Graphical abstract
Keywords: High-performance polymer; PEKK; Dental implants; Restorations, dental; Prosthodontics
Abstract
Polyetherketoneketone (PEKK) is a new evolving polymeric material. The present article comprehensively reviewed an overview of various applications of PEKK in prosthodontics and oral implantology, highlighting its prospects for clinical applications. PEKK biomaterials is an elastic material with good shock absorbance and fracture resistance and present ultra-high performance among all thermoplastic composites for excellent mechanical strength, chemical resistance, and high thermal stability. Available articles on PEKK for dental applications were reviewed from January 1957 to August 2020) using MEDLINE/PubMed, Web of Science, and ScienceDirect resources. PEKK presents suitable physical, mechanical, and chemical properties for applications in prosthodontics and oral implantology. PEKK has good potential for a wide range of dental applications, including tooth restorations, crowns, bridge, endoposts, denture framework, implant-supported fixed prosthesis, and dental implants. PEKK dental implants have shown lesser stress shielding compared to titanium for dental implant applications. Further modifications and improving material properties can result in broader applications in the field of dentistry. Long term evaluations are needed as PEKK is recently applied in dentistry, and there are limited studies published on PEKK.
Introduction
Polymers being one of the essential materials in dentistry, poses excellent physical, mechanical properties and are reported to have excellent biocompatibility. Various removable appliances, restorations, and denture base materials are fabricated from polymers [1], [2]. Polyetherketoneketone (PEKK) is a new polymeric material that has attracted the attention of researchers because of its excellent properties that can be used in many applications [3]. The PEKK is a methacrylate-free thermoplastic high-performance material [4]. PEKK was firstly introduced by Bonner in 1962 [5], and since then, it has been used for different industrial and military purposes [6]. Recently, PEKK has increasingly used as a biomaterial with properties suitable for dental and medical applications [7]. The PEKK has a wide range of applications in restorative, prosthetic, and implant dentistry. The PEKK is a promising material in the field of cranial and orthopedic implants. Their wide biomedical applications are because of its higher mechanical strength and the presence of the second ketone group that allows for more surface modification of its surface.
The PEKK and polyetheretherketone (PEEK) are the two most well-known of the polyaryletherketone (PAEK) family. The PAEK family are thermoplastic polymers and have been in the engineering field since the 1980s and shows excellent mechanical properties and chemical resistance [8]. PAEK family show ultra-high performance (superior mechanical performances with chemical resistant) among all thermoplastic composites linked to their processing parameters (Fig. 1A) [4]. The PEEK emerged in the late 1990s as a semi-crystalline material and showed excellent biological, mechanical, and physical properties for biomedical applications [9], [10]. Promising applications of PEEK biomaterial are dental implant [3], temporary abutment and fixed prosthesis [11] and removable denture [12], and finger prosthesis [13]. These incredible outcomes of PEEK as dental materials attracted the attention of researchers to study the other members of the PAEK family, PEKK. Available articles on PEKK for dental applications were reviewed from January 1957 to August 2020) were reviewed using MEDLINE/PubMed, Web of Science, and ScienceDirect resources. This article presents an overview of PEKK and its various applications in restorative, prosthetic, and implant dentistry.
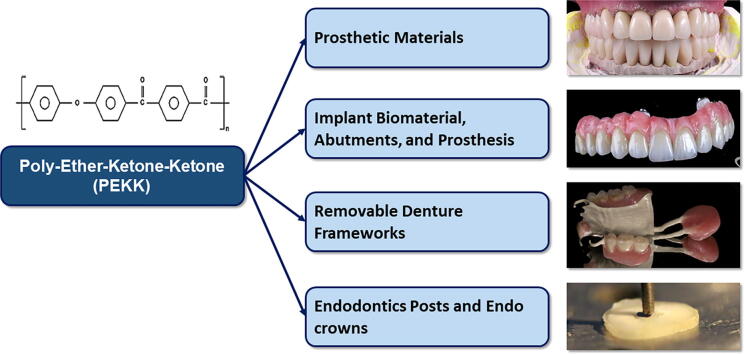
Fig. 1.
Structure and performance of PAEK (PEKK and PEEK), and fabrication of PEKK. (A) Performance of PAEK; (B) Structures of PAEK; (C) Production of PEKK by electrophilic substitution using nitrobenzene and aluminum chloride (AlCl3). PAEK = Polyaryletherketone, PEEK = Polyetheretherketone, PEKK = Polyetheretherketone, PPS = Polyphenylene sulfide, PAI = Polyamideimide, PES = Polyethersulfone, PEI = Polyethylenimine, POM = Polyoxymethylene, PC = Polycarbonates, PA = polyamide, PMMA = Polymethyl methacrylate.
Structure and synthesis of PEKK
The PAEK is a linear aromatic polyether ketone represented by ultrahigh molecular weight polyethylene. The structure of PEEK and PEKK have aromatic rings, which differ in the ratio of ether- and keto- group (Fig. 1B) [11]. There are some differences between PEKK and PEEK. PEKK has a second ketone group, and it increases polarity and backbone rigidity, which results in an increase in glass transition and melting temperature [14]. Moreover, PEKK displays both amorphous and crystalline behavior, and different products can be produced. A PEKK with 60% straight and 40% kinked segments melts at 305 °C but PEEK with 80% straight and 20% kinked melts at 360 °C. In addition, the extra ketone group in PEKK has strong polymer chains and shows better physical and mechanical properties, such as compressive strength [15].
PEKK is a liner thermoplastic polymer and consists of a benzene ring attached consecutively by ether or ketone- groups (Fig. 1B) [10]. PEKK can be produced from diphenyl ether and iso- and terephthaloyl chlorides with aluminum chloride (AlCl3) and nitrobenzene (Fig. 1C) [14].
Properties of PEKK
Physical and mechanical properties
PEKK shows excellent physical and mechanical properties, such as melting temperature and compressive strength in comparison to other polymeric materials [15]. In comparison to PEEK (pure and glass-reinforced), PEKK shows better mechanical properties in terms of flexure, tensile, and compressive strength [16]. Pekkton® ivory (Cendres + Métaux, SA, Switzerland), a product of PEKK has 80% higher compressive strength compared to un-reinforced PEEK [17]. The addition of titanium dioxide (TiO2) in PEKK, increases the hardness and wear resistance [18].
The shock absorbance with suitable strength (65 MPa) and fracture resistance properties of PEKK raises the possibility of using it as restorative material [19], [20]. The PEKK has similar compression strength with a lesser modulus of elasticity compared to dentin [20]. Similar to PEEK, the elastic modulus of PEKK is comparable to those of bone. Hence, PEKK can be used as a dental implant biomaterial for excellent mechanical properties and better stress distribution (Table 1, Table 2). Recently, Alsadon et al. evaluated the fatigue behavior of PEKK bilayered crowns in comparison to zirconia and nickel chromium-based crowns [16]. The fatigue limit of PEKK (754 N) was reported remarkably higher compared to zirconia (422 N), and nickel-chromium (586 N). Similarly, the fatigue limit of PEKK composite veneered molar crowns is also comparable with the cobalt-chromium and polymethylmethacrylate (PMMA) (750 N). According to Burke’s classification, the fracture code of PEKK was distributed between code one and two while Zr and NiCr exhibited code one and distribution between code 1 and 4, respectively, when subjected to loading below the group’s fatigue limit [16].
Table 1.
Comparison of mechanical properties between PEKK and some human structures.
Table 2.
Mechanical properties of PEKK and other prosthetic materials.
| Properties | PEEK | PEKK | Titanium | PMMA | Reference |
|---|---|---|---|---|---|
| Tensile strength (MPa) | 100.69 | 115 | 240–890 | 48–62 Mpa | [24] |
| Elastic modulus (GPa) | 3.5 | 5.1 | 103–114 | 3.8 × 103 | [24] |
| Flexural strength (MPa) | 163.88 | 200 | 65 | 107–117 | [3], [23], [24] |
| Compressive strength (MPa) | 118–169 | 246 | 130–170 | 76 Mpa | [24] |
| Melting temperature (°C) | 334–350 | 363–386 | 1650–1670 | 160 | [24], [25] |
| Hardness | 26–29 VHN | 252 MPa | 90 VHN | 89–95 MPa | [24] |
| Water absorption (µg/mm3) | 0.1–0.5 | 8.7 | 0.04 | 0.1–0.3 | [24], [26] |
| Density (g/cm3) | 1.3 | FEFF1.3 | 4.4–4.5 | 1.16–1.18 g/cc | [24] |
Biological properties
PEKK shows excellent biocompatibility and has been introduced as promising alternative material for long-term orthopedic applications over titanium [10], [13], [27]. It has been approved by the FDA for oro-maxillofacial and spinal surgery [28]. In addition, PEEK is being used extensively in dentistry as a prosthetic and implant biomaterial. It offers metal-free restorations and helpful in patients with allergies [19].
As implant material, Yuan et al. [29] investigated osteointegration in PEKK in terms of chemistry and surface microstructure. It was reported that the other ketone group in PEKK increases the ability of surface chemical modification. With more ketone groups, the presence of -SO3H will be more on PEKK than PEEK. This leads to complex surface topography, greater surface area, and micro rough surface, which will affect the cell behavior and osteointegration on the surface of PEKK [30]. The surface modification by increasing the porosity and incorporation of HA had a positive impact on the osteointegration property [29]. Bioactive PAEK material can be achieved by modifying the surface using various bioactive ceramic such as beta-tricalcium phosphate (β-TCP), hydroxyapatite (HA), and bioactive glasses (BG). Converse et al. [31] used a combination of different methods that include compression molding, particle leaching, and powder processing to develop a HA whisker reinforced porous PEKK. In comparison to uncoated PEEK, Walsh et al. reported that coating PEEK using plasma-sprayed titanium improved the histological and mechanical properties of the bone- implant interface after implantation [32].
Regarding antibacterial activity, according to Wang [7], PEKK shows less bacterial adhesion on its surface compared to the orthopedic industry PEEK. The adherence Staphylococcus epidermidis were 37% less on the surface of PEKK. After five days of culture, they found around 50% decrease in the attachment and growth of Pseudomonas aeruginosa on PEKK compared to PEEK without using antibiotics. Also, Moore et al. [33] found the less inflammatory response from PEKK compared to PMMA in a rat study.
Applications of PEKK in dentistry
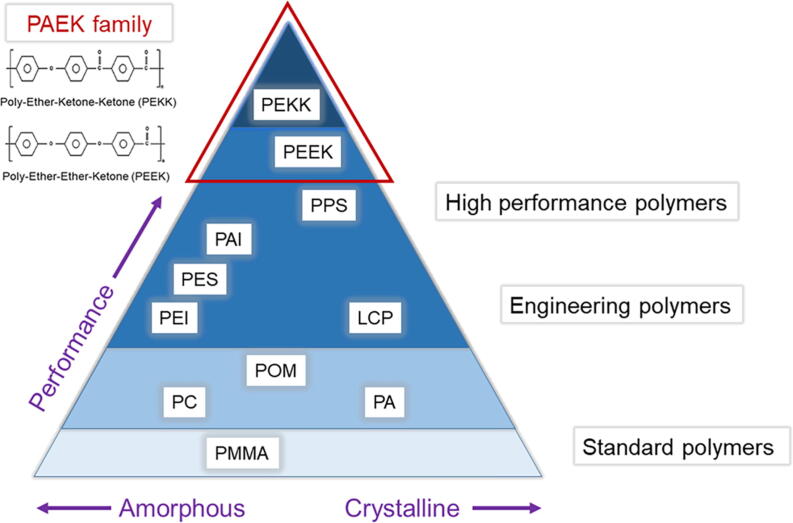
The PEKK has been successfully used in dentistry as a prosthetic and implant biomaterial. Recently, PEKK has been applied in various areas of dentistry due to suitable mechanical, fracture resistance, shock-absorbing, and better stress distribution [17], [34], [35], [36], [37]. The PEKK has excellent biocompatibility as it offers metal-free restorations, and it is considered as an alternative to metal and ceramics [19]. Fig. 2 shows the various applications of PEKK in dentistry.
Fig. 2.
Current and potential applications of PEKK in dentistry.
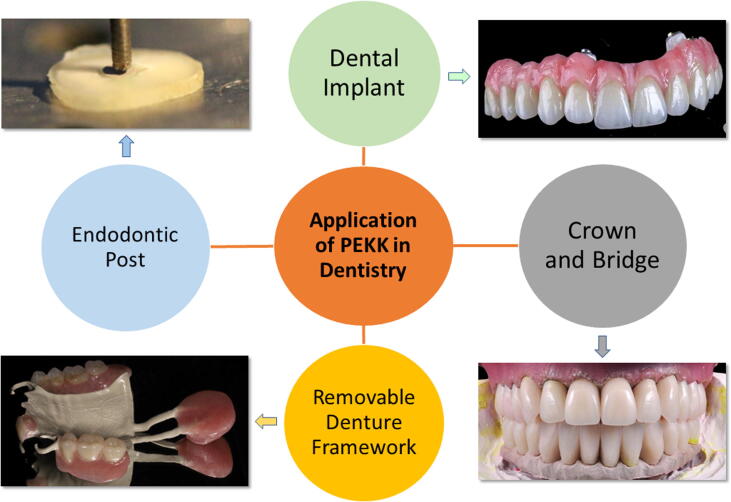
PEKK as a prosthetic material
The PEKK has low density, low elastic modulus, high strength, and acceptable wear resistance. It can be a potential material for application as a restorative material in fixed prosthodontics [34], [38]. Computer-aided design (CAD) and computer-aided manufacturing (CAM) technologies have increased accuracy and made it easier for the fabrication of modern restorative and prosthetic materials [39], [40], [41]. Individual ceramic produced from CAD/CAM can be incorporated in the complete denture to increase their wear resistance [40], [41], [42]. Recently, CAD/CAM technologies are used in the fabrication of PEKK prosthetic restorations [39], [43], [44]. Pekkton® ivory (PEKK) is used for monolithic and bi-layered material with an indirect composite veneer (Fig. 3A–C) [17].
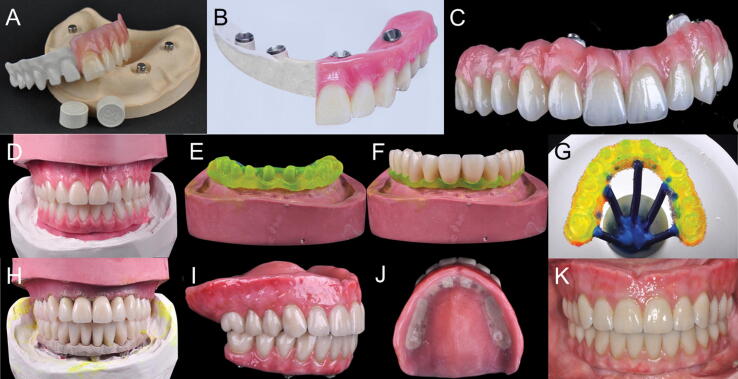
Fig. 3.
(A–C) Various PEKK implant prostheses made by Pekkton (Cendres + Métaux, Switzerland) containing monolithic and bi-layered veneered resin; (D–K) Use of PEKK for implant prosthesis framework with single lithium disilicate glass-ceramic crowns [62]. (D) Diagnostic tooth arrangement following the duplication of maxillary and mandibular interim dentures. (E) Maxillary framework resin pattern. (F) Maxillary teeth fitted on resin pattern framework. (G) Maxillary resin pattern framework for investment. (H) Teeth fitted over PEKK frameworks on maxillary and mandibular casts. (I) Maxillary complete denture, and mandibular implant-supported prosthesis. (J) Tissue surface of the maxillary denture. (K) Frontal view of the completed maxillary complete denture and mandibular implant-supported prosthesis.
Bonding of PEKK to restorative materials is essential in restorative and prosthetic dentistry. Various surface treatment methods of PEKK have been formulated for bonding using various adhesives systems [6], [45], [46], [47], [48], [49]. Lee et al. [45] studied the PEKK’s bond strength (shear) to dental resin composite by using various surface treatment methods for PEKK bonding and found that mechanical surface treatment behaves better than chemical surface treatment (95% sulfuric acid and air abrasion using alumina with 110 µm and 50 µm). Unlike other adhesives, 10-methacryloyloxydecyl dihydrogen phosphate and self-etching universal adhesive containing silane (Single Bond Universal) presented efficient shear bond strength in all treatments. Similarly, the non-thermal plasma surface modification with sandblasting increased the shear bond strength between the resin cement and PEKK [50]. Universal adhesive shows similar bonding as visio-link (light-polymerizing PMMA and composite resin primer) for PEKK [47].
The fit of the dental restoration is another important factor in the prosthetic dentistry. Poor marginal fit results in plaque deposition, recurrent caries with periodontal damage, and failure of the restoration [51], [52], [53]. Several researchers have proposed 24–110 μm as the acceptable marginal discrepancy for CAD/CAM fixed restorations [54], [55]. Bae et al. [39] studied the three-dimensional marginal fit (internal fit) of PEKK 51.64 ± 1.5 (36.12 ± 1.34) μm and zirconia copings 69.62 ± 8.11 (41.6 ± 1.63) μm and observed that the marginal fit (internal fit) were within the acceptable range. However, the PEKK presented less stress distribution around its loading areas, and better fitness was observed in the PEKK coping compared to zirconia coping [39].
Tooth/enamel wear caused by dental restorations is common and varies with the type of restorative materials. Ideally, the tooth/enamel wear due to dental restorations should not be more than the physiological wear of the teeth. The selection of appropriate restorative materials, aimed at having an almost similar degree of hardness to that of enamel is important for minimizing/retarding the harmful and irreversible consequences of tooth/enamel wear [56], [57]. Choi et al. [58] evaluated the effects of polymeric restoration on opposing tooth wear where they examined five materials fabricated from CAD/CAM: Pekkton (PEKK), Yamahachi PMMA (YAP), Mazic Duro (MZD), Vipi Block Monocolor (VBM), and Vita Enamic (ENA). It was seen that PEKK resulted in the most significant material wear but the least antagonist tooth wear. PEKK, YBM, and YAP were easily deformed and displaced by stress due to low elastic modulus. Therefore, appropriate restorative material should be selected for a specific clinical situation. Therefore, crowns fabricated from PEKK material show high wear than zirconia crowns [58], [59].
PEKK as an implant biomaterial, abutments, and prosthesis
The high-performance with iso-elastic characteristics of PEKK has potential applications in oral implantology [19]. PEKK has the advantage of being enough strength, lightweight, wear resistance, and elastic modulus close to that of dentin [34]. Dental implants fabricated from thermoplastic resins have also shown acceptable results for the percentages of bone contact [60]. In oral implantology, PEKK can be used as implant abutments [27], [61], framework material for implant prosthesis [17], [62], [63], [64], prosthetic crown materials over the implant [17], and implant biomaterial [27]. PEKK is metal-free and presents an alternative material to titanium implant [27]. The advantage of PEKK abutments is adjustable and compatible with various veneering materials [17] and can be used as a framework for an implant-supported prosthesis [65]. Combining the PEKK attachment system with titanium can be a potential material to provide long-term retention in implant prosthesis [66].
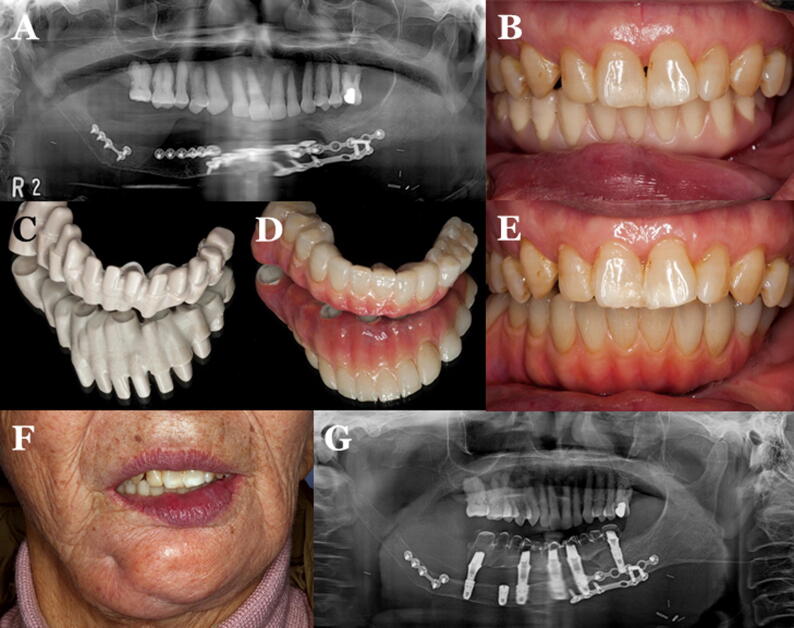
Conventional complete denture (CCD) opposed by an implant-supported fixed complete dental prosthesis (ICFDP) presents the problem of replacement of the posterior teeth due to wear of acrylic teeth in a few years following insertion. This problem is seen more in complete denture (47.7%) followed by ICFDP (19.6%) [67], [68], [69]. To overcome these problems, CAD/CAM zirconia teeth can be incorporated in a complete denture or another implant prosthesis to increase their wear resistance [40], [41], [42], [70], [71]. Dawson et al. [62] described the application of PEKK as a framework for ICFDP with single lithium disilicate glass-ceramic crowns and a CCD (Fig. 3D-K). The prosthesis provides a non-CAD-CAM option for the fabrication of ICFDPs and CCD with single ceramic crowns. PEKK can also be used in maxillofacial rehabilitation. Oh et al. [63] described the rehabilitation of a mandibulectomy patient with fibula free flap and implant-supported prosthesis using PEKK framework material (Fig. 4).
Fig. 4.
PEKK framework material for rehabilitation of a mandibulectomy patient [63]. (A) Panoramic radiograph of mandible following reconstruction with fibula free flap. (B) Trial denture. (C) PEKK framework fabricated after scanning the completed wax trial denture. (D) Final prosthesis after adding gingiva opaquer and gingiva-colored resins to match the gingiva, and cementing PMMA crowns to the framework. (E) Intraoral view of the prosthesis. (F) Final prosthesis in the patient. (G) Panoramic radiograph at follow up visit.
The PEKK framework shows less stress to the implant and tissue under compressive stress compared to tensile stress [37]. Therefore, the PEKK framework should be limited in some areas are they are resilient framework. The rigid framework prosthesis shows favorable stress distribution. Although there is a wide application of PEKK in oral implantology, they should be applied for a suitable purpose, and further studies are necessary for studying the chemical modulation of PEKK to increase the implant-contact.
PEKK for fabricating removable partial frameworks and attachments
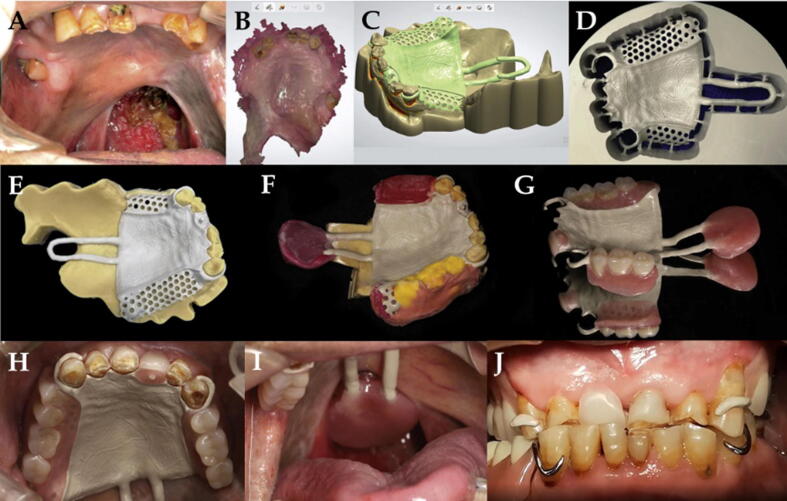
Metal clasps in removable prosthesis carry disadvantages of being unaesthetic and may cause oral galvanism and allergic reactions in some patients [72]. Thermoplastic materials have solved such problems to some extent [73], [74]. Recently, PEKK is used in removable partial denture (RPD) as dental clasps and frameworks using digital technology. Sun et al. [38] presented a digital workflow for applying PEKK in removal speech bulb prosthesis. The process consisted of intraoral scanning, 3D printing, designing, manufacture (digital milling of PEKK framework), and delivery (Fig. 5).
Fig. 5.
Digital workflow for the fabrication of a PEKK in removal speech bulb prosthesis [38]. (A) Pretreatment maxillary arch with a defect of the soft palate. (B) Intraoral scan of the maxillary arch. (C) Computer-aided design of PEKK framework with showing components design of PEKK framework. (D) Computed-aided manufacturing showing milled framework in PEKK disk. (E) PEKK framework on the master cast. (F) Maxillary edentulous area definitive impression, maxillo-mandibular record, and impression of the soft-palate defect. (G), Final PEKK removable prosthesis. (H) Maxillary major connector. (I) PEEK rod and acrylic bulb of the prosthesis. (J) Intraoral view of the removable prosthesis with speech bulb.
Retention is important in RPD prosthesis, Tannous et al. [75] studied the retentive force of CoCr alloy and three thermoplastics; PEEK, PEKK, and polyoxymethylene (POM). They fabricated 1.0 mm thick CoCr clasps in 0.25 mm undercuts and 1.0 or 1.5 mm thick thermoplastic resins in 0.5 mm undercuts, respectively. They found that all clasps showed high retentive force in the first period of cycling with a decrease till the end of the cycling. The resin clasps showed significantly lower retentive force than the CoCr clasps. Thermoplastic resin clasps-maintained longer retention with less retention than CoCr clasp. PEKK clasps can be used to provide retention for a longer duration. PEKK can also be used as inserts in the removable partial denture. Choi et al. [76] studied the attachment systems with a PEKK insert and found that PEKK insert showed less retention change and abrasion compared to the nylon inserts.
A finite element study by Keilig et al. revealed that there was a great influence of stress evenly distributed in the framework material of small bridges (three and four units). Furthermore, the surrounding tissues were not influenced by strain around them due to the choice of the material. This confirmed that the polymer PEKK could be an alternative to metal framework [77].
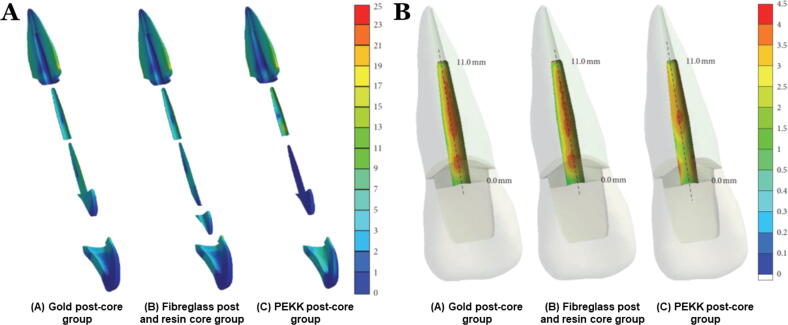
PEKK for endodontic posts-core and endocrowns
The PEKK biomaterial has been attracted in the post-core systems because of its acceptable processing (milling and pressing), suitable mechanical strength, and shock-absorbing ability [78], [79]. PEKK presents superior biomechanical behavior compared to metal and fiberglass post-core systems. The PEKK showed superior fracture resistance compared to metal and fiberglass post-core systems due to lower elastic modulus and flexural strength. Lee et al. [78] studied long term safety and biomechanical behavior of PEKK as intraradicular post and core material. Their study concluded PEKK as a dental post-core system has potentially high fracture resistance, although PEKK has a significantly lower elastic modulus and flexural strength than metal (gold) and fiberglass (Fig. 6). Thus, the PEKK post-core exhibited a favorable stress distribution at the intraradicular surface, indicating a less chance of root fracture than for conventional post-core materials. In addition, PEKK transferred higher stresses to the interface materials. Therefore, the probability of crown and cement debonding failure would be at interface level than that of rigid post-core systems where fracture of root might be anticipated [78]. PEKK post-core presents favorable stress distribution, reducing the possibility of root fracture. Nevertheless, debonding and crown failure may be higher in PEKK post-core due to its flexibility. PEKK material act as a stress breaker and reduces the forces transferred to the restoration and tooth-root [15]. Hence, PEKK can be used as endocrowns for endodontically treated teeth. This is important, especially in extensively damaged teeth.
Fig. 6.
Stress distribution of the PEEK post compared to gold post-core and fiberglass post with resin core [78]. (A) Sagittal section views of stress distribution of the components. (B) Coronal section views of the stress distribution at the labial side interface surface of dentine and post cement along the mid-plane.
In addition, PEKK posts are suitable for posts fabrication. Güven et al. [79] studied on the bonding of prefabricated PEKK posts, and custom made PEKK posts and conventional fiber posts. They found that the custom fabricated PEKK posts showed higher bond strength than prefabricated PEKK posts. The custom made PEKK post showed the maximum bond-strength (17.34 MPa) in the cervical region as confirmed from the scanning electron image. The conventional fiber posts showed the highest bond-strength values in the middle (11.53 MPa) and apical sections (6.86 MPa).
The conditioning of a material influences the bonding of PEKK. Fuhrmann et al. [15] evaluated the bond strength of adhesive systems to amorphous and crystalline PEKK and fiber-reinforced PEEK using five types of surface conditioning techniques. They found that the fiber-reinforced PEEK showed more considerable bond strengths and at all three storage times (5, 30, 150 days) than crystalline and amorphous PEKK. Silica coating conditioning and priming showed the highest tensile bond strength. Finally, although there is a wide application of PEKK in prosthodontics and oral implantology, long-term observation is needed as long-term data for the PEKK framework are yet not available.
Conclusions
The PEKK materials present suitable physical, mechanical, and chemical properties and can be used for various applications such as restorative material, crown and bridge work, endo crowns, framework material for an implant-supported fixed prosthesis, and as dental biomaterial implants. Further, modifications and improving material properties can result in wider applications in clinical dentistry. Long term evaluations are needed as PEKK is recently applied in dentistry, and there are limited studies available.
Compliance with Ethics Requirements
This article does not contain any studies with human or animal subjects.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Biographies

Hatim Alqurashi received Bachelor of Dental Surgery (BDS) from Dammam University in 2014. In 2018, he received MSc in Dental Materials from University of Sheffield, UK. Currently, he is a lecturer at Department of preventive sciences, Collage of Dentistry, King Faisal University. Also, he is doing his PhD in oral tissue engineering at School of Clinical Dentistry, University of Sheffield, UK. His research areas include Orthodontic, Extracellular vesicles, biomaterial, Tissue engineering and regenerative medicine.

Dr Zohaib Khurshid working as lecturer and course coordinator in the Prosthodontics and Dental Implantology Department, School of Dentistry, King Faisal University, Saudi Arabia. His research interest is dental biomaterials, oral antimicrobial peptides synthesis, salivary diagnostics, gingival crevicular fluids (GCFs) proteome, platelet-rich proteins (PRPs) proteome, and dental biomaterials proteomic analysis. He authored more than 100 publications including review papers, research papers, systematic reviews & metanalysis, books chapters, editorials, news magazines report, and scoping study. He is running a human salivary research group in Pakistan helping MSc, MDS, MPhil and PhD student for thesis projects and individual faculty projects as well. His editorial activity is with European Journal of Dentistry (EJD), Journal of Oral Research (JOralRes), Dentistry Journal, Materials, Polymer, International Journal of Molecular Sciences (IJMS), and European Journal of Dental Research and Biomaterials. He is the editor of the three books with Elsevier Publisher on “Advanced Dental Biomaterials”, “Dental implants: materials, coatings, surface modifications and interfaces with oral tissues” and “Biomaterials in Endodontics” with Elsevier Publisher. Scopus profile: https://www.scopus.com/authid/detail.uri?authorId=56530616000. Publons: https://publons.com/researcher/976438/zohaib-khurshid/.

Syed Azeem Ul Yaqin received BDS degrees from Karachi University, Pakistan in 2008 and Master of Science degree in Dental Materials from Faculty of Dentistry, University of Sheffield, United Kingdom, in 2013, and Doctorate in Clinical Dentistry in Prosthodontics from Faculty of Dentistry, University of Sheffield, United Kingdom in 2016. He has recently been working as Assistant Professor department of Prosthodontics, College of Dentistry, King Faisal University, Saudi Arabia. He is also Member of the Faculty of General Dentist Practitioners (MFGDP), United Kingdom since 2018. He is involved in both clinical and research activities in prosthetic dentistry, has few book chapters to his name in Advanced Dental Biomaterials and currently working on research related to strength of different polymeric crowns.

Syed Rashid Habib received BDS degree from de’ Montmorency College of Dentistry/University of Punjab, Lahore, Pakistan in 1999 and Fellowship from College of Physicians and Surgeons, Pakistan in the specialty of Prosthodontics in 2007. Dr. Habib has served as Clinical Assistant Director with Invisalign®, Pakistan; Assistant Professor at Islamic International Dental College, Islamabad, Pakistan and Assistant Professor at National University of Sciences and Technology, Islamabad, Pakistan. He joined Department of Prosthetic Dental Sciences, College of Dentistry, King Saud University, Riyadh, Saudi Arabia as a faculty in 2009 and is currently working as Associate Professor in the department. Besides full time involvement in teaching and clinical activities, Dr. Habib is actively involved in research. His research interests revolves around dental materials, dental education and contemporary topics of interest in the specialty of Prosthodontics.

Dinesh Rokaya received BDS degrees from Tribhuvan University, Nepal in 2009 and Master of Science degree in Dentistry from Faculty of Dentistry, Mahidol University, Thailand in 2015, and PhD in Dental Biomaterials Science from Faculty of Dentistry, Chulalongkorn University, Thailand in 2019. He is currently a Lecturer at Walailak University International College of Dentistry, Thailand. He has recently received Diploma of Membership of Faculty of Dental Surgery (MFDS) from Royal College of Physicians and Surgeons of Glasgow. He is involved in both clinical and research activities in prosthetic dentistry. His research includes various polymeric materials for dental applications.

Dr. Muhammad Sohail Zafar completed his Ph.D at Nottingham Trent University (2011) after obtaining master’s degree in Dental Materials from Queen Mary University of London, UK (Distinction level research project; 2007). Currently, he is working as an associate professor of dental biomaterials at College of Dentistry, Taibah University, Saudi Arabia, where he has been a faculty member since 2012. Before that (2011-2012), he worked as an associate researcher at Nottingham Trent University, UK. He holds fellowship of International College of Dentists, USA (FICD) and Academy of Dentistry international, USA (FADI). Being a research led academician, Dr. Zafar has a considerable exposure of teaching, research and clinics management and the successful implementation of operating procedures in academic and clinic activities. I have contributed substantially (more than 150 peer reviewed publications since 2013) in the field of dental materials, tissue engineering and clinical dentistry (Scopus: https://www.scopus.com/authid/detail.uri?authorId=56147787800h-index of 23; google scholar: https://scholar.google.co.uk/citations?user=N4S8HI8AAAAJ&hl=enh-index of 34; i10-index of 78). Dr. Zafar is an editorial board member for journals “Fluoride” (Official publication of fluoride: https://www.fluorideresearch.org/494Pt1/files/FJ2016_v49_n4Pt1_p00i-0ii_sfs.pdf (International Society for Fluoride Research, New Zealand) and https://www.thieme.com/edboards/EJD_EDITORIAL_BOARD.pdfEuropean Journal of Dentistry. His research interests include advances biomaterials, tissue regeneration, nanomaterials and polymeric biomaterials for dental applications.
Footnotes
Peer review under responsibility of Cairo University.
Contributor Information
Dinesh Rokaya, Email: dineshrokaya115@hotmail.com.
Muhammad Sohail Zafar, Email: MZAFAR@taibahu.edu.sa.
References
- 1.Xu X., He L., Zhu B., Li J., Li J. Advances in polymeric materials for dental applications. Polym Chem. 2017;8:807–823. [Google Scholar]
- 2.Rokaya D., Srimaneepong V., Sapkota J., Qin J., Siraleartmukul K., Siriwongrungson V. Polymeric materials and films in dentistry: an overview. J Adv Res. 2018;14:25–34. doi: 10.1016/j.jare.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Najeeb S., Zafar M.S., Khurshid Z., Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodontic Res. 2016;60:12–19. doi: 10.1016/j.jpor.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Choupin T. Mechanical performances of PEKK thermoplastic composites linked to their processing parameters; 2017.
- 5.Huang B., Qian J., Wang G., Cai M. Synthesis and properties of novel copolymers of poly (ether ketone diphenyl ketone ether ketone ketone) and poly (ether amide ether amide ether ketone ketone) Polym Eng Sci. 2014;54:1757–1764. [Google Scholar]
- 6.Stawarczyk B., Eichberger M., Uhrenbacher J., Wimmer T., Edelhoff D., Schmidlin P.R. Three-unit reinforced polyetheretherketone composite FDPs: influence of fabrication method on load-bearing capacity and failure types. Dent Mater J. 2015;34:7–12. doi: 10.4012/dmj.2013-345. [DOI] [PubMed] [Google Scholar]
- 7.Sorte N., Bhat V., Hegde C. Poly-ether-ether-ketone (PEEK): a review. Int J Recent Sci Res. 2017;8:19208–19211. [Google Scholar]
- 8.Kurtz S.M., Devine J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials. 2007;28:4845–4869. doi: 10.1016/j.biomaterials.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zoidis P., Papathanasiou I., Polyzois G. The use of a modified poly-ether-ether-ketone (PEEK) as an alternative framework material for removable dental prostheses. A clinical report. J Prosthodont. 2016;25:580–584. doi: 10.1111/jopr.12325. [DOI] [PubMed] [Google Scholar]
- 10.Amornvit P., Rokaya D., Sanohkan S. Applications of PEEK in implant retained finger prosthesis. J Int Dental Med Res. 2019;12:1606–1609. [Google Scholar]
- 11.J.W.H. Bonner, Aromatic polyketones and preparation thereof, U.S. Patent 3,065,205; 1962. p. 1–3.
- 12.Sakihara M., Taira Y., Sawase T. Effects of sulfuric and vinyl sulfonic acid etchants on bond strength of resin composite to polyetherketoneketone. Odontology. 2019;107:158–164. doi: 10.1007/s10266-018-0375-0. [DOI] [PubMed] [Google Scholar]
- 13.Wang M., Bhardwaj G., Webster T.J. Antibacterial properties of PEKK for orthopedic applications. Int J Nanomed. 2017;12:6471–6476. doi: 10.2147/IJN.S134983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kewekordes T., Wille S., Kern M. Wear of polyetherketoneketones—influence of titanium dioxide content and antagonistic material. Dent Mater. 2018;34:560–567. doi: 10.1016/j.dental.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 15.Guo R, McGrath J. In: Matyjaszewski K, Möller M, editors. Polymer science: a comprehensive reference. Amsterdam: Elsevier; 2012. p. 377–430.
- 16.Fuhrmann G., Steiner M., Freitag-Wolf S., Kern M. Resin bonding to three types of polyaryletherketones (PAEKs)—durability and influence of surface conditioning. Dent Mater. 2014;30:357–363. doi: 10.1016/j.dental.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Alsadon O., Wood D., Patrick D., Pollington S. Fatigue behavior and damage modes of high performance poly-ether-ketone-ketone PEKK bilayered crowns. J Mech Behav Biomed Mater. 2020;110:103957. doi: 10.1016/j.jmbbm.2020.103957. [DOI] [PubMed] [Google Scholar]
- 18.Han K., Lee J., Shin S.W., Han K., Lee J., Shin S.W. Implant-and tooth-supported fixed prostheses using a high-performance polymer (Pekkton) framework. Int J Prosthodont. 2016;29:451–454. doi: 10.11607/ijp.4688. [DOI] [PubMed] [Google Scholar]
- 19.Schwitalla A.D., Spintig T., Kallage I., Müller W. Flexural behavior of PEEK materials for dental application. Dent Mater. 2015;31:1377–1384. doi: 10.1016/j.dental.2015.08.151. [DOI] [PubMed] [Google Scholar]
- 20.Song C., Choi J., Jeon Y., Jeong C., Lee S., Kang E. Comparison of the microtensile bond strength of a polyetherketoneketone (PEKK) tooth post cemented with various surface treatments and various resin cements. Materials. 2018;11:916. doi: 10.3390/ma11060916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hench L, Wilson J. An introduction to bioceramics. 1993, Singapour: World Scientific; 1971. p. 200.
- 22.Krejci I., Mueller E., Lutz F. Effects of thermocycling and occlusal force on adhesive composite crowns. J Dent Res. 1994;73:1228–1232. doi: 10.1177/00220345940730061501. [DOI] [PubMed] [Google Scholar]
- 23.Kim H., Kwon T., Kim K., Kwon S., Cho D., Son J.S. Long-term release of chlorhexidine from dental adhesive resin system using human serum albumin nanoparticles. Polym Bull. 2014;71:875–886. [Google Scholar]
- 24.Wypych G. Elsevier; Toronto: 2016. Handbook of polymers. [Google Scholar]
- 25.Shibata M., Yosomiya R., Wang J., Zheng Y., Zhang W., Wu Z. Relationship between molecular structure and thermal properties of poly (aryl ether ketone) s. Macromol Rapid Commun. 1997;18:99–105. [Google Scholar]
- 26.Santos FdP, Campos Ed, Costa M, Melo FCL, Honda RY, Mota RP. Superficial modifications in TiO2 and Al2O3 ceramics, Mater Res 2003;6:353–7.
- 27.Schwitalla A., Müller W. PEEK dental implants: a review of the literature. J Oral Implantol. 2013;39:743–749. doi: 10.1563/AAID-JOI-D-11-00002. [DOI] [PubMed] [Google Scholar]
- 28.Adamzyk C., Kachel P., Hoss M., Gremse F., Modabber A., Hoelzle F. Bone tissue engineering using polyetherketoneketone scaffolds combined with autologous mesenchymal stem cells in a sheep calvarial defect model. J Cranio-Maxillofacial Surgery. 2016;44:985–994. doi: 10.1016/j.jcms.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Yuan B., Cheng Q., Zhao R., Zhu X., Yang X., Yang X. Comparison of osteointegration property between PEKK and PEEK: Effects of surface structure and chemistry. Biomaterials. 2018;170:116–126. doi: 10.1016/j.biomaterials.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 30.Olivares-Navarrete R., Hyzy S.L., Gittens R.A., Schneider J.M., Haithcock D.A., Ullrich P.F. Rough titanium alloys regulate osteoblast production of angiogenic factors. Spine J. 2013;13:1563–1570. doi: 10.1016/j.spinee.2013.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Converse G.L., Conrad T.L., Merrill C.H., Roeder R.K. Hydroxyapatite whisker-reinforced polyetherketoneketone bone ingrowth scaffolds. Acta Biomater. 2010;6:856–863. doi: 10.1016/j.actbio.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 32.Walsh W.R., Bertollo N., Christou C., Schaffner D., Mobbs R.J. Plasma-sprayed titanium coating to polyetheretherketone improves the bone-implant interface. Spine J. 2015;15:1041–1049. doi: 10.1016/j.spinee.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 33.Moore R., Beredjiklian P., Rhoad R., Theiss S., Cuckler J., Ducheyne P. A comparison of the inflammatory potential of particulates derived from two composite materials. J Biomed Mater Res: Off J Soc Biomater Japanese Soc Biomater. 1997;34:137–147. doi: 10.1002/(sici)1097-4636(199702)34:2<137::aid-jbm1>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 34.Stawarczyk B., Jordan P., Schmidlin P.R., Roos M., Eichberger M., Gernet W. PEEK surface treatment effects on tensile bond strength to veneering resins. J Prosthet Dent. 2014;112:1278–1288. doi: 10.1016/j.prosdent.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 35.Elkabbany A., Kern M., Elkhadem A.H., Wille S., Amer A.A., Chaar M.S. Retention of metallic and non-metallic double-crown-retained mandibular overdentures on implants: an in-vitro study. J Prosthodont Res. 2020;64:384–390. doi: 10.1016/j.jpor.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Nishihara H., Adanez M.H., Att W. Current status of zirconia implants in dentistry: preclinical tests. J Prosthodontic Res. 2019;63:1–14. doi: 10.1016/j.jpor.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Lee K., Shin S., Lee S., Kim J., Kim J., Lee J. Comparative evaluation of a four-implant-supported polyetherketoneketone framework prosthesis: a three-dimensional finite element analysis based on cone beam computed tomography and computer-aided design. Int J Prosthodont. 2017;30:581–585. doi: 10.11607/ijp.5369. [DOI] [PubMed] [Google Scholar]
- 38.Sun F., Shen X., Zhou N., Gao Y., Guo Y., Yang X. A speech bulb prosthesis for a soft palate defect with a polyetherketoneketone (PEKK) framework fabricated by multiple digital techniques: a clinical report. J Prosthet Dent. 2019 doi: 10.1016/j.prosdent.2019.10.020. [DOI] [PubMed] [Google Scholar]
- 39.Bae S., Park J., Jeong I., Kim H., Kim J., Kim W. Three-dimensional analysis of marginal and internal fit of copings fabricated with polyetherketoneketone (PEKK) and zirconia. J Prosthodontic Res. 2017;61:106–112. doi: 10.1016/j.jpor.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 40.Livaditis J.M., Livaditis G.J. The use of custom-milled zirconia teeth to address tooth abrasion in complete dentures: a clinical report. J Prosthodontics: Implant, Esthetic Reconstr Dent. 2013;22:208–213. doi: 10.1111/j.1532-849X.2012.00943.x. [DOI] [PubMed] [Google Scholar]
- 41.Afify A., Haney S. Enhancing fracture and wear resistance of dentures/overdentures utilizing digital technology: a case series report. J Prosthodontics. 2016;25:489–494. doi: 10.1111/jopr.12462. [DOI] [PubMed] [Google Scholar]
- 42.Myerson R.L. The use of porcelain and plastic teeth in opposing complete dentures. J Prosthet Dent. 1957;7:625–633. [Google Scholar]
- 43.Park M., Shin S. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J Prosthet Dent. 2018;119 doi: 10.1016/j.prosdent.2017.08.020. 861.e1–861.e7. [DOI] [PubMed] [Google Scholar]
- 44.Alsadon O., Wood D., Patrick D., Pollington S. Comparing the optical and mechanical properties of PEKK polymer when CAD/CAM milled and pressed using a ceramic pressing furnace. J Mech Behav Biomed Mater. 2019;89:234–236. doi: 10.1016/j.jmbbm.2018.09.039. [DOI] [PubMed] [Google Scholar]
- 45.Lee K., Shin M., Lee J., Ryu J., Shin S. Shear bond strength of composite resin to high performance polymer PEKK according to surface treatments and bonding materials. J Adv Prosthodont. 2017;9:350–357. doi: 10.4047/jap.2017.9.5.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stawarczyk B., Silla M., Roos M., Eichberger M., Lümkemann N. Bonding behaviour of polyetherketoneketone to methylmethacrylate-and dimethacrylate-based polymers. J Adhes Dent. 2017;19:331–338. doi: 10.3290/j.jad.a38894. [DOI] [PubMed] [Google Scholar]
- 47.Lümkemann N., Eichberger M., Stawarczyk B. Bond strength between a high-performance thermoplastic and a veneering resin. J Prosthet Dent. 2020 doi: 10.1016/j.prosdent.2019.10.017. [DOI] [PubMed] [Google Scholar]
- 48.Fokas G., Guo C.Y., Tsoi J.K. The effects of surface treatments on tensile bond strength of polyether-ketone-ketone (PEKK) to veneering resin. J Mech Behav Biomed Mater. 2019;93:1–8. doi: 10.1016/j.jmbbm.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 49.Gama L.T., Duque T.M., Özcan M., Philippi A.G., Mezzomo L.A.M., Gonçalves, Simek Vega Thais Marques. Adhesion to high-performance polymers applied in dentistry: a systematic review. Dent Mater. 2020;36:e93–e108. doi: 10.1016/j.dental.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 50.Labriaga W., Song S., Park J., Ryu J., Lee J., Shin S. Effect of non-thermal plasma on the shear bond strength of resin cements to Polyetherketoneketone (PEKK) J Adv Prosthodont. 2018;10:408–414. doi: 10.4047/jap.2018.10.6.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Habib S.R., Al Otaibi A.K. Comparison between five CAD/CAM systems for fit of zirconia copings. Quintessence Int. 2018;49:437–444. doi: 10.3290/j.qi.a40354. [DOI] [PubMed] [Google Scholar]
- 52.Habib S.R. Digital microscopic evaluation of vertical marginal discrepancies of CAD/CAM fabricated zirconia cores. Biomed Eng/Biomedizinische Technik. 2019;64:207–214. doi: 10.1515/bmt-2017-0234. [DOI] [PubMed] [Google Scholar]
- 53.Habib S.R., Al Ajmi M.G., Al Dhafyan M., Jomah A., Abualsaud H., Almashali M. Effect of margin designs on the marginal adaptation of zirconia copings. Acta Stomatol Croat. 2017;51:179–187. doi: 10.15644/asc51/3/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Papadiochou S., Pissiotis A.L. Marginal adaptation and CAD-CAM technology: a systematic review of restorative material and fabrication techniques. J Prosthet Dent. 2018;119:545–551. doi: 10.1016/j.prosdent.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Mously H.A., Finkelman M., Zandparsa R., Hirayama H. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J Prosthet Dent. 2014;112:249–256. doi: 10.1016/j.prosdent.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 56.Habib S.R., Ansari A.S., Alqahtani M., Alshiddi I.F., Alqahtani A.S., Hassan S.H. Analysis of enamel and material wear by digital microscope: an in-vitro study. Brazilian Oral Res. 2019;33 doi: 10.1590/1807-3107bor-2019.vol33.0121. [DOI] [PubMed] [Google Scholar]
- 57.Habib S.R., Alotaibi A., Al Hazza N., Allam Y., AlGhazi M. Two-body wear behavior of human enamel versus monolithic zirconia, lithium disilicate, ceramometal and composite resin. J Adv Prosthodont. 2019;11:23–31. doi: 10.4047/jap.2019.11.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Choi J., Song E., Shin J., Jeong T., Huh J. In vitro investigation of wear of CAD/CAM polymeric materials against primary teeth. Materials. 2017;10:1410. doi: 10.3390/ma10121410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kotthaus M., Hasan I., Keilig L., Grüner M., Bourauel C., Stark H. Investigation of the retention forces of secondary telescopic crowns made from Pekkton® ivory in combination with primary crowns made from four different dental alloys: an in vitro study. Biomed Eng/Biomedizinische Technik. 2019;64:555–562. doi: 10.1515/bmt-2018-0167. [DOI] [PubMed] [Google Scholar]
- 60.Cook S.D., Rust-Dawicki A. Preliminary evaluation of titanium-coated PEEK dental implants. J Oral Implantol. 1994;21:176–181. [PubMed] [Google Scholar]
- 61.Tetelman E.D., Babbush C.A. A new transitional abutment for immediate aesthetics and function. Implant Dent. 2008;17:51–58. doi: 10.1097/ID.0b013e318167648c. [DOI] [PubMed] [Google Scholar]
- 62.Dawson J.H., Hyde B., Hurst M., Harris B.T., Lin W. Polyetherketoneketone (PEKK), a framework material for complete fixed and removable dental prostheses: a clinical report. J Prosthet Dent. 2018;119:867–872. doi: 10.1016/j.prosdent.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 63.Oh K.C., Park J., Lee J., Moon H.S. Treatment of a mandibular discontinuity defect by using a fibula free flap and an implant-supported fixed complete denture fabricated with a PEKK framework: a clinical report. J Prosthet Dent. 2018;119:1021–1024. doi: 10.1016/j.prosdent.2017.07.024. [DOI] [PubMed] [Google Scholar]
- 64.Srinivasan M., Kalberer N., Maniewicz S., Muller F. Implant-retained overdentures using an attachment with true-alignment correction: a case series. Int J Prosthodont. 2019;32:482–496. doi: 10.11607/ijp.6469. [DOI] [PubMed] [Google Scholar]
- 65.Amelya A., Kim J., Woo C., Otgonbold J., Lee K., Kim J. Load-bearing capacity of posterior CAD/CAM implant-supported fixed partial dentures fabricated with different esthetic materials. Int J Prosthodont. 2019;32:201–204. doi: 10.11607/ijp.6128. [DOI] [PubMed] [Google Scholar]
- 66.Passia N., Ghazal M., Kern M. Long-term retention behaviour of resin matrix attachment systems for overdentures. J Mech Behav Biomed Mater. 2016;57:88–94. doi: 10.1016/j.jmbbm.2015.11.038. [DOI] [PubMed] [Google Scholar]
- 67.Bozini T., Petridis H., Garefis K., Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int J Oral Maxillofacial Implants. 2011;26:304–318. [PubMed] [Google Scholar]
- 68.Purcell B.A., McGlumphy E.A., Holloway J.A., Beck F.M. Prosthetic complications in mandibular metal-resin implant-fixed complete dental prostheses: a 5-to 9-year analysis. Int J Oral Maxillofac Implants. 2008;23:847–857. [PubMed] [Google Scholar]
- 69.Mello PC, Coppedê AR, Macedo AP, Mattos, da Gloria Chiarello de Maria, Rodrigues RCS, Ribeiro RF. Abrasion wear resistance of different artificial teeth opposed to metal and composite antagonists. J Appl Oral Sci 2009;17:451–6. [DOI] [PMC free article] [PubMed]
- 70.Lin W., Metz M.J., Pollini A., Ntounis A., Morton D. Digital data acquisition for a CAD/CAM-fabricated titanium framework and zirconium oxide restorations for an implant-supported fixed complete dental prosthesis. J Prosthet Dent. 2014;112:1324–1329. doi: 10.1016/j.prosdent.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 71.Maló P., de Araújo Nobre M., Borges J., Almeida R. Retrievable metal ceramic implant-supported fixed prostheses with milled titanium frameworks and all-ceramic crowns: retrospective clinical study with up to 10 years of follow-up. J Prosthodont: Implant, Esthetic Reconstr Dent. 2012;21:256–264. doi: 10.1111/j.1532-849X.2011.00824.x. [DOI] [PubMed] [Google Scholar]
- 72.Behr M., Zeman F., Passauer T., Koller M., Hahnel S., Buergers R. Clinical performance of cast clasp-retained removable partial dentures: a retrospective study. Int J Prosthodont. 2012;25:138–144. [PubMed] [Google Scholar]
- 73.Donovan T.E., Cho G.C. Esthetic considerations with removable partial dentures. J Calif Dent Assoc. 2003;31:551–557. [PubMed] [Google Scholar]
- 74.Donovan T.E., Derbabian K., Kaneko L., Wright R. Esthetic considerations in removable prosthodontics. J Esthetic Restorat Dent. 2001;13:241–253. doi: 10.1111/j.1708-8240.2001.tb00270.x. [DOI] [PubMed] [Google Scholar]
- 75.Tannous F., Steiner M., Shahin R., Kern M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent Mater. 2012;28:273–278. doi: 10.1016/j.dental.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 76.Choi J., Yun B., Jeong C., Huh J. Retentive properties of two stud attachments with polyetherketoneketone or nylon insert in mandibular implant overdentures. Int J Oral Maxillofac Implants. 2018;33:1079–1088. doi: 10.11607/jomi.6023. [DOI] [PubMed] [Google Scholar]
- 77.Keilig L., Stark H., Bourauel C. Does the material stiffness of novel high-performance polymers for fixed partial dentures influence their biomechanical behavior? Int J Prosthodont. 2016;30:595–597. doi: 10.11607/ijp.4940. [DOI] [PubMed] [Google Scholar]
- 78.Lee K., Shin J., Kim J., Kim J., Lee W., Shin S. Biomechanical evaluation of a tooth restored with high performance polymer PEKK post-core system: a 3D finite element analysis. BioMed Res Int. 2017;2017:1–9. doi: 10.1155/2017/1373127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Güven M.Ç., Dayan S.Ç., Yıldırım G., Mumcu E. Custom and prefabricated PolyEtherKetoneKetone (PEKK) post-core systems bond strength: scanning electron microscopy evaluation. Microsc Res Tech. 2020:804–810. doi: 10.1002/jemt.23471. [DOI] [PubMed] [Google Scholar]