Abstract
Introduction: Behavioral activation therapy (BAT) is designed to help individuals’ approach and access sources of positive reinforcement in their life, which can serve a natural antidepressant function and efforts to help depressed people reengage in their life through focused activation strategies.
Methods: In this study, 60 individuals were selected and randomly assigned to intervention and control groups. The intervention group received behavioral activation treatment, including eight treatment sessions and 5 weeks later, a follow-up study was conducted. The data were collected, using a Beck Depression Inventory-II and behavioral activation system (BIS)/ behavioral inhibition system (BAS) Carver and White questionnaires, before the intervention and after the intervention and five weeks after the intervention. SPSS 23 and analysis of covariance (ANCOVA) was used for data analysis.
Results: Results showed a significant increase in the two components of the BAS including reward seeking and response to reward in the intervention group, which indicates an increase in positive affect and appetitive motivation for reward seeking and decreases the risk of depression. Also, the results showed a significant decrease in the BIS and depression in the intervention group, which indicates a decline in experiencing negative emotions.
Conclusion: The implementation of BAT will cause depressed people to try to maximize future rewards and it’s effective in improving the reward seeking and reward response in depressed people because this treatment will increase the positive reinforcement and lead to learning cues that predict possible rewards in environments.
Keywords: Behavior therapy, Reward, Reinforcement, Psychology, Depression
Introduction
In pathology of mood disorders and depression, various factors are involved. 1 One of the new approaches to the pathology and treatment of depression is the neuropsychological perspective.1 Over the past few decades, research on the biological basis has identified certain regions of the brain and transmitters involved in the rewards. A related theory is the theory of brain reward deficiency syndrome, according to which the pleasure is a definite neurological function which is linked to the complex system of rewards and reinforcement.2,3 This syndrome is a form of sensory deprivation of pleasure mechanisms in the brain, which makes people not enjoy normal rewards and daily activities, and this factor leads to mental disorders such as depression.4 Lack of pleasure implies no interest in reaction to the pleasurable stimulants or experiences and lack of anticipation of pleasure, which is one of the main symptoms of depression. Lack of pleasure has been known to influence the motivation of depressed people in participating in potentially rewarding experiences.5
Collected evidence shows that hedonism (seeking pleasure and avoiding suffering) processing is not a single structure, but consists of a prediction phase and a conclusion phase, that is, in a depressed person, desire and motivation are separated. This finding suggests that pleasure is not a single structure, and in a depressed person, the lack of motivation for reward is primarily due to low levels of anticipation of pleasure rather than a decrease in interest.6,7 Also the importance of studying the reward processes can be illustrated by the fact that in certain conditions, one reward function can be impaired while the others remain intact. For example, individuals with major depression disorder have similar hedonic responses to sweet solutions compared to controls,8 but are less likely to engage in tasks requiring higher amounts of effort.9
Another theory is the reinforcement-learning model. This model draws on the assumption that an organism acts to maximize future rewards, and the brain estimates and holds in memory the value of possible actions based on the amount of reward each action has yielded in the past. In other words, an organism uses these stored values to predict, for any possible action, the likely resulting rewards or punishments. The actual reward gained from an action is then compared with the prediction, but this prediction is defective in depressed people.10,11
The researchers have also studied the individual basis of neuroscience in having or avoiding motivation. One of such studies is Davidson’s approach and withdrawal systems.12 This model has two separate systems of motivation and emotion and presents the approach system and withdrawal system. The approach system is hypothesized to control target and reward-based behaviors and in response to incentives and rewards and other positive stimuli. As the organism has a great motivation for a pleasurable goal, the approach system considers organism as the responsible of producing particular positive emotions. This system suggests that depression is considered to be a defect in approach motivation, therefore depressed people are considered as being less responsive to rewards. In support of this theory, several empirical studies reported that dysphoric students and those with major depression respond less to rewards compared to the control group.12
McFarland et al.,13 study results partially supported the hypothesis that behavioral activation system (BAS) deficits predict a worsening six-month course of depression. An underactive BAS is hypothesized to be related to a reduction in positive affect and appetitive motivation, increasing the risk for depression. Also, based on the cognitive behavioral approach and according to the model of Ferster,14 depression is a chain of loss, reduction or lack of rewards and inability to obtain rewards. In behavioral models, depression is caused by the failure to achieve reinforcements or the lack of dependence between individual behaviors and reinforcements.13
Therefore, considering that depressed people that have deficiency in reward seeking and tend to avoid certain behaviors, the purpose of this study is to improve the pattern of seeking rewards in depressed people by using behavioral activation therapy (BAT). BAT is an effective treatment for depression, because it helps to individuals’ approach and access sources of positive reinforcements in their life, which can serve a natural antidepressant function. BAT is a type of short-term psychotherapy used to reduce the symptoms of depression and prevent its onset. This type of treatment is premised on the hypothesis that people who are vulnerable to depressive disorder and provide inadequate responses to these problems, thus reducing their ability to receive rewards in their living environment, thus causing the symptoms of depressive disorder to appear in them. The goals of treatment activation are to systematically enhance the behavior of activities in a way that helps clients achieve greater rewards in their lives and solve their life’s problems. The process of behavioral activation treatment focuses directly on increasing some activities and preventing others (such as avoiding some behaviors and reducing the amount of mental rumination).15 In this way, the study of Gawrysiak et al.,16 showed the BAT group in post test phase than the control group had a significantly reductions in symptoms of depression and increased environmental reward which is consistent with our results. Also, Zemestani et al.,17 showed that BAT had a significant effect on reducing depression, anxiety symptoms, and rumination. Similarly, Takagaki et al.,18 indicated that adolescent students in the group BAT showed significant improvements (effect size −0.90, 95% CI −1.28 to −0.51) in their depressive symptoms in compared to the control group.
In contrast, Arias-Carrion and Poppel19 reported that depressed people might be less likely than non-depressed people to seek rewards, because they are less pleased with their rewards. Also, if the reduced motivation is completely related to anhedonia, then therapies such as cognitive behavior therapy (CBT (and BAT that are used as a positive reinforcement sources are not expected to be effective.19
Overall, the examination of the results of previous research shows that they reached to increasing the environmental reinforcements and reducing symptoms of depression with behavioral activation treatments is sufficient, But in the present study, we have tried to come up with a new and varied approach to the etiology of depression based on theories of brain reward deficiency syndrome, reinforcement learning model, Frester14 model, Davidson’s12 theory of approach/withdrawal system, and behavioral activation and inhibition system theory. We have implemented BAT in the context of these theories. On the other hand, in the present study, in contrast to previous research and because of the use of new and varied neuropsychological perspectives in the field of depression disorder, we used the BIS/BAS questionnaire (that examines response to reward, reward seeking and drive) and BDI-II to collect data and evaluate results. We have tried to show that BAT not only helps reduce depression symptoms, but it can also increase the response rate to rewarding and enhancing stimuli by helping to modify the brain’s reward circuitry and behavioral brain systems and it can serve a natural antidepressant function.
Thus, the aim of this study is to investigate the BAT on the reward seeking behaviors in depressed people. Also, the population of this study is university students, because the emotional transition to university can be challenging for young adults, with depression being the most common health problem for university students. It has to be added that depression is a serious and important issue on college campuses across the country and the university students are susceptible to depression20 due to potential factors such as stress with school, work, or finances, or possibly feeling isolated after moving away from friends and family.
Materials and Methods
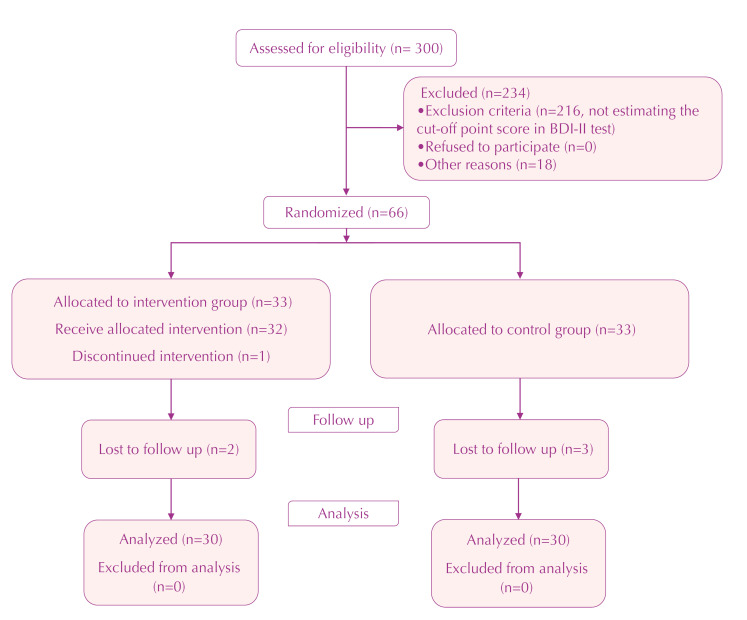
This is an experimental study with pretest-posttest and follow-up (5 weeks) and a control group. The research statistical population was University of Tabriz students in the academic year of 2018-2019 who were referred to the university counseling center. BDI-II was distributed among 300 students to determine the sample size. Of these 60 people were selected as the main sample for the intervention and control groups. In other words, the scale was used to determine the cut-off point (The cut-off point of this scale is 13) and diagnose the severity of depression. Based on the study objectives and the previous studies conducted on this issue, considering 95% confidence interval and 0.85 power, and by using power and sample size calculator software, a 60-subject sample size was selected for the study. Considering the attrition rate of 10 %, the sample size for each group was increased to 33 subjects (Figure 1). Individuals were randomly selected and assigned to the intervention group and the control group (demographic variables were used to randomly assign and match groups). The sampling method of this study was convenience sampling and the sample allocation to the groups was randomized and matched.
Figure 1.
Flow chart of the study.
The inclusion criteria were as the participants in the academic year of 2018-2019 were student in Tabriz University of Medical Sciences, who had referred to the counseling center. Absence in the treatment sessions, having other mental disorders and not estimating the cut-off point score in BDI-II test. were the criteria for exclusion. Also, all participants signed an informed consent form prior to the intervention, pre-test was given to participants and then the intervention was conducted (BAT) during the 8 sessions, 2 sessions per a week and 45 minutes per one session. Intervention sessions were conducted by a clinical psychologist with a PhD degree at the University of Tabriz Counseling Center at 11 AM. At the end of the intervention, a post-test was administered and 5 weeks later, a follow-up study was conducted. Also, the random assignment method was used to control the confounding variables and blinding was performed so that evaluator would not be aware of the intervention and control groups in the pre-test and post-test and the follow-up stages. At the end of this study, in order to observe ethical considerations, the intervention was performed on the control group. After expressing the research goals for the participants, their signed an informed consent form, and they were given assurances about the confidentiality of information and the right to participate in the research. Also, after the end of the research, the control group was also intervened to observe ethical considerations. Also, in order to data analysis, used the analysis of covariance (ANCOVA) and SPSS Ver.23.
Summary of BAT sessions21,22: 1&2; Familiarity and understanding of group members and communication between them (introduction); Familiarity with group rules and regulations (secrecy, regular attendance, etc.); Presenting the patterns of depression and behavioral activation. Homework: completing the sheet for daily activities. 3&4; Teaching skills functional analysis, breaking repetitive patterns of depression; Avoiding avoidance and strengthening effective coping strategies). Homework: using skills, completing a scale sheet of pleasure-achievement grading. 5&6; Explaining personal stressors and how they act as a trigger for depression; Discussing the avoidance and active coping strategies of people in coping with stress; Examining and preventing maladaptive coping methods such as oversleeping & smoking; Training new self-care skills to deal with depression. Homework: recording stressful situations during the week and how to apply self-care skills. 7&8; Discussing the social importance of coping with depression; Training assertive skills in order to be able to increase demand or saying no, asking for a better relationship and maintaining self-esteem; Preventing relapse; Reviewing techniques and exercises provided during the sessions & doing final summation; Making suggestions & criticisms & receiving feedback from group members; Implementing post-tests.
Beck Depression Inventory (BDI-II)
This scale is widely used as a self-reporting tool to measure depression-dependent cognitions. Items are graded from 0 to 3 according to the severity of the reported condition by the subject and are used to determine the cut-off point and to determine the severity of depression in this study. According to the Beck report, Cronbach’s alpha coefficient obtained was 0.92 for the outpatients and 0.93 for the students.23 The psychometric properties of this questionnaire in Iranian sample by Fata et al.,24 have been reported that the Cronbach’s alpha coefficient was 0.91, the correlation coefficient between the two halves was 0.89 and the test-retest coefficient was 0.97 for a week.
Behavioral Inhibition System & Behavioral Activation System Scale
In this study, the BIS & BAS Carver and White questionnaire was used to measure the reward seeking behavior patterns. It consists of 24 items that are scored by Likert scale. Of these 24 items, 7 items belong to the BIS scale and 13 items belong to the BAS scale. The BAS scale consists of three subcategories, drive, reward seeking, and a response to a reward, and 4 items are divergent items that are not graded. The internal consistency for the BIS subscale, 0.74 and internal consistency for the BAS subscales, a response to a reward, drive, and reward seeking were reported to be 0.73, 0.76 and 0.66, respectively, by Carver and White.25 In Iran, its reliability and validity have been obtained by Abdollahi Majarshin et al.26 According to their reports, the alpha coefficient for the BIS scale was 0.66 and for the BAS subscales, rewards, drive and reward seeking were 0.64, 0.70 and 0.61, respectively.26
Results
Sample size for each group (Intervention group & control group) was 33 but considering the attrition of 6 participants our data were analyzed with 30 participants each group. In this study we calculated demographic characteristics that included; age, sex, marital status, educational level and place of living. Total mean of age was 24.69 and 70 % of participants were female. Also 70 % of participants were single that has been shown in Table 1. Table 2 shows the mean and standard deviation of the variables in the intervention and control groups in the pretest, post-test and follow-up stages.
Table 1. Comparison of participants' distribution based on demographic variables .
| Variable |
Intervention group (n=30)
No. (%) |
Control group (n=30)
No. (%) |
Total
No. (%) |
P value b |
| Age a | 24.22 (13.60) | 25.16 (13.44) | 24.69 (13.08) | 0.14 |
| Sex | 0.19 | |||
| Male | 9 (29.7) | 9 (29.7) | 18 (30) | |
| Female | 21 (69.3) | 21(69.3) | 42 (70) | |
| Marital status | 0.13 | |||
| Single | 20 (66) | 22 (73.6) | 42 (70) | |
| Married | 3 (9.9) | 2 (6.6) | 5 (8) | |
| Divorced | 7 (23.1) | 6 (19.8) | 13 (22) | |
| Educational level | 0.16 | |||
| BA | 18 (59.4) | 19 (62.7) | 37 (62) | |
| MA | 8 (26.4) | 7 (24.1) | 15 (25) | |
| PhD | 4 (13.2) | 4 (13.2) | 8 (13) | |
| Place of living | 0.15 | |||
| Dormitory | 16 (53.8) | 17 (56.1) | 33 (55) | |
| Non-dormitory | 14 (46.2) | 13 (43.9) | 27 (45) |
aMean (SD) was reported. bChi-square test.
Table 2. The mean and standard deviation of scores related to BIS and BAS sub-scales .
| Group | Variable |
Pre-test
Mean (SD) |
Post-test
Mean (SD) |
Follow-up (5 weeks)
Mean (SD) |
| Intervention | BIS | 18.2(6.4) | 15.2(3.1) | 14.7(2.9) |
| Depression | 21.23(8.1) | 13.44(2.6) | 14.42(2.9) | |
| BAS | ||||
| Drive | 9.8(5.5) | 10.6(4.4) | 10.4(3.4) | |
| Reward-seeking | 8.1(3.1) | 14.9(2.1) | 13.9(3.1) | |
| Response to reward | 7.6(2.9) | 13.8(4.3) | 13.2(4.1) | |
| Control | BIS | 16.3(4.3) | 15.9(5.1) | 16.1(4.4) |
| Depression | 22.19(8.7) | 21.89(8.8) | 22.44(8.7) | |
| BAS | ||||
| Drive | 10.9(5.6) | 11.2(5.9) | 11.9(5.7) | |
| Reward seeking | 7.9(2.8) | 8.2(3.3) | 7.7(3.1) | |
| Response to reward | 8.2(3.3) | 6.9(2.5) | 7.4(3.5) |
Box test was used for homogenization of covariance matrices. Test results showed that the correlation of dependent variables in the studied groups was homogeneous, since F (0.78) calculated at (P >0.05) was not significant. To examine homogeneity of regression slopes results, the interaction table between the group and the pre-test scores were used. The results showed that F (BIS: 1.83, Drive: 1.06, Reward-seeking: 1.50, Response to reward: 2.32) calculated in any of the studied variables is not significant (P <0.05). Therefore, there is no interactivity between groups and pre-test scores, and as such the assumption of regression slope homogeneity is observed. Levene test was used to test the homogeneity of error variance. Test results showed that the error variance of the variables in the groups was homogeneous since the calculated F in the pre-test and post-test of BIS were (0.73, 0.98), the pre-test and the post-test of drive (0.15, 3.6), respectively, pre-test and post-test of reward seeking were (0.04, 0.09), and the pre-test and post-test of response to reward were (0.16, 304), so neither were not significant in P <0.05 level. Therefore, the variance of the variables in the studied groups is homogeneous.
The results of analysis covariance and the effect of group BAT on BIS and BAS subscales in the post-test and follow up phases are shown in Table 3.
Table 3. Results of the covariance analysis test .
| Scale | Stages | Variable index | df | F | P value | Effectiveness | Statistical power |
| BIS | Post-test | Pre-test | 1 | 25.1 | 0.01 | 0.50 | 0.997 |
| Intervention | 1 | 19.5 | 0.01 | 0.48 | 0.998 | ||
| Follow-up | Pre-test | 1 | 9.52 | 0.006 | 0.31 | 0.83 | |
| Intervention | 1 | 12.34 | 0.02 | 0.37 | 0.91 | ||
| BAS | |||||||
| Drive | Post-test | Pre-test | 1 | 7.5 | 0.08 | 0.15 | 0.388 |
| Intervention | 1 | 23.1 | 0.07 | 0.16 | 0.396 | ||
| Follow-up | Pre-test | 1 | 6.43 | 0.09 | 0.13 | 0.377 | |
| Intervention | 1 | 13.68 | 0.01 | 0.39 | 0.84 | ||
| BAS | |||||||
| Reward seeking | Post-test | Pre-test | 1 | 12.3 | 0.002 | 0.39 | 0.91 |
| Intervention | 1 | 19.3 | 0.01 | 0.48 | 0.98 | ||
| Follow-up | Pre-test | 1 | 3.15 | 0.09 | 0.13 | 0.39 | |
| Intervention | 1 | 13.6 | 0.002 | 0.38 | 0.93 | ||
| BAS | |||||||
| Response to reward | Post-test | Pre-test | 1 | 12.3 | 0.002 | 0.37 | 0.91 |
| Intervention | 1 | 19.3 | 0.01 | 0.48 | 0.90 | ||
| Follow-up | Pre-test | 1 | 3.15 | 0.09 | 0.13 | 0.39 | |
| Intervention | 1 | 13.6 | 0.002 | 0.38 | 0.93 |
The results of ANCOVA showed a significant increase in the two components of the BAS including; reward seeking (P <0.01) and response to reward (P <0.01) in the intervention group in the post-test and follow-up phase, which indicates an increase in positive affect and appetitive motivation for reward seeking and decreasing the risk for depression. Also, the results showed a significant decrease (P <0.01) in the BIS and depression in the intervention group in the post-test and follow-up stage, which indicates a decreasing in experience negative emotions (Table 3).
Discussion
The results of current study showed a significant increase in reward seeking and response to reward and a significant decrease in BIS and in depressed people. Valian et al.,22 showed that BAT has been effective in decreasing depression symptoms, because behavioral activation leads to reward seeking in the depressed people, which is concordant with our results. Karimpour et al.,8 also showed that reward tasks could increase affective levels (hedonic tone and energetic arousal) and decrease tense arousal (Neurotics experience) in depressed people, which is concordant with our results. Also, the study of Gawrysiak et al.,16 showed the BAT group in post test phase than the control group had a significantly reduction in symptoms of depression and increased environmental reward which is consistent with our results.
In contrast, Arias-Carrion and Poppel19 reported that depressed people might be less likely than non-depressed people to seek rewards, because they are less pleased with their rewards. Also, if the reduced motivation is completely related to anhedonia, then therapies such as CBT and BAT that are used as a positive reinforcement sources are not expected to be effective. But, the findings of Clark and Watson27 and our results show that CBT and BAT can be considered as a positive reinforcement source and are effective in reducing depression symptoms and improving reward seeking behaviors. This is so because it is assumed that the reward motivation system and its activity are associated with positive affective states. Because, based on the rules of conditioning theory, we should accept that stimulants that come before a reward have the capacity to activate the brain’s reward mechanism and the closer these stimulants are to the intrinsic stimulus of the reward the stronger the capacity gained will be. The reward mechanism works by maximizing these conditional or secondary reward stimuli through its connections with the motor system. Thus, in an environment where the sequence of stimulants flows in a particular order, the organism can be directed toward the stimulus of the reward. The reward seeking behavior and response to reward induce dopamine release in the reward circuitry and the mesolimbic dopamine pathway that this circuit points to pleasure, reinforcement, learning and reward seeking.28,29Therefore, taking rewards will produce pleasurable consequences, which will strengthen the tendency and activity for earning rewards and improve the reward seeking pattern.30,31 Also according to the Ferster14 model, depression is a chain of loss, reduction or lack of rewards and inability to obtain rewards. In behavioral models, depression is caused by a lack of access to reinforcements or a lack of dependence between individual behaviors and reinforcements.
Thus, BAT emphasizes the activation of predictable and rewarding response patterns to increase the relation between behavior and reward. As a result, this therapeutic approach encourages depressed patients to become more active in the face of fatigue and sadness, or to try to carry out behavioral homework related to the treatment process, and as a result, such a process, over time, will lead to increased environmental reinforcement and then, the improvement of the mood. Thus, it will lead to increasing the motivation in gaining rewards and improving the reward seeking pattern.32-34
It should be noted that in the current study, self-report tools have been used to collect data that may make the accuracy of the information difficult to establish. Thus, it is suggested that in future research the existing tools in cognitive neuroscience be used. Also, the short time of the follow-up phase is another limitation of this study, and it is thus suggested that in the future studies more time should be allotted to the follow-up stage.
Conclusion
The results of this study showed a significant increase in reward seeking and response to reward and a significant decrease in BIS and depression symptoms in depressed people. Also, the results of this study showed that BAT is effective in improving the rewards seeking behaviors in depressed people since this treatment will increase the positive reinforcement and the gaining reward from the patient. BAT facilitates the achievement of positive reinforcement which can be effective in improving the pattern of reward seeking behavior in depressed people.
Acknowledgment
We are grateful to all participants who helped us with this research. In this research, the budget was provided by Social Determinants of Health Research Center affiliated to Tabriz University of Medical Sciences, Tabriz, Iran.
Ethical Issues
The study was approved by the regional ethics committee under the code number of IR. TBZMED. REC. 1397. 1520. Project No: Mhrc.97.404.
Conflict of Interest
The authors declare no conflict of interest in this study.
Authors’ Contributions
AKV & KH: designed the study, collected the data, performed analysis and wrote the first draft; ABR: supervision; AKV, AR and LKH: study advisors and all authors read and approved the final revision of the manuscript.
Research Highlights
What is the current knowledge?
Theorists have proposed that depression is associated with abnormalities in the BAS and BIS. However, none study not examined the effect of behavioral activation on reward seeking behaviors.
What is new here?
BAT increased the response to reward and reward seeking in depressed people because consumption of rewards produces hedonic consequences and lead to learning cues that predict possible rewards in environments.
BAT decreased the negative emotions in depressed people because the negative affect reduces in rewarding situations.
References
- 1.Yim IS, Stapleton LRT, Guardino CM, Hahn-Holbrook J, Schetter CD. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu Rev Clin Psychol. 2015;11:99–137. doi: 10.1146/annurev-clinpsy-101414-020426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blum K, Baron D, McLaughlin T, Gold MS. Molecular neurological correlates of endorphinergic/dopaminergic mechanisms in reward circuitry linked to endorphinergic deficiency syndrome (EDS) Journal of the Neurological Sciences. 2020;15(411):116733. doi: 10.1016/j.jns.2020.116733. [DOI] [PubMed] [Google Scholar]
- 3.Blum K, Oscar-Berman M, Stuller E, Miller D, Giordano J, Morse S. et al. Neurogenetics and nutrigenomics of neuro-nutrient therapy for reward deficiency syndrome (RDS): clinical ramifications as a function of molecular neurobiological mechanisms. J Addict Res Ther. 2012;3(5):139. doi: 10.4172/2155-6105.1000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aliloo M, Hashemi Nosratabad T, Karimpour Vazifehkhorani AR. The role of impulsivity, sensitivity to reward and anhedonia in distinction people with symptoms of borderline personality disorder from ordinary people. Iranian Journal of Psychiatry and Clinical Psychology. 2018;24(2):136–47. [Persian] [Google Scholar]
- 5.Blum K, Thanos PK, Gold MS. Dopamine and glucose, obesity, and reward deficiency syndrome. Frontiers in psychology. 2014;5:919. doi: 10.3389/fpsyg.2014.00919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilley ED. Reward deficiency syndrome solution focused brief therapy to begin integrating the sciences of addiction & reward deficiency syndrome (RDS) J Reward Defic Syndr Addict Sci. 2019;5(1):1–6. doi: 10.17756/jrdsas.2019-042. [DOI] [Google Scholar]
- 7.Sherdell L, Waugh CE, Gotlib IH. Anticipatory pleasure predicts motivation for reward in major depression. J Abnorm Psychol. 2012;121(1):51–60. doi: 10.1037/a0024945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karimpour Vazifehkhorani A, Bakhshipour Roodsari A, Kamali Ghasemabadi H, Etemadi Chardah N. Effectiveness of reward-based task on affective levels of depressed individuals. Iranian Journal of Psychiatry and Clinical Psychology. 2018;24(1):6–15. [Persian] [Google Scholar]
- 9.Dickson JM, Moberly NJ, Kinderman P. Depressed people are not less motivated by personal goals but are more pessimistic about attaining them. J Abnorm Psychol. 2011;120(4):975–80. doi: 10.1037/a0023665. [DOI] [PubMed] [Google Scholar]
- 10.Zacharopoulos G, Lancaster T, Bracht T, Ihssen N, Maio GR, Linden DE. A hedonism hub in the human brain. Cerebral Cortex. 2016;26(10):3921–7. doi: 10.1093/cercor/bhw197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hyman SE, Malenka RC, Nestler EJ. Neural mechanisms of addiction: the role of reward-related learning and memory. Annu Rev Neurosci. 2006;29:565–98. doi: 10.1146/annurev.neuro.29.051605.113009. [DOI] [PubMed] [Google Scholar]
- 12.Davidson RJ. Affective style, psychopathology, and resilience: brain mechanisms and plasticity. Am Psychol. 2000;55(11):1196–214. doi: 10.1037//0003-066x.55.11.1196. [DOI] [PubMed] [Google Scholar]
- 13.McFarland BR, Shankman SA, Tenke CE, Bruder GE, Klein DN. Behavioral activation system deficits predict the six-month course of depression. J Affect Disord. 2006;91(2-3):229–34. doi: 10.1016/j.jad.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 14.Ferster CB. A functional anlysis of depression. Am Psychol. 1973;28(10):857–70. doi: 10.1037/h0035605. [DOI] [PubMed] [Google Scholar]
- 15.Cuijpers P, Van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clin Psychol Rev. 2007;27(3):318–26. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Gawrysiak M, Nicholas C, Hopko DR. Behavioral activation for moderately depressed university students: Randomized controlled trial. Journal of Counseling Psychology. 2009;56(3):468–75. doi: 10.1037/a0016383. [DOI] [Google Scholar]
- 17.Zemestani M, Davoodi I, Mehrabi-Zadeh Honarmand M, Zargar Y. Effectiveness of group behavioral activation on depression, anxiety and rumination in patients with depression and anxiety. Journal of Clinical Psychology. 2014;5(4):73–84. [Persian] [Google Scholar]
- 18.Takagaki K, Okamoto Y, Jinnin R, Mori A, Nishiyama Y, Yamamura T. et al. Behavioral activation for late adolescents with subthreshold depression: a randomized controlled trial. Eur Child Adolesc Psychiatry. 2016;25(11):1171–82. doi: 10.1007/s00787-016-0842-5. [DOI] [PubMed] [Google Scholar]
- 19.Arias-Carrion O, Poppel E. Dopamine, learning, and reward-seeking behavior. Acta Neurobiol Exp. 2007;67(4):481–8. doi: 10.55782/ane-2007-1664. [DOI] [PubMed] [Google Scholar]
- 20.Bombardier CH, Cunniffe M, Wadhwani R, Gibbons LE, Blake KD, Kraft GH. The efficacy of telephone counseling for health promotion in people with multiple sclerosis: a randomized controlled trial. Arch Phys Med Rehabil. 2008;89(10):1849–56. doi: 10.1016/j.apmr.2008.03.021. [DOI] [PubMed] [Google Scholar]
- 21.Newman CF. Competency in conducting cognitive–behavioral therapy: Foundational, functional, and supervisory aspects. Psychotherapy: Theory, Research, Practice, Training. 2010;47(1):12–9. doi: 10.1037/a0018849. [DOI] [PubMed] [Google Scholar]
- 22.Valian AM, Sudani M, Sharalinia K, Khojasteh Mehr R. The Effectiveness of behavioral activation therapy on depression symptoms and cognitive-behavioral avoidance for students. Quarterly Journal of Social Work. 2016;5(4):25–31. [Persian] [Google Scholar]
- 23.Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of beck depression inventories-ia and-ii in psychiatric outpatients. J Pers Assess. 1996;67(3):588–97. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 24.Fata L, Birashk B, Atefvahid MK, Dabson KS. Meaning assignment structures/schema, emotional states and cognitive processing of emotional information: comparing two conceptual frameworks. Iranian Journal of Psychiatry and Clinical Psychology. 2005;11(3):312–26. [Persian] [Google Scholar]
- 25.Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. Journal of personality and social psychology. 1994;67(2):319–33. doi: 10.1037/0022-3514.67.2.319. [DOI] [Google Scholar]
- 26.Abdollahi Majareshin R, Bakhshipour A, Mahmoud Alilou M. The relationship between personality traits of behavioural inhibition/ activation systems and conceptual implicit memory bias based on the Transfer Appropriate Processing (TAP) framework. Quarterly Journal of Psychological Studies. 2010;6(1):57–88. [Persian] [Google Scholar]
- 27.Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100(3):316–36. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- 28.Corr PJ. Reinforcement sensitivity theory and personality. Neurosci Biobehav Rev. 2004;28(3):317–32. doi: 10.1016/j.neubiorev.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Bilbao A, Neuhofer D, Sepers M, Wei SP, Eisenhardt M, Hertle S. et al. Endocannabinoid LTD in accumbal D1 neurons mediates reward-seeking behavior. Iscience. 2020;23(3):100951. doi: 10.1016/j.isci.2020.100951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cuijpers P, van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol. 2008;76(6):909–22. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- 31.Yang Z, Oathes DJ, Linn KA, Bruce SE, Satterthwaite TD, Cook PA. et al. Cognitive behavioral therapy is associated with enhanced cognitive control network activity in major depression and posttraumatic stress disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2018;3(4):311–9. doi: 10.1016/j.bpsc.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alexopoulos GS, Raue PJ, Gunning F, Kiosses DN, Kanellopoulos D, Pollari C. et al. “Engage” therapy: behavioral activation and improvement of late-life major depression. Am J Geriatr Psychiatry. 2016;24(4):320–26. doi: 10.1016/j.jagp.2015.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dunlop K, Rizvi SJ, Kennedy SH, Hassel S, Strother SC, Harris JK. et al. Clinical, behavioral, and neural measures of reward processing correlate with escitalopram response in depression: a Canadian Biomarker Integration Network in Depression (CAN-BIND-1) Report. Neuropsychopharmacology. 2020;45(8):1390–7. doi: 10.1038/s41386-020-0688-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dubey I, Georgescu AL, Hommelsen M, Vogeley K, Ropar D, Hamilton AF. Distinct neural correlates of social and object reward seeking motivation. EJN. 2020;26(12):1–16. doi: 10.1111/ejn.14888. [DOI] [PubMed] [Google Scholar]