Abstract
Background/purpose
Color-changeable chewing gum is used for the evaluation of masticatory performance. However, it is currently unclear whether colorimetric and visual assessment methods yield consistent results. This study aimed to clarify the consistency between colorimetric and visual methods used for the evaluation of color changes in color-changeable chewing gum.
Materials and methods
The sample comprised 644 older persons (mean age, 75.4 ± 6.4 years). The chewing gum was masticated 60 times at the participant's own chewing rate and then expectorated. The color of the chewing gum was evaluated with the ΔE values and a∗ values, measured using a colorimeter, and the 10 Color Shades (10CSh) and 5 Color Scales (5CSc), using visual evaluation. Spearman's correlation analysis was performed to examine the correlation between the results obtained by the four methods. The significance level was set at α = 0.05.
Results
The ΔE values, a∗ values, 10CSh scores, and 5CSc scores were all significantly correlated. The highest correlation coefficient (0.979) was between the ΔE values and a∗ values. The lowest correlation coefficient (0.847) was between the a∗ values and 5CSc scores. Decreased masticatory performance was observed with increased age.
Conclusion
Significant correlations were found for all four methods used in the assessment of masticatory performance with color-changeable chewing gum. While visually based assessments are valid, colorimetric methods are more sensitive to smaller changes in masticatory performance.
Keywords: Aged, Chewing gum, Colorimetry, Color, Mastication
Introduction
Decreased masticatory performance (MP) reportedly leads to compromised nutritional status and general-health worsening in older persons.1,2 Therefore, it is important to regularly evaluate MP for the maintenance of general health.
MP has been evaluated using masticatory samples such as peanuts,3 raw rice,4 silicone,5 paraffin wax,6 chewing gum (CG),7,8 and gummy jelly.9 Among these, color-changeable CG has been widely used in research because it is simple to use to differentiate the levels of MP.1,7,8,10, 11, 12, 13, 14, 15, 16, 17
Color-changeable CG can be used to evaluate MP based on color change after brief mastication. Masticating the CG raises its pH due to the buffering action of saliva and results in outflow of blue and yellow dye and citric acid contained in the CG. Consequently, the color of the chewing-gum gradually changes from yellowish-green to red.10 This color change has been evaluated using the ΔE and a∗ values measured on a colorimeter and via the “10 Color Shades” (10CSh) or “5 Color Scales” (5CSc) using visual evaluation.10
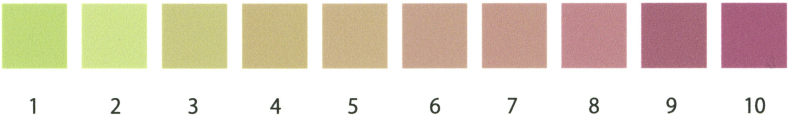
The ΔE and a∗ values are determined using the International Commission on Illumination L∗a∗b∗ (CIELAB) color space model, which expresses color as the L∗ (lightness), a∗ (red/green opponent colors), and b∗ (yellow/blue opponent colors) axes.10,18 The “redness” of the CG is evaluated by measuring only the a∗ value. To determine the ΔE, the difference between two colors in each CIELAB axis is determined and the values are substituted into the following equation: , where 72.3, −14.9, and 33.0, indicate the pre-test values for L∗, a∗, and b∗, respectively.11,13 The 10CSh and 5CSc are methods for visually judging colors considered close to the 10 or 5 color samples, respectively (Figure 1, Figure 2).8,13, 14, 15 However, the relationships between the two colorimetric and two visual evaluation methods remain unclear.
Figure 1.
The 10 Color Shades.
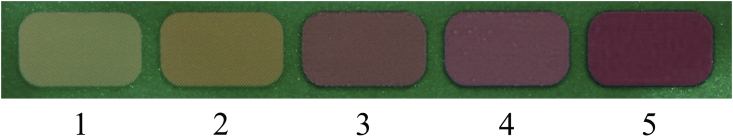
Figure 2.
The 5 Color Scales.
We aimed to clarify the relationships between the ΔE, a∗, 10CSh, and 5CSc values through the evaluation of MP with color-changeable CG in community-dwelling older individuals. A correlation between the colorimetric and visual evaluation results would support the use of visual evaluation, which does not require a dedicated device as a valid measure for assessing color change in color-changeable CG. This would broaden the applicability of color-changeable CG for the screening of MP by non-specialist clinicians and patients.
The two-color wax, which can evaluate MP similar to a color-changeable CG, has already been compared with digital image processing versus visual assessment,19 and a significant correlation was found between them; the digital assessment was able to judge MP more accurately. We expected a significant correlation among the four evaluation methods but hypothesized that a more accurate judgment would be possible using a colorimeter.
Materials and methods
Participants
The participants were adults aged ≥65 years (at the end of March 2019), living in Kusatsu town, Gunma Prefecture. Participants were mailed an invitation to participate in a comprehensive health examination at a public-health center. All participants provided written informed consent.20 The only exclusion criterion was refusal of the MP evaluation using color-changeable CG; all other individuals were evaluated for masticatory performance. The study was approved by the Ethics Committee of the Tokyo Metropolitan Institute of Gerontology (Approval No. 3 in 2008, No. zin 15 in 2018) and complied with the requirements of the Declaration of Helsinki and the Strengthening the Reporting of Observational Studies in Epidemiology statement guidelines.21 Participants who routinely used removable dentures underwent the intra-oral examination while wearing their dentures to ensure optimum MP.
Evaluation methods
MP was evaluated using a piece of color-changeable CG (Masticatory Performance Evaluating Gum XYLITOL, Lotte Co., Ltd., Tokyo, Japan). Participants were instructed to masticate the CG 60 times at their own chewing rate.10,11 After mastication, the CG was expectorated into a clear plastic bag and pressed to a thickness of 1.5 mm. The CG color after mastication was evaluated by the four evaluation methods in random order. All four evaluation methods were completed within an average of 3 min. Four dentists used standardized criteria to evaluate the CG color change. Each dentist was previously trained in the use of one assigned assessment method and only conducted evaluations using this specific method. None of the evaluators had visual impairments, e.g., color blindness.
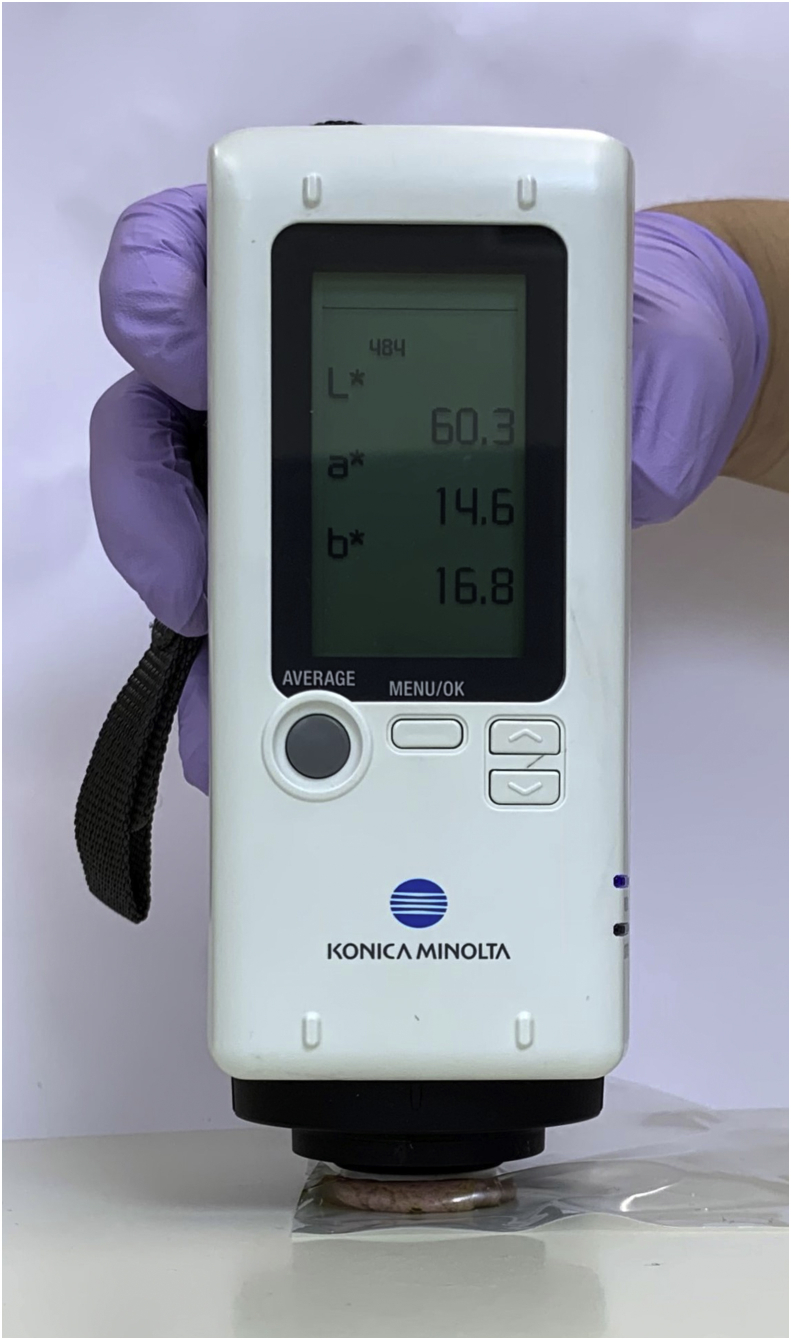
Colorimeter measurement
The CG color after mastication was evaluated using a colorimeter (CR-20 Color Reader, KONICA MINOLTA, Tokyo, Japan; Fig. 3),11, 12, 13 pressed on the surface of the gum at five random locations. The ΔE and a∗ values were measured at each location, and their mean value was calculated.10
Figure 3.
Colorimeter.
Visual evaluation
The CG color after mastication was evaluated with the 10CSh,13, 14, 15 consisting of 10 colors (see Fig. 1, scores 1–10), and the 5CSc,8 consisting of five colors (see Fig. 2, scores 1–5). The evaluator selected one color each from the 10CSh and 5CSc that were closest to the color of the CG after mastication. Each color score increased as it approached red. When visually judging a CG where there was a mix of multiple colors, the color of the area considered the largest was evaluated.
Other recorded variables
Participant characteristics related to MP were also evaluated and included the number of present,17 artificial,17 and functional teeth22; and the use of removable dentures.17 The number of artificial teeth referred to those present in the removable dentures, if they were worn. The number of functional teeth referred to the sum of the number of present teeth, artificial teeth, pontics, and superstructures of implant prostheses. Stump teeth or teeth that were not in occlusion due to significant mobility were not included in the number of present teeth. Additionally, dry mouth was evaluated using an oral moisture checker (Mucus, Life Co., Ltd., Saitama, Japan)23 and a self-administered questionnaire containing the question: “Do you often experience dry mouth?”24 All factors were evaluated by six dentists who were trained in the use of the standardized assessment criteria.
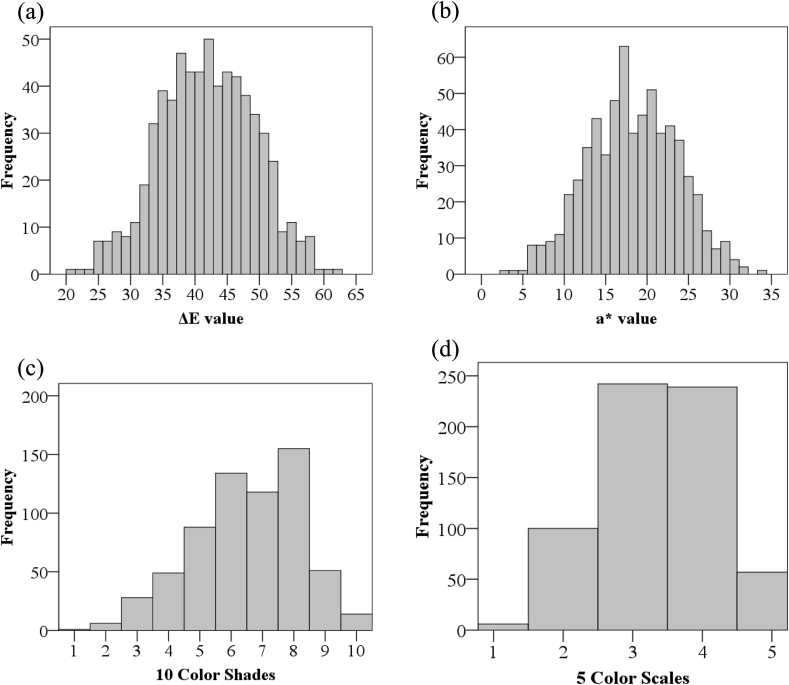
Statistical analysis
The statistical analysis was performed in four stages. First, the Shapiro–Wilk test was conducted to confirm the normality of the ΔE values, a∗ values, 10CSh scores, and 5CSc scores. The P-values were 0.300, 0.423, <0.001, and <0.001, respectively. As the 10CSh and 5CSc scores were non-normally distributed, non-parametric tests were used for comparisons. The histograms for each of the four evaluation methods are shown in Fig. 4. Second, sex differences in the outcome measures were examined with the Mann–Whitney U and chi-squared tests. Third, the tendency for age-related differences in the evaluation results was examined using the Jonckheere–Terpstra test, followed by Bonferroni correction. Since Bonferroni correction impacts the significance level, only the results pertaining to the color-changeable CG were subjected to the Jonckheere–Terpstra test. Finally, correlations between the ΔE values, a∗ values, 10CSh scores, and 5CSc scores were examined by Spearman's correlation analyses. The sample size for the correlation analysis (i.e., the main analysis) was calculated using G∗ power (3.1.9.2).25 To achieve an effect size of 0.3, α error of 0.05, and power (1-β error probability) of 0.95 for a two-sided test, the required sample size was 134. Analyses were performed using SPSS version 24 (IBM Corp., Armonk, NY, USA). The significance level was set at 0.05.
Figure 4.
Histograms for each of the four evaluation methods. a. Distribution of ΔE values, b. Distribution of a∗ values, c. Distribution of 10CSh scores, d. Distribution of 5CSc scores. Based on the Shapiro–Wilk test results, the ΔE values and a∗ values showed a normal distribution, but the 10CSh and 5CSc scores did not. 5CSc: 5 Color Scales,10CSh: 10 Color Shades.
Results
Of the 2478 older persons who received the invitation, 769 visited the public-health center and participated in the health examination. Among them, 125 participants refused to undergo the MP evaluation using color-changeable CG and were excluded. Thus, 644 (377 women; mean age, 75.4 ± 6.4 years) individuals were included in the MP analysis.
The participant characteristics are shown in Table 1. The ΔE values, a∗ values, 10CSh scores, and 5CSc scores used to evaluate color change in the CG were significantly higher among men. Altogether, 392 participants (61.0%) wore removable dentures. The mean ± standard deviations of the number of present and functional teeth was 15.1 ± 10.2 and 26.9 ± 2.9, respectively. Regarding occlusal support, the Eichner index was A in 177 (27.9%), B in 232 (36.6%), and C in 225 (35.5%) participants. There was a sex difference in subjective symptoms of dry mouth but not in the oral moisture score.
Table 1.
Participant characteristics.
| Overall |
Men |
Women |
P value | ||
|---|---|---|---|---|---|
| n = 644 |
n = 267 |
n = 377 |
|||
| Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | |||
| Age (years) | 75 (70, 80) | 75 (70, 79) | 76 (71, 80) | 0.056∗ | |
| ΔE value | 41.8 (36.8, 47.2) | 43.8 (38.7, 48.5) | 41.0 (35.9, 46) | <0.001∗ | |
| a∗ value | 18.1 (14.4, 22.3) | 19.6 (15.7, 23.1) | 17.5 (13.6, 21.5) | <0.001∗ | |
| 10 Color Shades | 7 (5, 8) | 7 (6, 8) | 6 (5, 8) | <0.001∗ | |
| 5 Color Scales | 3 (3, 4) | 4 (3, 4) | 3 (3, 4) | <0.001∗ | |
| Number of present teeth | 18 (6, 25) | 19 (6, 25) | 17 (5, 24) | 0.104∗ | |
| Number of artificial teeth | 6 (0, 22) | 5 (0, 20) | 7 (0, 22) | 0.294∗ | |
| Number of functional teeth | 28 (27, 28) | 28 (27, 28) | 28 (27, 28) | 0.112∗ | |
| Oral moisture score | 28.5 (26.8, 29.8) | 28.5 (27.1, 29.8) | 28.5 (26.7, 29.8) | 0.680∗ | |
| n (%) |
n (%) |
n (%) |
P value |
||
| Eichner index | A | 177 (27.9) | 80 (30.5) | 97 (26.1) | 0.414∗∗ |
| B | 232 (36.6) | 95 (36.3) | 137 (36.8) | ||
| C | 225 (35.5) | 87 (33.2) | 138 (37.1) | ||
| Removable denture use | Yes | 392 (61.0) | 158 (59.4) | 234 (62.1) | 0.494∗∗ |
| Subjective symptoms of dry mouth | Yes | 200 (31.1) | 56 (21.0) | 144 (38.2) | <0.001∗∗ |
Q1: First quartile, Q3: Third quartile.
∗: Mann–Whitney U test.
∗∗: Chi-squared test.
The results of the four evaluation methods for chewing gum color change all showed significant differences between men and women.
The results of age-specific color changes and factors related to MP are shown in Table 2, Table 3, Table 4. When the results of the four evaluation methods were examined for the whole sample, the values were lower with increased age. Men did not show decreased values with increased age in any of the evaluation methods; for women, only the ΔE value was lower with increased age. The number of present teeth tended to be lower with increased age.
Table 2.
Values of the evaluation items for the different age groups.
| Years | 65–69 |
70–74 |
75–79 |
80–84 |
≥85 |
P value |
|---|---|---|---|---|---|---|
| n = 137 |
n = 155 |
n = 189 |
n = 111 |
n = 52 |
||
| Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | ||
| Age (years) | 68 (66, 69) | 72 (71, 74) | 77 (76, 78) | 82 (81, 83) | 88 (86, 90) | – |
| ΔE value | 44.3 (37.4, 48.4) | 43.9 (38, 49) | 40.5 (35.9, 45.6) | 41.4 (37.9, 46.5) | 38.2 (34.0, 43.5) | <0.001 |
| a∗ value | 19.6 (14.7, 23.0) | 19.9 (15.5, 23.3) | 17.3 (13.6, 21.0) | 18.0 (15.2, 21.6) | 16.5 (13.2, 19.9) | 0.001 |
| 10 Color Shades | 7 (6, 8) | 7 (6, 8) | 6 (5, 8) | 7 (6, 8) | 6 (5, 8) | 0.005 |
| 5 Color Scales | 4 (3, 4) | 4 (3, 4) | 3 (3, 4) | 3 (3, 4) | 3 (2, 4) | 0.006 |
| Number of present teeth | 22 (17, 27) | 21 (12, 25) | 15 (4, 24) | 9 (0, 24) | 3.5 (0, 13) | – |
| Number of artificial teeth | 0 (0, 8) | 2 (0, 14) | 11 (0, 23) | 17 (0, 28) | 24 (14, 28) | – |
| Number of functional teeth | 27 (26, 28) | 28 (26, 28) | 28 (27, 28) | 28 (27, 28) | 28 (28, 28) | – |
| Oral moisture score |
28.6 (26.9, 29.8) |
28.9 (27.1, 30.0) |
28.3 (26.7, 29.7) |
28.7 (27.7, 29.6) |
28.0 (25.9, 29.6) |
– |
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
||
| Subjective symptoms of dry mouth | 38 (27.7) | 44 (28.4) | 64 (33.9) | 38 (34.2) | 16 (30.8) | – |
Q1: First quartile, Q3: Third quartile.
Jonckheere–Terpstra test; Bonferroni corrected P value, P < 0.0125.
All four evaluation methods for color-changeable chewing gum showed decreased values with increased age.
Table 3.
Values of the evaluation items for the different age groups among men.
| Years | 65–69 |
70–74 |
75–79 |
80–84 |
≥85 |
P value |
|---|---|---|---|---|---|---|
| n = 66 |
n = 67 |
n = 70 |
n = 44 |
n = 20 |
||
| Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | ||
| Age (years) | 68 (66, 69) | 72 (71, 73) | 77 (76, 78) | 82 (81, 83) | 88 (85, 92) | – |
| ΔE value | 45.3 (40.5, 49.5) | 45.3 (38.7, 49.1) | 42.7 (37.1, 47.3) | 43.8 (39.7, 48.1) | 38.8 (34.1, 46.8) | 0.033 |
| a∗ value | 20.3 (17.0, 23.6) | 21.0 (15.9, 23.4) | 18.5 (14.3, 22.1) | 19.5 (16.4, 23.5) | 16.1 (11.7, 22.6) | 0.061 |
| 10 Color Shades | 7 (6, 8) | 7 (6, 8) | 7 (6, 8) | 7 (6, 8) | 7 (4, 8) | 0.097 |
| 5 Color Scales | 4 (3, 4) | 4 (3, 4) | 3 (3, 4) | 4 (3, 4) | 3 (2, 4) | 0.080 |
| Number of present teeth | 23 (12, 27) | 21 (12, 25) | 16 (2, 25) | 13 (2, 25) | 6 (0, 15) | – |
| Number of artificial teeth | 0 (0, 13) | 2 (0, 13) | 11 (0, 23) | 14 (0, 26) | 20 (2, 28) | – |
| Number of functional teeth | 28 (26, 28) | 28 (26, 28) | 28 (27, 28) | 28 (27, 28) | 28 (26, 28) | – |
| Oral moisture score |
28.6 (27.0, 29.7) |
28.9 (27.2, 30.0) |
28.4 (27.0, 29.7) |
28.9 (27.9, 30.0) |
26.4 (23.9, 29.5) |
– |
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
||
| Subjective symptoms of dry mouth | 11 (16.7) | 11 (16.4) | 20 (28.6) | 8 (18.2) | 6 (30.0) | – |
Q1: First quartile, Q3: Third quartile.
Jonckheere–Terpstra test; Bonferroni corrected P value, P < 0.0125.
When the results of the four evaluation methods for chewing gum color change were examined according to age and sex, there was no age-related decrease in masticatory performance in men.
Table 4.
Values of the evaluation items for the different age groups among women.
| Years | 65–69 |
70–74 |
75–79 |
80–84 |
≥85 |
P value |
|---|---|---|---|---|---|---|
| n = 71 |
n = 88 |
n = 119 |
n = 67 |
n = 32 |
||
| Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | Median (Q1, Q3) | ||
| Age (years) | 67 (67, 68) | 72 (71, 74) | 77 (76, 78) | 82 (81, 83) | 88 (87, 90) | – |
| ΔE value | 41.4 (35.4, 47.2) | 43.2 (37.3, 48.6) | 39.5 (35.1, 44.7) | 40.4 (36.6, 45.0) | 38.2 (34.0, 41.4) | 0.006 |
| a∗ value | 17.6 (13.5, 22.2) | 19.0 (14.6, 23.2) | 16.8 (13.4, 20.2) | 17.0 (14.5, 20.5) | 16.6 (13.4, 18.3) | 0.026 |
| 10 Color Shades | 6 (5, 8) | 7 (5, 8) | 6 (5, 7) | 6 (5, 7) | 6 (5, 7) | 0.068 |
| 5 Color Scales | 3 (3, 4) | 4 (3, 4) | 3 (3, 4) | 3 (3, 4) | 3 (2, 4) | 0.074 |
| Number of present teeth | 21 (19, 26) | 22 (12, 26) | 15 (4, 23) | 6 (0, 22) | 1 (0, 9) | – |
| Number of artificial teeth | 0, (0, 6) | 3 (0, 14) | 11 (0, 22) | 20 (0, 28) | 27 (19, 28) | – |
| Number of functional teeth | 27 (25, 28) | 28 (26, 28) | 28 (27, 28) | 28 (27, 28) | 28 (28, 28) | – |
| Oral moisture score |
28.6 (26.6, 29.8) |
28.5 (26.9, 29.9) |
28.3 (26.4, 29.7) |
28.6 (27.2, 29.6) |
28.2 (26.5, 29.7) |
– |
| n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
||
| Subjective symptoms of dry mouth | 27 (38.0) | 33 (37.5) | 44 (37.0) | 30 (44.8) | 10 (31.3) | – |
Q1: First quartile, Q3: Third quartile.
Jonckheere–Terpstra test; Bonferroni corrected P value, P < 0.0125.
When the results of the four evaluation methods for chewing gum color change were examined according to age and sex, the ΔE value showed a tendency to decrease with aging in women.
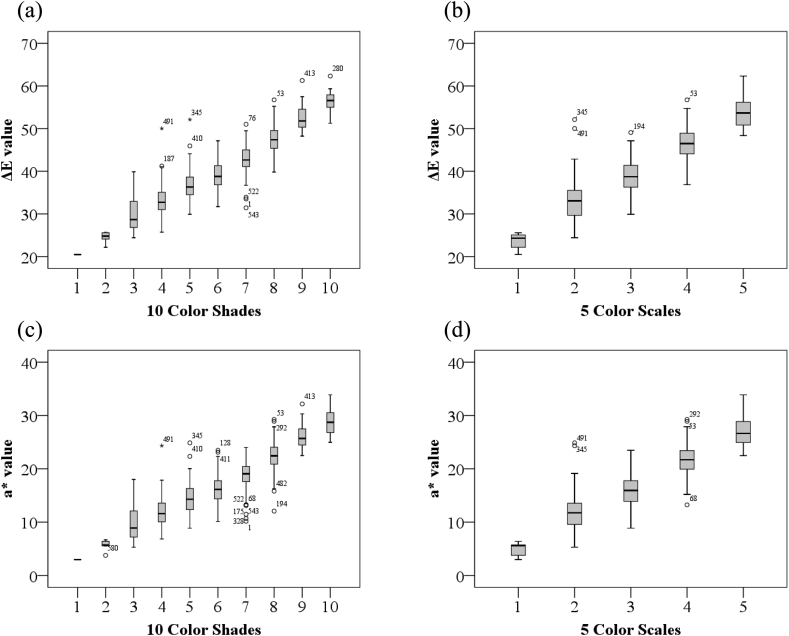
The correlations among the four evaluation methods are shown in Table 5, Table 6, Table 7. All four evaluation methods were significantly correlated, both for the overall sample and when analyzed by sex. For the overall sample, the highest correlation coefficient (0.979) was between the ΔE and a∗ values. The lowest correlation coefficient (0.847) was between the a∗ values and 5CSc scores. The box and whisker plots of the ΔE and a∗ values and the 10CSh and 5CSc scores are shown in Fig. 5.
Table 5.
Correlation analysis of the four evaluation methods for the overall sample.
| Evaluation methods | ΔE value | a∗ value | 10 Color Shades | 5 Color Scales |
|---|---|---|---|---|
| ΔE value | 1.000 | |||
| a∗ value | 0.979 | 1.000 | ||
| 10 Color Shades | 0.878 | 0.862 | 1.000 | |
| 5 Color Scales | 0.854 | 0.847 | 0.921 | 1.000 |
Spearman rank correlation test.
In the whole-sample analysis, there were significant correlations between all four evaluation methods.
P < 0.001 for all correlations.
Table 6.
Correlation analysis of the four evaluation methods in men.
| Evaluation methods | ΔE value | a∗ value | 10 color shades | 5 color scales |
|---|---|---|---|---|
| ΔE value | 1.000 | |||
| a∗ value | 0.968 | 1.000 | ||
| 10 Color Shades | 0.888 | 0.860 | 1.000 | |
| 5 Color Scales | 0.862 | 0.850 | 0.913 | 1.000 |
Spearman rank correlation test.
In the men-only correlation analysis, there were significant correlations between all four evaluation methods.
P < 0.001 for all correlations.
Table 7.
Correlation analysis of the four evaluation methods in women.
| Evaluation methods | ΔE value | a∗ value | 10 Color Shades | 5 Color Scales |
|---|---|---|---|---|
| ΔE value | 1.000 | |||
| a∗ value | 0.986 | 1.000 | ||
| 10 Color Shades | 0.867 | 0.862 | 1.000 | |
| 5 Color Scales | 0.843 | 0.842 | 0.922 | 1.000 |
Spearman rank correlation test.
In the women-only correlation analysis, there were significant correlations between all four evaluation methods.
P < 0.001 for all correlations.
Figure 5.
Box-and-whisker plots of the ΔE values, a∗ values, 10CSh scores, and 5CSc scores. a. Boxplot of ΔE values and 10CSh scores, b. Boxplot of ΔE values and 5CSc scores, c. Boxplot of a∗ values and 10CSh scores, d. Boxplot of a∗ values and 5CSc scores. 10CSh and 5CSc scores increased with increased ΔE values and a∗ values. 5CSc: 5 Color Scales, 10CSh: 10 Color Shades.
Discussion
Regular MP evaluation is important, as impairment may contribute to general-health deterioration.1,2 While the use of a color-changeable CG is a simple and sensitive means of evaluating MP,1,7,8,10, 11, 12, 13, 14, 15, 16, 17 the relationships between the methods used for its assessment remain unclear. Here, we aimed to clarify the relationships between the ΔE values, a∗ values, 10CSh scores, and 5CSc scores via MP assessment with color-changeable CG in community-dwelling older individuals.
In most participants, missing teeth had been replaced by prostheses. While the difference in the number of functional teeth in participants with, versus without, prostheses was not large, the number of present teeth was low among all participants.1,16,26,27 The color-change values for the CG were higher for men as previously reported.1 Dry mouth affected MP in older persons as assessed by color-changeable CG.12 Additionally, epidemiologic studies have shown that women have a higher prevalence of perceived symptoms of dry mouth or xerostomia at all ages.28 Here, the percentage of subjective symptoms of dry mouth was higher in women, and this may have accounted for the higher MP level in men. MP, along with several factors related to MP, showed a tendency to decrease with age. Similar results have been previously reported for older persons.1,26
The color change in the CG used here is caused by long-term chemical reactions10 continuing after the initial rapid color change. Particularly, significant color changes occur 30 min after mastication.29 Accordingly, color evaluation must be performed within the first 30 min after the mastication test. Here, the four evaluation methods were used in random order, and all evaluations were completed within a mean time of 3 min. Therefore, measurement bias due to the sequence of assessment and color change over time was minimal.
The ΔE values, a∗ values, 10CSh scores, and 5CSc scores used for the color-change evaluation were significantly and highly correlated. The 5CSc scores are significantly correlated with the a∗ values,8 and the scores obtained from the 11 Color Shades (from which the 10CSh is derived) are significantly correlated with the ΔE values.13 These findings support the present results.
This was the first study to examine the relationships between the four evaluation methods currently used to assess color changes in color-changeable CG. Furthermore, a high correlation coefficient (0.854) between the ΔE values and the 5CSc scores was firstly reported. The results here support the practicality of the 5CSc for MP assessment. As this study included older persons who required regular MP evaluation, we believe that our results have practical utility in real-world clinical settings. A strength of this study is that we accounted for the number of present and functional teeth and the presence of dry mouth; such reference data may inform the development of future studies aiming to investigate MP with color-changeable CG.
Studies evaluating MP with color-changeable CG have mainly been conducted among young adults with very few missing teeth or older individuals with either very few remaining teeth or edentulism.8,11,13,29,30 Our sample comprised older persons who had a wider range in the number of either natural or prosthetic teeth (Table 1, Table 2, Table 3, Table 4). The finding of significant correlations between the ΔE values, a∗ values, 10CSh scores, and 5CSc scores among such a heterogeneous population highlights both the broad applicability and validity of each assessment method.
Measuring the MP of the overall sample using the ΔE values, a∗ values, 10CSh scores, and 5CSc scores clearly showed that the older the individual, the lower the MP. However, the median 5CSc score was four and three in the 65–69- and 70–74-year-old groups, respectively, and three in the oldest age groups. Based on these results, the 10CSh can be considered more suitable than the 5CSc when visually evaluating slight MP changes (e.g., physiological changes over time due to aging). While the 5CSc is a less sensitive MP measure, it may be more suitable in cases where large changes are expected (e.g., before and after treatment) or where screening is to be performed by non-specialists or patients.
The reliability and validity of visual evaluation have been reported.13 However, based on the results divided by sex, there was no tendency for decreased MP with aging when using visual evaluation. Therefore, when the purpose is to evaluate MP accurately and in detail, it is considered preferable to use a colorimeter instead of visual evaluation.
Measurement of the ΔE and a∗ values requires a dedicated and expensive color discriminator. Moreover, to obtain the ΔE value, a numerical value must be derived using the appropriate formula after measurement with the colorimeter.11,13 As a very high correlation was found between the ΔE and a∗ values, it may be possible to evaluate MP with the a∗ value, which is simpler than ΔE value calculation. However, only the ΔE value could demonstrate the tendency for decreased MP with aging in the analysis by sex. Therefore, among the four evaluation methods, the ΔE value is considered the most accurate.
This study had some limitations. The color-changeable CG was evaluated by four dentists without color blindness. While the evaluation of MP using color-changeable CG has been reported to have high intra- and inter-examiner consistency,8 the significant correlations between the four evaluation methods may have been influenced by the properly trained dentists carrying out the assessments using standardized criteria. The results may have been different if the evaluators lacked experience with the use of colorimeters or had color blindness. Additionally, there was a discrepancy between both the subjective and objective evaluation of dry mouth between men and women; the cause of this could not be clarified and should be examined in future studies.
Our findings suggest that the four currently used measures for assessing color change in color-changeable CG yield consistent results when used to evaluate MP in community-dwelling older individuals. Nevertheless, as current protocols for MP evaluation vary in terms of mastication duration and number of chewing cycles performed, future comparative studies are required to optimize and standardize these parameters.
In conclusion, significant correlations were found between the ΔE values, a∗ values, 10CSh scores, and 5CSc scores when used in the evaluation of MP using color-changeable CG in older persons. The finding of significant correlations between visual and colorimeter-based evaluations suggests that visual evaluation methods, such as the 10CSh and 5CSc, are valid.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgement
We would like to express our sincere appreciation to the staff of Research on Social and Human Sciences, Tokyo Metropolitan Institute of Gerontology, for their tremendous support. This study was supported by grants from the Tokyo Metropolitan Government, Tokyo Metropolitan Institute of Gerontology, and AMED under Grant Number JP18dk0110019; Research Funding for Longevity Sciences (29–42) from the National Center for Geriatrics and Gerontology (NCGG); and JSPS KAKENHI (grant number: JP16K11908, JP17K13239, JP20K10297).
References
- 1.Tanaka T., Takahashi K., Hirano H. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci. 2018;73:1661–1667. doi: 10.1093/gerona/glx225. [DOI] [PubMed] [Google Scholar]
- 2.Kossioni A.E. The association of poor oral health parameters with malnutrition in older adults: a review considering the potential implications for cognitive impairment. Nutrients. 2018;10:1709. doi: 10.3390/nu10111709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manly R.S., Braley L.C. Masticatory performance and efficiency. J Dent Res. 1950;29:448–462. doi: 10.1177/00220345500290040701. [DOI] [PubMed] [Google Scholar]
- 4.Imamura T. A new spectrophotometric method for simple determination of masticatory efficiency. Ann Jpn Prosthodont Soc. 1979;23:603–612. [Google Scholar]
- 5.Khoury-Ribas L., Ayuso-Montero R., Rovira-Lastra B., Peraire M., Martinez-Gomis J. Reliability of a new test food to assess masticatory function. Arch Oral Biol. 2018;87:1–6. doi: 10.1016/j.archoralbio.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Sato H., Fueki K., Sueda S. A new and simple method for evaluating masticatory function using newly developed artificial test food. J Oral Rehabil. 2003;30:68–73. doi: 10.1046/j.1365-2842.2003.01049.x. [DOI] [PubMed] [Google Scholar]
- 7.Hayakawa I., Watanabe I., Hirano S., Nagao M., Seki T. A simple method for evaluating masticatory performance using a color-changeable chewing gum. Int J Prosthodont. 1998;11:173–176. [PubMed] [Google Scholar]
- 8.Kamiyama M., Kanazawa M., Fujinami Y., Minakuchi S. Validity and reliability of a self-implementable method to evaluate masticatory performance: use of color-changeable chewing gum and a color scale. J Prosthodont Res. 2010;54:24–28. doi: 10.1016/j.jpor.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Igarashi K., Watanabe Y., Kugimiya Y. Validity of a visual scoring method using gummy jelly for evaluating chewing efficiency in a large-scale epidemiological survey. J Oral Rehabil. 2019;46:409–416. doi: 10.1111/joor.12761. [DOI] [PubMed] [Google Scholar]
- 10.Tarkowska A., Katzer L., Ahlers M.O. Assessment of masticatory performance by means of a color-changeable chewing gum. J Prosthodont Res. 2017;61:9–19. doi: 10.1016/j.jpor.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Hama Y., Kanazawa M., Minakuchi S., Uchida T., Sasaki Y. Properties of a color-changeable chewing gum used to evaluate masticatory performance. J Prosthodont Res. 2014;58:102–106. doi: 10.1016/j.jpor.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Kubota C., Kanazawa M., Hama Y., Komagamine Y., Minakuchi S. Association between chewing-stimulated salivary flow under the effects of atropine and mixing ability assessed using a color-changeable chewing gum. J Prosthodont Res. 2017;61:387–392. doi: 10.1016/j.jpor.2016.12.009. [DOI] [PubMed] [Google Scholar]
- 13.Hama Y., Kanazawa M., Minakuchi S., Uchida T., Sasaki Y. Reliability and validity of a quantitative color scale to evaluate masticatory performance using color-changeable chewing gum. J Med Dent Sci. 2014;61:1–6. [PubMed] [Google Scholar]
- 14.Matsuo K., Taniguchi H., Nakagawa K. Relationships between deterioration of oral functions and nutritional status in elderly patients in an acute hospital. Jpn J Gerodont. 2016;31:123–133. [Google Scholar]
- 15.Nakazawa M., Mori H., Handa J. Simple training for maintaining and improving chewing ability. Jpn J Gerodont. 2018;33:63–69. [Google Scholar]
- 16.Murakami M., Hirano H., Watanabe Y., Sakai K., Kim H., Katakura A. Relationship between chewing ability and sarcopenia in Japanese community-dwelling older adults. Geriatr Gerontol Int. 2015;15:1007–1012. doi: 10.1111/ggi.12399. [DOI] [PubMed] [Google Scholar]
- 17.Kugimiya Y., Watanabe Y., Igarashi K. Factors associated with masticatory performance in community-dwelling older adults: a cross-sectional study. J Am Dent Assoc. 2020;151:118–126. doi: 10.1016/j.adaj.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Wargalla H. 2003. [Device independent color: an introduction to lab color model] Farbe geräteunabhängig: Eine Einführung in das Lab-Farbmodell. [Google Scholar]
- 19.van der Bilt A., Speksnijder C.M., de Liz Pocztaruk R., Abbink J.H. Digital image processing versus visual assessment of chewed two-colour wax in mixing ability tests. J Oral Rehabil. 2012;39:11–17. doi: 10.1111/j.1365-2842.2011.02229.x. [DOI] [PubMed] [Google Scholar]
- 20.Kugimiya Y., Watanabe Y., Ueda T. Rate of oral frailty and oral hypofunction in rural community-dwelling older Japanese individuals. Gerodontology. 2020 Mar 6 doi: 10.1111/ger.12468. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.von Elm E., Altman D.G., Egger M. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 22.Hirano H., Ishiyama N., Watanabe I., Nasu I. Masticatory ability in relation to oral status and general health on aging. J Nutr Health Aging. 1999;3:48–52. [PubMed] [Google Scholar]
- 23.Takano T., Kugimiya Y., Morita K., Tazawa S., Ueda T., Sakurai K. Intra- and inter-investigator reliabilities of oral moisture measured using an oral moisture-checking device. J Oral Rehabil. 2020;47:480–484. doi: 10.1111/joor.12919. [DOI] [PubMed] [Google Scholar]
- 24.Arai H., Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015;15:518–519. doi: 10.1111/ggi.12397. [DOI] [PubMed] [Google Scholar]
- 25.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G∗Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 26.Watanabe Y., Hirano H., Arai H. Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc. 2017;65:66–76. doi: 10.1111/jgs.14355. [DOI] [PubMed] [Google Scholar]
- 27.Ikebe K., Matsuda K., Murai S., Maeda Y., Nokubi T. Validation of the Eichner index in relation to occlusal force and masticatory performance. Int J Prosthodont. 2010;23:521–524. [PubMed] [Google Scholar]
- 28.Han P., Suarez-Durall P., Mulligan R. Dry mouth: a critical topic for older adult patients. J Prosthodont Res. 2015;59:6–19. doi: 10.1016/j.jpor.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Yamaga E., Kanazawa M., Uchida T. The influence of storage methods of a chewed colour-changeable chewing gum on colour difference. J Jpn Soc Masticatory Sci Health Promot. 2013;23:75–80. [Google Scholar]
- 30.Hirano K., Takahashi Y., Hirano S., Hayakawa I., Seki T. A study on measurement of masticatory ability using a color-changeable chewing gum with a new coloring. Ann Jpn Prosthodont Soc. 2002;46:103–109. [Google Scholar]