated sufficiently with nonoperative care. 9 , 14 Once hospital capacity for performing spine surgeries does return to normal or near‐normal, we encourage spine surgeons to maintain evidence‐based indications for conservative care vs surgical intervention. The practice of peer‐to‐peer communication and indications review regarding the appropriateness of treatment plans, both nonoperative and operative should be continued into the distant future to ensure an appropriate treatment plan and allocation of resources.
The COVID‐19 pandemic has been accompanied by considerable financial uncertainty for spine surgeons. In fact, the timeline to resume clinical practice and economic concerns were identified as two of the three most common stressors shared by respondents to our survey. Furthermore, a majority reported experiencing a personal decrease in revenue, and half of respondents had no timeline for return to “normal” clinical care. This financial uncertainty for both practices and individual providers is not only a key source of stress, but also an issue that may carry lasting repercussions. Vaccaro et al shared the experience and tentative financial plan of three prominent orthopedic surgery practices with academic ties in the United States. 15 All three reported an expected loss in revenue and income for the practice and care providers that last until the third quarter of the 2020 fiscal year, assuming that elective surgeries are able to restart in the summer of 2020. Each had enacted work hour restrictions or furlough for ancillary staff. The timeline for these changes remains unclear, and is dependent largely on the easing of surgery restrictions. Furthermore, when spine surgeons are able to perform elective procedures once again, their patient population may be considerably different from the prepandemic population. That is, patients may not have the same health insurance that they previously carried, patients may not have time to seek elective surgery following an extended period of diminished or no income, and many will simply not wish to seek care in a hospital setting where COVID‐19 is present. 16 Although there have been some efforts in the United States to help provide fiscal support to struggling physicians and practices, such as the Coronavirus Aid, Relief and Economic Security (CARES) Act, the effectiveness of these interventions has yet to be seen. 17 Spine surgeons should optimize financial and scheduling flexibility until a prepandemic level of productivity and fiscal security can be realized.
Finally, many respondents to our survey anticipate a long‐term emphasis on efforts to avoid a similar public health crisis in the future. When asked if they had any words they wished to share, a large proportion offered messages of caution and safety, with the largest percentage directed towards patients in particular. Similarly, the most likely changes that surgeons anticipated 1 year from now included an increased emphasis on hygiene and proper use of personal protective equipment. Habits such as these are critical, as multiple rebounds in the number of patients with COVID‐19 are expected until a vaccine becomes available or herd immunity can be realized. 18 In addition, despite the fact that a minority of surgeons reported working at an institution that had guidelines for the pandemic, nearly all respondents believed that such guidelines should be a priority and in place moving forward. Clearly there is a need for evidence‐based protocols. Hospitals and medical centers must disclose anticipated needs and provide solutions to local government, at which point data can be gathered from multiple centers within a region. Plans can be developed at the local, regional, and national levels around the world to provide formal guidelines that are evidence‐based and aligned with the research and experience of the COVID‐19 pandemic.
4.2. Education and collaboration
The COVID‐19 pandemic has resulted in new sources of stress, changes to patient care, and uncertainty regarding future practice. The education of residents and fellows, in addition to the continued learning of faculty, has not been immune to these changes 1 , 19 A majority of respondents in our survey noted that the education of their residents and fellows had been adversely affected, and their personal research productivity had fallen or stopped. Despite many negatives, the pandemic has stimulated a wave of web‐based learning and global collaboration that has not been seen before. 20 In fact, over 80% of respondents indicated being interested or very interested in the continued use of novel learning modalities. Interestingly, providers who reported spending a majority of their time in clinical medicine, vs teaching or research were more likely to express interest in this continued use. This may be attributable to the relative ease and convenience of participating and/or leading educational experiences on virtual platforms that simultaneously allow for a high‐volume clinical practice. Furthermore, this may be a valuable avenue for academic departments and professional societies and to engage spine providers in educational endeavors who were previously too occupied.
Virtual meeting platforms in particular have revolutionized the way clinicians interact and learn while spending time away from their normal work environment. 21 The examples are numerous. Residency and fellowship programs in orthopedic surgery and neurosurgery have adopted online platforms for departmental conferences and meetings. Governing bodies and subspecialty societies within spine surgery have organized and led international seminars that surgeons can access from their own home. Industry and independent education foundations have held virtual case reviews, research study group meetings, and topical debates. In response to high attendance and positive feedback, time and money invested for these endeavors has risen drastically. 22 Given the number of spine care providers that have met the learning curve and successfully adopted these platforms, our hope is that these powerful learning tools continue to serve important roles into the distant future.
Concerns regarding the spread of disease and placing spine care providers at risk has resulted in the cancellation or postponement of conferences around the world. Furthermore, once providers return to clinical practice, they may lack the financial and scheduling freedom to attend traditional in‐person conferences. Many of these conferences have therefore adopted virtual formats, in which presentations and resources can be accessed via computer remotely. However, a timeline to return to normalcy and a long‐term plan for medical conferences remains unknown. When asked if they would attend a scheduled conference 1 year from now, roughly two out of three respondents indicated that they would feel comfortable doing so. Those who reside in a region that had a shelter in place order, and those who reported being impacted by a prior pandemic (SARS), expressed a higher likelihood of feeling comfortable. This is likely reflective of provider confidence in local governing bodies to develop policies to limit the spread of a pathogen, recover once the pandemic has resolved, and to determine if and when a medical conference is appropriate. 23 , 24
Although face‐to‐face interaction is valuable, there has been a growing interest for global collaborative platforms for spine providers that may serve a similar function to medical conferences of the past. When asked in our survey, 34% reported they would be active readers on such a platform, and 60% reported they would both read and contribute. Spine governing bodies and subspecialty societies should consider these data when planning meetings and collaborative opportunities in a postCOVID‐19 world.
5. CONCLUSIONS
The effects of the COVID‐19 pandemic have been far reaching, many of which have been felt by spine surgeons around the world. The present study suggests that spine surgeons share a high level of concern regarding the pandemic, with drastic changes to daily routines, finances, and methods of learning. Understanding the current attitudes, sources of stress, and unique areas of interest for spine surgeons may enable planning and anticipation for future challenges. Web‐based learning and global collaboration have seen a unique surge in utilization. Rising to meet the challenges of COVID‐19 and maintaining the unanticipated benefits will help the field of spine surgery to continue moving forward.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
AUTHOR CONTRIBUTIONS
All authors played an important role in the development of this manuscript. Michael T. Nolte, Arash J. Sayari, Dino Samartzis drafted and revised the manuscript. Garrett K. Harada, Philip K. Louie, Michael H. McCarthy, G. Michael Mallow, Zakariah Siyaji, Niccole Ger, and Dino Samartzis were responsible for data acquisition, analysis, and interpretation. Jason PY Cheung, Marko H. Neva, Mohammad El‐Sharkawi, Marcelo Valacco, Daniel M. Sciubba, Norman B. Chutken, Howard S. An, and Dino Samartzis were responsible for manuscript revision, and approval of final version. All authors have read and approved the final submitted manuscript.
Nolte MT, Harada GK, Louie PK, et al. COVID‐19: Current and future challenges in spine care and education ‐ a worldwide study. JOR Spine. 2020;3:e1122 10.1002/jsp2.1122
REFERENCES
- 1. Kogan M, Klein SE, Hannon CP, Nolte MT. Orthopaedic education during the COVID‐19 pandemic. J Am Acad Orthop Surg. 2020;28:e456‐e464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Massey PA, McClary K, Zhang AS, Savoie FH, Barton RS. Orthopaedic surgical selection and inpatient paradigms during the coronavirus (COVID‐19) pandemic. J Am Acad Orthop Surg. 2020;28:436‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ambrosio L, Vadalà G, Russo F, Papalia R, Denaro V. The role of the orthopaedic surgeon in the COVID‐19 era: cautions and perspectives. J Exp Orthopaed. 2020;7:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schwartz AM, Wilson JM, Boden SD, Moore TJ Jr, Bradbury TL Jr, Fletcher ND. Managing resident workforce and education during the COVID‐19 pandemic: evolving strategies and lessons learned. JBJS Open Access. 2020;5(2):e0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. de Caro F, Hirschmann TM, Verdonk P. Returning to orthopaedic business as usual after COVID‐19: strategies and options. Knee Surg Sports Traumatol Arthrosc. 2020;1:1699‐1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Louie PK, Harada GK, McCarthy MH, et al. The impact of COVID‐19 pandemic on spine surgeons worldwide. Global Spine J. 2020;10:534‐552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Soh TLT, Ho SWL, Yap WMQ, Oh JY. Spine surgery and COVID‐19: challenges and strategies from the front lines. JBJS. 2020:e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ghogawala Z, Kurpad S, Falavigna A, et al. COVID‐19 and spinal surgery. J Neurosurg Spine. 2020;1:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Phillips MR, Chang Y, Zura RD, et al. Impact of COVID‐19 on orthopaedic care: a call for nonoperative management. Therapeutic Adv Musculoskeletal Disease. 2020;12:1759720X20934276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lancaster EM, Sosa JA, Sammann A, et al. Rapid response of an academic surgical department to the COVID‐19 pandemic: implications for patients, surgeons, and the community. J Am Coll Surg. 2020;230:1064‐1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adams JG, Walls RM. Supporting the health care workforce during the COVID‐19 global epidemic. JAMA. 2020;323(15):1439‐1440. [DOI] [PubMed] [Google Scholar]
- 12. Lancet T. COVID‐19: protecting health‐care workers. Lancet (London, England). 2020;395(10228):922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baimas‐George M, Fleischer B, Korndorffer JR Jr, Slakey D, DuCoin C. The economics of private practice versus academia in surgery. J Surg Educ. 2018;75(5):1276‐1280. [DOI] [PubMed] [Google Scholar]
- 14. Epstein NE. COVID‐19 provides an opportunity to reassess how frequent and how extensive elective spine surgery should be. Surg Neurol Int. 2020;11(58):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vaccaro AR, Getz CL, Cohen BE, Cole BJ, Donnally CJ 3rd. Practice management during the COVID‐19 pandemic. J Am Acad Orthop Surg. 2020;28:464‐470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gangopadhyaya A, Garrett AB. Unemployment, Health Insurance, and the COVID‐19 Recession. Health Insurance, and the COVID‐19 Recession. Washington DC, USA: Robert Wood Johnson Foundation's Urban Institute; 2020:2020 https://www.urban.org/research/publication/unemployment-health-insurance-and-covid-19-recession [Google Scholar]
- 17.What the $2 trillion coronavirus relief plan means for doctors [Internet].; 2020, Available from: https://www.ama-assn.org/delivering-care/public-health/what-2-trillion-coronavirus-relief-plan-means-doctors.
- 18. Fang Y, Nie Y, Penny M. Transmission dynamics of the COVID‐19 outbreak and effectiveness of government interventions: a data‐driven analysis. J Med Virol. 2020;92:645‐659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dowdell J, Louie PK, Virk S, et al. Spine fellowship training reorganizing during a pandemic: perspectives from a tertiary orthopaedic specialty center in the epicenter of outbreak. Spine J. 2020. https://pubmed.ncbi.nlm.nih.gov/32344060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stambough JB, Curtin BM, Gililland JM, et al. The past, present, and future of orthopaedic education: lessons learned from the COVID‐19 pandemic. J Arthroplasty. 2020;35:S60‐S64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fraser H, Soanes K, Jones SA, Jones CS, Malishev M. The value of virtual conferencing for ecology and conservation. Conserv Biol. 2017;31(3):540‐546. [DOI] [PubMed] [Google Scholar]
- 22.Investments in edtech platforms are powering online learning in the age of COVID; 2020. Available from: https://impactalpha.com/investing-in-the-post-covid-future-of-education/.
- 23. Cheng LT, Chan LP, Tan BH, et al. Déjà vu or jamais vu? How the severe acute respiratory syndrome experience influenced a Singapore radiology department's response to the coronavirus disease (COVID‐19) epidemic. Am J Roentgenol. 2020;214(6):1206‐1210. [DOI] [PubMed] [Google Scholar]
- 24. Weiner JA, Swiatek PR, Johnson DJ, et al. Learning from the past: did experience with previous epidemics help mitigate the impact of COVID‐19 among spine surgeons worldwide? Eur Spine J. 2020;29:1‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]


