Abstract
Introduction: Glycaemic status of the patient is often monitored using capillary blood glucose test which is fairly accurate. Traditional finger stick sampling is done to obtain sample, which can be painful and may be a barrier for repeated testing. The current study was conducted to compare fingertip and palm site sampling on pain perception, and variation in capillary blood glucose level.
Methods: This study was conducted among 284 diabetic patients, who were selected by convenience sampling method. The data was collected by measuring capillary blood glucose levels from fingertip and palm site of the left hand at an interval of 10 minutes using a standard glucometer. The level of pain perceptions was measured with a numerical rating pain scale. Data analysis was accomplished using descriptive analysis, Mann-Whitney U test and Kruskal- Wallis test.
Results: The level of pain perception at the palm site (2) was lesser than fingertip (3) which was significant at P < 0.001. 223 (78.52%) of the participants experienced more pain at fingertip than palm site, the difference in the measured capillary blood glucose level between fingertip [mean (SD): 226.65 (87.86)] and palm site [mean (SD): 225.65(92.13)] was minimum. The agreement of palm site was 90.7% in single measurement and 95.1% in average measurement.
Conclusion: The present study concludes that, majority of the participants experienced less pain perception at the palm site sampling (alternate site sampling) than fingertip sampling with very minimal variation in the blood glucose level.
Keywords: Blood glucose self-monitoring, Pain, Blood glucose, Diabetes mellitus
Introduction
Diabetes mellitus is a group of metabolic diseases characterized by chronic hyperglycemia produced by defective insulin secretion from the pancreas, defects in the insulin action, or both. Diabetes is growing at an alarming rate in India.1,2 According to International Diabetes Federation, globally 352 million people suffer from impaired glucose tolerance and India had 77 million people with diabetes. Ageing populations, dietary changes, increasing urbanization and reduced physical activity are the common reasons for increasing burden. The chronic hyperglycemia of diabetes is associated with long-term target organ damages, dysfunction, and failure of multiple organs, especially the kidneys, eyes, heart, nerves, and blood vessels.3,4
Capillary blood glucose monitoring gives the average blood glucose value in routine hospital care of diabetic patients and quick assessment of blood sugar in emergency cases and self- home monitoring which helps in regulation of diet and identification of dangerous blood sugar levels and related emergencies.5
Traditionally the samples for capillary blood sugar monitoring have been obtained from fingers by using needles and lancets to puncture their fingertip.6 but this can be a painful procedure and may be a barrier to repeated testing. In the last several years, it is been possible to obtain samples from other skin sites other than fingertips such as palm, forearm, abdomen, thigh etc. using a lancing device. These areas are less vascular and also less densely innervated with pain receptors than the fingertips.7 As it is less painful, alternate site sampling also improves the patients’ adherence to the self-monitoring of blood glucose. Inadequate knowledge regarding this method makes it less popular and not been practiced at clinical setup and during self-monitoring of blood glucose.8,9
Although testing at alternate body sites has many advantages (e.g., less pain, sparing of fingertips), acceptance of the alternate site testing ultimately depends on how accurately glucose levels of alternate sites reflect one’s glycemic state. Several recent publications have spoken this issue, but questions on glucose equivalence still remain. Most of the health care professionals and patients are not introduced to alternate site which is relatively less painful, easy to collect the adequate volume of sample, easy to control the bleeding. Compared to fingertip with alternate sites, fingertips are more interfering area when working.10,11
If we use alternate site sampling using a lancing device will reduce level of pain, provide adequate volume of sample, easy to control the bleeding and these sites will not interfere with the normal daily activities of the patients.12 Though the alternative site sampling reduces pain perception, its impact on estimated difference in blood glucose level in published studies is inconclusive.3,8,11,12 Further establishing data on this would help to reduce the cumulative discomfort from multiple finger sticks. Hence this study was conducted to assess the level of pain perception, and Blood glucose variability in both fingertip and palm site sampling.
Materials and Methods
Single group of study subjects, with two time measurement of capillary blood glucose at different sites at 10 minutes interval at random sequence, was participated. This study was conducted with the objective to compare the level of pain perception in fingertip vs palm site in capillary blood glucose sampling (Figures 1 and 2) and to assess the variation in capillary blood glucose level at both sites. The study was conducted in diabetic clinic of a tertiary care center under government of India during August 2019 to February 2020. As palm of the hand has shown to be more accurate and less painful in previous studies, palm site has chosen for this study.
Figure 1.
Fingertip.
Figure 2.
Palm site sampling.
The capillary blood glucose level is used as a parameter for calculating sample size based the pilot study finding using paired t test with the mean and standard deviation of fingertip vs palm site as 244.8 (65.86) and 238.2 (78.4) with a maximum allowed difference 12 and with a level of significance of 0.05 and power of 0.80 we require 284 participants for this study(since the sample size calculated based on the pain perception difference was minimal, the sample size calculated based on capillary blood glucose level was adopted).
Patients diagnosed with diabetes mellitus who are aged ≥18 years, attending diabetes clinic of a tertiary care center were included in the study. Patient with any wound or altered skin integrity in hands, patients with peripheral neuropathy were excluded from the study. Consecutive participants, who attended diabetic clinic and met the inclusion criteria were recruited into the study by convenience sampling method by the principal investigator.
The participant data sheet consists of first part which included Socio demographic profile section, and second part of which included clinical data section with the details on participants height, weight, body mass index (BMI), hemoglobin (Hb)level, glycosylated hemoglobin level (HbA1C), and blood glucose level from fingertip and palm site, type of diabetes mellitus, duration of diabetes mellitus, medication details, practice of self-monitoring of blood sugar at home and its frequency, presence of co-morbidities. The third part contains, intensity of pain measured using a numerical pain scale from fingertip sampling and palm site sampling. The numerical pain rating scale (NPRS) is a unidimensional estimation of pain intensity in adults. The scale is a segmented numeric type of the visual analogue scale (VAS) in which a respondent selects a whole number (0–10 integers) that best reflects the intensity of his/her pain. The used format is a horizontal line anchored by terms describing pain severity extremes like mild pain (0-3), moderate pain (4-6), and severe pain (7-10).
The investigator self-introduced to the study participants and rapport was established. The purpose of the study was explained to them and assurance was given to participants regarding the strict confidentiality of the information gathered. After obtaining the written informed consent from the participants, the investigator collected data through the self-structured data collection perform. After obtaining data on clinical and socio demographic parameters, the patients’ left hand was washed with lukewarm water and dried thoroughly for capillary blood glucose sampling. The sample was obtained by the Principal Investigator with the help of a lancing device, from fingertip and palm site at a 10 minutes interval and capillary blood glucose using standardized, calibrated Control D glucometer. The random sequence method was adopted to get sample either from fingertip or palm site first. The palm site was massaged for 10 seconds to improve the blood circulation before taking the sample from the palm site. Blood glucose at both the sites was recorded and difference was noted. With the help of the numerical rating scale, pain perception was assessed for both the site sampling of capillary blood glucose.
Content validity of the participant data sheet was established with medical and nursing experts, and consensus on the measurement parameters was established with content validity index of 0.8. About the numerical rating scale for pain measurement, its Test–retest reliability has been shown to be good, but higher among literate (r= 0.94, P =0.001) than illiterate patients (r = 0.71, P =0.001). In the absence of a gold standard for pain, criterion validity cannot be evaluated. For construct validity, numeric rating scale has shown co-relation (with response options from “no pain” to “unbearable pain”), as 0.62–0.91.
Results
Among 284 participants, 49.6% of the patients were between the age group of 40–60 years. About 54.9% of the patients were males. About 77.1% of the patients’ educational qualification was ≤10th standard or secondary school leaving certificate (SSLC). About 47.5% of the patients belong to the occupational group of clerical/shop/agriculture and 39.4% of the patients were unemployed. Forty-four percent of the patients were overweighed and 6% were obese. About 97.2% of the patients were diagnosed with type II diabetes, 48.6% of them were having diabetes mellitus for more than 5 years and 57.75 % of them were getting oral hypoglycemic agents only (Table 1).
Table 1. Frequency distribution of socio-demographic and clinical data (N=284) .
| Variable | Group | No. (%) |
| Age (years) | <40 | 15 (5.3) |
| 40-60 | 141 (49.6) | |
| >60 | 128 (45.1) | |
| Gender | Male | 156 (54.9) |
| Female | 128 (45.1) | |
| Education | ≤SSLC | 219 (77.1) |
| PUC/Diploma | 43 (15.1) | |
| Graduate | 19 (6.7) | |
| Post graduate | 3 (1.1) | |
| BMI | Under weighed | 8 (2.8) |
| Normal | 134 (47.2) | |
| Over weighed | 125 (44.0) | |
| Obese | 17 (6.0) | |
| Type of DM | Type I | 8 (2.8) |
| Type II | 276 (97.2) | |
| Duration of DM | <5 years | 84 (29.6) |
| 5-15 years | 138 (48.6) | |
| >15 years | 62 (21.8) | |
| Use of insulin (with insulin syringe) | No | 165 (58.1) |
| Yes | 119 (41.9) | |
| Practice of self-monitoring of blood glucose at home |
No | 271 (95.4) |
| Yes | 13 (4.6) | |
| Use of medication | Oral Hypoglycemic agents (OHA) | 164 (57.75) |
| Insulin | 29 (10.21) | |
| OHA + Insulin | 91 (32.04) | |
| Use of oral hypoglycaemic agent | Metformin | 164 (64.31) |
| Metformin + Glimepiride | 81 (31.77) | |
| Metformin + Glibenclamide | 10 (3.92) | |
| Use of insulin | Human actrapid | 12 (9.92) |
| Human mixtard | 85 (70.25) | |
| NPH | 15 (12.4) | |
| Human actrapid + Human mixtard | 5 (4.13) | |
| Human actrapid+ NPH | 3 (2.48) | |
| Human mixtard+ NPH | 1 (0.82) | |
| Presence of comorbidities | Chronic inflammatory demyelinating polyneuropathy | 1(0.73) |
| Hypertension | 72 (52.17) | |
| Hypertension + CAD (coronary artery disease) | 3 (2.17) | |
| Hypertension + Hypercholesterolemia | 52 (37.68) | |
| Hyperthyroidism | 1 (0.73) | |
| Hypertension + Hyperthyroidism | 2 (1.45) | |
| Hypercholesterolemia | 1 (0.73) | |
| Hypertension + Hypercholesterolemia + CAD | 6 (4.34) | |
| Complications | Transient ischemic attack | 1(6.25) |
| Stroke | 4(25) | |
| Diabetic foot | 4(25) | |
| Gestational Diabetes Mellitus | 4(25) | |
| Acute renal failure | 1(6.25) | |
| Chronic kidney disease | 2(12.5) | |
| Hemoglobin level a | 12.87(1.02) | |
| HbA1C level a | 11.56(6.55) | |
a Mean (SD) was reported
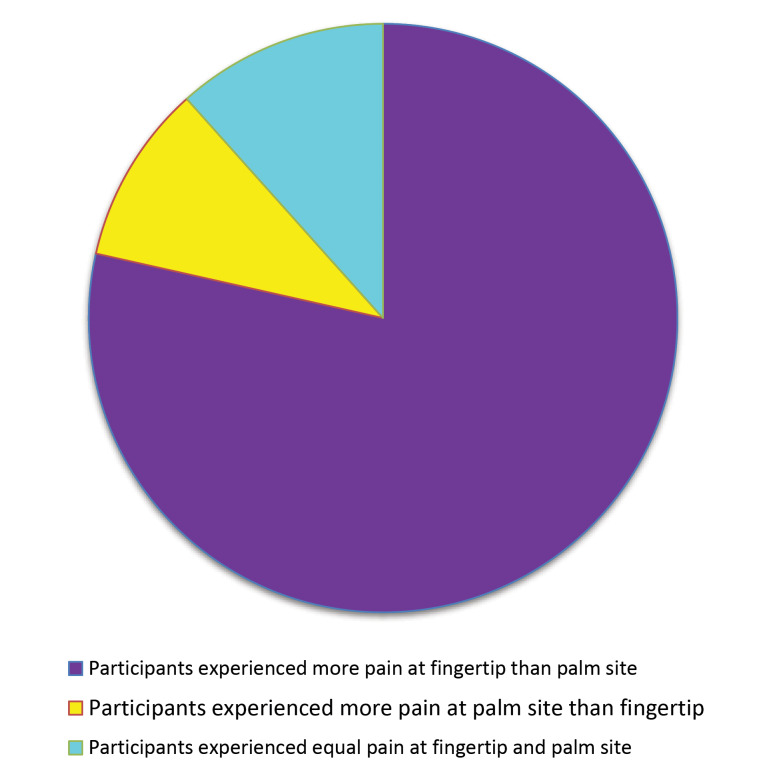
The level of pain experienced by the participants at the palm site (median=2) was lesser than that of fingertip (median=3), which was highly significant at P <0.001 (Table 2). When we compared the pain perception at fingertip and palm, 78.52% of participants experienced more pain at fingertip than palm site. About 28 (9.86%) of the participants experienced more pain at palm site than fingertip and 33 (11.62%) of the participants experienced equal score of pain at fingertip and palm site (Figure 3). Among 13 participants, who were practicing self-monitoring of blood glucose at home, experienced the pain score of 3 (minimum value-2, maximum value-7) at the fingertip compared to pain score of 2 (minimum value-0, maximum value-4) when it was checked at palm site which was statistically significant at P <0.05.
Table 2. Comparison of pain level at fingertip and Palm site(N=284) .
| Pain score | Fingertip | Palm site | P value a |
| Median | 3 | 2 | 0.001* |
| Minimum value | 0 | 0 | |
| Maximum value | 8 | 8 |
a Wilcoxon signed rank test, *Statistically significant
Figure 3.
Distribution pain perception among participants.
The capillary blood sugar level of fingertip and palm site was 226.08 (87.86) and 225.65 (92.13) respectively. The difference was 0.43 (P <0.08) and non-significant. The intra-class correlation shows that the agreement between fingertip and palm site was 90.7% in a single measurement and 95.1% in average measurement (Table 3).
Table 3. Intra-class correlation of the blood glucose level at fingertip and palm site (N=284) .
| Site | Mean (SD) | Intra class correlation | Lower bound | Upper bound | P value a | |
| Fingertip | 226.08(87.86) | Single measure | 0.90 | 0.88 | 0.92 | 0.001 |
| Palm site | 225.65(92.13) | Average measure | 0.95 | 0.83 | 0.96 | 0.001 |
a Intra class correlation.
The correlation between pain perception at fingertip and duration of diabetes mellitus is negative (r = -0.197) which was statistically significant at P <0.05. The patients experienced less pain level at fingertip when the duration of the diabetes mellitus increases. There is a negative correlation between the pain perceptions at palm site with the duration of diabetes mellitus but it is not statistically significant. Overall there is a reduction in the pain perception at both the sites (Table 4).
Table 4. Correlation of the level of pain perception at fingertip and palm site with respect to duration of diabetes mellitus (N=284) .
| Variable | Pain score | |
| Fingertip | Palm site | |
| Duration of diabetes | r= -0.19a P =0.02* |
r=-0.09a P =0.25 |
aSpearman rank correlation, *Statistically significant.
Discussion
The current study showed that the median value of the level of pain perception at the palm site was lesser than fingertip which was statistically significant at P <0.001. Similar findings were reported by Fineberg et al.,12 showed that 60% of the patients reported that alternate site testing was less painful. The similar reports have been reported in other study also. Pain related with finger piercing is one of the main barriers for daily monitoring of blood glucose, further, it has been discussed that skin pricking at alternate sites which has less nerve endings other than fingertip may increase blood glucose monitoring compliance at home.13
Although testing at alternate body sites has benefits including sparing of fingertips and lesser pain, its full acceptance eventually rest on how precise the blood glucose levels at alternate sites which reflect one’s glycemic state. If a patient does not have reliance in the test, the patient may re do the testing at fingertip thereby refuting any advantage of palm site testing.14
The present study found that, the difference in the capillary blood sugar level between fingertip [mean (SD): 226.08 (87.86)] and palm site [mean (SD): 225.65 (92.13)] was minimum when it was checked at random sequence. The intra-class correlation showed that the agreement between fingertip and palm site was 90.7% in a single measurement and 95.1% in average measurement. A similar result was reported by Jungheim and Koschinsky15 that, the difference in the blood glucose levels between fingertip sampling and alternate sampling was minimal [(7.8 (2.4) vs. 7.2 (2.3) mmol/L, respectively P = 0.06)].15 In contrast, to present study, Lee et al., reported that, that patients who test during first one hour time period after taking food could expect to have significant differences between their alternate site and finger glucose measurements.11 Ellison et al., reported that the accuracy of immediate postprandial changes in the blood glucose level is difficult to measure at the alternate sites.16
Testing on the forearm and thigh has been shown to be adequately accurate in pre meal and steady state levels only.Palm testing, unlike forearm and thigh testing, has been shown to be an accurate substitute for fingertip testing in evaluating blood glucose values at all times (including pre-meal, post-meal, and postexercise).17
The use of alternate site (palm site) sampling of capillary blood glucose monitoring is also effective method as fingertip sampling. Patients can utilize this method for the routine self- monitoring of capillary blood glucose levels at home and prevent complications like hyperglycemia or hypoglycaemia.10 Patients will experience less pain perception at the palm site with minimal variation in the capillary blood glucose level. This can be minimized by washing the hand with lukewarm water and gently massage over the palm before sampling.
The current study noted that there is no significant association between the pain perception at fingertip and palm site with regards to the age, gender, BMI, type of diabetes, or usage of the medication (administration of insulin subcutaneously with insulin syringe). So this method can be effectively practiced in any diabetic patients with regardless of the use of insulin. The similar results have been obtained in a study by Farmer et al., found that pain rating was significantly lower with palm site (1.65) than with the standard site (2.83) (P <0.001). There was no significant difference in mean glucose measurements between standard care (150 mg/dL) and palm site (149 mg/dL). The numbers were closely correlated (r = 0.98).18
Among the occupational groups, the participants belong to the unskilled worker experienced less pain at palm site (the median pain scores were 1 and 1.5 respectively which was statistically significant at P <0.05) than the fingertip. Similarly, Khawaja et al., specified that, compared to patients who were physically active, patients with not regular physical activity were less likely to have diabetic peripheral neuropathy, hence patients with less physical activity will experience more pain perception than patients with more physical activity.2 However in this study we have not studied about this aspect.
The current study showed that 13 out of 284 patients were practicing self-monitoring of blood glucose at home. Participants experienced the pain score of 3 at the fingertip and experienced less pain score of 2 at palm site which was significant at P <0.05. Monitoring of capillary blood sugar level at palm site among participants who were self-monitoring blood glucose level experienced less pain at palm site than fingertip sampling, which a similar result was reported by Ito et al.,19 and Cristiano et al.20 Sampling was less painful and were desired to continue alternate site sampling at home.19-21
The correlation between pain perception at fingertip and duration of diabetes mellitus is negative (r = -0.19) in this study, which was statistically significant at P <0.05. The patients experienced less pain level at fingertip when the duration of the diabetes mellitus increases more than 15 years. There was a negative correlation between the pain perceptions at palm site with the duration of diabetes mellitus but it is not statistically significant. Overall there was a reduction in the pain perception at both the site, Similarly other studies found, a lower prevalence of polyneuropathy in those with duration of DM < 5 years and highest in those with a duration of DM > 15 years.22-24 Hence the level of pain perception will reduce in diabetic patients when the duration of diabetes is more than 15 years.
As this study is one group, there is a possibility of altered pain perception, however randomization of sampling sequence and adequate interval between the sampling has been considered to minimize the carry over effect.
Conclusion
The current study supports the use of palm site (alternate site) sampling for the self-monitoring of capillary blood glucose level at home and for routine clinical practice which is less painful than traditional fingertip sampling and without variation in blood glucose level. Further, palm site sampling would help the patient to adhere to routine monitoring of glucose as they perceive less pain than fingertip.
Acknowledgement
Authors thank all the staff of Diabetic Clinic of study institute and participants in this study.
Ethical Issues
After approval from Institute Research Monitoring committee, permission was obtained from the Institute Ethical Committee, Human studies (Reg. No: JIP/IEC/2019/0020). Ethical issues involved in the study were a minor increase over minimal risk or low. Informed consent was obtained from every participant after a brief explanation regarding the study by the investigator. Confidentiality of the data, the right to withdraw from the study, and the anonymity of the subjects were explained before data collection. Good clinical practice guidelines of ICMR were followed.
Conflict of Interest
The authors declare no conflict of interest in this study.
Authors’ Contributions
AAP: Conceived and designed the study, Data collection, Manuscript preparation; LR: Conceived and designed the study, Data analysis, Interpretation, Manuscript preparation, Manuscript review; SBS: Designed the study, Data analysis, Interpretation, Manuscript review; RM: Data analysis, Manuscript review; KMJ: Designed the study, Manuscript review.
Research Highlights
What is the current knowledge?
Although blood sampling for capillary blood glucose monitoring is usually practiced from the fingertip as it reflects the accurate changes in capillary blood glucose levels, due to increased nerve endings in fingertip which may causes painful experience that often leads to poor adherence to regular monitoring of blood glucose at home among diabetic patients.
What is new here?
This study identified that palm site can be used as alternative site for capillary blood glucose sampling as it is less painful without significant variability in capillary blood glucose level.
References
- 1.Tabish A. Lifestyle diseases: consequences, characteristics, causes and control. J Cardiol Curr Res. 2017;9(3):326. doi: 10.15406/jccr.2017.09.00326. [DOI] [Google Scholar]
- 2.Khawaja N, Abu-Shennar J, Saleh M, Dahbour SS, Khader YS, Ajlouni KM. The prevalence and risk factors of peripheral neuropathy among patients with type 2 diabetes mellitus; the case of Jordan. Diabetol Metab Syndr. 2018;10:8. doi: 10.1186/s13098-018-0309-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bina DM, Anderson RL, Johnson ML, Bergenstal RM, Kendall DM. Clinical impact of prandial state, exercise, and site preparation on the equivalence of alternative-site blood glucose testing. Diabetes Care. 2003;26(4):981–5. doi: 10.2337/diacare.26.4.981. [DOI] [PubMed] [Google Scholar]
- 5.Aqtam I, Darawwad M. Health promotion model: an integrative literature review. Open J Nurs. 2018;8(7):485–503. doi: 10.4236/ojn.2018.87037. [DOI] [Google Scholar]
- 6.Greenhalgh S, Bradshaw S, Hall CM, Price DA. Forearm blood glucose testing in diabetes mellitus. Arch Dis Child. 2004;89(6):516–8. doi: 10.1136/adc.2002.019307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cunningham DD, Henning TP, Shain EB, Young DF, Hannig J, Barua E. et al. Blood extraction from lancet wounds using vacuum combined with skin stretching. J Appl Physiol (1985) 2002;92(3):1089–96. doi: 10.1152/japplphysiol.00798.2001. [DOI] [PubMed] [Google Scholar]
- 8.Nakayama T, Kudo H, Sakamoto S, Tanaka A, Mano Y. Painless self-monitoring of blood glucose at finger sites. Exp Clin Endocrinol Diabetes. 2008;116(4):193–7. doi: 10.1055/s-2007-993146. [DOI] [PubMed] [Google Scholar]
- 9.Jacoby JM. An analysis of alternate site tests to improve patient compliance with self-monitoring of blood glucose. J Diabetes Sci Technol. 2010;4(4):911–2. doi: 10.1177/193229681000400421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfützner A, Schipper C, Ramljak S, Flacke F, Sieber J, Forst T. et al. Evaluation of the effects of insufficient blood volume samples on the performance of blood glucose self-test meters. J Diabetes Sci Technol. 2013;7(6):1522–9. doi: 10.1177/193229681300700612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DM, Weinert SE, Miller EE. A study of forearm versus finger stick glucose monitoring. Diabetes Technol Ther. 2002;4(1):13–23; discussion 45. doi: 10.1089/15209150252924049. [DOI] [PubMed] [Google Scholar]
- 12.Fineberg SE, Bergenstal RM, Bernstein RM, Laffel LM, Schwartz SL. Use of an automated device for alternative site blood glucose monitoring. Diabetes Care. 2001;24(7):1217–20. doi: 10.2337/diacare.24.7.1217. [DOI] [PubMed] [Google Scholar]
- 13.Knapp PE, Showers KM, Phipps JC, Speckman JL, Sternthal E, Freund KM. et al. Self-monitoring of blood glucose with finger tip versus alternative site sampling: effect on glycemic control in insulin-using patients with type 2 diabetes. Diabetes Technol Ther. 2009;11(4):219–25. doi: 10.1089/dia.2008.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kempe KC, Budd D, Stern M, Ellison JM, Saari LA, Adiletto CA. et al. Palm glucose readings compared with fingertip readings under steady and dynamic glycemic conditions, using the OneTouch Ultra Blood Glucose Monitoring System. Diabetes Technol Ther. 2005;7(6):916–26. doi: 10.1089/dia.2005.7.916. [DOI] [PubMed] [Google Scholar]
- 15.Jungheim K, Koschinsky T. Glucose monitoring at the arm: risky delays of hypoglycemia and hyperglycemia detection. Diabetes Care. 2002;25(6):956–60. doi: 10.2337/diacare.25.6.956. [DOI] [PubMed] [Google Scholar]
- 16.Ellison JM, Stegmann JM, Colner SL, Michael RH, Sharma MK, Ervin KR. et al. Rapid changes in postprandial blood glucose produce concentration differences at finger, forearm, and thigh sampling sites. Diabetes Care. 2002;25(6):961–4. doi: 10.2337/diacare.25.6.961. [DOI] [PubMed] [Google Scholar]
- 17.Fedele D, Corsi A, Noacco C, Prisco F, Squatrito S, Torre E. et al. Alternative site blood glucose testing: a multicenter study. Diabetes Technol Ther. 2003;5(6):983–9. doi: 10.1089/152091503322641033. [DOI] [PubMed] [Google Scholar]
- 18.Farmer L, Winfield C, Quatrara B, Letzkus L, Schenck P, Finneran P. et al. Does site matter? comparing accuracy and patient comfort of blood glucose samples taken from the finger and palm of the perioperative patient. J Perianesth Nurs. 2017;32(6):573–7. doi: 10.1016/j.jopan.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 19.Ito T, Kamoi K, Minagawa S, Kimura K, Kobayashi A. Patient perceptions of different lancing sites for self-monitoring of blood glucose: a comparison of fingertip site with palm site using the OneTouch Ultra Blood Glucose Monitoring System. J Diabetes Sci Technol. 2010;4(4):906–10. doi: 10.1177/193229681000400420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cristiano C, Catanuso M, Di Gregorio C, Di Gregorio A, Profeta G, Di Guardo A. Comparing the use of traditional sites and alternative sites puncture for determination of blood glucose by glucometer. Br J Med Pract. 2015;8(4):A835. [Google Scholar]
- 21.Villena Gonzales W, Mobashsher AT, Abbosh A. The progress of glucose monitoring-a review of invasive to minimally and non-invasive techniques, devices and sensors. Sensors (Basel) 2019;19(4):800. doi: 10.3390/s19040800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christina MB. Unlocking the full potential of self-monitoring of blood glucose. US Pharm. 2019;44(10):29–32. [Google Scholar]
- 23.Oguejiofor OC, Odenigbo CU, Oguejiofor CB. Evaluation of the effect of duration of diabetes mellitus on peripheral neuropathy using the United Kingdom screening test scoring system, bio-thesiometry and aesthesiometry. Niger J Clin Pract. 2010;13(3):240–7. [PubMed] [Google Scholar]
- 24.Nisar MU, Asad A, Waqas A, Ali N, Nisar A, Qayyum MA. et al. Association of diabetic neuropathy with duration of type 2 diabetes and glycemic control. Cureus. 2015;7(8):e302. doi: 10.7759/cureus.302. [DOI] [PMC free article] [PubMed] [Google Scholar]