Abstract
Sometimes the only indicator of a serious infection in a neonate is a fever. Citrobacter koseri (C. koseri) has been reported to cause neonatal brain abscesses in the setting of meningitis. Although rare, pneumocephalus, secondary to C. koseri, carries a very high mortality. A 17-day-old male presented to the emergency department with a fever, decreased oral intake, and lethargy. The patient developed pneumocephalus and cerebral edema and was diagnosed with C. koseri meningitis, leading to death. This case demonstrates the presentation of C. koseri meningitis with pneumocephalus and cerebral edema in a neonate presenting with fever.
Keywords: Citrobacter koseri, Meningitis, Pneumocephalus, Encephalitis, Neonatal
Introduction
The presence of a fever, a rectal temperature greater than 38°C, may be the only indicator of a serious infection in a neonate [1,2]. Thus, it is considered standard of care to perform an extensive work-up upon emergency department (ED) arrival in febrile patients <60 days of age to assess for underlying infection. Pruitt et al. found that infants with bacterial meningitis and bacteremia were more likely to experience adverse outcomes than patients with only bacteremia [1].
Citrobacter koseri (C. Koseri) is a facultative anaerobic, gram-negative bacillus that produces gas by catabolizing glucose and other carbohydrates and is a possible cause of meningitis within the first 2 months of life [3,4]. It is unclear whether neonates acquire the infection via vertical transmission or inoculation from environmental factors, however there might be a developmental protection obtained after the first few months of life [3]. This is further evidenced by Alviedo et al., who found a lack of reported cases of C. koseri meningitis in infants over 2 months old [5].
C. koseri in most cases causes cerebral adhesions and abscesses [3,4]. Rare cases resulting in fatality have been reported of neonates acquiring meningitis from C. koseri and developing pneumocephalus and encephalitis [5,6].
Research suggests a possible predisposition of preterm infants to develop C. koseri meningitis, as approximately one-third of reported cases have occurred in infants with a gestational age of less than 36 weeks [5]. To our knowledge, this is the first case of C. koseri meningitis with cerebral edema and pneumocephalus in a previously healthy infant born nearly full term.
Case Report
A 17-day-old male presented to the ED with decreased oral intake, lethargy, and fever for less than 1 day, with a rectal temperature of 38.3°C. The patient was born via cesarean delivery secondary to breech presentation at 37 weeks gestation. Family denied any known sick contacts, travel outside the country, and any changes to formula. Past medical history was only remarkable for a mildly elevated bilirubin, which was monitored and did not require phototherapy.
Review of systems was positive for fever and decreased activity, oral intake, and urinary output. The patient's triage vitals were: blood pressure 65/37, heart rate 210, temperature 39.2°C, respirations 52, weight 8lbs 6.4oz, and oxygen saturation 100% on room air. A septic work-up was initiated with laboratories and a chest x-ray. Lumbar puncture was delayed due to the mother's hesitancy.
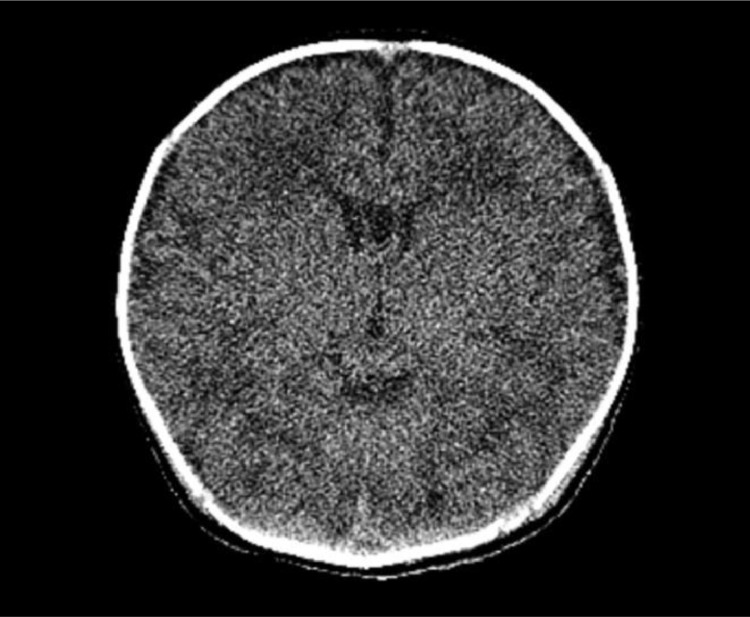
Within an hour of arrival, the patient became hypoxic, with an oxygen saturation of 76% on room air and frequent periods of apnea. Intubation was complicated by vomiting and he decompensated into cardiopulmonary arrest. After multiple failed attempts, 2 rounds of cardiopulmonary resuscitation, and administration of epinephrine, intubation was successful, with return of spontaneous circulation. Ampicillin was initiated and a head computerized tomography (CT) was ordered and performed while the patient was in the ED, but was unremarkable (Image 1).
Image 1.
Normal computed tomography head of patient performed during the ED assessment.
The patient was admitted to the Pediatric Intensive Care Unit, where cefotaxime was initiated.
The following day, his lumbar puncture was positive for gram negative rods. The cerebral spinal fluid culture grew C. koseri. Ampicillin was stopped, and cefotaxime was continued.
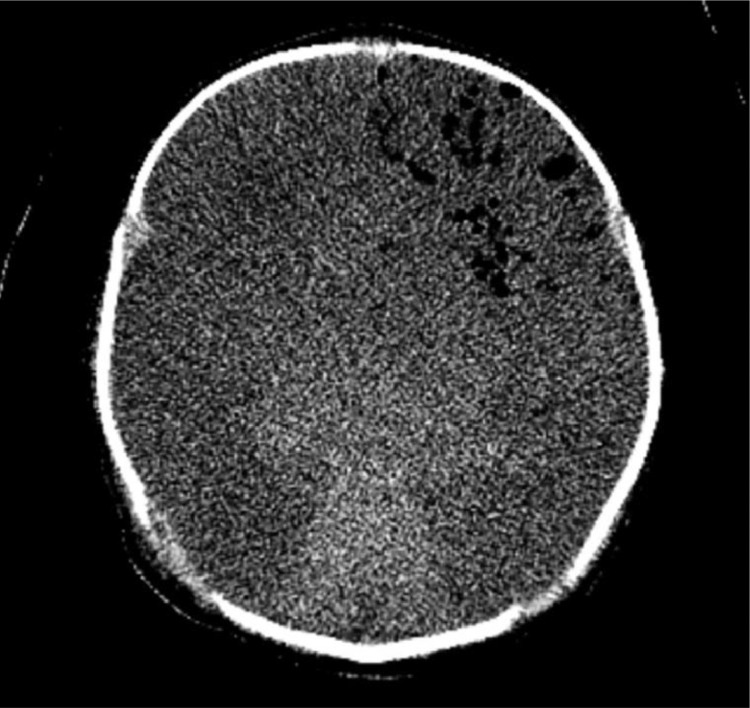
After two days, he began demonstrating signs of herniation. A repeat head CT on hospital day 3 (Image 2) demonstrated diffuse loss of the gray-white matter junction within the supratentorial brain and basal ganglia, diffuse parenchymal edema with new and near complete effacement of the basilar cisterns, diffuse gas throughout the left frontal lobe, and questionable partial herniation of the cerebellar tonsils beneath the foramen magnum.
Image 2.
Repeat computed tomography head of patient on hospital day 3 demonstrating diffuse gas throughout the left frontal lobe, diffuse loss of gray-white matter differentiation, and diffuse parenchymal edema.
Neurologic examination showed no spontaneous movements, response to painful stimuli, pupillary response to light, or cough, gag, and corneal reflexes. An echoencephalography further confirmed diffuse cerebral edema.
Four days after the patient's presentation, brain death was confirmed and the decision was made the following morning to terminally extubate the patient. The coroner verified it was not a coroner's case, and the family requested no autopsy.
Discussion
To our knowledge, this is the first reported case of C. koseri meningitis with cerebral edema and pneumocephalus in a previously healthy neonate born nearly full term. Previously reported neonatal cases of C. koseri meningitis and pneumocephalus were in premature infants or those who have had medical complications prior to diagnosis [5,6]. Martínez-Lage et al. reported a case of a previously healthy 2-month old who was diagnosed with C. koseri meningitis, but without pneumocephalus on the CT scan [4]. Consistent with Pruitt et al.’s results, this case presented a neonate with bacterial meningitis and bacteremia that ended in death despite intervention [1].
Although the exact pathophysiology of how C. koseri contributes to such fatal outcomes is not understood, evidence suggests that it is a largely destructive process, which should be treated quickly and aggressively. Research found that when different strains of C. diversus (now C. koseri) were tested through multilocus enzyme electrophoresis, a 32-kDa outer membrane protein was expressed primarily on those obtained from the cerebral spinal fluid of infants with meningitis [7]. This suggests that this protein may play the role of a virulence factor.
Conclusion
This case serves to acknowledge the possible presentation of C. koseri meningitis with pneumocephalus and cerebral edema in a neonate presenting to the ED with fever. Further study is necessary to understand the bacteria's mechanism of infection in neonates in the hopes of preventing more fatal cases.
Declaration
No written consent has been obtained from the patients as there is no patient identifiable data included in this case report and the patient is deceased.
Footnotes
Acknowledgments: The authors would like to acknowledge Jasdip Kaur, BS for her scholarly assistance with editing and formatting this Case Report.
Competing Interests: None. The authors have no outside support information, conflicts or financial interest to disclose and this work has not been published elsewhere. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Pruitt C.M., Neuman M.I., Shah S.S., Shabanova V., Woll Christopher, Wang M.E. Factors associated with adverse outcomes among febrile young infants with invasive bacterial infections. J Pediatr. 2019;204:177–182. doi: 10.1016/j.jpeds.2018.08.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ramgopal S., Janofsky S., Zuckerbraun N.S., Ramilo O., Mahajan P., Kuppermann N. Risk of serious bacterial infection in infants aged ≤60 days presenting to emergency departments with a history of fever only. J Pediatr. 2019;204:191–195. doi: 10.1016/j.jpeds.2018.08.043. [DOI] [PubMed] [Google Scholar]
- 3.Doran Terence I. The role of Citrobacter in clinical disease of children: review. Clin Infect Dis. 1999;28(2):384–394. doi: 10.1086/515106. [DOI] [PubMed] [Google Scholar]
- 4.Martínez-Lage J.F., Martínez-Lage A.L., Almagro M.J., Bastida M.E., Reyes S., Tellez C. Citrobacter koseri meningitis: a neurosurgical condition? European J Paediatr Neurol. 2010;14(4):360–363. doi: 10.1016/j.ejpn.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Alviedo J.N., Sood B.G., Aranda J.V., Becker C. Diffuse pneumocephalus in neonatal Citrobacter meningitis. Pediatr. 2006;118(5):1576–1579. doi: 10.1542/peds.2006-1224. [DOI] [PubMed] [Google Scholar]
- 6.Pooboni S.K., Mathur S.K., Dux A., Hewertson J., Nichani S. Pneumocephalus in neonatal meningitis: diffuse, necrotizing meningo-encephalitis in Citrobacter meningitis presenting with pneumatosis oculi and pneumocephalus. Pediatr Crit Care Med. 2004;5(4):393–395. doi: 10.1097/01.pcc.0000129136.45258.af. [DOI] [PubMed] [Google Scholar]
- 7.Li J., Musser J.M., Beltran P., Kline M.W., Selander R.K. Genotypic heterogeneity of strains of Citrobacter diversus expressing a 32-kilodalton outer membrane protein associated with neonatal meningitis. J Clin Microbiol. 1990;28(8):1760–1765. doi: 10.1128/jcm.28.8.1760-1765.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]