Patients approaching end-stage kidney disease (ESKD) face numerous disadvantages. They have a high comorbidity burden [1] with decreased life expectancy [2], decreased quality of life [3], and suffer from anxiety and depression [4]. These patients and their caregivers must make crucial decisions that will impact their future life and health conditions.
The first decision is whether they want to undertake the burden of renal replacement therapy. For the elderly and frail subjects with ESKD, the benefit of dialysis treatment might not be as high as it is for the younger patients, considering the related discomfort, pain and disruption of their lifestyle. They might be offered the option of comprehensive conservative kidney care as an alternative to dialysis [5].
The next decision to be made by the patients undergoing renal replacement therapy and their family members is about dialysis modality. Every patient approaching ESKD should be given unbiased information and education on both dialysis modalities, unless there are contraindications to any particular modality. It is important to recognize that a large proportion of patients approaching ESKD are in a state of anxiety or mental distress [4]. They might prefer a home dialysis modality but may not be confident in self-care and self-management. Patient education level and socio-economic status are diverse. The role of education is crucial in this situation. Education should be tailored to patient’s intellectual level and socio-economic situation. An interactive strategy with audiovisual and written materials may be desirable for some patients [6].
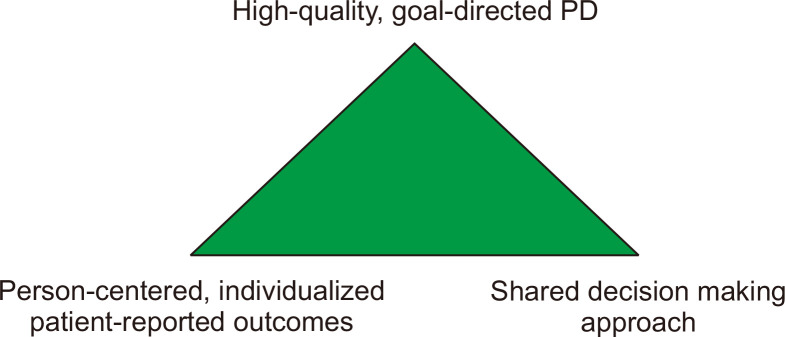
The International Society for Peritoneal Dialysis (ISPD) has recently published practice recommendations on prescribing high-quality goal-directed peritoneal dialysis (PD) [7]. The ISPD recommended that PD should be prescribed using shared decision making between the person doing PD and the care team in order to achieve realistic care goals tailored to each individual patient (the concept of ‘patient-centeredness’ or ‘person-centeredness’) (Fig. 1) [8].
Figure 1. The concept of high-quality, goal-directed peritoneal dialysis.
Choice of PD and PD prescription should be undertaken using shared decision making between the person doing PD and the care team in order to achieve realistic care goals tailored to each individual patient (the concept of ‘patient-centeredness’ or ‘person-centeredness’).
PD, peritoneal dialysis.
The Institute of Medicine defined patient-centered care as “a care that is respectful of and responsive to individual patient preferences, needs, and values” and that ensures “that patient values guide all clinical decisions” [9]. This definition highlights the importance of clinicians and patients working together to produce the best outcomes possible. Transition in the focus of care from ‘adequate’ dialysis to ‘person-centered’, ‘goal-directed’ dialysis was recently proposed at the Kidney Disease Improving Global Outcomes (KDIGO) Controversies Conference on Dialysis Initiation, Modality Choice and Prescription [6]. Here, it was proposed that dialysis modality should be chosen with timely and shared decision making among the healthcare team, patients, and their caregivers. The approach to choosing a dialysis modality should be ideally person-centered, engaging the patient in the context of their goals of care, local resources, out-of-pocket costs, the capacity of regional healthcare facilities, and medical feasibility. Moving away from a “one-size-fits-all” approach and providing more individualized or personalized care to patients is an important component of dialysis care.
In this issue of Kidney Research and Clinical Practice, Watanyu et al [10] conducted an open-label controlled clinical trial comparing customized versus conventional video counseling on PD decision-making. For this clinical trial, they created video materials customized to the language environment, occupation and household income of individual patients. The study was carried out in Thailand, a country with a PD-first policy. As the result, there was no difference in the PD acceptance rate, which was very high for both groups (66.6% for the customized group, 63.3% for the conventional group). Patient knowledge of and confidence in PD increased after counseling in both groups, but the difference was not significant. Although this study exhibited negative results in terms of the primary and secondary outcomes, PD acceptance rate may not be an optimal end-point for determining the effect of patient education, particularly in the setting of a PD-first policy. It is not desirable for all the subjects with ESKD to choose PD as their first dialysis modality. Other tools for assessing the quality of customized counseling should be employed. The study also provided only one-time counseling for half an hour, which may be insufficient to change the attitude of chronically-ill patients, as the authors state in their manuscript.
Nevertheless, the study showed some benefits from customized video counseling. In the customized video counseling group, there were fewer barriers to starting PD in terms of concerns regarding infection due to a limited home environment and fear of PD catheter insertion. The customized video counseling addresses common concerns about PD, especially the PD catheter insertion procedure, which helps to diminish fears among patients who might otherwise postpone the decision to accept PD.
In conclusion, the approach to choosing a dialysis modality should be person-centered and goal-directed, with consideration of the goals of care, local resources, socio-economics and healthcare cost. Multiple measures including patient-reported outcome measures need to be employed when assessing the quality of person-centered care and education.
Footnotes
Conflicts of interest
The author has no conflicts of interest to declare.
References
- 1.Nesrallah GE, Dixon SN, MacKinnon M, et al. Home palliative service utilization and care trajectory among Ontario residents dying on chronic dialysis. Can J Kidney Health Dis. 2018;5:2054358118783761. doi: 10.1177/2054358118783761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foster BJ, Mitsnefes MM, Dahhou M, Zhang X, Laskin BL. Changes in excess mortality from end stage renal disease in the United States from 1995 to 2013. Clin J Am Soc Nephrol. 2018;13:91–99. doi: 10.2215/CJN.04330417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aguiar R, Pei M, Qureshi AR, Lindholm B. Health-related quality of life in peritoneal dialysis patients: a narrative review. Semin Dial. 2019;32:452–462. doi: 10.1111/sdi.12770. [DOI] [PubMed] [Google Scholar]
- 4.Bezerra CIL, Silva BC, Elias RM. Decision-making process in the pre-dialysis CKD patients: do anxiety, stress and depression matter? BMC Nephrol. 2018;19:98. doi: 10.1186/s12882-018-0896-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muthalagappan S, Johansson L, Kong WM, Brown EA. Dialysis or conservative care for frail older patients: ethics of shared decision-making. Nephrol Dial Transplant. 2013;28:2717–2722. doi: 10.1093/ndt/gft245. [DOI] [PubMed] [Google Scholar]
- 6.Chan CT, Blankestijn PJ, Dember LM, et al. Conference Participants, author. Dialysis initiation, modality choice, access, and prescription: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) controversies conference. Kidney Int. 2019;96:37–47. doi: 10.1016/j.kint.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Brown EA, Blake PG, Boudville N, et al. International Society for Peritoneal Dialysis practice recommendations: prescribing high-quality goal-directed peritoneal dialysis. Perit Dial Int. 2020;40:244–253. doi: 10.1177/0896860819895364. [DOI] [PubMed] [Google Scholar]
- 8.Blake PG, Brown EA. Person-centered peritoneal dialysis prescription and the role of shared decision-making. Perit Dial Int. 2020;40:302–309. doi: 10.1177/0896860819893803. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine (US) Committee on Quality of Health Care in America, author. Crossing the quality chasm: a new health system for the 21st century. National Academies Press (US); Washington D.C.: 2001. [PubMed] [Google Scholar]
- 10.Watanyu P, Wannapat P, Laddaporn W, Kanin T, Lalana R. Customized versus conventional video counseling for peritoneal dialysis decision-making in patients with stage 5 chronic kidney disease under a PD-first policy: a randomized controlled study. Kidney Res Clin Pract. 2020;39:451–459. doi: 10.23876/j.krcp.20.035. [DOI] [PMC free article] [PubMed] [Google Scholar]