Abstract
Background/purpose
Extraction of impacted mandibular third molar (MTM) is one of the most common procedures in clinical dental treatment; building a decision tree to perform MTM extraction can be prudent in alleviating periodontal diseases. This study is to review the latest research on the management of periodontal osseous defect (POD) after MTM extraction and rebuild a new clinical decision tree.
Materials and methods
Current study was conducted according to PRISMA statement. Medline, Embase, Scopus, and Google Scholar were searched concerning treatment of MTM extraction up to Oct.2019. Three focused questions revolving around asymptomatic versus disease site, age, and necessity of ridge preservation after >6 months follow up will be answered.
Results
A total of 7 studies were included for meta-analysis. Evidences were inadequate in regards to asymptomatic vs disease site of MTM extraction in the long-term follow-up. For patients with age <25 years, postoperative probing depth (PD) always remained at < 4 mm. However, for patients with age >25 years with initial PD > 7 mm, residual pockets still remained at 5 mm. For ridge preservation, significant positive effect in reduction of second molar distal site PD was observed, regardless of different biomaterials being placed (z = 4.69, p < 0.00001).
Conclusion
Age is of utmost importance in preoperative evaluation during impacted MTM extraction. The timing for ridge preservation is essential determinant for achieving optimal treatment outcome. The clinical decision tree as proposed could serve as guidance when dealing with POD after impacted MTM extraction.
Keywords: Impacted third molar, Ridge preservation, Periodontal osseous defect, Clinical decision tree, Systematic review, Meta-analysis
Introduction
There have been countless studies on surgical guidelines and procedures in management of impacted mandibular third molar (MTM), with asypmtomatic and second molar periodontal osseous defect (POD) treatment in particular; however most results still remain to be controversial. Currently it is still a challenge in making decisions on whether to receive MTM extractions, more specifically as to when and how the procedure should be done.
As early as 1932, Montelius reported higher total incidence of impactions in Chinese than those of Caucasian patients.1 Impacted MTM are always found in Asian Chinese people, with occurrence of 3.2 times more in the mandible than in the maxilla of Singapore Chinese population.2 Furthermore, MTM were the most common impacted teeth (82.5%) than others among the 3853 impacted teeth in Hong Kong Chinese population.3 The main factors in contributing impacted third molars include insufficient dental arch space to accommodate tooth eruption, ectopic or abnormal eruptive pathway, existence of associated pathology, and other reasons.
Unfortunately, complication of deep MTM extraction is common in the formation of intrabony defects at the distal site of adjacent second molar. The loss of heavy wide alveolar processes contour always show intrabony pockets and vertical resorptive lesions of the bone housing, notably with mandibular molar teeth more prone to be affected.4 In order to improve bone healing after tooth extraction, the use of graft and/or membranes was reported to be effective in controlling POD; clinically, loss of width in sites without intervention ranging from 2.46 to 4.56 mm as compared to 1.14–2.5 mm in sites using graft and/or membranes, conversely, loss of height in control sites ranging from 0.9 to 3.6 mm was compared to a gain of 1.3 mm and a loss of 0.62 mm for sites using graft and/or membranes.5 Furthermore, a study on Taiwanese patients with a mean follow up years of 8.66, observed significant increase in both radiographic bony destruction and intrabony defect formation on the distal aspect of second molar after MTM extraction without any ridge preservation as compared to the control group (congenitally missing third molar).6
Thus, the objective of this study is to gather the latest research on impacted MTM and summarize the concept behind several procedures, ultimately to rebuild a new clinical decision tree in treating impacted MTM and timing for ridge preservation.
Materials and methods
Study registration
The review protocol was registered with the PROSPERO (International Prospective Register of Systematic Reviews) hosted by the Centre for Reviews and Dissemination, University of York, National Institute for Health Research, United Kingdom under the identification number CRD42018115702.
Research design
This systemic review and meta-analysis was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.7
Type of studies
Three focused questions to be addressed:
-
1.
Are asymptomatic site of third molar free from disease in long-term follow up?
-
2.
Can age be an independent factor in evaluating MTM extraction?
-
3.
Will ridge preservation enhance postoperative extraction prognosis?
Search strategy
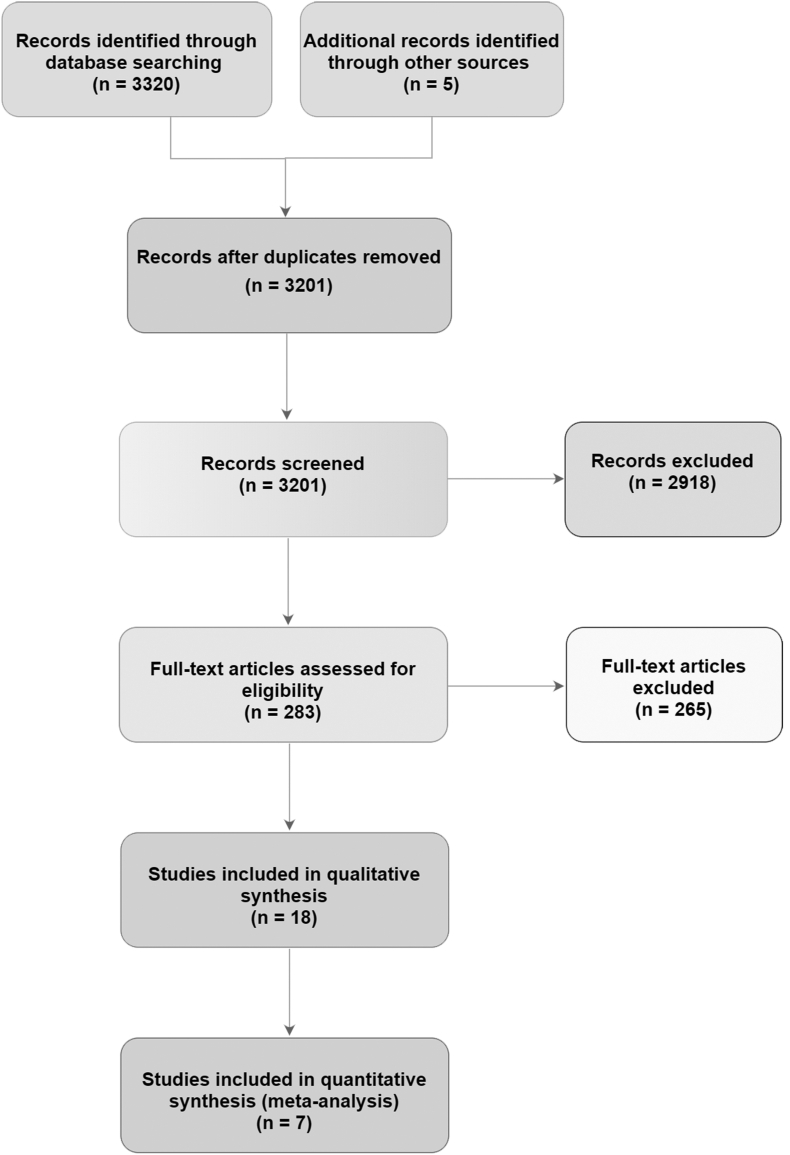
Electronic databases were searched for articles that are eligible for this review, including the MEDLINE (Pubmed), EMBASE, Scopus, and Google Scholar. Bibliographies of articles and conference proceedings were checked for additional studies. The following search strategy was used with a combination of MeSH (Medical Subject Headings) terms (impact∗ AND ( [wisdom tooth] or [third molar]) AND ([defect] or [osseous defect] or [periodontal] or [probing depth] or [PD]) and ([guided tissue regeneration] or [GTR] or [periodontal regeneration] or [regenerative therapy]). No publication year or language limit was used, and the last search was conducted on Oct. 2019. The full search strategy was shown in Fig. 1.
Fig. 1.
Flowchart of search strategy and screening process.
Subjects/participants
Types of participant
Participants included in the studies with the following characteristic:
-
1.
Age of participants was denoted clearly in the inclusion criteria
-
2.
Undergoing impacted MTM extraction with same or different kind of surgical approaches
-
3.
With or without ridge preservation under different type of biomaterials
-
4.
Follow up duration of at least 6 months
Types of intervention
The interventions of interest were included:
-
1.
Asymptomatic or disease site – Compare whether or not the impacted third molar existed in disease free condition
-
2.
Age – Compare the age between included participants
-
3.
Ridge preservation – Compare the benefit of with or without ridge preservation
Selection criteria
Inclusion criteria
The inclusion criteria of the selected articles for present systematic review were as follows:
-
1.
Randomized clinical trials (RCT), prospective and retrospective controlled clinical trials (CCT)
-
2.
Diagnosis of third molar impaction based on radiographic examination
-
3.
Age of patients was defined clearly and in good general health
-
4.
A minimum follow up time of 6 months
-
5.
Outcome variables evaluating the changes of baseline and postoperative data
Exclusion criteria
The exclusion criteria of the selected articles for present systematic review were as follows:
-
1.
In vivo & in vitro study, animal studies, and personal opinion
-
2.
Articles based on Editor's choices or interviews
-
3.
Patients with a systemic disease
-
4.
A follow up period of <6 months
-
5.
Data analysis presenting only in median value
-
6.
Incomplete or no clinical initial measurement outcomes
Data collection procedure
Section of studies
The eligibility of papers and data extraction were carried out by two reviewers (S–H. Low and S-L. Lu). Endnote X7 software was used to manage all included literatures for current study. This study was approved by the Taipei Medical University Joint Institutional Review Board (Approval No. 201305008).
Data extraction
Two reviewers (S–H. Low and S-L. Lu) independently screen the titles and abstracts of articles to exclude articles with unrelated topics. Full texts of potential articles were read for data extraction. Any disagreements were resolved by discussion, and a third reviewer (H–K. Lu) was consulted when necessary. When an agreement cannot be reached, data was excluded until further clarification was available. Only data directly associated with measures of the outcome were extracted. Inter-examiner agreement was evaluated by calculating the kappa value.
Outcome measures
The outcome measures of interest in this review included:
-
1.
The clinical condition before third molar extraction
-
2.
Subject age
-
3.
Preoperative probing depth (PD) over second molar distal site
-
4.
Postoperative PD over second molar distal site
-
5.
PD change after different kind of surgical approaches
Assessment of risk of bias
Quality assessment of risk of bias were recorded, assessed, and classified according to Cochrane Handbook for Systematic Reviews of Intervention8 with the following six domains: 2 selection bias (sequence generation, allocation concealment), performance and detection bias (blinding of participants, operators, examiners), attrition bias (loss to follow up and missing values or participants), reporting bias (selective reporting, unclear withdrawals, missing outcomes) and other bias.
The risk of bias and quality of evidence assessment was performed independently and in duplicate by two reviewers (S.H. Low and S.L Lu). For each study, an assessment of low, high, or unclear risk of bias were given. Low risk, if all criteria were met, moderate risk when only one criterion was missing, and high risk if two or more criteria were missing. Overall risk of bias for each domain across all studies were tabulated by RevMan version 5.3 software (Cochrane Collaboration, Copenhagen, Denmark).
Statistical analysis
To assess heterogeneity, we calculated the I2 statistic. Heterogeneity was defined as low, high, or unclear.9 Estimated effect sizes and 95% CIs based on individual studies and combined analyses were displayed with forest plots. Meta-analysis was performed to evaluate the correlation between the primary outcome and the different variables. P < 0.05 was considered statistically significant. All statistical analyses and forest plots were performed and drawn with statistical software RevMan software (Review Manager, version 5.3., Cochrane Collaboration, Copenhagen, Denmark), with fixed- and random-effects models.
Results
Search strategy and screening process
The flowchart of search strategy and screening process was summarized in Fig. 1. In brief, a total of 3320 records were identified through electronic search and 5 records from hand search. After exclusion of duplicates, 3201 articles remained for title and abstract screening. 2918 articles were excluded and 283 records were left for full text assessment. Finally, 18 studies were included for qualitative review and 7 studies were included for meta-analysis.
The reasons for excluded studies which were categorized into 4 details: (1) unclear presentation of the clinical parameters, incomplete or no clinical initial measurement outcomes; (2) data analysis presenting only in median value; (3) unquantifiable/indirect clinical measurements, radiographic assessment only and (4) follow up periods of <6 months (Table 1).
Table 1.
Brief overview of the excluded studies.
| Study | Reasons for exclusion |
|---|---|
|
Karapataki, 2000 Kan, 2002 Chang, 2004 Kaul, 2012 Durmuslar, 2014 Singh, 2015 Ge, 2016 |
Unclear presentation of the clinical parameters, incomplete or no clinical initial measurement outcomes |
|
Montevecchi, 2014 Cortell-Basllester, 2015 |
Data analysis presenting only in median value |
|
Faria, 2013 Faria, 2013 Walker, 2017 |
Unquantifiable/indirect clinical measurements, radiographic assessment only |
|
Suarez-Cnquerio, 2003 Sammartino, 2005 Chaves, 2008 Sammartino, 2009 Kim, 2011 Baqain, 2012 Korkmaz, 2015 Kumar, 2015 |
Follow up periods <6 months |
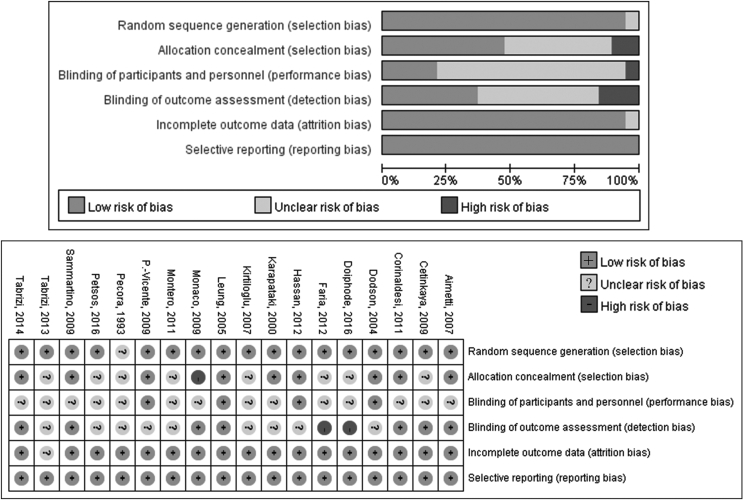
Risk of bias assessment
All included studies were assessed for risk of bias, and results were summarized in Fig. 2. The kappa value between 2 reviewers (S–H. Low and S-L. Lu) was 0.91.
Fig. 2.
Risk of bias of the included studies.
The high risks of bias are mostly in the area of allocation concealment, blinding of participants, and the outcome assessors. Of all 18 included studies, the risks of bias assessment were low to unclear risk.
Qualitative review and meta-analysis of studies
The summary of the included studies were listed in Table 2. Of the 18 studies included in the qualitative evaluation, 8 split-mouth RCTs,10, 11, 12, 13, 14, 15, 16, 17 4 parallel RCTs,18, 19, 20, 21 2 split-mouth CCTs,22,23 and 4 parallel CCTs.24, 25, 26, 27
Table 2.
Summary of included studies.
| 1st Author, year | Study Design | No. of patients recruited | Age range (mean, years) | Characteristics of impacted 3rd molar | Socket debridementa | Grafting materials | Membrane Selection | Max. F/U periods (months) | Preoperative PD (mean ± SD, mm) | Postoperative PD (mean ± SD, mm) |
|---|---|---|---|---|---|---|---|---|---|---|
| Pecora,20 1993 | RCT, parallel | 20 Test:10 Ctrl:10 |
26–50 | Horizontal, unclear | Yes (scaling and RP) | No | Test: e-PTFE (Gore-Tex®) Ctrl: No | 12 | Test: 9.00 ± 2.49 Ctrl: 8.90 ± 2.08 |
Test: 3.30 ± 0.95 Ctrl: 4.90 ± 1.45 |
| Karapataki,18 2000 | RCT, parallel | 18 | 43 ± 7 | Unclear | Yes (scaling and RP) | No | T1: PLA (Guidor®) T2: e-PTFE (Gore-Tex®) |
12 | T1: 9.50 ± 1.40 T2: 8.20 ± 1.10 |
T1: 4.20 ± 1.40 T2: 4.60 ± 1.30 |
| Dodson,12 2004 | RCT, split-mouth | 24b T1:12 T2:12 |
≥26 T1: 31.3 ± 7.1 T2: 28.1 ± 2.6 |
Mesioangular, distoangular, horizontal or vertical, fully or partial impacted | Yes (RP) | T1: Allograft (Grafton®) C1: No T2: No C2: No |
T1: No C1: No T2: Collagen membrane (Biomend®) C2: No |
6 | T1: 7.30 ± 3.50 C1: 7.90 ± 2.20 T2: 6.20 ± 2.30 C2: 5.40 ± 2.50 |
T1: 3.70 ± 1.60 C1: 4.60 ± 1.50 T2: 4.30 ± 1.40 C2: 3.60 ± 1.20 |
| Leung,19 2005 | RCT, parallel | 30 Test: 14 Ctrl: 16 |
Test: 35.7 ± 6.8 Ctrl: 28.9 ± 7.3 |
Mesioangular impacted | Test: Yes (scaling) Ctrl: No |
No | No | 6 | Test: 6.10 ± 1.40 Ctrl: 6.50 ± 1.50 |
Test: 3.20 ± 1.20 Ctrl: 5.20 ± 0.70 |
| Aimetti,10 2007 | RCT, split-mouth | 15 | 24.9 ± 5.46 | Mesioangular, fully soft tissue impacted | Yes (scaling and RP) | No | Test: PGA/PLA (Gore Resolut XT®) Ctrl: No |
12 | Test: 5.13 ± 0.43 Ctrl: 4.92 ± 0.59 |
Test: 2.24 ± 0.34 Ctrl: 4.37 ± 0.58 |
| Kırtıloğlu,14 2007 | RCT, split-mouth | 18c | 16-32 (20.8) | Vertical or mesioangular, fully impacted | Unclear | No | No | 12 | T1: 2.89 ± 0.58 T2: 2.78 ± 0.65 |
T1: 3.00 ± 0.69 T2: 2.56 ± 0.70 |
| Cetinkaya,22 2009 | CCT, split-mouth | 15d | 16-21 (18.53 ± 1.60) | Vertical or mesioangular, fully bony impacted | No | No | No | 6 | T1: 2.87 ± 0.52 T2: 2.93 ± 0.70 |
T1: 3.00 ± 0.76 T2: 3.93 ± 0.70 |
| Monaco,15 2009 | RCT, split-mouth | 12e | 15-19 (16) | Incompletely root formed, unclear | Unclear | Collagen sponge | No | 6 | T1: 2.70 ± 0.20 T2: 2.90 ± 0.20 |
T1: 2.70 ± 0.30 T2: 2.80 ± 0.20 |
| Sammartino,16 2009 | RCT, split-mouth | 45f T1:30 T2:30 Ctrl:30 |
21–30 | Mesioangular or horizontal, soft tissue or bony impacted | Yes (scaling and RP depends on case) | T1: Xenograft (Bio-Oss®) T2: Xenograft (Bio-Oss®) Ctrl: No |
T1: No T2: Collagen membrane (Bio-Gide®) Ctrl: No |
72 | T1: 7.60 ± 0.55 T2: 7.66 ± 0.55 Ctrl: 7.68 ± 0.56 |
T1:3.88 ± 0.45 T2: 3.15 ± 0.20 Ctrl: 6.40 ± 0.51 |
| P.-Vicente,21 2009 | RCT, parallel | 43g | >18 | Mesioangular, fully or partial impacted | Yes (scaling or RP) | No | No | 6 | T1: 4.75 ± 0.90 T2: 5.50 ± 1.27 |
T1: 4.00 ± 0.67 T2: 4.70 ± 0.95 |
| Corinaldesi,11 2011 | RCT, split-mouth | 11h | 32–55 | Mesioangular and horizontal, fully bony impacted | Yes (scaling and RP) | No | T1: Collagen membrane (Biomend®) T2: e-PTFE (Gore-Tex®) |
9 | T1: 9.10 ± 3.50 T2: 9.20 ± 3.00 |
T1: 3.90 ± 1.50 T2: 3.70 ± 1.40 |
| Montero,25 2011 | CCT, parallel | 48i | 18-29 (23.1 ± 6.1) | Fully or partial impacted | Unclear | No | No | 12 | Deep: 6.50 ± 1.90 Shallow: 3.80 ± 0.80 |
Deep: 3.70 ± 1.60 Shallow: 1.50 ± 1.10 |
| Faria,24 2013 | CCT, parallel | 25 patients with 40 teeth | 16-35 (21.03 ± 4.38) | Mesioangular, horizontal or vertical, fully impacted | Yes (scaling and RP) | No | No | 12 | 5.70 ± 3.80 | 3.77 ± 2.86 |
| Hassan,13 2012 | RCT, split-mouth | 14 | 30-35 (32.0 ± 2.03) | Horizontal impacted | Yes (RP) | Test: Xenograft (Bio-Oss®) Ctrl: No |
Test: Collagen membrane (Bio-Gide®) Ctrl: No |
12 | Test: 7.50 ± 0.70 Ctrl: 7.80 ± 0.80 |
Test: 3.10 ± 0.40 Ctrl: 4.90 ± 0.50 |
| Tabrizi,27 2013 | CCT, parallel | 42 | 18-25 (20.9) | Mesioangular, fully impacted | Unclear | No | No | 6 | 2.71 ± 0.59 | 3.60 ± 0.88 |
| Tabrizi,17 2014 | RCT, split-mouth | 20 | 25-30 (26.5 ± 1.9) | Mesioangular or horizontal, fully impacted | Unclear | T1: Allograft (Cenobone®) C1: No T2: Allograft (Cenobone®) + lincomycin (Upjohn SA®) C2: No |
T1: No C1: No T2: No C2: No |
6 | T1: 3.10 ± 2.10 C1: 3.90 ± 1.40 T2: 3.55 ± 1.30 C2: 2.85 ± 0.90 |
T1: 2.20 ± 1.10 C1: 2.30 ± 0.60 T2: 2.50 ± 0.50 C2: 2.70 ± 0.90 |
| Doiphode,23 2016 | CCT, split-mouth | 30 | 18–30 | Fully or partial impacted | Unclear | T1: PRP T2: PRF Ctrl: No |
T1: No T2: No Ctrl: No |
6 | T1: 4.20 ± 0.52 T2: 2.68 ± 0.55 Ctrl: 4.35 ± 0.39 |
T1: 1.77 ± 0.21 T2: 1.29 ± 0.33 Ctrl: 2.99 ± 0.34 |
| Petsos,26 2016 | CCT, parallel | 78 | 16.0 ± 2.0 | Fully impacted | Unclear | No | No | 6 | 3.25 ± 0.65 | 2.57 ± 0.50 |
Ctrl: Control; RP:root planing; Max. F/U: maximum follow up; PD: probing depth; RCT: randomized clinical trial; CCT: controlled clinical trial.
Socket debridement over 2nd molar distal side.
T1: Demineralized bone powder therapy T2:GTR therapy C1,C2:Control group.
T1: Triangular flap T2: modified Szmyd Flap.
T1: Anchor suture T2: Simple suture.
T1: Triangular flap T2: Envelope Flap.
T1: Xenograft T2: Xenograft & Collagen membrane Control:untreated.
T1:≤ 25 years group T2: >25 years group.
T1: Resorbable membrane group T2: Non-resorbable membrane group.
authors divided the molar position into 2 groups which were deep molars or shallow molars.
Asymptomatic versus disease site of third molar
Due to the settings of present inclusion criteria, none of the included articles reported and/or relevantly discussed the issue on asymptomatic versus disease site of third molar in a long-term follow up. Regretfully, the scope and emphasis of the included articles could not adequately answer our first focus question.
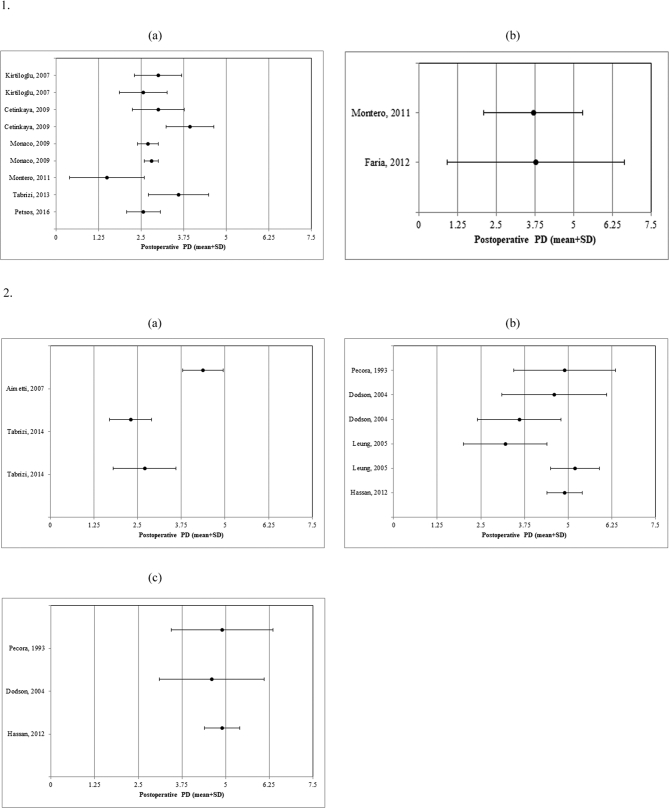
Age
According to the included data, from studies with participants within the mean age of 25 years and below, we found that regardless of whether preoperative PD over second molar distal site was lesser or greater than 5 mm, the postoperative PD over second molar distal site would still remain lesser than 4 mm (Figs. 3–1).
Fig. 3.
1. The postoperative PD over second molar distal site of patients with mean age of <25 years. (a) Preoperative PD < 5 mm. (b) Preoperative PD > 5 mm 2.The postoperative PD over second molar distal site of patients with mean age of >25 years. (a) Preoperative PD < 5 mm. (b) Preoperative PD > 5 mm. (c) Preoperative PD > 7 mm
In contrast, participants with mean age of 25 years and above, the initial PD over second molar distal site were >5 or 7 mm, the results for postoperative PD over second molar distal site did not have a coherent result, more pronounced in cases with initial PD of >7 mm, the residual pockets still remained to be around 5 mm even after 6 months of extraction (Figs. 3–2).
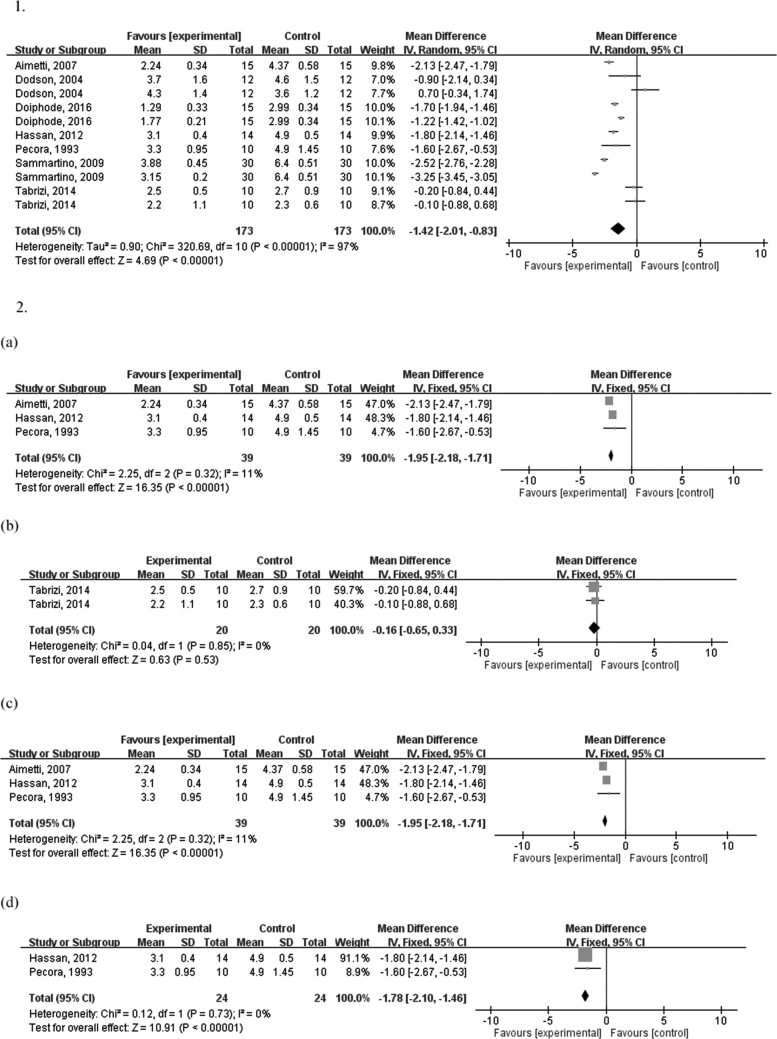
Ridge preservation
For ridge preservation over MTM extraction site, significant positive effect can be seen in the reduction of second molar distal site PD, regardless of the different biomaterials being placed during the 6 months follow up period (z = 4.69, p < 0.00001), a higher heterogeneity was reported (I2 = 97%) (Figs. 4–1).
Fig. 4.
1. Weighted mean difference of PD over second molar distal site after >6 months follow up. 2. Weighted mean difference of PD over second molar distal site with mean age >25 years and more than 12 months follow up. (a) Membrane used. (b) Preoperative PD < 5 mm. (c) Preoperative PD > 5-7 mm. (d) Preoperative PD > 7 mm.
Membrane used
When comparing between the membrane being used (bioresorbable or non-resorbable) with control group under detailed circumstance, definition of mean age being > 25 years, and follow up periods of >12 months, we presented that there was significant positive effect in PD reduction over second molar distal site as compared to the control group (z = 16.35, p < 0.00001, I2 = 11%) (Figs. 4–2a).
Preoperative probing depth <5 mm over second molar distal site
Predictably, under the circumstance with preoperative PD < 5 mm over second molar distal site, no significant impact was observed on PD reduction postoperatively in the follow up period of >12 months under the mean age of >25 years (z = 0.63, p = 0.53, I2 = 0%) (Figs. 4–2b).
Preoperative probing depth > 5–7 mm over second molar distal site
In a fixed-effects analysis for conditions of preoperative PD > 5–7 mm over second molar distal site, significant difference was found on PD reduction over second molar distal site after postoperative period of >12 months under the mean age of >25 years (z = 16.35, p < 0.00001, I2 = 11%) (Figs. 4–2c).
Preoperative probing depth >7 mm over second molar distal site
In fixed-effects analysis for conditions of preoperative PD > 7 mm over second molar distal site, significant positive effect was calculated for the PD reduction over second molar distal site after postoperative period of over 12 months under the mean age of >25 years (z = 10.91, p < 0.00001, I2 = 0%) (Figs. 4–2d).
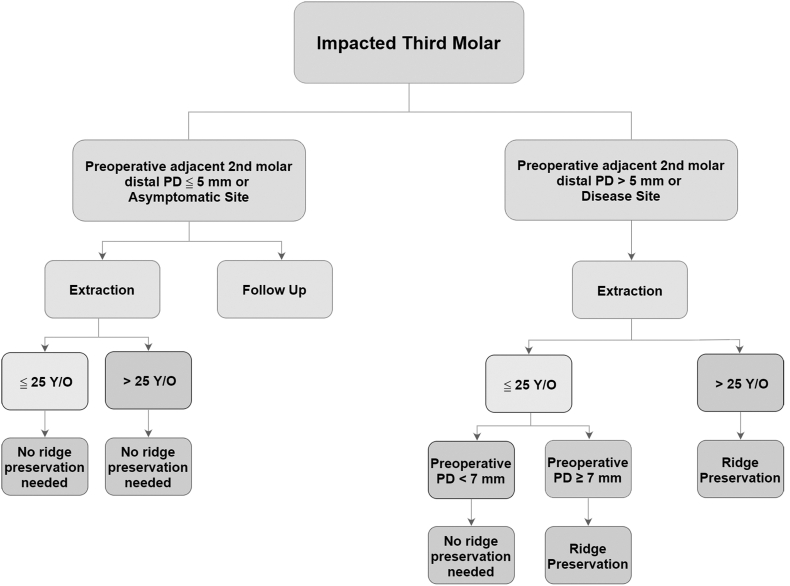
Clinical decision making dealing with impacted third molar
Our current outcomes and results of present systematic review and analysis, an evidence-based and optimized clinical decision-making tree was to be demonstrated in Fig. 5. The clinical periodontal assessment along with preoperative evaluation of age and ridge preservation after extraction are the important key factors in making clinical decision during impacted third molar extraction.
Fig. 5.
Clinical decision making dealing with impacted third molar.
Discussion
The aim of this study was to review in detail the latest research on managing impacted MTM and establish a new clinical decision tree. There were substantial amount of articles being published concerning current topic, but there was limited evidence regarding long-term clinical follow up with complete clinical data (Table 1). To address our focus questions, long-term clinical study is essential to the cause, thus we looked for articles with study frame of at least 6 months and up to a year of statistics in order to investigate concrete clinical scenarios. Comprehensive discussion of each focus questions will be explored in the following three sections.
In reviewing asymptomatic versus disease site of third molar, there were no articles that are in line with the criteria we have established. A recent split-mouth study observed that the third molar group has a significantly higher PD over second molar distal site than the extraction group in elderly patients (age > 25 years), furthermore there was also significant prevalence of distal caries over second molar (p = 0.003).28
With a median follow up of 5.9 years, white et al. found that the severity of the initial periodontal disease was significantly increased at the site of young adults with present disease (PD > 4 mm) in the third molar as compared to baseline. This proves that the risk of disease still remains substantial for retained third molar, which is probably due to lack of periodontal maintenance.29 Moreover in a study of 262 participants with over 2 years follow up, Fisher et al. concluded that routine dental prophylaxis in patients with asymptomatic third molar site has almost no impact on reducing deep PD in young adults.30
In 2016, a longitudinal study on first and second molars of 416 subjects reported that presence of third molar may increase the risk of second molar pathology from a range of 1.74–4.88-fold. In the same study, the survival plot demonstrated how loss of third molar optimizes the chance of second molar survival.31 It has been reported by another study that even non-impacted third molar may influence adjacent second molar periodontal health and/or other pathologies, as observed through 1958 participants.32
Similarly, a systemic review that included 7 studies of sample sizes ranging from 70 to 821 subjects with follow up periods of 1–18 years by Bouloux et al. concluded that initial asymptomatic third molars that require extraction may progress towards periodontal disease at a mean incidence rate of 3.0% (ranging from 1.0 to 9.0%) annually.33 Therefore risks and benefits of molar extraction and retention, along with age of patients should be taken into consideration while discussing treatment outcomes.
However in a Cochrane systemic review on comparing outcomes of wisdom tooth surgical extraction and retention, there were not enough robust evidence to elucidate whether removal of wisdom tooth is advantageous in preventing periodontal destruction progression.34 Due to insufficient evidence that indicates, further RCTs and prospective cohort studies are warranted, as well as taking patients’ age, type of impaction, baseline periodontal situation, and other circumstances into account before deciding between extraction or retention of asymptomatic third molar as the appropriate treatment.
While identification of asymptomatic versus disease was one of the deciding factors, age of patients is another crucial point to consider. It was known that prevalence and severity of post-surgery complication increases with age, a consensus of literature as presented by both Bataineh and Valmaseda-Castellon had concluded that postoperative risks from third molar extraction may increase with age,35,36 more specifically there may be a higher chance of postoperative fracture when the mean age is at 45 years, as observed by Krimmel.37 Faria et al. reported that of 26 impacted MTM extracted from 16 patients with mean age of 21.12 ± 4.80 years, only 3.8% had radiographic infrabony defect of ≥6 mm (1/26) and 96.2% with ≤5 mm (25/26) at 12 months follow up,24 thus supporting the idea that extraction of impacted molar yields better periodontal outcome at a younger age.
The age of 25 years was chosen as the cut-off point for patients in present study, mainly because there has been several large scale research in the past to support the rationale. As early as 1985, Kugelberg et al. has noted the occurrence of periodontal defects after MTM removal over the age of 25 is 2–3 times more common, suggesting postoperative defects were indeed age related.38 Additionally, Kugelberg observed that 51% of patients over the age of 26 had postoperative defects following MTM extraction, being twice as common as those under 25 year of age.39 Again in a different study, 215 s molars were quantified for significant postoperative defects in both age groups, confirming that POD were 3 times more common over the age of 25.40
In our study, we found that postoperative PD over second molar distal site would still remain <5 mm for all of the participants with mean age of <25 years, regardless of initial PD over second molar distal site being lesser or greater than 5 mm. Even with preoperative MTM PD conditions of either shallow (<5 mm) or deep (>5 mm) in initial evaluation, Montero and Mazzaglia also showed significant reduction in PD in both groups after 1 year of follow up for young adults.25 On the contrary, with participants aging ≥ 25 years, the results for postoperative PD over second molar distal site do not have consistent outcome without any ridge preservation intervention. Furthermore, undergoing third molar extraction at the age of >25 years would increase risk of complications (odds ratio = 1.5, p = 0.05).41
Several researches agreed on the age of ≤25 as the average age for MTM root formations. Maber et al. reported that the age of third molar apex closure at 97th percentile is 24.18 years in girls and 23.47 years in boys.42 Liversidge also found out that the average age of apex closure was 19.27–20.88 in both White and Bangladeshi children from London and Black African, Cape colored children from South Africa.43 The development of the MTM shows strong correlation with age.
Thus, age was an independent factor for third molar extraction. The age of 25 years can be considered as an effective and powerful cut-off age in postoperative defects treatment before MTM extraction.
The purpose of ridge preservation is to limit and prevent soft tissue from collapsing into extraction sockets, to achieve reduction of alveolar ridge resorption, while simultaneously supporting vital bone formation.44,45
According to recent systemic review and meta-analysis, there is limited evidence to support which biomaterials provide optimal results in vital bone formation, and all of the osteoinduction still depends on the characteristic of biomaterials being used.46,47 Nevertheless, present discussion in regards to the determination of a decision tree will put its emphasis on diagnostic and treatment strategy rather than evaluating the usage of different graft materials.
In the age group of <25 years, despite PD being more or less than 5 mm, oftentimes spontaneous healing will occur under follow up with any ridge preservation after a certain period of time. Of all asymptomatic impacted MTM in 78 patients with mean age of 16.0 ± 2.0 years, Petsos et al. found that the group with preoperative PD ≥ 4 mm has significant reduction of 2.6 ± 0.5 mm (p < 0.05) after 6 months.26 In 48 patients with mean age of 23.1 years, Montero and Mazzaglia observed progressive decrease from mean preoperative PD > 5 mm to a final mean PD of 2.6 ± 0.8 mm after 12 months were observed.25 Thus, ridge preservation may not be recommended for the age < 25 years under MTM extraction.
To sum up some evidence mentioned earlier, in the course of ≥25 years of age, we generally need to perform ridge preservation after extraction, especially under circumstances of disease or with PD ≥ 5 mm. Pecora et al. observed a statistically significant benefit for using GTR therapy as opposed to no intervention in study subjects aged 26 years or greater, with their PD decreasing from 9 ± 2.5 mm to 3.3 ± 1.0 mm a year post-surgery.20 Besides, in a RCT study by Hassan et al., there was a statistically significant gain in the CAL and a reduction in PD of the grafted sites as compared to the nongrafted sites (p < 0.001) 12 months after MTM removal.13
Although we have excluded Sammartino study due to its mean age being unclearly defined, the results of the study are quite interesting. They randomly assigned 90 MTM impactions into three groups: xenograft (Bio-Oss) alone, xenograft plus collagen membrane (Bio-Gide), and untreated control group. The group of xenograft plus collagen membrane had the best outcome for the prevention of second molar periodontal defect after 6 years, when compared to xenograft (Bio-Oss) alone (7.60 ± 0.55 mm to 3.88 ± 0.45 mm). From the results we conclude that usage of membrane provides potential benefit in ridge preservation.16
Two recent meta-analysis48,49 also showed that ridge preservation can provide adjunctive clinical benefit as effective in gaining CAL or reducing PD at the distal site of the mandibular second molar as compared to MTM extraction without ridge preservation procedures. Thus, ridge preservation should be considered as a main role for postoperative outcome. Ridge preservation can always be an alternative choice in creating successful and long-lasting support for periodontal defects after MTM extraction, in particularly for cases with severe intrabony destruction, deep PD, and being over the age of 25 years.
As previously demonstrated, clinicians should review the benefits and risks of MTM extraction and retention. Consequently, the age and asymptomatic or disease site, as well as the timing for ridge preservation under circumstances mentioned above, should be in first consideration before proceeding with extraction in order to achieve decent treatment outcome. The decision tree proposed here could serve as guidance for clinicians on how to deal with impacted MTM. Further studies are still needed to create a more comprehensive and accurate treatment plan prior to MTM extraction.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
This research has been prepared without any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required. The authors acknowledge the support of the writers of the primary studies who provided data and information for this study. Furthermore, special thanks to Prof. Li-Sheng Chen (Taipei Medical University) and Dr. Jiiang-Huei Jeng (National Taiwan University) for their helpful comments.
References
- 1.Montelius G. Impacted teeth a comparative study of Chinese and caucasian dentitions. J Dent Res. 1932;12:931–938. [Google Scholar]
- 2.Quek S., Tay C., Tay K., Toh S., Lim K. Pattern of third molar impaction in a Singapore Chinese population: a retrospective radiographic survey. Int J Oral Maxillofac Surg. 2003;32:548–552. [PubMed] [Google Scholar]
- 3.Chu F., Li T., Lui V., Newsome P., Chow R., Cheung L. Prevalence of impacted teeth and associated pathologies- a radiographic study of the Hong Kong Chinese population. Hong Kong Med J. 2003;9:158–163. [PubMed] [Google Scholar]
- 4.Goldman H.M., Cohen D.W. The infrabony pocket: classification and treatment. J Periodontol. 1958;29:272–291. [Google Scholar]
- 5.Morjaria K.R., Wilson R., Palmer R.M. Bone healing after tooth extraction with or without an intervention: a systematic review of randomized controlled trials. Clin Implant Dent Relat Res. 2014;16:1–20. doi: 10.1111/j.1708-8208.2012.00450.x. [DOI] [PubMed] [Google Scholar]
- 6.Peng K.Y., Tseng Y.C., Shen E.C., Chiu S.C., Fu E., Huang Y.W. Mandibular second molar periodontal status after third molar extraction. J Periodontol. 2001;72:1647–1651. doi: 10.1902/jop.2001.72.12.1647. [DOI] [PubMed] [Google Scholar]
- 7.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Higgins J.P., Green S. John Wiley & Sons; UK, Oxford: 2011. Cochrane handbook for systematic reviews of interventions. [Google Scholar]
- 9.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aimetti M., Pigella E., Romano F. Clinical and radiographic evaluation of the effects of guided tissue regeneration using resorbable membranes after extraction of impacted mandibular third molars. Int J Periodontics Restor Dent. 2007;27:51–59. [PubMed] [Google Scholar]
- 11.Corinaldesi G., Lizio G., Badiali G., Morselli-Labate A.M., Marchetti C. Treatment of intrabony defects after impacted mandibular third molar removal with bioabsorbable and non-resorbable membranes. J Periodontol. 2011;82:1404–1413. doi: 10.1902/jop.2011.100466. [DOI] [PubMed] [Google Scholar]
- 12.Dodson T.B. Management of mandibular third molar extraction sites to prevent periodontal defects. J Oral Maxillofac Surg. 2004;62:1213–1224. doi: 10.1016/j.joms.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 13.Hassan K.S., Marei H.F., Alagl A.S. Does grafting of third molar extraction sockets enhance periodontal measures in 30-to 35-year-old patients? J Oral Maxillofac Surg. 2012;70:757–764. doi: 10.1016/j.joms.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Kırtıloğlu T., Bulut E., Sümer M., Cengiz İ. Comparison of 2 flap designs in the periodontal healing of second molars after fully impacted mandibular third molar extractions. J Oral Maxillofac Surg. 2007;65:2206–2210. doi: 10.1016/j.joms.2006.11.029. [DOI] [PubMed] [Google Scholar]
- 15.Monaco G., Daprile G., Tavernese L., Corinaldesi G., Marchetti C. Mandibular third molar removal in young patients: an evaluation of 2 different flap designs. J Oral Maxillofac Surg. 2009;67:15–21. doi: 10.1016/j.joms.2007.05.032. [DOI] [PubMed] [Google Scholar]
- 16.Sammartino G., Tia M., Bucci T., Wang H.L. Prevention of mandibular third molar extraction-associated periodontal defects: a comparative study. J Periodontol. 2009;80:389–396. doi: 10.1902/jop.2009.080503. [DOI] [PubMed] [Google Scholar]
- 17.Tabrizi R., Khorshidi H., Shahidi S., Gholami M., Kalbasi S., Khayati A. Use of lincomycin-impregnated demineralized freeze-dried bone allograft in the periodontal defect after third molar surgery. J Oral Maxillofac Surg. 2014;72:850–857. doi: 10.1016/j.joms.2013.11.028. [DOI] [PubMed] [Google Scholar]
- 18.Karapataki S., Hugoson A., Falk H., Laurell L., Kugelberg C.F. Healing following GTR treatment of intrabony defects distal to mandibular 2nd molars using resorbable and non-resorbable barriers. J Clin Periodontol. 2000;27:333–340. doi: 10.1034/j.1600-051x.2000.027005333.x. [DOI] [PubMed] [Google Scholar]
- 19.Leung W.K., Corbet E.F., Kan K.W., Lo E., Liu J.K. A regimen of systematic periodontal care after removal of impacted mandibular third molars manages periodontal pockets associated with the mandibular second molars. J Clin Periodontol. 2005;32:725–731. doi: 10.1111/j.1600-051X.2005.00773.x. [DOI] [PubMed] [Google Scholar]
- 20.Pecora G., Celletti R., Davarpanah M., Covani U., Etienne D. The effects of guided tissue regeneration on healing after impacted mandibular third-molar surgery: 1-year results. Int J Periodontics Restor Dent. 1993;13:397–407. [Google Scholar]
- 21.Pons-Vicente O., Valmaseda-Castellón E., Berini-Aytés L., Gay-Escoda C. Effect on pocket depth and attachment level of manual versus ultrasonic scaling of lower second molars following lower third molar extraction: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e11–e19. doi: 10.1016/j.tripleo.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Cetinkaya B.O., Sumer M., Tutkun F., Sandikci E.O., Misir F. Influence of different suturing techniques on periodontal health of the adjacent second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:156–161. doi: 10.1016/j.tripleo.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 23.Doiphode A.M., Hegde P., Mahindra U., Kumar S.S., Tenglikar P.D., Tripathi V. Evaluation of the efficacy of platelet-rich plasma and platelet-rich fibrin in alveolar defects after removal of impacted bilateral mandibular third molars. J Int Soc Prev Community Dent. 2016;6:47–52. doi: 10.4103/2231-0762.181167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faria A.I., Gallas-Torreira M., López-Ratón M., Crespo-Vázquez E., Rodríguez-Núñez I., López-Castro G. Radiological infrabony defects after impacted mandibular third molar extractions in young adults. J Oral Maxillofac Surg. 2013;71:2020–2028. doi: 10.1016/j.joms.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 25.Montero J., Mazzaglia G. Effect of removing an impacted mandibular third molar on the periodontal status of the mandibular second molar. J Oral Maxillofac Surg. 2011;69:2691–2697. doi: 10.1016/j.joms.2011.06.205. [DOI] [PubMed] [Google Scholar]
- 26.Petsos H., Korte J., Eickholz P., Hoffmann T., Borchard R. Surgical removal of third molars and periodontal tissues of adjacent second molars. J Clin Periodontol. 2016;43:453–460. doi: 10.1111/jcpe.12527. [DOI] [PubMed] [Google Scholar]
- 27.Tabrizi R., Arabion H., Gholami M. How will mandibular third molar surgery affect mandibular second molar periodontal parameters? Dent Res J. 2013;10:523–526. [PMC free article] [PubMed] [Google Scholar]
- 28.Chou Y.H., Ho P.S., Ho K.Y., Wang W.C., Hu K.F. Association between the eruption of the third molar and caries and periodontitis distal to the second molars in elderly patients. Kaohsiung J Med Sci. 2017;33:246–251. doi: 10.1016/j.kjms.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 29.White R.P., Phillips C., Hull D.J., Offenbacher S., Blakey G.H., Haug R.H. Risk markers for periodontal pathology over time in the third molar and non–third molar regions in young adults. J Oral Maxillofac Surg. 2008;66:749–754. doi: 10.1016/j.joms.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Fisher E.L., Blakey G.H., Offenbacher S., Phillips C., White R.P. Mechanical debridement of subgingival biofilm in participants with asymptomatic third molars does not reduce deeper probing depths in the molar regions of the mouth. J Oral Maxillofac Surg. 2013;71:467–474. doi: 10.1016/j.joms.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 31.Nunn M., Fish M., Garcia R. Retained asymptomatic third molars and risk for second molar pathology. J Dent Res. 2013;92:1095–1099. doi: 10.1177/0022034513509281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Z.B., Qu H.L., Zhou L.N., Tian B.M., Chen F.M. Influence of non-impacted third molars on pathologies of adjacent second molars: a retrospective study. J Periodontol. 2017;88:450–456. doi: 10.1902/jop.2016.160453. [DOI] [PubMed] [Google Scholar]
- 33.Bouloux G.F., Busaidy K.F., Beirne O.R., Chuang S.-K., Dodson T.B. What is the risk of future extraction of asymptomatic third molars? A systematic review. J Oral Maxillofac Surg. 2015;73:806–811. doi: 10.1016/j.joms.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 34.Ghaeminia H., Nienhuijs M.E., Toedtling V. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst Rev. 2020;5:CD003879. doi: 10.1002/14651858.CD003879.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bataineh A.B. Sensory nerve impairment following mandibular third molar surgery. J Oral Maxillofac Surg. 2001;59:1012–1017. doi: 10.1053/joms.2001.25827. [DOI] [PubMed] [Google Scholar]
- 36.Valmaseda-Castellón E., Berini-Aytés L., Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:377–383. doi: 10.1067/moe.2001.118284. [DOI] [PubMed] [Google Scholar]
- 37.Krimmel M., Reinert S. Mandibular fracture after third molar removal. J Oral Maxillofac Surg. 2000;58:1110–1112. doi: 10.1053/joms.2000.9566. [DOI] [PubMed] [Google Scholar]
- 38.Kugelberg C.F., Ahlström U., Ericson S., Hugoson A. Periodontal healing after impacted lower third molar surgery: a retrospective study. Int J Oral Surg. 1985;14:29–40. doi: 10.1016/s0300-9785(85)80007-7. [DOI] [PubMed] [Google Scholar]
- 39.Kugelberg C.F. Periodontal healing two and four years after impacted lower third molar surgery: a comparative retrospective study. Int J Oral Maxillofac Surg. 1990;19:341–345. doi: 10.1016/s0901-5027(05)80077-3. [DOI] [PubMed] [Google Scholar]
- 40.Kugelberg C.F., Ahlström U., Ericson S., Hugoson A., Kvint S. Periodontal healing after impacted lower third molar surgery in adolescents and adults: a prospective study. Int J Oral Maxillofac Surg. 1991;20:18–24. doi: 10.1016/s0901-5027(05)80689-7. [DOI] [PubMed] [Google Scholar]
- 41.Chuang S.K., Perrott D.H., Susarla S.M., Dodson T.B. Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg. 2007;65:1685–1692. doi: 10.1016/j.joms.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 42.Maber M., Liversidge H., Hector M. Accuracy of age estimation of radiographic methods using developing teeth. Forensic Sci Int. 2006;159:S68–S73. doi: 10.1016/j.forsciint.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 43.Liversidge H. Timing of human mandibular third molar formation. Ann Hum Biol. 2008;35:294–321. doi: 10.1080/03014460801971445. [DOI] [PubMed] [Google Scholar]
- 44.Araújo M.G., Silva C.O., Misawa M., Sukekava F. Alveolar socket healing: what can we learn? Periodontol. 2000;68:122–134. doi: 10.1111/prd.12082. [DOI] [PubMed] [Google Scholar]
- 45.Barallat L., Ruíz-Magaz V., Levi P.A., Jr., Mareque-Bueno S., Galindo-Moreno P., Nart J. Histomorphometric results in ridge preservation procedures comparing various graft materials in extraction sockets with nongrafted sockets in humans: a systematic review. Implant Dent. 2014;23:539–554. doi: 10.1097/ID.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 46.Avila-Ortiz G., Elangovan S., Kramer K., Blanchette D., Dawson D. Effect of alveolar ridge preservation after tooth extraction a systematic review and meta-analysis. J Dent Res. 2014;93:950–958. doi: 10.1177/0022034514541127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chan H.L., Lin G.H., Fu J.H., Wang H.L. Alterations in bone quality after socket preservation with grafting materials: a systematic review. Int J Oral Maxillofac Implants. 2013;28:710–720. doi: 10.11607/jomi.2913. [DOI] [PubMed] [Google Scholar]
- 48.Lee C.T., Hum L., Chen Y.W. The effect of regenerative periodontal therapy in preventing periodontal defects after the extraction of third molars: a systematic review and meta-analysis. J Am Dent Assoc. 2016;147:709–719. doi: 10.1016/j.adaj.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 49.Barbato L., Kalemaj Z., Buti J. Effect of surgical intervention for removal of mandibular third molar on periodontal healing of adjacent mandibular second molar: a systematic review and bayesian network meta-analysis. J Periodontol. 2016;87:291–302. doi: 10.1902/jop.2015.150363. [DOI] [PubMed] [Google Scholar]