Abstract
Background/purpose
Tongue pressure measurement conveys important information about eating and swallowing function. The Iowa Oral Performance Instrument® (IOPI) and KAY Swallowing Workstation® are internationally used for tongue pressure measurement, but for legal reasons cannot be used in Japan; rather the JMS tongue pressure measurement device® has been approved for use in Japan. However, it is not clear whether measurement obtained with these devices are directly comparable.
Materials and methods
This study investigated the correlation between the maximum tongue pressure data measured by the IOPI and the JMS tongue pressure measurement device in young healthy participants (34 males; 23.2 ± 2.0 years old, and 40 females; 21.4 ± 1.3 years old).
Results
Measurements obtained with these two devices showed significant correlations in the total cohort, and in male and female participants, separately (P < 0.05).
Conclusion
These findings demonstrate that the measurements obtained with the JMS device is comparable to those obtained with the IOPI. In Japan, JMS tongue pressure measurement device is used not only in dysphagia research field, but also geriatrics field, and extensive and detailed investigations has been carried out.
Keywords: Deglutition, Dysphagia, Tongue, Tongue pressure, Oral examination oral function
Introduction
With the increase in the elderly population, swallowing disorders and swallowing rehabilitation are increasingly gaining attention. Tongue pressure measurement is the one of the important evaluations for assessing eating and swallowing function. The Iowa Oral Performance Instrument® (IOPI, Northwest Co., LLC, Carnation, WA, USA) and KAY swallowing workstation® are internationally recognized tongue pressure measurement devices. However, the IOPI and KAY swallowing workstation are currently not permitted to be used because they were not approved as the medical device in Japan. On the other hand, the JMS tongue pressure measurement device (TPM-01, JMS Co. Ltd., Hiroshima, Japan) has been approved for use as a medical device in Japan; it has been sold since 2011 and is now used widely in clinical and research fields in Japan.
The IOPI and JMS tongue measurement devices are similar in terms of the measurement method, in that the probes of both devices should be set such that they are pressed against the hard palate by the tongue, from the tip to the middle of the tongue surface. A significant correlation between the IOPI and the prototype of tongue pressure measurement device (PS-03, ALNIC, Higashi-Hiroshima, Japan) has been reported.1
However, it remains unclear if there is a correlation between the IOPI and the TPM-01 as the second generation of PS-03. TPM-01 was common in Japan now, while PS-03 did not become widespread and wasn't commercially available because it was an exploratory device. For this reason, it is unclear whether data obtained with the TPM-01 is comparable to that obtained with the IOPI.
Thus, the main purpose of this study was to investigate whether measurements using the TPM-01 are comparable to those obtained with the IOPI.
Materials and methods
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Participants
This study was a cross-sectional study. A total of 74 participants who attended the class of dysphagia rehabilitation in the XXX University and the XXX University and applied for the participation of this study by watching poster and advertise sheet from May 1st to August 31st, 2018 were potentially eligible for the study. All participants had no history of dysphagia and maintained 28–32 teeth and occlusal contact in the premolar and molar regions with their own teeth. We excluded the people who had a symptom of dysphagia and wore orthodontic appliance.
This research was conducted with the approval of the XXX Ethics Committee (E−1053) and XXX University (Rin 17-044). Written consent was obtained from the participants prior to the start of the study. Seventy-four healthy young adults (34 men; 23.2 ± 2.0 years old, 40 women; 21.4 ± 1.3 years old) participated in this study.
Tongue pressure measurements
Measurements of maximum tongue pressure were performed using the TPM-01 and IOPI PRO™ (Model 3.1). For each participant, measurements were performed three times with each device, with the participants resting for about 30 s and rinsing their mouths between measurements to be relaxed and unify their oral conditions. The maximum value of the three measurements in both devices was confirmed by the liquid crystal display of the main body, and defined as the representative maximum tongue pressure for each subject. Furthermore, participants were allowed to rest for 5 min between measurements using the TPM-01 and IOPI PRO™.
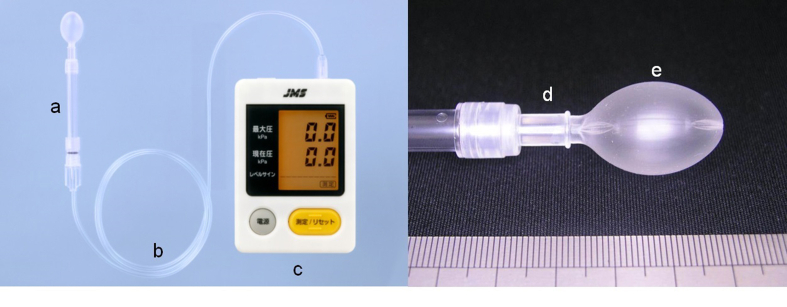
Using the TPM-01, tongue pressure was measured with a disposable probe and a simple pressure recording manometer (Fig. 1). By pushing the pressurization button in the body of TPM-01, the probe was inflated with air at an initial pressure of 19.6 kPa, setting the balloon's diameter to approximately 18 mm and the volume to 3.7 ml. This pressure was taken as zero for calibration.
Figure 1.
JMS tongue pressure measurement device. This device consists of a) disposable oral probe, b) tube, and c) digital device (TPM-01). The probe consists of d) hard plastic ring and e) air-filled balloon.
Pressures were recorded with participants seated comfortably in an upright position during all measurements. There was no difference in measurement instruction by the examiner basically between TPM-01 and IOPI measurements. In short, the differences were the design of the balloon in TPM-01 and the bulb in IOPI, and the vertical distance between upper and lower incisors because of the diameter of plastic pipe in TPM-01 (5 mm) and silicon tube in IOPI PRO™ (1 mm).
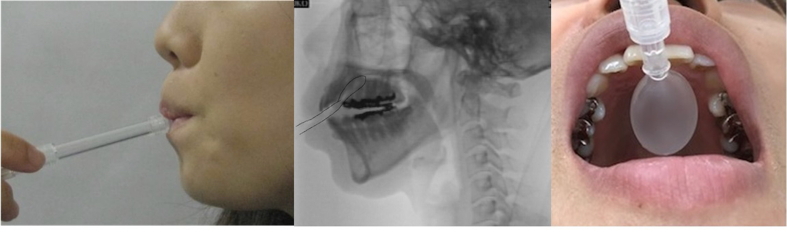
Participants were asked to place a plastic pipe lightly between the upper and lower incisors to stabilize the balloon parts in the oral cavity (Fig. 2). During all measurements, the participants held the cylinder with their incisors such that the balloon could be placed between the tongue and the anterior section of the palate. Also, the participants asked not to bite that plastic parts so hard. The pressure of the front part of the tongue, especially the tongue tip, made by the extrinsic and intrinsic muscles of the tongue against the hard palate could be measured using the probe. Participants were also asked to close their lips. Then, the examiner asked the participants to compress the balloon onto the palate for a few seconds with maximum voluntary effort. Consequently, tongue pressure is measured with the mouth slightly open, which may affect the accuracy of the measurement. The measurement method was based on the method described by Hayashi et al.2
Figure 2.
Placement of the probe of the JMS tongue pressure measurement device. A hard and plastic ring was placed between the upper and lower incisors and the balloon was placed on the tongue, from the tip to the middle of tongue.
As for the measurement of tongue pressure with IOPI PRO™ (Fig. 3), the border between the air-filled bulb and the silicon tube was placed at the center of upper incisors at first by the examiner, and participants were asked to close their mouth and lips slightly to keep bulb at the same place for the upper and lower incisors. Also, the participants asked not to bite the tube parts so hard. The bulb itself was held between the tongue and the hard palate (Fig. 4), which was the “tongue-front” measurement position that written in IOPI PRO™ use manual. The bulb was placed between the tongue and anterior part of the palate, placed just behind the alveolar ridge, and in a location similar to that used with the balloon of the TPM-01. Then, the examiner asked the participants to compress the bulb as hard as possible for a few seconds.
Figure 3.
IOPI PROTM (Model 3.1).
Figure 4.
Placement of the probe of the IOPI device. The bulb of the IOPI was placed immediately behind the upper incisors, flat, between the hard palate and the anterior part of the tongue.
Statistical analyses
The maximum values in TPM-01 and IOPI PRO™ were compared using Pearson's coefficient of correlation. The analyses were performed using SPSS version 21 (IBM Corporations, Tokyo, Japan). The statistical significance level was set at < 5%.
Results
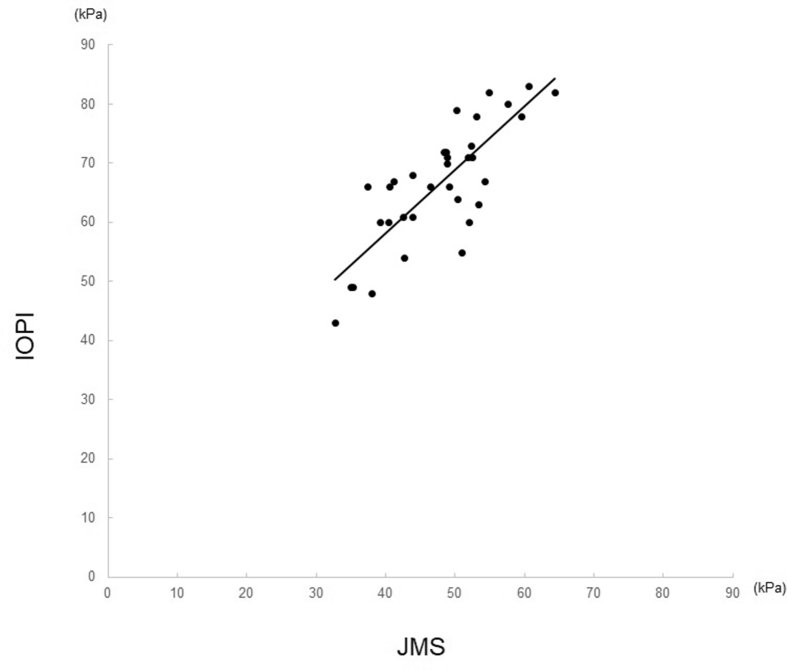
Male participants
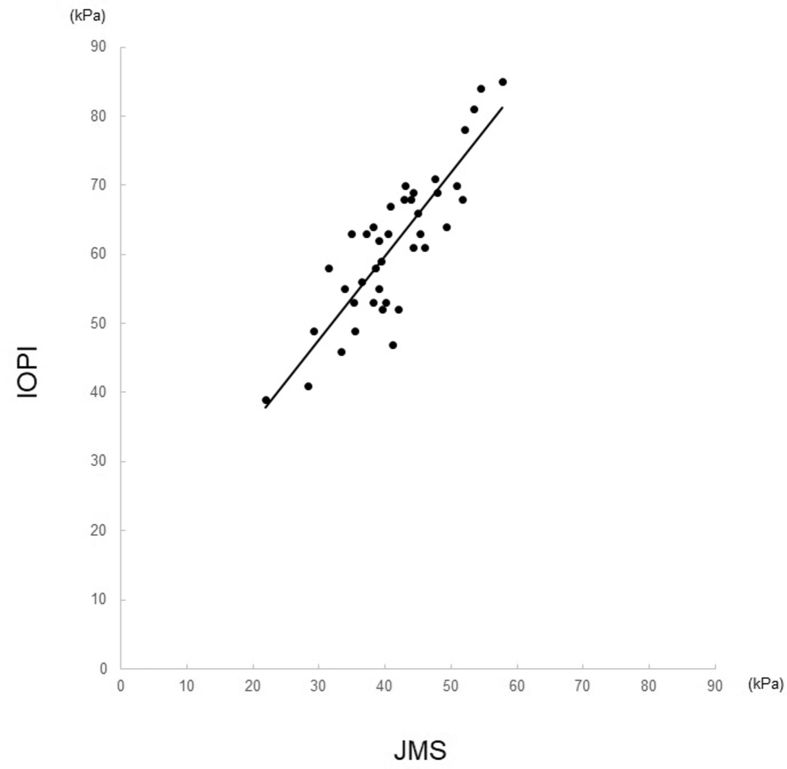
The representative maximum value for tongue pressure in the male participants using the TPM-01 was 47.6 ± 7.8 kPa and that with the IOPI was 66.3 ± 10.4 kPa. Significant correlations were found between measurements made by the TPM-01 and the IOPI PRO™ (R2 = 0.64, P < 0.01) (Fig. 5). The values were related as follows for males: IOPI PRO™ = TPM-01 × 1.07 + 15.4.
Figure 5.
Comparison of maximum tongue pressure values (kPa) in male participants obtained using the JMS (X axis) and IOPI (Y axis) devices.
Female participants
The mean value for maximum tongue pressure in female participants obtained using the TPM-01 was 41.3 ± 7.6 kPa and that obtained with the IOPI was 61.3 ± 10.7 kPa. Significant correlations were found between measurements made with the TPM-01 and the IOPI (R2 = 0.74, P < 0.01) (Fig. 6). The two measurements in female participants were related as follows: IOPI PRO™ = TPM-01 × 1.21 + 11.2.
Figure 6.
Comparison of maximum tongue pressure values (kPa) in female participants obtained using the JMS (X axis) and IOPI (Y axis) devices.
Discussion
In this study, we compared tongue pressure measurements obtained with the internationally used IOPI PRO™ and TPM-01 used in Japan.
The data in this study suggest that the tongue pressure measurements obtained by TPM-01 are comparable to pressures obtained by IOPI PRO™ in males (IOPI PRO™ = TPM-01 × 1.07 + 15.4) as well as females (IOPI PRO™ = TPM-01 × 1.21 + 11.2).
TPM-01 can be used to generate useful, meaningful and valid tongue pressure values. Our study found that the maximum tongue pressure measured by the IOPI PRO™ was slightly higher than that measured by TPM-01. The average tongue pressures in our study, as measured using the JMS device, were 47.6 ± 7.8 kPa in males and 41.3 ± 7.6 kPa in females. These values were similar to the previously reported standard values of individuals in their twenties (41.8 ± 10.8 kPa overall, 46.5 ± 9.8 kPa in males, 36.9 ± 9.6 in females).3
The evaluation of tongue function was often quite subjective, though the range of motion, strength, and coordination were basically the clinical evaluation of swallowing function. However, it become clearer for the dysphagia patients to be able to get the objective assessments and treatment goals including changing tongue performance during swallowing and speech after the development of tongue pressure measurement devices.
In the super-aged society of Japan, tongue pressure measurement is utilized in many contexts, including geriatric research. Deterioration of tongue pressure has been reported with aging,3 stroke,4 neuromuscular diseases,5, 6, 7, 8 malnutrition, sarcopenia,9 and tongue cancer.10 It has also been reported that deterioration of tongue pressure is frequently found in the dependent elderly.11 There is a correlation between the food texture level and tongue pressure in the elderly.12 Moreover, a tongue pressure of 25–30 kPa by TPM-01 is reportedly needed to maintain a healthy life expectancy,13 which is particularly relevant to the Japanese super-aged society. Tongue pressure is one of the indexes of oral frailty defined by the Japanese Society of Gerodontology. The relationship between physical function and tongue pressure in community-dwelling elderly14 and low tongue pressure in individuals with sarcopenia people and dynapenia15 has become clear. Yoshikawa et al. reported the relationship between IOPI and PS-03 which was the prototype of TPM-01.1 PS-03 was not generic because it was an exploratory device. On the other hand, TPM-01 was marketed as a medical equipment in 2011, and there are many users in clinical and research fields now in Japan. Some researchers give the presentations of their research in the international congresses nowadays, but often got troubled with questions “How many kPa of your data in IOPI?” from the researchers in USA and European countries. Therefore, the results in this study might contribute to their troubles.
The IOPI is globally used for measuring tongue pressure and is used in rehabilitation of dysphagic patients.16 Previous reports using this device have described the effects of aging on tongue pressure,17 the increased risk of dysphagia in elderly individuals with low tongue pressure,18 the relationship between handgrip and tongue pressure,19 jumping mechanography and tongue pressure,20 tongue pressure in Parkinson's disease patients,21 strength training to improve tongue pressure,22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 and tongue pressure in head and neck cancer patients.35,36
Thus, tongue pressure measurement is generic, useful, safe, and can be able to reflect some parts of swallowing function and the results of swallowing rehabilitation objectively.
This study had some limitations, in that only young participants were included, although the standard values of tongue pressure of each gender with PS-03 in the generation of 20 s, 30 s, 40 s, 50 s, 60 s, and 70 s more over had already reported.3
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The author would like to express their sincere appreciation to Dr. Hida E for his tremendous support.
References
- 1.Yoshikawa M., Yoshida M., Tsuga K., Akagawa Y., Groher M.E. Comparison of three types of tongue pressure measurement devices. Dysphagia. 2011;26:232–237. doi: 10.1007/s00455-010-9291-3. [DOI] [PubMed] [Google Scholar]
- 2.Hayashi R., Tsuga K., Hosokawa R., Yoshida M., Sato Y., Akagawa Y. A novel handy probe for tongue pressure measurement. Int J Prosthodont (IJP) 2002;15:385–388. [PubMed] [Google Scholar]
- 3.Utanohara Y., Hayashi R., Yoshikawa M., Yoshida M., Tsuga K., Akagawa Y. Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia. 2008;23:286–290. doi: 10.1007/s00455-007-9142-z. [DOI] [PubMed] [Google Scholar]
- 4.Nakamori M., Hosomi N., Ishikawa K. Prediction of pneumonia in acute stroke patients using tongue pressure measurements. PloS One. 2016;11 doi: 10.1371/journal.pone.0165837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Umemoto G., Tsuboi Y., Kitashima A., Furuya H., Kikuta T. Impaired food transportation in Parkinson's diseases related to lingual bradykinesia. Dysphagia. 2011;26:250–255. doi: 10.1007/s00455-010-9296-y. [DOI] [PubMed] [Google Scholar]
- 6.Mano T., Katsuno M., Bannno H. Tongue pressure as a novel biomarker of spinal and bulbar muscular atrophy. Neurology. 2014;82:255–262. doi: 10.1212/WNL.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 7.Hiraoka A., Yoshikawa M., Nakamori M. Maximum tongue pressure is associated with swallowing dysfunction in ALS patients. Dysphagia. 2017;32:542–547. doi: 10.1007/s00455-017-9797-z. [DOI] [PubMed] [Google Scholar]
- 8.Kikutani T., Tamura F., Nishikaki K. Case presentation: dental treatment with PAP for ALS patient. Int J Orofac Myol. 2006;32:32–35. [PubMed] [Google Scholar]
- 9.Maeda K., Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015;30:80–87. doi: 10.1007/s00455-014-9577-y. [DOI] [PubMed] [Google Scholar]
- 10.Hamahata A., Beppu T., Shirakura S. Tongue pressure in patients with tongue cancer resection and reconstruction. Auris Nasus Larynx. 2014;41:563–567. doi: 10.1016/j.anl.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Tsuga K., Yoshikawa M., Oue H. Maximal voluntary tongue pressure is decreased in Japanese frail elderly persons. Gerodontology. 2012;29:e1078–e1085. doi: 10.1111/j.1741-2358.2011.00615.x. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka Y., Nakano Y., Yokoo M., Takeda Y., Yamada K., Kayashita J. Examination about the relation of meal form, tongue pressure, grip and walking state in inpatient and elderly residents. Jpn J Dysphagia Rehabil. 2015;19:52–62. (in Japanese) [Google Scholar]
- 13.Tabuchi K., Norikoshi K., Kobayashi T. Literature review on tongue pressure of healthy Japanese. Sci J Publ Health. 2018;6:86–90. [Google Scholar]
- 14.Mihara Y., Matsuda K., Ikebe K. Association of handgrip strength with various oral functions in 82- to 84- year-old community-dwelling Japanese. Gerodontology. 2018;35:214–220. doi: 10.1111/ger.12341. [DOI] [PubMed] [Google Scholar]
- 15.Suzuki M., Koyama S., Kimura Y. Relationship between characteristics of skeletal muscle and oral function in community-dwelling older women. Arch Gerontol Geriatr. 2018;79:171–175. doi: 10.1016/j.archger.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 16.Adams V., Mathisen B., Baines S., Lazarus C., Callister R. A systematic review and meta-analysis of measurements of tongue and hand strength and endurance using the Iowa oral performance instrument (IOPI) Dysphagia. 2013;28:350–369. doi: 10.1007/s00455-013-9451-3. [DOI] [PubMed] [Google Scholar]
- 17.Nicosia M.A., Hind J.A., Roecker E.B. Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A Biol Sci Med Sci. 2000;55:M634–M640. doi: 10.1093/gerona/55.11.m634. [DOI] [PubMed] [Google Scholar]
- 18.Robbins J., Levine R., Wood J., Roecker E.B., Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50:M257–M262. doi: 10.1093/gerona/50a.5.m257. [DOI] [PubMed] [Google Scholar]
- 19.Adams V., Mathisen B., Baines S., Lazarus C., Callister R. Reliability of measurements of tongue and hand strength and endurance using the Iowa oral performance instrument with elderly adults. Disabil Rehabil. 2015;37:389–395. doi: 10.3109/09638288.2014.921245. [DOI] [PubMed] [Google Scholar]
- 20.Buehring B., Hind J., Fidler E., Krueger D., Binkley N., Robbins J. Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc. 2013;61:418–422. doi: 10.1111/jgs.12124. [DOI] [PubMed] [Google Scholar]
- 21.Pitts L.L., Morales S., Stierwalt J.A.G. Lingual pressure as a clinical indicator of swallowing function in Parkinson's disease. J Speech Lang Hear Res. 2018;61:257–265. doi: 10.1044/2017_JSLHR-S-17-0259. [DOI] [PubMed] [Google Scholar]
- 22.Robbins J., Gangnon R.E., Theis S.M., Kays S.A., Hewitt A.L., Hind J.A. The effects of lingual exercise on swallowing older adults. J Am Geriatr Soc. 2005;53:1483–1489. doi: 10.1111/j.1532-5415.2005.53467.x. [DOI] [PubMed] [Google Scholar]
- 23.Robbins J., Kays S.A., Gangnon R.E., Hind J.A., Hewitt A.L., Hind J.A. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88:150–158. doi: 10.1016/j.apmr.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Yeates E.M., Molfenter S.M., Steele C.M. Improvements in tongue strength and pressure-generation precision following a tongue-pressure training protocol in older individuals with dysphagia: three case reports. Clin Inerv Aging. 2008;3:735–747. doi: 10.2147/cia.s3825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lazarus C., Logemann J.A., Huang C.F., Rademaker A.W. Effects of two types of tongue strengthening exercises in young normals. Folia Phoniatrica Logop. 2003;55:199–205. doi: 10.1159/000071019. [DOI] [PubMed] [Google Scholar]
- 26.Van den Steen L., Schellen C., Verstraelen K. Tongue -strengthening exercises in healthy older adults: specificity of bulb position and detraining effects. Dysphagia. 2018;33:337–344. doi: 10.1007/s00455-017-9858-3. [DOI] [PubMed] [Google Scholar]
- 27.Steele C.M., Bayley M.T., Peladeau-Pigeon M. A randomized trial comparing two tongue-pressure resistance training protocols for post-stroke dysphagia. Dysphagia. 2016;31:452–461. doi: 10.1007/s00455-016-9699-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steele C.M., Bayley M.A., Peladeau-Pigeon M., Stokely S.L. Tongue pressure profile training for dysphagia post stroke (TPPT): study protocol for an exploratory randomized controlled trial. Trials. 2013;14:126. doi: 10.1186/1745-6215-14-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steele C.M., Bayley G.L., Polacco R., Hori S.F., Molfenter S.M., Yeates E.M. Outcomes of tongue-pressure strength and accuracy training for dysphagia following acquired brain injury. Int J Speech Lang Pathol. 2013;15:492–502. doi: 10.3109/17549507.2012.752864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oh J.C. Effect of the head extension swallowing exercise on suprahyoid muscle activity in elderly individuals. Exp Gerontol. 2018;110:133–138. doi: 10.1016/j.exger.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Park J.S., Kim H.J., Oh D.J. Effects of tongue strength training using the Iowa oral performance instrument in stroke patients with dysphagia. J Phys Ther Sci. 2015;27:3631–3632. doi: 10.1589/jpts.27.3631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van den Steen L., Vanderwegen J., Guns C., Elen R., De Bodt M., Van Nuffelen G. Tongue - strengthening exercises in healthy older adults: does exercise load matter? A randomized controlled trial. Dysphagia. 2019;34:315–324. doi: 10.1007/s00455-018-9940-5. [DOI] [PubMed] [Google Scholar]
- 33.Namasivayam-MacDonald A.M., Burnett L., Nagy A., Waito A.A., Steele C.M. Effects of tongue strength training on mealtime function in long-term care. Am J Speech Lang Pathol. 2017;26:1213–1224. doi: 10.1044/2017_AJSLP-16-0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lazarus C.L., Logemann J.A., Pauloski B.R. Effects of radiotherapy with or without chemotherapy on tongue strength and swallowing in patients with oral cancer. Head Neck. 2007;29:632–637. doi: 10.1002/hed.20577. [DOI] [PubMed] [Google Scholar]
- 35.Lazarus C.L., Logemann J.A., Pauloski B.R. Swallowing and tongue function following treatment for oral and oropharygeal cancer. J Speech Lang Hear Res. 2000;43:1011–1023. doi: 10.1044/jslhr.4304.1011. [DOI] [PubMed] [Google Scholar]
- 36.Van den Steen L., Vanderveken O., Vanderwegen J. Member of the Belgian Cancer Plan 29_033_Dysphagia Group. Feasibility of tongue strength measurements during (chemo) radiotherapy in head and neck cancer patients. Support Care Canc. 2017;25:3417–3423. doi: 10.1007/s00520-017-3761-1. [DOI] [PubMed] [Google Scholar]