Abstract
Background/purpose
Artificial intelligence (AI) has made deep inroads into dentistry in the last few years. The aim of this systematic review was to identify the development of AI applications that are widely employed in dentistry and evaluate their performance in terms of diagnosis, clinical decision-making, and predicting the prognosis of the treatment.
Materials and methods
The literature for this paper was identified and selected by performing a thorough search in the electronic data bases like PubMed, Medline, Embase, Cochrane, Google scholar, Scopus, Web of science, and Saudi digital library published over the past two decades (January 2000–March 15, 2020).After applying inclusion and exclusion criteria, 43 articles were read in full and critically analyzed. Quality analysis was performed using QUADAS-2.
Results
AI technologies are widely implemented in a wide range of dentistry specialties. Most of the documented work is focused on AI models that rely on convolutional neural networks (CNNs) and artificial neural networks (ANNs). These AI models have been used in detection and diagnosis of dental caries, vertical root fractures, apical lesions, salivary gland diseases, maxillary sinusitis, maxillofacial cysts, cervical lymph nodes metastasis, osteoporosis, cancerous lesions, alveolar bone loss, predicting orthodontic extractions, need for orthodontic treatments, cephalometric analysis, age and gender determination.
Conclusion
These studies indicate that the performance of an AI based automated system is excellent. They mimic the precision and accuracy of trained specialists, in some studies it was found that these systems were even able to outmatch dental specialists in terms of performance and accuracy.
Keywords: Artificial intelligence dentistry, Machine learning, Computer-aided diagnosis, Deep learning models, Convolutional neural networks, Artificial neural networks
Introduction
The exponential growth in science and technology has introduced different applications that are used daily, such as siri and alexa. These applications are found on the top of artificial intelligence (AI) and its components. The term AI is mostly associated with robotics. It describes how technology is used to develop a software or a machine that can easily mimic human intelligence and perform specific activities.
John McCarthy, a mathematician coined the term artificial intelligence in 1955, and widely recognized as the father of artificial intelligence. He chose this term to explain the potential of machines to perform tasks that can fall in the range of “intelligent” activities.1
In the year 1956, John McCarthy organized a famous Dartmouth conference, which was formally on the research project artificial intelligence, this is when this discipline originated. The conference sparked the crucial period, from 1950s to 1970s, wherein extensive research was done on AI.2
In 1978 Richard Bellman, an applied mathematician defined artificial intelligence as the automation of activities associated with human thinking abilities, which includes learning, decision making and problem solving.3
In the modern day world, artificial intelligence refers to any machine or technology that is able to mimic human cognitive skills like problem solving. To understand AI, it is important to know few of these key aspects (Fig. 1).
-
⁃
Artificial intelligence is termed as a capability of machines that exhibits a form of its own intelligence. The aim here was to develop machines that can learn through data so that they can solve the problems.
-
⁃
Machine learning is part of AI, which depends on algorithms to predict outcomes based on a dataset. The purpose of machine learning is to facilitate machines to learn from data so they can resolve issues without human input.
-
⁃
Neural networks are a set of algorithms that compute signals via artificial neurons. The purpose of neural networks is to create neural networks that function like the human brain.
-
⁃
Deep learning is a component of machine learning that utilizes the network with different computational layers in a deep neural network to analyze the input data. The purpose of deep learning is to construct a neural network that automatically identifies patterns to improve feature detection.4
Figure 1.
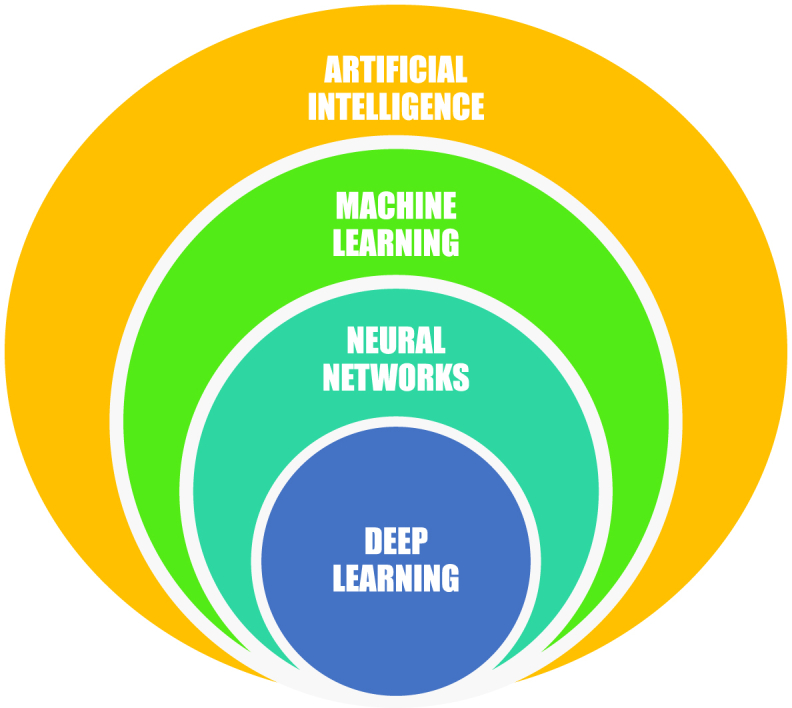
Key aspects of artificial intelligence.
Deep learning is also known as convolutional neural networks. They collect features from the abstracted layer of filters and are primarily used to process large and complex images.5
Application of AI in dentistry
AI has been used mainly in dentistry to make the process of diagnosis more accurate and efficient, which is of atmost importance in achieving best results to the treatments provided along with superior quality patient care.
Dentists need to use all their acquired knowledge to diagnose and decide the best treatment option. They are also required to predict the prognosis where they need accurate clinical decision-making skills. However, in some cases, dentists do not have enough knowledge to make the right clinical decision in a limited period. AI applications can serve as their guide so that they can make better decisions and perform better.
Shortliffe,6 Chae et al.,7 Schleyer et al.,8 reported that dentists have become dependent on computer applications to get insights for clinical decision making. The aim of this systematic review was to identify the development of AI applications that are widely employed in dentistry and to evaluate their performance in terms of diagnosis, clinical decision-making, and predicting the prognosis of the treatment.
Materials and methods
Data sources
This systematic review was carried after referring the guidelines for preferred reporting items for Systematic reviews and Meta-analyses extension for Diagnostic Test Accuracy (PRISMA-DTA).9 The literature for this paper was identified and selected by performing a thorough search in the electronic data bases like Pubmed, Medline, Embase, Cochrane, Google scholar, Scopus, Web of science, and Saudi digital library published over the past two decades (January 2000–March 15, 2020) by using keywords such as artificial intelligence in dentistry, deep learning, machine learning, artificial neural networks, convolutional neural networks, and computer-aided diagnosis. This search was based on the PICO (problem/patient/population, intervention/indicator, comparison, and outcome) elements (Table 1).
Table 1.
Description of the PICO (P= Population, I= Intervention, C= Comparison, O= Outcome) elements.
| Research question | What are the developments, performance, and application of artificial intelligence in dentistry? |
|---|---|
| Population | Patients diagnostic images related to oral and maxillofacial regions [clinical images, radiographs, CBCT, confocal laser endomicroscopy (CLE) Images, intraoral fluorescence images, cephalometric radiographs, near-infrared-light transillumination (NILT) images] |
| Intervention | AI based models for diagnosis, treatment planning, clinical decision making, predicting the need for treatment, and predicting the prognosis. |
| Comparison | Expert opinions, reference standards |
| Outcome | Measurable or predictive outcomes such as accuracy, sensitivity, specificity, ROC = receiver operating characteristic curve, AUC = Area Under the Curve, ICC = Intraclass Correlation Coefficient, Positive/Negative Predictive Values (PPV/NPV) |
Resources selection
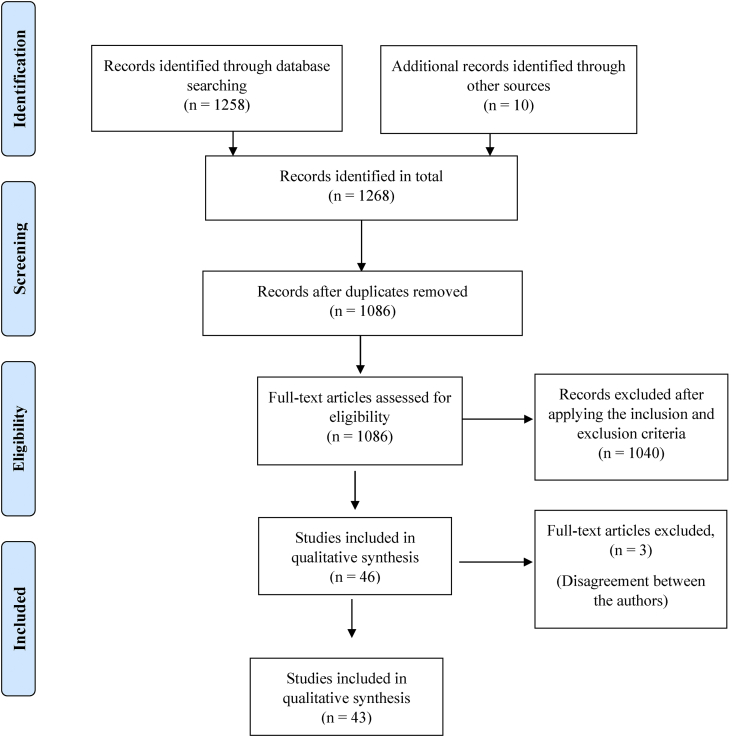
Full-length articles were retrieved. Hand searching and electronic searching was performed to go through the journals. The required data for this review was selected in two stages. In the first stage the articles were selected based on the title and abstracts related to our research topic. The preliminary search resulted in 1268 articles that were appropriate enough to address the paper's aim. Due to duplication, 182 articles were removed. Hence, we retrieved 1086 articles for the second stage of selection. Next, the following criterion was applied.
Criteria for considering studies for this review
Inclusion criteria
-
1.
The article must be focused on AI and its application should be related to dentistry.
-
2.
There must be some predictive or measurable outcomes so they can be quantified.
-
3.
There has to be a proper mention of datasets that are used to assess a model.
Exclusion criteria
-
1.
The articles that are related to non-AI areas.
-
2.
Uistaploaded articles that were unpublished.
-
3.
Articles that consisted of only abstracts without the full text.
-
4.
Articles that were not written in English.
This criteria cut down the number of articles to 46. The name of the journals and names of the authors were hidden and spread among the authors. A critical assessment was carried out for all the articles by following QUADAS-2 (Quality Assessment and Diagnostic Accuracy Tool) guidelines, a tool for quality assessment of the studies on diagnostic accuracy.10 3 more articles were excluded due to disagreement from the authors. Eventually, this systematic review performed qualitative synthesis on 43 articles (Fig. 2).
Figure 2.
Flow chart for screening and selection of articles.
All the articles were read fully. The years of these articles were taken in account to study the progress of AI trends that were developed and evolved over the years in dentistry.
Results
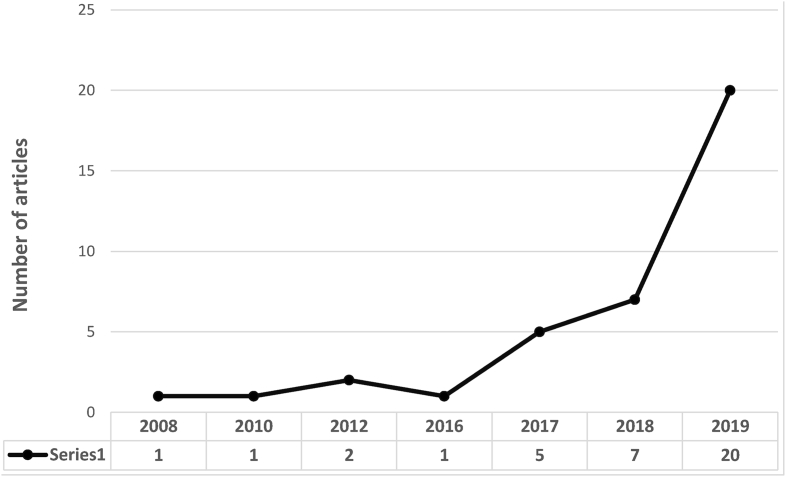
This systematic review included 43 research articles that were analyzed for quantitative data. The analysis of the literature revealed that most of the studies were conducted in the past 12 years (Fig. 3). The trends showed that there is a gradual increase in the research related to artificial intelligence in dentistry.
Figure 3.
Trends of research on artificial intelligence in dentistry.
The studies that were included in this systematic review were mainly on the application of AI for detection and diagnosis of dental caries, diagnosis of proximal dental caries, tooth detection and numbering, detection of vertical root fractures, detection of apical lesions, locating minor apical foramen, assessment of root morphology, diagnosis of salivary gland diseases, diagnosis of maxillary sinusitis, maxillofacial cysts, cervical lymph nodes metastasis, detection of osteoporosis, predicting diagnosis of orthodontic extractions, assessing need for orthodontic treatments, determining the growth and development of cervical vertebrae stages, cephalometric analysis, identifying cephalometric landmarks, diagnosis of orthognathic surgeries, assessing the impact of orthodontic treatment on the facial attractiveness, gender determination using mandibular morphometric parameters, estimating the age based on third molar development, classifying the cancerous tissues, predicting postoperative facial swelling following extractions, detection of periodontal bone loss, detecting the degree of alveolar bone loss.
Most of the studies have used convolutional neural networks (CNNs) and artificial neural networks (ANNs). Some of the studies were based on bayesian network (BN) and probabilistic neural networks (PNNS). The purpose of these neural networks is to determine computer tomography (CT) images, cone beam computed tomography (CBCT) images, lateral cephalometric radiographs, bitewing radiographs, facial photos, panoramic radiographs (OPG). (Table 2).
Table 2.
Details of the studies that have used AI based models in various specialties of dentistry for diagnosis, treatment planning, clinical decision making, predicting the need for treatment, and predicting the prognosis.
| Serial no | Authors | Year of publication | Algorithm Architecture |
Objective of the study | No. of images/photographs for testing | Study factor | Modality | Evaluation accuracy/average accuracy | Comparison if any | Results (+)effective, (−)non effective (N) neutral |
Outcomes | Authors suggestions/recommendations |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Devito et al.11 | 2008 | ANNs | AI based model for diagnosing the proximal dental caries | 160 | Tooth Decay | Bite-wing Radiographs | ROC curve area of 0.884 | 25 examiners | (+) Effective | This neural network could improve the performance of diagnosing proximal caries. | None |
| 2 | Xie et al.12 | 2010 | ANNs | ANN based AI model for deciding if extractions are necessary prior to orthodontic treatment | 200 | Tooth malocclusion | Lateral cephalometric radiographs | Accuracy of 80% | Not mentioned | (+)Effective | ANN was effective in determining whether extraction or non-extraction treatment was best for malocclusion patients | None |
| 3 | Saghiri et al.13 | 2012 | ANNs | ANN based AI model for determining the working length | 50 | Tooth | Human cadavers | Accuracy of 96% | 2 Endodontists | (+)Effective | The accuracy of ANN was more than the endodontists | The ANN model is accurate method for working length determination |
| 4 | Saghiri et al.14 | 2012 | ANNs | ANN system for locating the minor apical foramen (AF) | 50 | Tooth | Human dried skull | Accuracy of 93% | Endodontists | (+)Effective | ANN can useful for secondary opinion for locating the AF on radiographs and it can be helpful in enhancing the accuracy in determining the working length | ANN can be used for decision making similar clinical scenarios |
| 5 | Jung et al.15 | 2016 | ANNs | Artificial Intelligence expert system for orthodontic decision-making of required permanent tooth extraction | 156 | Tooth malocclusion | Lateral cephalometric radiographs | Accuracy of 92% | 1 Experienced orthodontists | (+)Effective | The success rates of the models were 92% for the system's recommendations for extraction vs non extraction | AI expert systems with neural network machine learning could be useful in orthodontics |
| 6 | Johari et al.16 | 2017 | PNNs | Probabilistic Neural Network (PNN) for diagnosing (VRFs) in intact and the teeth that has undergone endodontic treatment | 240 | Tooth | CBCT and periapical radiographs | Accuracy of 96.6, sensitivity of 93.3 and specificity of 100% | Not mentioned | (+)Effective | The designed neural network can be used as a proper model for the diagnosis of VRFs on CBCT images of endodontically treated and intact teeth; CBCT images were more effective than periapical radiographs. | None |
| 7 | Tobel et al.17 | 2017 | CNNs | An automated technique for staging the development of lower third molar. | 200 | Tooth | Panoramic radiographs (OPG) | Mean ICC was 0.95 | 2 observers | (+)Effective | Deep CNN based AI system demonstrated similar results to the results demonstrated by other trained examiners. | Further optimization is required to achieve a fully automated system for estimating the dental age. |
| 8 | Aubreville et al.18 | 2017 | CNNs | AI based automatic system for diagnosing (OSCC) oral squamous cell carcinoma | 7894 | Oral cavity | Confocal laser endomicroscopy (CLE) images | AUC of 0.96 and a mean accuracy of 88.3%, sensitivity 86.6%, specificity 90% | Not clear | (+)Effective | This approach was found to outperform the state of the art in CLE image recognition | None |
| 9 | Imangaliyev et al.19 | 2017 | CNNs | CNN model for the automatic classification of red fluorescent dental plaque images. | 427 | Tooth | Quantitative light-induced fluorescence images | Predictive accuracy of 0.89% | Reference models | (+)Effective | CNN model prediction performance was higher than other models. | None |
| 10 | Niño-Sandoval et al.20 | 2017 | ANNs | AI based model for predicting the mandibular morphology | 229 | Anatomical landmarks | Lateral cephalograms | Coefficients from 0.84 until 0.99 | Support vector regression | (+)Effective | This model demonstrated high predictability ability | This model may be the key for facial reconstruction |
| 11 | Zhang et al.21 | 2018 | ANNs | ANN for predicting postoperative facial swelling following the extraction of impacted mandibular third molars. | 100 | Face | Data set | Accuracy of 98.00% | 1 Oral surgeon | (+)Effective | This AI based model proved to be an accurate in predicting of the facial swelling following the extraction of impacted mandibular third molars. | None |
| 12 | Lee et al.22 | 2018 | CNNs | (DCNN)-Based Computer-Assisted Diagnosis (CAD) systems. Single-Column DCNN (SC-DCNN), Single-Column with Data Augmentation DCNN (SC-DCNN Augment) and Multicolumn DCNN (MC-DCNN). | 200 | Face | Panoramic radiographs (OPG) | (AUC) values obtained using SC-DCNN was 0.9763, SC-DCNN (Augment) was 0.9991, MC-DCNN for 0.9987 | 2 Experienced oral and maxillofacial radiologists | (+)Effective | The system that was based on DCNN was effective in detecting osteoporosis and also demonstrated high agreement with the experienced oral and maxillofacial radiologists | None |
| 13 | Lee et al.23 | 2018 | CNNs | Diagnosing and predicting of PCT using a computer -assisted detection system based on a deep CNN | 348 | Tooth | Intra oral periapical radiographs | Mean predictive accuracy of 78.9% | 3 calibrated board-certified periodontists | (+)Effective | The DCNN based model was effective and efficient in diagnosing and predicting of (PCT). | Further optimization of the PCT dataset is required for improvement |
| 14 | Thanathornwong24 | 2018 | Bayesian network (BNs) | Bayesian network (BN) for predicting the need for orthodontic treatment. | 1000 | Tooth malocclusion | Data sets | AUC (0.91) | 2 Experienced orthodontists | (+)Effective | This BN based system; and demonstrated promising results with high degree of accuracy in the need for orthodontic treatment. | None |
| 15 | Zhang et al.25 | 2018 | CNNs | Teeth recognition using label tree with cascade network structure. | 200 | Tooth | Intra oral periapical radiographs | Precision of 95.8% | Reference models | (+)Effective | This approach demonstrated a high precision of 95.8% and recall of 96.1%. | None |
| 16 | Lee et al.26 | 2018 | CNNs | AI based deep learning system for detecting and diagnosing dental caries | 600 | Dental caries | Intraoral periapical radiographic images | Mean AUC of 0.890 | 4 calibrated board-certified dentists | (+)Effective | This DCNN based system algorithm performed considerably good in detection dental caries on periapical radiographs. | None |
| 17 | Yauney et al.27 | 2018 | CNNs | AI based system for automated oral health screenings and cross correlations of oral-systemic health | 810 | Periodontium | Intraoral fluorescence images | AUC of 0.677, precision of 0.271, Recall of 0.429 | Dentists | (+)Effective | This automated process was effective in correlating poor periodontal health with systemic health outcomes | Machine learning, can be used for automated diagnoses and systemic health screenings for other diseases |
| 18 | Kök et al.28 | 2019 | ANNs | AI algorithms for determining the stages of the growth and development by cervical vertebrae | 300 | Cervical Vertebrae | Cephalometric radiographs | Mean accuracy of 77.02% | 1 orthodontists | (+)Effective | ANN could be the preferred method for determining cervical vertebrae stages | None |
| 19 | Park JH et al.29 | 2019 | CNNs | Comparing latest deep-CNN based systems for identifying cephalometric landmarks | 283 | Landmarks | Cephalometric radiographs | 5% higher accuracy with (YOLOv3) than Single (SSD) | Single shot multibox detector (SSD) | (+)Effective | You-Only-Look-Once model outperformed in accuracy and computational time than the shot multibox detector | This model can be used in clinical practice for identifying the cephalometric landmarks. |
| 20 | Choi et al.30 | 2019 | ANNs | ANN based model for deciding on surgery/non-surgery and determining extractions. | 316 | Landmarks | Lateral cephalometric radiographs | ICC 0.97–0.99 | 1 Experienced orthodontists | (+)Effective | This ANN based model demonstrated higher success rate in deciding on surgery/non-surgery and was also successful in deciding on the extractions. | This ANN based model will be useful in diagnosing of orthognathic surgery cases. |
| 21 | Patcas. et al.31 | 2019 | CNNs | AI system for describing the impact of orthognathic treatments on facial attractiveness and age appearance | 2164 | Facial landmarks | Facial photographs | Not Clear | Not mentioned | (+)Effective | This CNN based AI system can be used for scoring facial attractiveness and apparent age in patients under orthognathic treatments. | None |
| 22 | Casalegno et al.32 | 2019 | CNNs | AI based model for detecting and localizing dental lesions in Near-Infrared Transillumination (TI) images | 217 | Dental caries | Near-infrared transillumination (TI) imaging | ROC of 83.6 for occlusal and ROC of 84.6% for proximal | Dental experts with clinical experience | (+)Effective | This CNN based model demonstrated promising results with increased speed and accuracy in detecting caries. | None |
| 23 | Fukuda et al.33 | 2019 | CNNs | CNN based AI system for detection of vertical root fracture (VRF) | 60 | Tooth | Panoramic radiographs (OPG) | Precision of 0.93 Recall was 0.75 F- Measure of 0.83. |
2 radiologists and 1 endodontist | (+)Effective | The CNN based AI model is an efficient tool in detecting VRFs | None |
| 24 | Kise et al.34 | 2019 | CNNs | AI system for detection of Sjögren's syndrome (SjS) on CT, and comparing its performance with radiologists | 100 | Salivary glands | Computed tomography (CT) images | Accuracy of 96.0, Sensitivity of 100% and specificity of 92.0% | 6 radiologists | (+)Effective | The deep learning system demonstrated a higher diagnostic performance | Can be used as a diagnostic support while interpreting CT images |
| 25 | Hiraiwa et al.35 | 2019 | CNNs | AI system for classifying root morphologies of mandibular first molars | 760 | Tooth | Cone beam computed tomography (CBCT) Images | Accuracy of 86.9% | 2 radiologists | (+)Effective | The deep learning system demonstrated high accuracy in the differential diagnosis of a single or extra root in the distal roots of mandibular first molars. | None |
| 26 | Tuzoff et al.36 | 2019 | CNNs | CNN based AI system for automatic teeth detection and numbering | 222 | Tooth | Panoramic radiographs (OPG) | Precision of 0.9945 and mean sensitivity of 0.987 | Dental experts | (+)Effective | The performance of the this system was comparable to the level of performance of the experts | This system can simplify the process of filling digital dental charts. |
| 27 | Ekert et al.37 | 2019 | CNNs | CNNs based AI system for detecting apical lesions (ALs) | 2001 | Tooth | Panoramic radiographs (OPG) | AUC of 0.85 (0.04) sensitivity 0.65 and specificity 0.87 | 6 Dentists | (+)Effective | This deep CNN based AI system was successful in detecting apical lesions | None |
| 28 | Murata et al.38 | 2019 | CNNs | AI based system for diagnosing of maxillary sinusitis | 120 | Maxillary sinusitis | Panoramic radiographs (OPG) | Accuracy of 87.5%, sensitivity of 86.7%, specificity of 88.3%, AUC of 0.875 | 2 experienced radiologists, 2 dental residents. | (+)Effective | The AI based deep learning system demonstrated higher diagnostic performance. | The deep-learning system can provide diagnostic support for inexperienced dentists |
| 29 | Chen et al.39 | 2019 | CNNs | CNN based tool package for detecting and numbering the teeth | 250 | Tooth | Intra oral periapical films | Precisions and recalls exceed 90%, IOU of 91% |
3 Dentists | (+)Effective | The results indicate that machines performance was close to the level of a junior dentist | None |
| 30 | Vinayahalingam et al.40 | 2019 | CNNs | CNN based AI system to detect and segment the approximate of inferior alveolar nerve (IAN) to the roots of lower third molars (M3) on OPGs | 81 | Tooth | Panoramic radiographs (OPG) | Mean dice-coefficients for M3s and IAN were 0.947 ± 0.033 and 0.847 ± 0.099 | Portable network graphics (PNG) files as gold standard | (+)Effective | Deep-learning is an encouraging approach to segment anatomical structures | Further enhancement of the algorithm is advised to improve the accuracy |
| 31 | Mallishery et al.41 | 2019 | ANNs | Machine learning to generate an algorithm which can help predict the difficulty level of the case and decide on referral | 500 | Tooth | Data Set | Sensitivity of 94.96% | 2 pre-calibrated endodontists | (+)Effective | This study provides an option for automation for increasing the speed of decision-making and referrals. | An AAE endodontic case difficulty assessment form when utilized along with machine learning can assist general dentists in rapid assessment of the case difficulty |
| 32 | Patcas et al.42 | 2019 | CNNs | AI system for evaluating the facial attractiveness of patients who have undergone treatment for clefts and the facial attractiveness of controls and to compare these results with panel ratings performed by laypeople, orthodontists, and oral surgeons | 30 | Face | Frontal and profile images | Cleft cases (all Ps ≥ 0.19), for control group (all Ps ≤ 0.02) | 15 laypeople, 14 orthodontists, and 10 oral surgeons | (−)Non Effective | AI system scores were comparable with the scores of the other groups for the cleft patients, but the scores were lower for the controls | There is a need for further refinement in this AI based system |
| 33 | Krois et al.43 | 2019 | CNNs | Deep- CNN based system for detecting periodontal bone loss | 2001 | Periodontium | Panoramic radiographs (OPG) | Predictive accuracy of 81% and were similar to the examiners | 6 Experienced dentists | (N) Neutral | CNN demonstrated similar results to that of the dentists in detecting periodontal bone loss. | Machine -learning based technologies can reduce the dentists' diagnostic efforts. |
| 34 | Ariji et al.44 | 2019 | CNNs | AI system for diagnosing metastasis of lymph node. | 441 | Cervical lymph nodes | Computed tomography (CT) images | Accuracy of 78.2%, sensitivity of 75.4%, specificity of 81.0%, positive predictive value of 79.9%, negative predictive value of 77.1%, and ROC of 0.80 | Not clear | (N) Neutral | The diagnostic results of the CNN based system were similar to the results of the radiologists. | This CNN based system is a valuable for diagnostic support. |
| 35 | Ariji et al.45 | 2019 | CNNs | Performance of deep learning classification in diagnosing extranodal extension of cervical lymph node metastases in CT images | 703 | Cervical lymph nodes | Computed tomography (CT) images | Accuracy of 84.0% | 4 Radiologists | (+)Effective | The deep learning diagnostic performance in extra nodal extension was significantly higher when compared with the performance of the radiologists | This method is expected to improve diagnostic accuracy by further study with increasing sample size of patients. |
| 36 | Hung et al.46 | 2019 | CNNs | AI based model for predicting root caries | 5135 | Root caries | Data set | Accuracy of 97.1%, precision of 95.1%, sensitivity of 99.6% and specificity of 94.3% AUC of 0.997 |
Trained medical personnel | (+)Effective | This model perform well and can be allowed for clinical implementation | Can be utilized by both dental and non-dental professionals |
| 37 | Kim et al.47 | 2019 | CNNs | AI based (CNNs) for diagnosing maxillary sinusitis | 200 | Maxillary sinusitis | Waters' view radiographs | AUC of 0.93 for the temporal and 0.88 for geographic external |
5 Radiologists | (+)Effective | AI based (CNNs) demonstrated statistically significantly higher AUC than radiologist in both test sets | None |
| 38 | Schwendicke et al.48 | 2020 | CNNs | AI based (CNNs) to detect caries lesions in near-infrared-light transillumination (NILT) images. | 226 | Tooth decay | NILT images | The mean) AUC of 0.74, Sensitivity of 0.59 and specificity of 0.76 PPV was 0.63 and NPV was 0.73 |
2 Experienced dentists | (+)Effective | The model demonstrated satisfying discriminatory ability to detect caries lesions. | None |
| 39 | Kunz et al.49 | 2020 | CNNs | An automated cephalometric X-ray analysis using a specialized (AI) algorithm | 50 | Landmarks | Cephalometric radiographs | Not clear | 12 experienced examiners | (+)Effective | AI algorithm was able to analyze unknown cephalometric X-rays similar to the quality level of the experienced human examiners | None |
| 40 | Hwang et al.50 | 2020 | CNNs | Deep -learning based automated system for detecting the patterns of 80 cephalometric landmarks | 283 | Landmarks | Cephalometric radiographs | Not Mentioned | Human examiners | (+)Effective | This system accuracy in identifying of cephalometric landmarks similar to the human examiners | This system might be a viable option when repeated identification of multiple cephalometric landmarks. |
| 41 | Lee et al.51 | 2020 | CNNs | Deep (CNNs), on the classification of specific features of osteoporosis | 136 | Face | Dental panoramic radiographs (DPRs) | ROC of 0.858 | Gold standard reference models | (+)Effective | This Deep (CNNs), could of use and reliable system for automated screening of osteoporosis patients. | None |
| 42 | Patil et al.52 | 2020 | ANNs | ANN for gender determination | 509 | Mandible | Panoramic radiographs (OPG) | Accuracy of 75% | 1 experienced oral and maxillofacial radiologist | (+)Effective | ANN proved as a good tool for predicting the gender and can be applied in the forensic sciences for near accurate results. | This automated application is promising for identifying gender or age with minimal errors |
| 43 | Yu et al.53 | 2020 | CNNs | AI based skeletal diagnostic system | 5890 | Anatomical landmarks | Lateral cephalograms | Mean AUC of >95% | 2 orthodontists | (+)Effective | This model demonstrated excellent performance for skeletal orthodontic diagnosis | None |
ANNs = Artificial Neural Networks, CNNs = Convolutional Neural Networks, DCNNs = Deep Convolutional Neural Networks, BN = Bayesian Network, PNN = Probabilistic Neural Network, ROC = Receiver Operating Characteristic curve, AUC = Area Under the Curve, ICC = Intraclass Correlation Coefficient, F = F- measure, VRF = Vertical Root Fracture, PTC = Periodontal Compromised Teeth, Positive/Negative Predictive Values (PPV/NPV).
The studies that have been analyzed in this systematic review revealed that the AI technology has been widely used in different specialties of dentistry. AI technology has been applied in 18 studies on oral & maxillofacial radiology,11,22,25,26,32,34,36, 37, 38, 39, 40, 41,44, 45, 46, 47, 48,51 11 studies on orthodontics and dentofacial orthopedics,12,15,24,28, 29, 30, 31,42,49,50,53 5 studies on endodontics,13,14,16,33,35 4 studies on periodontics,19,23,27,43 2 studies from oral and maxillofacial surgery18,21 and 3 studies from forensic odontology.17,52,20
Risk of bias assessment
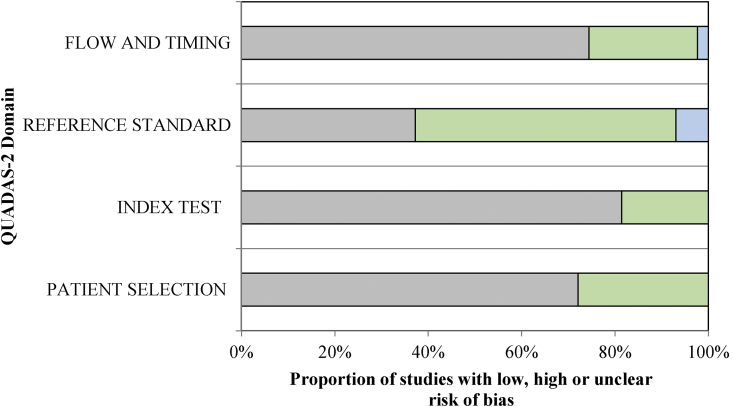
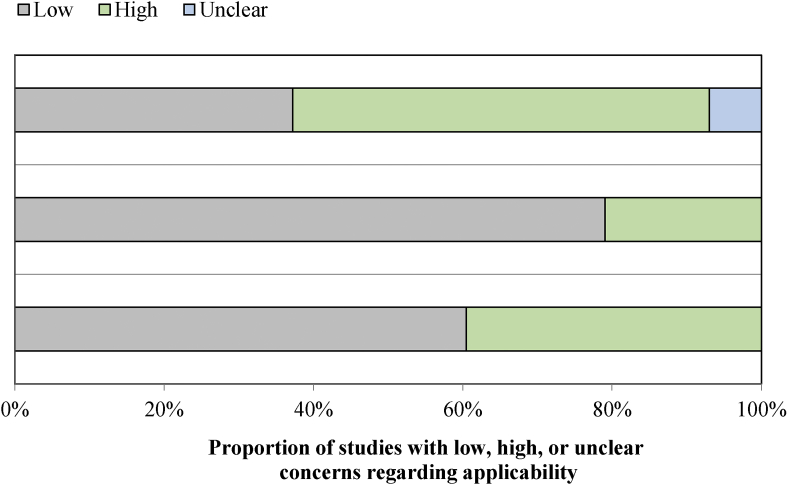
All the studies were based on assessing the diagnostic accuracy of AI in various fields of dentistry. Hence, risk of bias assessment was assessed using QUADAS-2 assessment tool, which is frequently used tool in the literature (Supplementary Table 1). The studies conducted on human beings for determining the reference standard were rated as high risk. In the present analysis, 55.81% of studies reported high risk of bias for the reference standard. Since the data feeding in AI technology was highly standardized, AI had no effect on the flow, and time frame in the final output, hence categorized as low risk categories. In the present systematic review, low risk of bias was reported in index test (81%) and (74.41%) in flow and timings. Some studies conducted on the cadaveric samples and extracted specimens, under the applicability domain were considered as high risk for patient selection and index test domain (Supplementary Table 2). Even though, comparable results were obtained for the applicability arm of the QUADAS-2 (Figure 4, Figure 5).
Figure 4.
Assessment of individual risk of bias domains.
Figure 5.
Concerns regarding applicability.
Discussion
AI is modernizing the traditional aspects of dentistry. AI based systems are often used for designing automated software programs that streamlines the diagnosis and data management in dentistry.8 Mostly they are clinical decision support systems that assist and guide experts to make better decisions. These systems have been used for better diagnosis, treatment planning and also for predicting the prognosis.54 The demand for these systems is booming due to their effectiveness in providing explanations and reasoning.55
AI has revolutionized in the field of dentistry and making the dentist's task easier. The clinical decision support systems that work on the AI technology are mainly designed to provide expert support to the health professionals.56 Clinical decision support systems is defined as, any computer program that has been designed to help health professionals in making clinical decisions, and also deals with the medical data or with the knowledge of medicine necessary for interpreting such data.6
In this systematic review we analyzed studies on the application of AI technology in dentistry and evaluated their performance in terms of diagnosis, clinical decision-making, and predicting the prognosis of the treatment.
Application of AI technologies in the specialty of oral and maxillofacial radiology and diagnostics
Zhank et al.,25 reported the use of AI-based CNNs and evaluated effective teeth recognition by relying on the label tree along with cascade network structure. The model demonstrated a high precision of 95.8%. A study by Tuzoff et al.,36 showed very similar results when utilized an AI-powered CNNs model for teeth identification, which was then arranged numerically. This computer-aided diagnostic technique displayed a mean sensitivity of 0.987 and precision 0.9945. This output was similar to that of an expert.
Chen et al.,39 applied the CNNs to detect the teeth number in intra oral periapical films and then to identify the tooth. The model demonstrated very high precision. The results indicated that AI technologies make it convenient for clinicians to do their job. They do not have to enter the details manually. Using these automated systems dentists can enter their dental charts digitally, resulting in higher efficiency.
AI technology in the detection of dental caries has demonstrated excellent results which were reflected in the study done by Lee et al.,26 who reported applying of CNN algorithms for detection and diagnosis of dental caries on periapical radiographs. The result of the application demonstrated considerably good performance. Similar results were seen in the study done by Casalegno et al.,32 who used deep learning model designed for the detection and localization of dental lesions in near-infrared transillumination (TI) images which revealed promising results. Schwendicke et al.,48 reported using of near-infrared-light transillumination (NILT) images for diagnosing dental caries and showed that the performance of this AI based models was satisfactory.
Devito et al.,11 used an AI based ANN model for diagnosing proximal caries using the bitewing radiographs and found a quite encouraging results. Study by Hung et al.,46 reported AI technology for predicting root caries and demonstrated excellent results. Ekert et al.,37 was successful in detecting apical lesion when they applied CNNs to detect apical lesions (ALs) on panoramic dental radiographs.
Hiraiwa et al.,34 reported of applying CNNs for detection of sjögren's syndrome (SjS) on CT images and compared the results with the performance of radiologists and showed a higher diagnostic performance. In another study by Murata et al.,38 the authors applied the deep learning system for diagnosing maxillary sinusitis on panoramic radiography. The diagnostic performance of this system was sufficiently high. These results were similar to the study conducted by kim et al.,47 when compared the performance with experienced radiologists.
Ariji et al.,45 applied CNN system for deep learning image classification for diagnosing lymph node metastasis on (CT) Images and showed higher diagnosing accuracy, sensitivity, and specificity. These results were similar to the study conducted by Hung et al.,46 who assessed the performance of deep learning classification in diagnosing extra nodal extension of cervical lymph node metastases in CT images. Both the studies showed similar performance or even higher performance when compared to professional radiologists.
Lee et al.,22 evaluated the efficiency and performance of AI in diagnosis and detection of osteoporosis. In this study deep convolutional neural network (DCNN) based computer-assisted diagnosis (CAD) systems was applied for detection of osteoporosis, using panoramic radiographs and exhibited very promising results. This was well above in par with experienced oral and maxillofacial radiologists in detecting osteoporosis. These results were similar to the results done by Lee et al.,51 who used deep convolutional neural networks (DCNN) for detecting osteoporosis in dental panoramic radiographs.
Application of AI technologies in the specialty of orthodontics and dentofacial orthopedics
Accurate diagnosis, treatment planning and prediction of prognosis are the key factors for successful orthodontic treatment. AI technology has been applied for deciding if extractions are necessary prior to the orthodontic treatment. In a study by Xie et al.,12 artificial neural network (ANN) model was applied for deciding if extractions are necessary using lateral cephalometric radiographs. The results were quite promising. Jung et al.,15 showed 92% accuracy using AI expert system for deciding on permanent tooth extraction, using lateral cephalometric radiographs. The results of both the studies are suggestive that the AI modes were effective and accurate in predicting the need for extraction. These models can be used as a tool for making decisions in clinical practice. High accuracy was seen in the study by Thanathornwong,24 who suggested AI model based on bayesian network (BN) for assessing the need for orthodontic treatment.
Various studies have been conducted to demonstrate AI technologies and its application in identifying cephalometric landmarks. Park et al.,29 compared the efficiency and accuracy of the updated deep-learning algorithms for automatic identification of cephalometric landmarks using cephalometric radiographs. The results revealed that the system was extremely accurate in the computation of the landmarks. Studies conducted by Kunz et al.,49 and Hwang et al.,50 showed excellent accuracy in identifying the landmarks similar to the trained human examiners using a specialized artificial intelligence (AI) algorithm and deep learning based automated identification system respectively. Yu et al.53 demonstrated excellent results with automated skeletal classification with lateral cephalometry based on the AI Model. The results of the above mentioned studies indicates that, these systems prove to be a viable option for repeatedly identifying multiple cephalometric landmarks.
Establishing of accurate diagnosis and treatment planning in orthognathic surgery is the most important step for the success of the treatment.57 Arnet et al.,58 in his literature on facial keys to orthodontic diagnosis and treatment planning suggested that if diagnosis is incorrect, the patient esthetics may further deteriorate creating a major problem. This suggests that diagnosis is an important aspect for the dentist to analyze the problems of the patient accurately. AI technology is striving to make dentists job much accurate and precise. Choi et al.,30 reported the use of new artificial intelligence model to decide the case for surgery/non-surgery using the lateral cephalometric radiographs. He showed that the system was very effective with 96% success rate in diagnosing the surgery/non-surgery cases. This model has shown promising results, hence can be applied for the diagnosis of orthognathic surgery cases.
Hagg et al.,59 stated that determining the chronological age of the patient is not alone sufficient for estimating the actual growth time, hence various skeletal maturation indicators have been developed for this task. Determination of the growth and development, and estimation of the skeletal maturation stages have been used to predict the time of pubertal development, determining the growth rate and for mainly estimating the remaining growth and development potential of an individual as mentioned by Flores-mir et al.60 These are usually determined by using hand-wrist radiographs, cephalometric analysis, and with the help of maturation stages of cervical vertebra. AI technology has also been applied for determining the growth and development by cervical vertebrae stages. Kok H et al.,28 showed a mean accuracy of 77.02%, using artificial intelligence algorithms for determining the growth and development by cervical vertebrae stages when applied on the cephalometric radiographs.
Application of AI technologies in the specialty of endodontics
The success of root canal treatment mainly depends on accuracy of working length determination. The prognosis of the treatment can only be ensured when instrumentation terminates at the apical constriction.61 Saghiri et al.13 used artificial neural network (ANN) system in determining the working length and showed exceptional accuracy of 96% which is higher than the accuracy compared to professional endodontists. These results were similar to the study by Saghiri et al.,14 where they used the ANN system for locating the minor apical foramen, with an accuracy of 93%.
In endodontics, AI is used to diagnose vertical root fractures. A study employed by Johari et al.,16 who used probabilistic neural network (PNN) for the diagnosis of vertical root fractures. This PNN system displayed excellent performance with an accuracy of 96.6%. Similarly convolutional neural network in detecting vertical root fracture, showing a highly encouraging precision was conducted by Fukuda et al.33 These assessments indicate that AI-based models are incredibly effective when it comes to the detection of vertical root fractures on CBCT images and panoramic radiographs.
Application of AI technologies in the specialty of periodontics
Periodontal diseases are one of the most common oral diseases affecting the mankind. It is a known fact that this is one of the main reasons for the early loss of teeth. It is well reported by Lee et al.,62 that continuous progression of the disease will eventually lead to the loss of teeth in the adults. Various studies have been done to ascertain AI technology application to diagnose and predict periodontal diseases. Lee et al.,23 reported use of CAD system, based on a deep convolutional neural network (CNN) algorithm for diagnosing and predicting the teeth that are compromised with periodontal health. The outcome were quite acceptable with a mean predictive accuracy of 78.9%. Yauney et al.,27 used an AI based system based on CNNs for correlating poor periodontal health with systemic health outcomes and reported that, AI can be used for automated diagnoses and can also be useful for screenings for other diseases. Krois et al.,43 used CNNs to detect periodontal bone loss (PBL) on panoramic dental radiographs. The results of this study were similar to that of the expert opinions. This system can still help in reducing the dentist's diagnostic efforts.
Application of AI technologies in the specialty of oral and maxillofacial surgery
It is estimated that every year there are around 657,000 new cases detected of cancers of the oral cavity and pharynx and is also a reason for 330,000 deaths as noted in the article of oral cancer by WHO.63 AI technology has been used for detecting cancers. There is revolutionary development and refinement of convolutional neural networks that have demonstrated improved ability for automated cancer detection as seen in the study by Xu et al.64
Aubreville et al.,18 showed extremely positive and promising results when employed CNNs for an automatic approach for diagnosing Oral Squamous Cell Carcinoma when used with confocal laser endomicroscopy images. The study indicated that AI model will be helpful for early diagnosis. AI technology has also been used for predicting postoperative facial swelling after extraction of teeth. Zhang et al.,21 used an artificial intelligence model based on ANN for predicting the postoperative facial swelling following the extraction of impacted mandibular 3rd molars. The model demonstrated excellent results and will be of great importance for clinicians for predicting the prognosis of the treatment.
Application of AI technologies in the forensic odontology
Forensic odontology is relatively new, but it has made a stellar contribution to the field of dentistry. A dentist plays an important role when they have to identify people for child abuse, crime, sexual assault, mass calamities, and other legal issues. Their moral duty compels them to provide justice to the victims and their families, especially when there is no other evidence other than the dental remains. AI technology has been applied in this field and has shown excellent results.
De Tobel et al.,17 used automated technique based on CNNs for staging lower third molar development for estimating the age of a person after applying on panoramic radiographs. The system showed remarkable results, when compared to the trained examiners. Patil et al.,52 used ANNs to determine gender using panoramic radiographs, the results were quite promising. This system is very useful as it automates and eases the method of identifying unknown gender or age with minimal errors. Niño-Sandoval et al.,20 reported an AI model based on ANNs for predicting the mandibular morphology and demonstrated promising results. Hence AI can be used effectively in forensic dentistry.
Uses of AI in dentistry based on the conclusions from the articles reviewed in the paper
-
⁃
AI systems can assist the clinicians so they can offer high-quality dental care to their patients.
-
⁃
Dentists can use AI systems as an ancillary tool for increasing the accuracy of diagnosis, treatment planning, and predicting the treatment outcomes.
-
⁃
Non-specialty dentists can receive diagnostic support via the deep-learning systems.
-
⁃
Automated systems can save a lot of time and increase the efficiency of the clinicians (for e.g. automatic completion of electronic dental records by identifying the tooth and numbering).
-
⁃
The use of these systems for secondary opinions can improve the accuracy of diagnosis.
-
⁃
These systems provide a great deal of value for forensic diagnosis.
Conclusion
AI has revolutionized dentistry in the last few years. Studies show that these AI-powered automated systems performed extremely well in various scenarios. Few authors found them to be more accurate than even dental specialists. Although these outcomes do not make them better than the dentists, they do establish that AI can be considered for clinical applications. These systems bring terrific value to the table by improving the accuracy of diagnosis, enhancing clinical decision-making, and predicting the treatment prognosis which can help the clinicians in rendering best quality care to their patients. There are also documented studies that have also reported that these automated systems are of greater value for screening the patients for osteoporosis, oral cancer, and metastasis of the lymph nodes. This is a priceless benefit because it can help professionals to diagnose cases in the early stages, which in turn can save many lives. Although AI is widely used in various fields of dentistry, some specialties such as pedodontics and oral pathology still lack the development and application of AI technology.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
This is a non-funded research and there has been no financial support for this work that could have influenced its outcome.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jds.2020.06.019.
Contributor Information
Sanjeev B. Khanagar, Email: khanagars@ksau-hs.edu.sa.
Prabhadevi C. Maganur, Email: prabhadevi.maganur@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Rajaraman V. 2014. John McCarthy Father of artificial intelligence. Reson; pp. 198–207. [Google Scholar]
- 2.National Research Council . The National Academies Press; Washington, DC: 1999. Funding a revolution: government support for computing research; p. 302. [Google Scholar]
- 3.Bellman Richard. Thomson Course Technology; 1978. Artificial intelligence: can computers think? p. 146. [Google Scholar]
- 4.Jef Akst. The Scientist Exploring Life; Inspiring Innovation: 2019. A primer: artificial intelligence versus neural networks; p. 65802. [Google Scholar]
- 5.Rabuñal J.R., Dorado J. Artificial neural networks in real-life applications. IGI Global: Hershey. 2005:166–346. [Google Scholar]
- 6.Shortliffe E.H. Testing reality: the introduction of decision-support technologies for physicians. Methods Inf Med. 1989;28:1–5. [PubMed] [Google Scholar]
- 7.Chae Y.M., Yoo K.B., Kim E.S., Chae H. The adoption of electronic medical records and decision support systems in Korea. Healthc Inform Res. 2011;17:172–177. doi: 10.4258/hir.2011.17.3.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schleyer T.K., Thyvalikakath T.P., Spallek H., Torres-Urquidy M.H., Hernandez P., Yuhaniak J. Clinical computing in general dentistry. J Am Med Inf Assoc. 2006;13:344–352. doi: 10.1197/jamia.M1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGrath T.A., Alabousi M., Skidmore B. Recommendations for reporting of systematic reviews and meta-analyses of diagnostic test accuracy: a systematic review. Syst Rev. 2017;6:194. doi: 10.1186/s13643-017-0590-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whiting P.F., Rutjes A.W., Westwood M.E. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 11.Devito K.L., De Souza Barbosa F., Felippe Filho W.N. An artificial multilayer perceptron neural network for diagnosis of proximal dental caries. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:879–884. doi: 10.1016/j.tripleo.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Xie X., Wang L., Wang A. Artificial neural network modeling for deciding if extractions are necessary prior to orthodontic treatment. Angle Orthod. 2010;80:262–266. doi: 10.2319/111608-588.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saghiri M.A., Asgar K., Boukani K.K. A new approach for locating the minor apical foramen using an artificial neural network. Int Endod J. 2012;45:257–265. doi: 10.1111/j.1365-2591.2011.01970.x. [DOI] [PubMed] [Google Scholar]
- 14.Saghiri M.A., Garcia-Godoy F., Gutmann J.L., Lotfi M., Asgar K. The reliability of artificial neural network in locating minor apical foramen: a cadaver study. J Endod. 2012;38:1130–1134. doi: 10.1016/j.joen.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Jung S.K., Kim T.W. New approach for the diagnosis of extractions with neural network machine learning. Am J Orthod Dentofacial Orthop. 2016;149:127–133. doi: 10.1016/j.ajodo.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 16.Johari M., Esmaeili F., Andalib A., Garjani S., Saberkari H. Detection of vertical root fractures in intact and endodontically treated premolar teeth by designing a probabilistic neural network: an ex vivo study. Dentomaxillofacial Radiol. 2017;46:20160107. doi: 10.1259/dmfr.20160107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Tobel J., Radesh P., Vandermeulen D., Thevissen P.W. An automated technique to stage lower third molar development on panoramic radiographs for age estimation: a pilot study. J Forensic Odontostomatol. 2017;35:42–54. [PMC free article] [PubMed] [Google Scholar]
- 18.Aubreville M., Knipfer C., Oetter N. Automatic Classification of cancerous tissue in laser endomicroscopy images of the oral cavity using deep learning. Sci Rep. 2017;7:11979. doi: 10.1038/s41598-017-12320-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Imangaliyev S., van der Veen M.H., Volgenant C.M.C., Keijser B.J.F., Crielaard W., Levin E. Springer; 2016. Deep learning for classification of dental plaque images; pp. 407–410. [Google Scholar]
- 20.Niño-Sandoval T.C., Guevara Pérez S.V., González F.A., Jaque R.A., Infante-Contreras C. Use of automated learning techniques for predicting mandibular morphology in skeletal class I, II and III. Forensic Sci Int. 2017;281:187.e1–187.e7. doi: 10.1016/j.forsciint.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Zhang W., Li J., Li Z. Predicting postoperative facial swelling following impacted mandibular third molars extraction by using artificial neural networks evaluation. Sci Rep. 2018;8:12281. doi: 10.1038/s41598-018-29934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee J.S., Adhikari S., Liu L., Jeong H.G., Kim H., Yoon S.J. Osteoporosis detection in panoramic radiographs using a deep convolutional neural network-based computer-assisted diagnosis system: a preliminary study. Dentomaxillofacial Radiol. 2019;48:20170344. doi: 10.1259/dmfr.20170344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee J.H., Kim D.H., Jeong S.N., Choi S.H. Diagnosis and prediction of periodontally compromised teeth using a deep learning-based convolutional neural network algorithm. J Periodontal Implant Sci. 2018;48:114–123. doi: 10.5051/jpis.2018.48.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thanathornwong B. Bayesian-based decision support system for assessing the needs for orthodontic treatment. Healthc Inform Res. 2018;24:22–28. doi: 10.4258/hir.2018.24.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang K., Wu J., Chen H., Lyu P. An effective teeth recognition method using label tree with cascade network structure. Comput Med Imag Graph. 2018;68:61–70. doi: 10.1016/j.compmedimag.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Lee J.H., Kim D.H., Jeong S.N., Choi S.H. Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. J Dent. 2018;77:106–111. doi: 10.1016/j.jdent.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 27.Yauney G., Rana A., Wong L.C., Javia P., Muftu A., Shah P. Automated process incorporating machine learning segmentation and correlation of oral diseases with systemic health. EMBC. 2019:3387–3393. doi: 10.1109/EMBC.2019.8857965. [DOI] [PubMed] [Google Scholar]
- 28.Kök H., Acilar A.M., İzgi M.S. Usage and comparison of artificial intelligence algorithms for determination of growth and development by cervical vertebrae stages in orthodontics. Prog Orthod. 2019;20:41. doi: 10.1186/s40510-019-0295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park J.H., Hwang H.W., Moon J.H. Automated identification of cephalometric landmarks: part 1-comparisons between the latest deep-learning methods YOLOV3 and SSD. Angle Orthod. 2019;89:903–909. doi: 10.2319/022019-127.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi H.I., Jung S.K., Baek S.H. Artificial intelligent model with neural network machine learning for the diagnosis of orthognathic surgery. J Craniofac Surg. 2019;30:1986–1989. doi: 10.1097/SCS.0000000000005650. [DOI] [PubMed] [Google Scholar]
- 31.Patcas R., Bernini D.A.J., Volokitin A., Agustsson E., Rothe R., Timofte R. Applying artificial intelligence to assess the impact of orthognathic treatment on facial attractiveness and estimated age. Int J Oral Maxillofac Surg. 2019;48:77–83. doi: 10.1016/j.ijom.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 32.Casalegno F., Newton T., Daher R. Caries detection with near-infrared transillumination using deep learning. J Dent Res. 2019;98:1227–1233. doi: 10.1177/0022034519871884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fukuda M., Inamoto K., Shibata N. Evaluation of an artificial intelligence system for detecting vertical root fracture on panoramic radiography. Oral Radiol. 2019 doi: 10.1007/s11282-019-00409-x. [DOI] [PubMed] [Google Scholar]
- 34.Kise Y., Ikeda H., Fujii T. Preliminary study on the application of deep learning system to diagnosis of sjögren's syndrome on CT images. Dentomaxillofacial Radiol. 2019;48:20190019. doi: 10.1259/dmfr.20190019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hiraiwa T., Ariji Y., Fukuda M. A deep-learning artificial intelligence system for assessment of root morphology of the mandibular first molar on panoramic radiography. Dentomaxillofacial Radiol. 2019;48:20180218. doi: 10.1259/dmfr.20180218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tuzoff D.V., Tuzova L.N., Bornstein M.M. Tooth detection and numbering in panoramic radiographs using convolutional neural networks. Dentomaxillofacial Radiol. 2019;48:20180051. doi: 10.1259/dmfr.20180051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ekert T., Krois J., Meinhold L. Deep learning for the radiographic detection of apical lesions. J Endod. 2019;45:917–922. doi: 10.1016/j.joen.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 38.Murata M., Ariji Y., Ohashi Y. Deep-learning classification using convolutional neural network for evaluation of maxillary sinusitis on panoramic radiography. Oral Radiol. 2019;35:301–307. doi: 10.1007/s11282-018-0363-7. [DOI] [PubMed] [Google Scholar]
- 39.Chen H., Zhang K., Lyu P. A deep learning approach to automatic teeth detection and numbering based on object detection in dental periapical films. Sci Rep. 2019;9:3840. doi: 10.1038/s41598-019-40414-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vinayahalingam S., Xi T., Bergé S. Automated detection of third molars and mandibular nerve by deep learning. Sci Rep. 2019;9007 doi: 10.1038/s41598-019-45487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mallishery S., Chhatpar P., Banga K.S., Shah T., Gupta P. The precision of case difficulty and referral decisions: an innovative automated approach. Clin Oral Invest. 2020;24:1909–1915. doi: 10.1007/s00784-019-03050-4. [DOI] [PubMed] [Google Scholar]
- 42.Patcas R., Timofte R., Volokitin A. Facial attractiveness of cleft patients: a direct comparison between artificial-intelligence-based scoring and conventional rater groups. Eur J Orthod. 2019;41:428–433. doi: 10.1093/ejo/cjz007. [DOI] [PubMed] [Google Scholar]
- 43.Krois J., Ekert T., Meinhold L. Deep learning for the radiographic detection of periodontal bone loss. Sci Rep. 2019:8495. doi: 10.1038/s41598-019-44839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ariji Y., Fukuda M., Kise Y. Contrast-enhanced computed tomography image assessment of cervical lymph node metastasis in patients with oral cancer by using a deep learning system of artificial intelligence. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127:458–463. doi: 10.1016/j.oooo.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 45.Ariji Y., Sugita Y., Nagao T. CT evaluation of extranodal extension of cervical lymph node metastases in patients with oral squamous cell carcinoma using deep learning classification. Oral Radiol. 2020;36:148–155. doi: 10.1007/s11282-019-00391-4. [DOI] [PubMed] [Google Scholar]
- 46.Hung M., Voss M.W., Rosales M.N. Application of machine learning for diagnostic prediction of root caries. Gerodontology. 2019;36:395–404. doi: 10.1111/ger.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim Y., Lee K.J., Sunwoo L. Deep Learning in diagnosis of maxillary sinusitis using conventional radiography. Invest Radiol. 2019;54:7–15. doi: 10.1097/RLI.0000000000000503. [DOI] [PubMed] [Google Scholar]
- 48.Schwendicke F., Elhennawy K., Paris S., Friebertshäuser P., Krois J. Deep learning for caries lesion detection in near-infrared light transillumination images: a pilot study. J Dent. 2020;92:103260. doi: 10.1016/j.jdent.2019.103260. [DOI] [PubMed] [Google Scholar]
- 49.Kunz F., Stellzig-Eisenhauer A., Zeman F., Boldt J. Artificial intelligence in orthodontics: evaluation of a fully automated cephalometric analysis using a customized convolutional neural network. J Orofac Orthop. 2020;81:52–68. doi: 10.1007/s00056-019-00203-8. [DOI] [PubMed] [Google Scholar]
- 50.Hwang H.W., Park J.H., Moon J.H. Automated identification of cephalometric landmarks: Part 2-Might it be better than human? Angle Orthod. 2020;90:69–76. doi: 10.2319/022019-129.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee K.S., Jung S.K., Ryu J.J., Shin S.W., Choi J. Evaluation of transfer learning with deep convolutional neural networks for screening osteoporosis in dental panoramic radiographs. J Clin Med. 2020;9:392. doi: 10.3390/jcm9020392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patil V., Vineetha R., Vatsa S. Artificial neural network for gender determination using mandibular morphometric parameters: a comparative retrospective study. Cogent Engineering. 2020;7:1723783. [Google Scholar]
- 53.Yu H.J., Cho S.R., Kim M.J., Kim W.H., Kim J.W., Choi J. Automated skeletal classification with lateral cephalometry based on artificial intelligence. J Dent Res. 2020;99:249–256. doi: 10.1177/0022034520901715. [DOI] [PubMed] [Google Scholar]
- 54.Mendonça E.A. Clinical decision support systems: perspectives in dentistry. J Dent Educ. 2004;68:589–597. [PubMed] [Google Scholar]
- 55.Begum S., Ahmed M.U., Funk P., Xiong N., Von Schéele B. A case-based decision support system for individual stress diagnosis using fuzzy similarity matching. Comput Intell. 2009;25:180–195. [Google Scholar]
- 56.Khanna S. Artificial intelligence: contemporary applications and future compass. Int Dent J. 2010;60:269–272. [PubMed] [Google Scholar]
- 57.Proffit W.R., Fields H.W., Sarver D.M. 5th ed. Mosby; St Louis: 2013. Contemporary orthodontics. [Google Scholar]
- 58.Arnett G.W., Bergman R.T. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofacial Orthop. 1993;103:299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 59.Hägg U., Taranger J. Maturation indicators and the pubertal growth spurt. Am J Orthod. 1982;82:299–309. doi: 10.1016/0002-9416(82)90464-x. [DOI] [PubMed] [Google Scholar]
- 60.Flores-Mir C., Nebbe B., Major P.W. Use of skeletal maturation based on hand-wrist radiographic analysis as a predictor of facial growth: a systematic review. Angle Orthod. 2004;74:118–124. doi: 10.1043/0003-3219(2004)074<0118:UOSMBO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 61.Baugh D., Wallace J. The role of apical instrumentation in root canal treatment: a review of the literature. J Endod. 2005;31:333–340. doi: 10.1097/01.don.0000145422.94578.e6. [DOI] [PubMed] [Google Scholar]
- 62.Lee J.H., Lee J.S., Choi J.K., Kweon H.I., Kim Y.T., Choi S.H. National dental policies and socio-demographic factors affecting changes in the incidence of periodontal treatments in Vorean: a nationwide population-based retrospective cohort study from 2002-2013. BMC Oral Health. 2016;118 doi: 10.1186/s12903-016-0310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.WHO . 2020. Oral cancer.https://www.who.int/cancer/prevention/diagnosis-screening/oral-cancer/en/ [Google Scholar]
- 64.Xu B., Wang N., Chen T., Li M. 2015. Empirical evaluation of rectified activations in convolutional network.https://arxiv.org/abs/1505.00853 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.