Abstract
The current study examined the impact of the lockdown due to the Covid-19 disease on mood state and behaviours of children and adolescents with ADHD. Nine hundred ninety-two parents of children and adolescents with ADHD filled out an anonymous online survey through the ADHD family association website. The survey investigated the degree of severity of six emotional and mood states (sadness, boredom, little enjoyment/interest, irritability, temper tantrums, anxiety) and five disrupted behaviours (verbal and physical aggression, argument, opposition, restlessness) based on their frequency/week (absent; low: 1–2 days/week; moderate: 3–4 days/week; severe: 5–7 days/week) before and during the lockdown. Important fluctuations were found in all dimensions during the lockdown independently by the severity degree. Subjects with previous low severity degree of these behaviors significantly worsened in almost all dimensions during the lockdown. On the contrary, ADHD patients with moderate and severe degree showed important improvement during the lockdown. Little enjoyment/interests and boredom resulted the dimensions more strongly affected by the condition of restriction, overall in children. Children vs. adolescents showed substantially similar trend but the former resulted significantly more vulnerable to emotive changes. The results provided both the individuation of domains affected, and the indirect benefits produced by restriction condition.
Keywords: Covid-19, Lockdown, Distress, Attention deficit hyperactivity/impulsivity disorder, Mood state, Behavioral problems
1. Introduction
The confinement due to the Covid-19 disease has represented a great challenge for children and adolescent of the entire world because it required a sudden adaptive change in daily lifestyle caused by imposed restrictions within familiar context. Italy is one of the major COVID-19 hotspots; to prevent disease spread, the lockdown started on March 9, 2020 until May 18 (seventy-one days) forcing people into home confinement and imposed restrictions on the movement of individuals in the entire national territory; but some restriction continued until June 15. The lockdown on the entire Italian territory was total and the population adhered very well to the confinement rules.
The interruption of social relationships, a reduction of physical activities as well as the academic and normal working activities, has caused important disruptions of family routines, with alteration of circadian rhythm (Cellini et al., 2020) and eating habits (Pietrobelli et al., 2020) in all the countries affected by Covid-19. This unfavorable change has negatively affected mental health of the general population, especially of children and adolescents. Recent studies have shown an increase of irritability due to the prolonged boredom times in the general population with rapid swing of mood as well as behavioural problems. (Wang et al., 2020; Cao et al., 2020).
Children and adolescents with attention deficit hyperactivity disorders (ADHD) might be potentially vulnerable to the distress caused by lockdown due to Covid-19 and the European ADHD Guidelines Group alerted for ADHD management during the pandemic period, highlighting this investigation as a field of high priority.
ADHD patients have intolerance for uncertainty, and they face difficulties in following instructions and understanding the complexity of the pandemic situation. Cortese et al., 2020, reported that the enforced condition at home and the unfriendly environment, altering their regular routine, could increase the chances of more severe hyperactivity and impulsive behaviors causing difficulty for the caregivers to engage these children in meaningful activities.
Some studies confirmed the worsening of ADHD symptoms (Zhang et al., 2020), but, on the other hand, other authors reported improvements in restlessness and in the length of time of study in relation to a decrease of distress created by rhythm imposed of scholastic activities (Bobo et al., 2020). The authors stated that intra familiar environmental enforced condition could lead to a relaxation overall for children and adolescents with ADHD that experienced several external stressors.
Studies performed on general population of children and adolescents showed that the pandemic and lockdown had a great impact on emotion and social relationships (Jiao et al., 2020; Lee, 2020). Nevertheless, the understanding of the effect created by lockdown on behavioural and emotional-mood domains in children and adolescents with ADHD poses great challenges based on the following considerations. First, negative mood and behavioural impairment are often expressed by most patients with ADHD with different degrees of severity, independently by the distress caused by Covid-19; as a consequence, we might expect that the impact of confinement on ADHD patients, will be defined by the changes in severity degree with respect to the previous status. Second, considering that the general functioning of children with ADHD is highly dependent on environmental context (Purper-Ouakil et al., 2004), we could expect that children and adolescents emotional- mood and behavioral variations during Covid-19 could represent a critical indicator of the change with respect to previous lifestyle.
Therefore, the aim of the study is to examine the effect of lockdown on children and adolescents with ADHD based on the changes in severity degree of their emotional-mood state and behaviours with respect to previous condition, and to individuate which ADHD patients will result mostly vulnerable to the restriction condition.
2. Methods
2.1. Subjects
An anonymous online survey to be completed by parents was appointed for the study in order to evaluate the effect of the lockdown on emotional-mood states and behaviours of children and adolescents with ADHD. All parents were informed of the survey through the National ADHD Family Association website, for a limited time window (from June 4 to June 21, 2020), targeting patients with ADHD from 5 to 18 years old. The families were in total and partial lockdown for 88 days at the time of the survey.
Before accessing the survey, parents were asked to read the written consent form and to agree to participate in the study. Informed consent represented an obligate field for advancing to the compilation of the questionnaire.
A total of 992 participants (M = 847 (85.4%); F= 145(14.6%) mean age 11.52, S.D .3.17) completed the survey and none of them were excluded.
All ADHD patients were followed and diagnosed by a child and adolescent psychiatrist of the Child and Adolescent Mental Health Services before the survey and the parents provided this information since they were registered in the National ADHD Family Association with a certified ADHD diagnosis. The Italian child and adolescent psychiatrists follow the ADHD Italian guidelines (that reflect international guidelines of the American Academy of Child and Adolescent Psychiatry) for clinical diagnosis and the obligatory protocol of the Italian Superior Health Institute.
The total sample is to be considered as representative for the entire Italian territory with the participation of all regions, 20 metropolitan cities and 78.3% (72/92) Italian provinces. Data reported in this study were part of a wider research project designed with multiple purposes regarding the psychological impact of home confinement in Italy. There was no monetary or credit compensation for participating in the study. The study was approved by the Ethics Committee of the Department of Developmental and Social Psychology Sapienza University and was conducted in accordance with the Declaration of Helsinki (October 2008).
2.2. Procedures
The questionnaire relative to this study included 11 items indicative of most common negative emotional/mood (sadness, boredom, little enjoyment/interest, irritability, temper tantrums, anxiety) and disruptive behavioral problems (verbal and physical aggression, argument, disobedience/opposition, restlessness). We selected 11 questions and format of the items among emotional and behavioural dimensions of validated Italian version of Child Behavior Checklist (CBCL) 6–18 questionnaire (Achenbach and Rescorla, 2000; Frigerio, 2001). We choose these 11 items as the most appropriate to evaluate the psychological and behavioral effect of confinement condition in children and adolescents.
Parents were requested to choose a single response defining severity degree based on the frequency per week by which their children/adolescents expressed each behavioural and emotional-mood dimension (1–2 time/week (low degree); 3–4 time/week (moderate degree); 5–7 time/week (severe degree), absent) before and during the confinement for Covid-19 (Table 1 ).
Table 1.
Survey on emotional-mood and behavioral changes.
Which emotional state and behavioral problems shows your son/daughter before and during the lockdown Covid-19? Sign only one for row.
| Mood-behavioral dimensions | 1–2 times/week | 3–4 times/week | 5–7 times/week | NO |
|---|---|---|---|---|
| He/she shows restlessness | □ | □ | □ | □ |
| He/she shows boredom | □ | □ | □ | □ |
| He/she shows irritability | □ | □ | □ | □ |
| He/she shows Temper tantrum | □ | □ | □ | □ |
| He/she argues polemically with parents | □ | □ | □ | □ |
| He/she is sad | □ | □ | □ | □ |
| He/she shows little enjoyment/interest in activities | □ | □ | □ | □ |
| He/she shows anxiety | □ | □ | □ | □ |
| He/she shows oppositional behaviors | □ | □ | □ | □ |
| He/she shows verbally aggression | □ | □ | □ | □ |
| He/she shows physically aggression | □ | □ | □ | □ |
The questions were repeated in two separated items.
For the transitory period of the confinement (two months in Italy), we have considered that the expression of these problems in terms of frequency/week could be easier for parents in order to evaluate the severity parameter.
3. Statistical analyses
The responses of parents in the single question were modified in categorical variables (1= yes-0 =no) for each of the selected evaluation of severity degree. In order to identify which dimensions increased or decreased in severity under restriction, or which dimensions, not present before the lockdown, were expressed with one of three defined severity degree only during the lockdown (ODL), we have recoded the data of each participant on the base of severity changes with respect to previous condition.
McNemar nonparametric chi square test for dependent samples was performed to compare: 1) each emotional-behavioural dimension with the same severity degree “before-during” lockdown; 2) worsening vs. improvement during the lockdown. Chi square was performed to compare children vs. adolescents on each mood and behavioural dimension.
Statistical significance is set at a nominal two-tail P<.05, unless otherwise specified. Statistical analyses were conducted using SPSS software release 17.0 (SPSS INC, Chicago, Illinois).
3.1. Results
The sample was composed by 528 children [441 M (83.5%); 87 F (16.5%); age range 5–11.11 years; mean age 9.06 y, S.D. 1.63] and 464 adolescents [406 M (87.5%); 58 F (12.5%); age range 12–17.11 years; mean age 14.33 y, S.D.1.92]. No significant gender difference between two age groups was found (χ²=3.130; p=.077).
Family economic status of the whole sample was high in 3%, middle in 75.2% and low in 21.8%. Mothers were the main compiler of the survey (88.6%).
As for the education level the majority of participants have a graduate (29%) or high school degree (52.6%); middle school was represented in 17.9% and elementary school in 0.5%. Moreover, the family composition was reported as follows: parents with one offspring member: 31.3%; parents with two offspring members: 51.9%; parents with three offspring members: 13.3%; parents with four or more offspring members: 3.5%.
Parents reported that 441 ADHD patients were taking medication, while 551 did not take medication before and during the lockdown.
3.1.1. Changes in frequency of each emotional mood and behavioural domain before and during the lockdown
During the lockdown we observed a significant decreased frequency of mood and behavioural problems expressed with low severity degree in both children and adolescents, with the exception of little enjoyment/interest in children and physical aggression in adolescents (Table 2 ). In parallel, under restriction, we found an increase in frequency of the boredom, in temper tantrums and little enjoyment/interest domains expressed with moderate severity degree in both ADHD age groups; moreover, children also showed an increase in percentage of sadness and adolescents in physical aggression. No significant differences were found in both age groups in restlessness, opposition, verbal aggression, argument, irritability and anxiety dimensions.
Table 2.
Comparison of emotional-behavioral dimensions expressed with the same severity degree before and during lockdown in children and adolescents with ADHD.
| Low Before | Low Before | Low During | Low During | Moderate Before | Moderate Before | Moderate During | Moderate During | Severe Before | Severe Before | Severe During | D Severe uring | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NO | YES | NO | YES | χ² | p | NO | YES | NO | YES | χ² | p | NO | YES | NO | YES | χ² | p | ||
| Boredom | C | 377 (71.4%) | 151 (28.6%) | 446 (84.5%) | 82 (15.5%) | 28.720 | .000 | 410 (77.7%) | 118 (22.3%) | 349 (66.1%) | 179 (33.9 | 21.053 | .000 | 447 (84.7%) | 81 (15.3%) | 377 (71.4%) | 151 (28.6%) | 44.226 | .000 |
| A | 345 (74.4%) | 119 (25.6%) | 384 (82.8%) | 80 (17.2%) | 10.090 | .000 | 367 (79.1%) | 97 (20.9%) | 316 (68.1%) | 148 (31.9%) | 20.325 | .000 | 400 (86.2%) | 64/13.8%) | 366 (78.9%) | 98 (21.2%) | 16.500 | .000 | |
| Temper tantrum | C | 382 (72.3%) | 146 (27.7%) | 439 (83.1%) | 89 (16.9%) | 21.930 | .000 | 427 (80.9%) | 101 (19.1%) | 397 (75.2%) | 131 (24.8%) | 5.760 | .016 | 474 (89.8%) | 54 (10.2%) | 446 (84.5%) | 82 (15.5%) | 13.500 | .000 |
| A | 326 (70.3%) | 138 (29.7%) | 381 (82.1%) | 83 (17.9%) | 24.009 | .000 | 387 (83.4%) | 77 (16.6%) | 357 (76.9%) | 107 (23.1%) | 8.087 | .004 | 433 (93.3%) | 31 (6.7%) | 419 (90.3%) | 45 (9.7%) | 4.447 | .035 | |
| Sadness | C | 421 (79.7%) | 107 (20.3%) | 462 (87.5%) | 66 (12.5%) | 12.800 | .000 | 489 (92.6%) | 39 (7.4%) | 454 (86%) | 74 (14%) | 15.413 | .000 | 518 (98.1%) | 10 (1.9%) | 497 (94.1%) | 31 (5.9%) | 14.205 | .000 |
| A | 368 (79.3%) | 96 (20.7%) | 409 (88.1%) | 55 (11.9%) | 18.824 | .000 | 409 (88.1%) | 55 (11.9%) | 397 (85.6%) | 67 (14.4%) | 2.017 | .156 | 450 (97.0%) | 14 (3%) | 445 (95.9%) | 19 (4.1%) | .359* | ||
| Little enjoy/interest | C | 440 (83.3%) | 88 (16.7%) | 460 (87.1%) | 68 (12.9%) | 3.167 | .075 | 482 (91.3%) | 46 (8.7%) | 423 (80.1%) | 105 (19.9%) | 32.038 | .000 | 509 (96.4%) | 19 (3.6%) | 472 (89.4%) | 56 (10.6%) | 24.453 | .000 |
| A | 389 (83.8%) | 75 (16.2%) | 411 (88.6%) | 53 (11.4%) | 5.128 | .024 | 413 (89.0%) | 51 (11.0%) | 386 (83.2%) | 78 (16.8%) | 7.429 | .006 | 443 (95.5%) | 21 (4.5 | 427 (92%) | 37 (8%) | 6.618 | .010 | |
| Restlessness | C | 387 (73.3%) | 141 (26.7%) | 431 (81.6%) | 97 (18.4%) | 12.006 | .001 | 343 (65%) | 185 (35%) | 339 (64.2%) | 189 (35.8%) | .052 | .819 | 413 (78.2%) | 115 (21.8%) | 398 (75.4%) | 130 (24.6%) | 2.613 | .106 |
| A | 320 (69%) | 144 (31%) | 350 (75.4%) | 114 (24.6%) | 5.128 | .024 | 330 (71%) | 134 (28.9%) | 327 (70.5%) | 137 (29.5%) | .030 | .862 | 397 (85.6%) | 67 (14.4%) | 393 (84.7%) | 71 (15.3%) | .155 | .694 | |
| Opposition | C | 425 (80.5%) | 103 (19.5%) | 451 (85.5%) | 77 (14.6%) | 6.010 | .014 | 389 (73.7%) | 139 (26.3%) | 394 (74.6%) | 134 (25.4%) | .139 | .709 | 426 (80.7%) | 102 (19.3%) | 415 (78.6%) | 113 (21.4%) | 1.887 | .170 |
| A | 361 (77.1%) | 103 (22.2%) | 398 (85.8%) | 66 (14.2%) | 12.832 | .000 | 353 (76.1%) | 111 (23.9%) | 347 (74.8%) | 117 (25.2%) | .227 | .634 | 395 (85.1%) | 69 (14.9%) | 389 (83.8%) | 75 (16.2%) | .500 | .480 | |
| Irritability | C | 374 (70.8%) | 154 (29.2%) | 436 (82.6%) | 92 (17.4%) | 24.162 | .000 | 368 (69.7%) | 160 (30.3%) | 361 (68.4%) | 167 (31.6%) | .203 | .652 | 447 (84.7%) | 81 (15.3%) | 424 (80.3%) | 104 (19.7%) | 6.817 | .009 |
| A | 310 (66.8%) | 154 (33.2%) | 354 (76.3%) | 110 (23.7%) | 11.556 | .001 | 346 (74.6%) | 118 (25.4%) | 345 (74.8%) | 119 (25.6%) | .000 | 1.00 | 411 (88.6%) | 53 (11.4%) | 397 (85.6%) | 67 (14.4%) | 2.914 | .088 | |
| Anxiety | C | 427 (80.9%) | 101 (19.1%) | 468 (88.6%) | 60 (11.4%) | 18.391 | .000 | 438 (83%) | 90 (17%) | 434 (82.2%) | 94 (17.8%) | .094 | .759 | 498 (94.3%) | 30 (5.7%) | 477 (90.3%) | 51 (9.7%) | 8.889 | .003 |
| A | 363 (78.2%) | 101 (20.7%) | 403 (86.9%) | 61 (13.1%) | 15.210 | .000 | 382 (82.3%) | 82 (17.2%) | 391 (84.3%) | 73 (15.7%) | .810 | .368 | 435 (93.8%) | 29 (6%) | 425 (91.6%) | 39 (8.4%) | 2.382 | .123 | |
| Verbal aggression | C | 442 (83.7%) | 86 (16.3%) | 468 (88.6%) | 60 (11.4%) | 7.813 | .005 | 434 (82.2%) | 94 (17.8%) | 436 (82.6%) | 92 (17.4%) | .013 | .911 | 483 (91.5%) | 45 (8.5%) | 466 (88.3%) | 62 (11.7%) | 5.224 | .022 |
| A | 371 (80%) | 93 (20%) | 401 (86.4%) | 63 (13.6%) | 10.782 | .001 | 380 (81.9%) | 84 (18.1%) | 374 (80.6%) | 90 (19.4%) | .321 | .571 | 428 (92.2%) | 36 (7.8%) | 417 (89.9%) | 47 (10.1%) | 3.226 | .072 | |
| Argument | C | 400 (75.8%) | 128 (24.2%) | 445 (84.3%) | 83 (15.7%) | 11.877 | .000 | 388 (73.5%) | 140 (26.5%) | 370 (70.1%) | 158 (29.9%) | 1.389 | .239 | 452 (85.6%) | 76 (14.4%) | 418 (79.2%) | 110 (20.8%) | 7.669 | .006 |
| A | 329 (70.9%) | 135 (29.1%) | 380 (81.9%) | 84 (18.1%) | 15.528 | .000 | 326 (70.3%) | 138 (29.7%) | 335 (72.2%) | 129 (27.8%) | .362 | .548 | 403 (86.9%) | 61 (13.1%) | 367 (79.1%) | 97 (20.9%) | 10.560 | .001 | |
| Physical aggression | C | 442 (83.7%) | 86 (16.3%) | 462 (87.5%) | 66 (12.5%) | 4.628 | .031 | 481 (91.1%) | 47 (8.9%) | 473 (89.6%) | 55 (10.4%) | .875 | .350 | 505 (95.6%) | 23 (4.4%) | 492 (93.2%) | 36 (6.8%) | .011* | |
| A | 403 (86.9%) | 61 (13.1%) | 405 (87.3%) | 59 (12.7%) | .019 | .890 | 436 (94%) | 28 (6%) | 422 (90.9%) | 42 (9.1%) | 4.694 | .030 | 453 (97.6%) | 11 (2.4%) | 457 (98.5%) | 7 (1.5%) | .388* |
using binomial distribution C=children; A= adolescents.
During the lockdown, children and adolescents with ADHD with high severity degree showed a different trend: we found in children an increase in percentage in almost all dimensions with the exception of restlessness and opposition while in adolescents we observed an increased percentage only in boredom, temper tantrums, little enjoyment/interest and argument.
3.1.2. Changes in severity degree of emotional - mood and behaviours dimensions during the lockdown
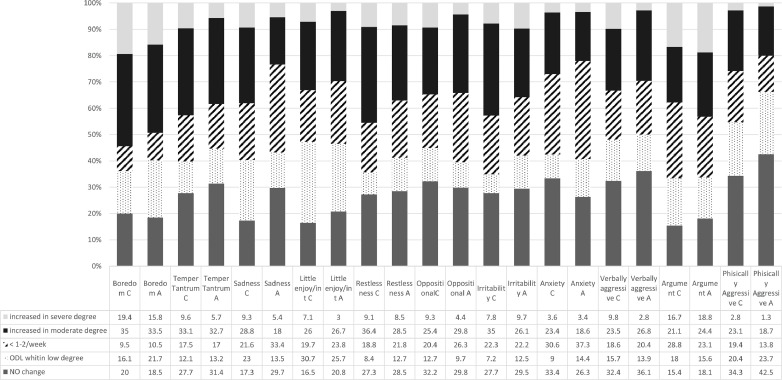
Children and adolescents with ADHD with previously low severity degree showed the lowest percentage of stability (no change) before-during the lockdown with significant fluctuations toward moderate and severe degree in all the dimensions, mainly in boredom, temper tantrums, little enjoyment/interest, argument, restlessness, irritability and sadness (Fig. 1 ). During the lockdown, these fluctuations contribute to explain either the decrease or the increase of frequencies in examined domains in ADHD patients with low and with high severity degrees, observed in the comparative analyses in Table 2. Moreover, we found a percentage > 20% of children and/or adolescents with ADHD that started to express little enjoyment/interest and physical aggression, and sadness and boredom with low severity degree during the lockdown (Fig. 1).
Fig. 1.
Changes in Children and Adolescents with Low Severity Degree
% of Children (C) and Adolescents (A) with previous low degree that maintained (no change), increased or lowered their severity degree or started to express emotional-mood behavioural problems with low severity degree (ODL) during lockdown.
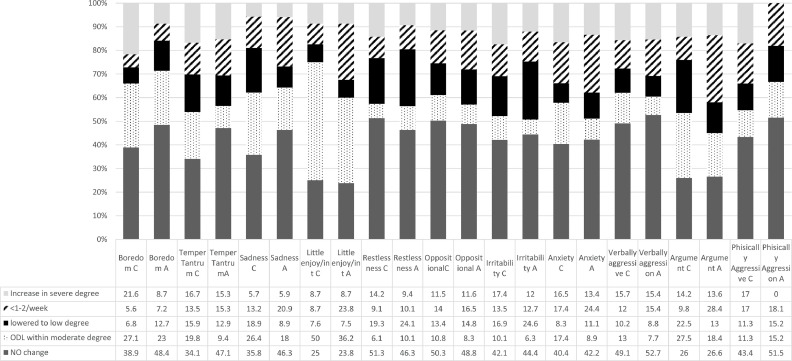
Children and adolescents with ADHD with moderate degree showed more stability (no change) before-during the lockdown; nevertheless, we also registered a change toward the lower severity degree in all the dimensions with the exception of boredom among children. Moreover, we continued to find a percentage around 20% of children and/or adolescents that, during the lockdown, started to express boredom, sadness, argument and overall little enjoyment/interest with moderate severity degree (Fig. 2 ).
Fig. 2.
Changes in children and adolescents with moderate severity degree. % of Children (C) and Adolescents (A) with previous moderate degree that maintained (no change), increased or lowered their severity degree or started to express emotional-behavioural problems with moderate severity degree (ODL) during lockdown.
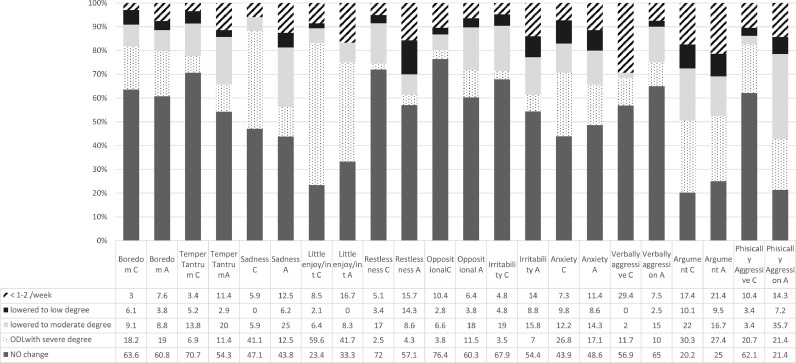
Children and adolescents with high severity degree reported the major stability before-during lockdown with rates between 52% and 72% in boredom, temper tantrum, restlessness oppositional and verbal aggression and, in physical and verbal aggression behaviours among children and adolescents respectively. In parallel, in children and adolescents that have a severe degree, only during the lockdown (ODL), we observed a trend toward a lower severity in all dimensions but boredom, little enjoyment/interest and, only among children, sadness (Fig. 3 ).
Fig. 3.
Changes in children and adolescents with high severity degree. % of Children (C) and Adolescents (A) with previous high severity degree that maintained (no change), lowered their severity degree or started to express affective-behavioural problems with severe degree (ODL) during lockdown.
When we compared worsening and improvement relative to each domain during the lockdown, children and adolescents with previous low severity degree, showed significant worsening in almost all dimension with exception of anxiety and, only among adolescents, of sadness. In particular, boredom and little enjoyment/interest and temper tantrum and irritability showed a difference in percentage between worsening-improvement > 30% until 50% in both age groups. Moreover, a difference in percentage >30% was found in sadness and restlessness and verbal aggression among children and in argument among adolescents (Table 3 ). Under restriction, children and adolescents with previous moderate severity expression continued to report high rates of worsening in boredom and little enjoyment/interest, although with significant values only among children. Moreover, adolescents showed significant higher rates of improvement in restlessness and irritability.
Table 3.
Comparison of worsening and improving within and between children and adolescents during the lockdown.
| Previous low severity degree | Children vs. adolescents | Previous moderate severity degree | Children vs. adolescents | Previous high severity degree | Children vs. adolescents | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Improving N (%) | WorseningN (%) | χ² | p | χ² | p | ImprovingN (%) | Worsening N (%) | χ² | p | χ² | p | Improving N (%) | Worsening N (%) | χ² | p | χ² | p | ||
| Boredom | C | 17 (9.5%) | 127 (70.5%) | 82.507 | .000 | .112 | .946 | 20 (12.4%) | 79 (48.7%) | 33.980 | .000 | 10.338 | .006 | 18 (18.2%) | 18 (18.2%) | .000 | 1.000 | .025 | .988 |
| A | 16 (10.5%) | 108 (71%) | 66.782 | .000 | 25 (19.9%) | 40 (31.7%) | 3.015 | .082 | 16 (20.2%) | 15 (19%) | .000 | 1.000 | |||||||
| Temper tantrums | C | 29 (17.5%) | 91 (54.8%) | 31.008 | .000 | .093 | .955 | 37 (29.4%) | 46 (36.5%) | .771 | .380 | 8.789 | .012 | 13 (22.4%) | 4 (6.9%) | .049* | .050 | .975 | |
| A | 27 (17%) | 82 (51.6%) | 26.752 | .000 | 24 (28.2%) | 21 (24.7%) | .089 | .766 | 12 (34.3%) | 4 (11.4%) | .077* | ||||||||
| Sadness | C | 30 (21.6%) | 85 (61.1%) | 25.357 | .000 | 12.934 | .002 | 17 (32.1%) | 17 (32.1%) | .000 | 1.000 | .873 | .646 | 2 (11.8%) | 7 (41.1%) | .180* | 5.655 | .061 | |
| A | 37 (33.4%) | 41 (36.9%) | .115 | .734 | 20 (29.8%) | 16 (23.9%) | .250 | .617 | 7 (43.8%) | 2 (12.5%) | .180* | ||||||||
| Little enjoy/int | C | 25 (19.7%) | 81 (63.8%) | 28.538 | .000 | 2.254 | .324 | 15 (16.3%) | 54 (58.7%) | 20.928 | .000 | 5.632 | .060 | 8 (17%) | 28 (59.6%) | 10.028 | .002 | 2.773 | .250 |
| A | 24 (23.8%) | 56 (55.4%) | 12.013 | .001 | 25 (31.3%) | 36 (44.9%) | 1.639 | .200 | 9 (25%) | 15 (41.7%) | . | .307* | |||||||
| Restlessness | C | 29 (18.8%) | 83 (53.9%) | 25.080 | .000 | 3.074 | .215 | 56 (28.4%) | 40 (20.3%) | 2.344 | .126 | .685 | .710 | 30 (25.5%) | 3 (2.5%) | 20.485 | .000 | 034 | .983 |
| A | 36 (21.8%) | 82 (49.7%) | 17.161 | .000 | 51 (34.2%) | 29 (19.5%) | 5.513 | .019 | 16 (38.6%) | 3 (4.3%) | 17.633 | .000 | |||||||
| Opposition | C | 24 (20.4%) | 56 (47.4%) | 12.013 | .001 | 1.808 | .405 | 43 (27.4%) | 35 (22.3%) | .628 | . 428 | 939 | .625 | 21 (19.8%) | 4 (3.8%) | .001 | 3.065 | .216 | |
| A | 30 (26.3%) | 50 (43.9%) | 4.513 | .034 | 38 (31.3%) | 24 (19.9%) | 2.726 | .099 | 22 (28.2%) | 9 (11.5%) | 4.645 | .031 | |||||||
| Irritability | C | 37 (22.3%) | 83 (50%) | 16.875 | .000 | 2.138 | .303 | 54 (30.4%) | 49 (27.5%) | .155 | .693 | 6.947 | .0.31 | 24 (28.6%) | 3 (3.5%) | 14.815 | .000 | .329 | .848 |
| A | 39 (22.2%) | 85 (48.3%) | 16.331 | .000 | 47 (37.3%) | 23 (18.3%) | 7.557 | .006 | 22 (38.6%) | 4 (7%) | 11.115 | .001 | |||||||
| Anxiety | C | 34 (30.6%) | 40 (36%) | ,338 | .561 | 4.415 | .110 | 28 (25.7%) | 37 (33.9%) | .985 | .321 | 4.198 | .123 | 12 (29.3%) | 11 (26.8%) | 1.000* | 1.006 | .605 | |
| A | 44 (37.3%) | 43 (36.4%) | .000 | 1.000 | 32 (35.5%) | 20 (22.3%) | 2.327 | .127 | 12 (34.3%) | 6 (17.1%) | .238* | ||||||||
| Verbal aggression | C | 19 (18.6%) | 50 (49%) | 13.043 | .000 | .984 | .612 | 24 (22.2%) | 31 (28.7%) | .655 | .418 | .811 | .667 | 16 (31.4%) | 6 (11.7%) | .052* | .940 | .625 | |
| A | 22 (20.4%) | 47 (43.5%) | 8.348 | .004 | 22 (24.2%) | 21 (23.1%) | .000 | 1.000 | 10 (25%) | 4 (10%) | .180* | ||||||||
| Argument | C | 45 (28.8%) | 87 (55.8%) | 12.735 | .000 | 2.377 | .305 | 66 (32.3%) | 85 (41.7%) | 2.146 | .143 | 4.832 | .089 | 54 (49.5) | 33 (30.3%) | 4.598 | .032 | 1.649 | .438 |
| A | 37 (23.1%) | 94 (58.8%) | 23.939 | .000 | 70 (41.4%) | 54 (32%) | 1.815 | .178 | 40 (47.6%) | 23 (27.4%) | 4.063 | .044 | |||||||
| Physical aggression | C | 21 (19.4%) | 50 (46.3%) | 11.042 | .001 | 3.395 | .183 | 15 (28.3%) | 15 (28.3%) | .000 | 1.000 | 4.146 | .126 | 5 (17.2%) | 6 (20.7%) | 1.000* | 1.793 | .408 | |
| A | 11 (13.8%) | 35 (43.7%) | 11.500 | 0.001 | 11 (33.3%) | 5 (15.2 | .210* | 8 (57.2%) | 3 (21.4%) | 0.227* | |||||||||
using binomial distribution C=children; A= adolescents. Worsening includes also ODL.
Children and adolescents with previous severe degree, during the lockdown, showed a significant improvement in opposition, restlessness irritability and argument; however, they continued to report higher rates of worsening in little enjoyment/ interest and equivalent rates of worsening-improvements in boredom.
Inter-ADHD age groups comparison showed a significant difference in sadness among children with low severity degree while those with moderate degree reported high percentage in boredom and temper tantrum and irritability than adolescents.
4. Discussion
The current study in ADHD patients, aimed to examine the impact of the lockdown on emotional-mood and behavioural domains based on changes in severity degree with respect to previous condition and to individuate ADHD patients who resulted more vulnerable to lockdown experience.
During the lockdown, a first evidence of the study consists in finding different profiles of the emotional-mood states and behavioural dimensions among ADHD patients with distinct severity degree. These differences were found either in the percentage of stability of degree before-during the lockdown than in the changes. During the lockdown, ADHD with low severity degree in the mood-behavioral domains showed the least before-during stability, the largest scale of fluctuation and significant worsening in almost examined domains. The understanding of this general worsening would require further investigations, although emotional lability and mood instability, and adaptive dis-functioning are closely associated and common features reported among ADHD patients (Anastopoulos et al., 2011; Barkley andFischer, 2010; Brotman et al., 2006; Sobansky et al., 2010).
Because similar results were reported in Lee et al. (2020) study on children and adolescents during the lockdown, it is presumable that the sudden interruption of friendly relationships or of the opportunities of pleasant activities, in patients with lower dis-functioning, could have caused a critical adaptation problem with consequent outbreaks of emotional-mood status and of the behaviours. In general, these results support the consideration that excessive and rapid changes, in affective–motivation–arousal, and/or behaviors represent a critical expression of distress to environmental mismatch independently by age and by mental health state.
Conversely, ADHD patients with high and moderate severity degree, although maintained a higher stability of their severity degree before and during the lockdown, showed important rates of improvement in several emotional mood and behavioural dimensions. Due to fact that similar results were found in both age ADHD groups, they suggest that the restriction could have represented, for some children, a protective condition from common social stressors, such as fewer friendships, bullying, victimization, and rejection of peers (Hoza, 2007; Nijmeijer et al., 2008) or school time constraints (Bobo et al., 2020; Chawal et al., 2020). The findings, in confirming the strong relationship between severity degree and stability of behavioural impairment, highlighted that these ADHD patients are improvable when environmental context is more flexible and responsive.
Our results are consistent with those of Zhang et al. (2020), that reported significant relationship between improvements in the online study at home with longer time of study and a decrease of ADHD symptoms.
To a closer exam relative to each domain, the findings highlighted that, the lockdown has overall caused, in both age groups, a worsening of boredom, in particular among ADHD patients with low and moderate severity, and of the enjoyment/interest, independently by severity degree, although with significant results exclusively among children. The first finding was expected because boredom is closely linked to ADHD condition, susceptible to important fluctuations as well as a critical hallmark of distress caused by environmental condition. The results are consistent with previous studies (Zhang et al., 2020), that reported a positive association between negative mood states and worsening of ADHD symptoms during the lockdown. Nevertheless, the co-occurrence of boredom and little enjoyment/interest in activities oriented versus a closer relation to lockdown condition. It is reported that the lockdown has caused a significant increased difficulty in keeping track of time (Cellini et al., 2020) providing prolonged boredom times (Cao et al., 2020; Wang et al., 2020).
The psychological perception of the time is usually marked by the duration of the activities, by the variability of information and stimulations, by dynamic environments and contextual changes. In agreement with our findings, it is well documented that the reduction of pace of time promotes an increase of boredom and of the under-motivation state, sometime associated to a general decrease of well-being reflecting on adaptive behaviors. (DanZakai, 2014). The high percentage of ADHD in both age groups that, only during the lockdown, showed boredom and little enjoyment/interest, confirms these domains as the most affected by the restriction. In particular, among children, little enjoyment/interest was the only mood dimension that significantly worsened independently by severity degree. Conversely, despite the risk of Covid-19 infection and according with some studies (Bobo et al., 2020), ADHD patients didn't result particularly affected by anxiety in both age group and, independently by severity degree, showed equivalent rates between worsening and improving. With the exception of ADHD patients with low severity degree, we registered the highest rates in stability degree before-during the lockdown in physical and verbal aggression, oppositional behaviours, and restlessness and an important percentage of patients of both age groups that started to express argument with significant severity parameters, during the lockdown. According with other studies (Bobo et al., 2020), our findings confirmed that the condition of restriction could promote conflict within family environment.
To a general examination, the trend of worsening and improving was substantially similar in both age groups, although children resulted more susceptible to mood fluctuations than adolescents did. It is well documented that ADHD patients showed less flexibility in the use of coping strategies for dealing with stressful situations than control subjects as shown by Babb et al. (2010). The same authors reported a higher coping flexibility in older (10–11 years) vs. younger (7–8 years) typically developing children while this difference was not found in ADHD children with the same age. Since studies show a developmental delay of brain areas implied in the executive functioning among children with ADHD (Shaw et al., 2007) we can assume that the difference in coping flexibility might become evident at later ages. Therefore, the mood patterns differences found between children and adolescents with ADHD in our sample could be linked to the higher flexibility of adolescents in the use of emotional coping strategies.
Considering the representativeness of the sample, these findings represent an important goal of the study, in defining ADHD emotional-mood and behavioural responses to distress caused lockdown.
5. Conclusion
The current approach provided a punctual individuation of domains affected and the indirect benefits produced by restriction condition in children and adolescents with ADHD. In view of reinstatement of regular routine, the major challenge after the pandemic will be to deal with its sequelae, also considering the risk of going back to previous severity condition in patients that improved during the lockdown.
Moreover, it is our opinion that these findings could provide implication for the clinical practice and interventions independently from the specific aim of the study.
The current study has some limitations that must be acknowledged. Although the survey was conducted after few days the end of lockdown and in condition of ongoing yet restriction, we cannot exclude a memory bias of the parents. We have not evaluated the relationship between impairment of the examined domains and ADHD severity, focusing on the problems reported as most concerning for parents. Moreover, we did not examine the relationship with the medication status, since parents did not answer to a specific question about the access to medication during the lockdown. Another limitation is that we did not include the ADHD diagnosis of parents as covariate/confounder in our analyses. Finally, considering the richness of the survey, we decided to select 11 items of the CBCL, as the most appropriate to evaluate the psychological and behavioral effect of confinement condition, in order to ensure the best return rate.
Future extensions of the present study will allow to uncover the relationships with acute stress symptoms, with the comorbidity profiles of the ADHD patients, as well strategies adopted by parents to manage the child-adolescent's problems.
Authorship responsibility
Each author made a substantive intellectual contribution to the study.
-
•
Maria Grazia Melegari: conceptualization and study design; data collection and interpretation; preparation and revision of the manuscript; approved the final manuscript as submitted
-
•
Martina Giallonardo: data collection and interpretation; revision of the manuscript; approved the final manuscript as submitted.
-
•
Roberto Sacco: data analysis and revision of the manuscript; approved the final manuscript as submitted.
-
•
Lavinia Marcucci: data collection, preparation and revision of the manuscript; approved the final manuscript as submitted
-
•
Silvia Orecchio: data collection; preparation and revision of the manuscript; approved the final manuscript as submitted.
-
•
Oliviero Bruni: conceptualization and study design, data collection, interpretation; revision of the manuscript; approved the final manuscript as submitted.
Funding
The authors received no financial support for the research, authorship, and/or publication for this article.
Declaration of Competing Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments
The authors gratefully acknowledge the Italian President of Family Association of ADHD (AIFA), Patrizia Stacconi, all Regional referents and parents who have participated to this study.
References
- Achenbach T.M., Rescorla L.A. University of Vermont, Research Center for Children, Youth & Families; Burlington: 2000. Manual for the ASEBA Preschool Forms & Profiles. [Google Scholar]
- Anastopoulos A.D., Smith T.F., Garrett M.E., Morrissey-Kane E., Schatz N.K., Sommer J.L., et al. Self-regulation of emotion, functional impairment, and comorbidity among children with AD/HD. J. Atten. Disord. 2011;15(7):583–592. doi: 10.1177/1087054710370567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babb K.A., Levine L.J., Arseneault J.M. Shifting gears: coping flexibility in children with and without ADHD. Int. J. Behav. Dev. 2010;34(1):10–23. doi: 10.1177/0165025409345070. [DOI] [Google Scholar]
- Barkley R.A., Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J. Am. Acad. Child Adolesc. Psychiatry. 2010;49(5):503–513. doi: 10.1097/00004583-201005000-00011. [DOI] [PubMed] [Google Scholar]
- Bobo E., Lin L., Acquaviva E., Caci H., Franc N., Gamon L., Picot M.-.C., Pupier F., Speranza M., Falissard B., Purper-Ouakil D. How do children and adolescents with attention deficit hyperactivity disorder (ADHD) experience during the COVID-19 outbreak? Encephale J. 2020;46(3S):S85–S92. doi: 10.1016/j.encep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman M.A., Schmajuk M., Rich B.A., Dickstein D.P., Guyer A.E., Costello E.J., Egger H.L., Angold A., Pine D.S., Leibenluft L. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol. Psychiatry. 2006;60(9):991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cellini N., Canale N., Mioni G., Costa S. Changes in sleep pattern, sense of time and digital media use during Covid-19 lockdown in Italy. J. Sleep Res. 2020 doi: 10.1111/jsr.13074. 22 April. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chawla N., Sharma P., Sagar R. Psychological impact of COVID-19 on children and adolescents: is there a silver lining? Indian J. Pediatr. 2020 doi: 10.1007/s12098-020-03472-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortese S., Asherson P., Sonuga-Barke E., Banaschewski T., Brandeis D., Buitelaar J., Coghill D., Daley D., Danckaerts M., Dittmann R.W., Doepfner M., Ferrin M., Hollis C., Holtmann M., Konofal E., Lecendreux M., Santosh P., Rothenberger A., Soutullo C., Simonoff E. ADHD management during the COVID-19 pandemic: guidance from the European ADHD guidelines group. Lancet Child Adolesc. Health. 2020;4(6):412–414. doi: 10.1016/S2352-4642(20)30110-3. Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DanZakay Psychological time as information: the case of boredom. Front. Psychol. 2014 doi: 10.3389/fpsyg.2014.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frigerio A. Istituto Scientifico “E. Medea”, Assoc. “La Sacra Famiglia.”; Bosisio Parini, Italy: 2001. ASEBA (Achenbach System of Empirically Based Assessment) Questionario sul Comportamento Del Bambino [Questionnaire On Child Behaviour] [Google Scholar]
- Hoza B. Peer functioning in children with ADHD. J. Pediatric Psychol. 2007;Vol 32(Issue 6):655–663. doi: 10.1093/jpepsy/ism024. [DOI] [PubMed] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020;221:264–266. doi: 10.1016/j.jpeds.2020.03.013. 2020 June 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. 2020. Lancet Child. Adolesc. Health. 2020;4(6):421. doi: 10.1016/S2352-4642(20)30109-7. 2020 Jun. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijmeijer J.S., Minderaa R.B., Buitelaar J.K., Mulligan A., Hartman A., Hoekstra P.J. Attention-deficit/hyperactivity disorder and social dysfunctioning. Clin. Psychol. Rev. 2008;Vol. 28(Issue 4):692–708. doi: 10.1016/j.cpr.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Pietrobelli A., Pecoraro L., Ferruzzi A., Mooseong H., Faith M., Zoller T., Antoniazzi F., Piacentini G., Fearnbach S.N., Heymsfield S.B. (2020) Effect of Covid-19 lockdown on lifestyle. behaviors in children with obesity living in Verona, Italy: a longitudinal study. doi:10.1002/oby.22861 (an article not yet in an issue). [DOI] [PMC free article] [PubMed]
- Purper-Ouakil D., Wohl M., G., Mouren M.C., Gorwood P. Symptom variations in ADHD: importance of context, development and comorbidity. Encephale. 2004;30(6):533–539. doi: 10.1016/s0013-7006(04)95467-x. [DOI] [PubMed] [Google Scholar]
- Shaw P., Eckstrand K., Sharp W., Blumenthal J., Lerch J.P., Greenstein D., Clasen L., Evans A., Giedd J., Rapoport J.L. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc. Natl. Acad. Sci. U.S.A. 2007;104(49):19649–19654. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobanski E., Banaschewski T., Asherson P., Buitelaar J., Chen W., Franke B., Holtman M., Krumm B., Sergeant J., Sonuga-Barke E., Strigaris A., Taylor E., Anney R., Ebstein R.P., Gill M., Miranda A., Mulas F., Oades R.D., Roeyers H., Rothenberg A., Steinhausen H.C., Faraone S.V. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J. Child Psychol. Psychiatry. 2010;51(8):915–923. doi: 10.1111/j.1469-7610.2010.02217.x. [DOI] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F., The Lancet Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lond. Engl. 2020;2020(395):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Shuai L., Yu H., Wang Z., Qiu M., Lu L., Cao X., Xia W., Wang Y., Chen R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatry. 2020;51:10207-7. doi: 10.1016/j.ajp.2020.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]