Highlights
-
•
Bee sting are the most common insect emergencies.
-
•
Often bee stings occur only with local allergic reactions.
-
•
A very rare case of brachial artery thrombosis after a honey bee sting is presented.
Keywords: Bee sting, Ischemic attack, Trombosis
Abstract
Introduction
Bee stings are the most common among insect emergencies.
Presentation of case
We present a 47-year-old male patient who was admitted to the emergency department with complaints of pallor, chills, numbness and bruising on the left palm one hour after a bee sting on his left leg, and a very rare case of brachial artery stenosis in Dopler ultrasonography.
Discussion
Often bee stings occur only with local allergic reactions; sometimes it can also cause myocardial infarction, pulmonary edema, bleeding, hemolytic anemia, and kidney disease and neurological manifestations. Side effects are generally thought to be related to the dose of this venom in these patients who are admitted to the emergency room with a bruise extending from the left hand to the arm after bee bites.
Conclusion
With this case presented, we wanted to emphasize that thrombosis may occur due to bee stings, albeit rarely, and doctors in emergency departments should recognize these very rare cases.
1. Introduction
Severe reactions may occur following bee stings and other insects. These reactions can be local or systemic. Local reactions are often characterized by pain, swelling, erythema, itching, and blister, and in general, type 1 mast cells surround the sting site and this is an anaphylactic reaction [1,2]. It differs in poisoning clinics due to honey bee or wasp. Most people are usually locally allergic, and after insertion, reactions including pain, redness, swelling occur in the area and usually disappear within a few hours. It can cause a wide variety of reactions such as bee sting, neurological findings, seizure, ischemic attack. However, in less frequent severe cases, myocardial infarction, pulmonary edema, bleeding, kidney failure, and life-threatening anaphylactic shock may also occur [3]. This case is presented in order to emphasize this very rare and non-literature situation that physicians should be aware of such a complication in order to make an emergency diagnosis and to start early treatment.
2. Presentation of case
A 47-year-old man without comorbid disease applied to the emergency room in the morning with a complaint of paleness, coldness, numbness and bruising in the left palm developing at 1 h after bee sting from his left leg. It was determined that the patient had a history of medication, a family history including genetic information or smoking status, and did not engage in beekeeping. The patient did not have any known chronic conditions. On examination, there were signs of coldness, partial parasy and ischemia on the left palm and fingers. Brachial radial and ulnar pulses were nonpalpable. Cardiac rhythms were in sinus rhythm. Doppler ultrasonography performed on the patient revealed stenosis in the brachial artery. Digital angiography was performed by entering the upper extremity femoral artery immediately. Vascular occlusion was observed after brachial bifurcation. It was seen that filling was made from collateral. After the brachial artery was reached with the catheter tip, the metalyse bolus was performed. Then 25,000 of heparin was given. Then, metalyse brachial trunktan was given again. Balloon angioplasty was performed on the radial artery. Then, it was observed that the filling of the brachial trunk and ulnar, radial artery increased. Increased flow in collaterals was observed (Fig. 1, Fig. 2, Fig. 3, Fig. 4). During peroperative angiography, it was observed that the vessel was opened and the blood supply increased. All these procedures were performed by the cardiovasculer surgeon. The patient was taken to cardiovascular intensive care after the operation. Heparin infusion of 1000 units / h iv was given for 24 h. Oral coumadin and aspirin (100 mg) were started on the patient who was taken into the service on the 2nd day. Cyanosis of the patient's arm disappeared and radial and ulnar artery pulses were palpable. There were no complications related to the intervention and the patient tolerated this procedure easily. The patient stated that his complaints disappeared after the treatment, he received after the operation. On the 10th day, the patient was discharged with necessary recommendations.
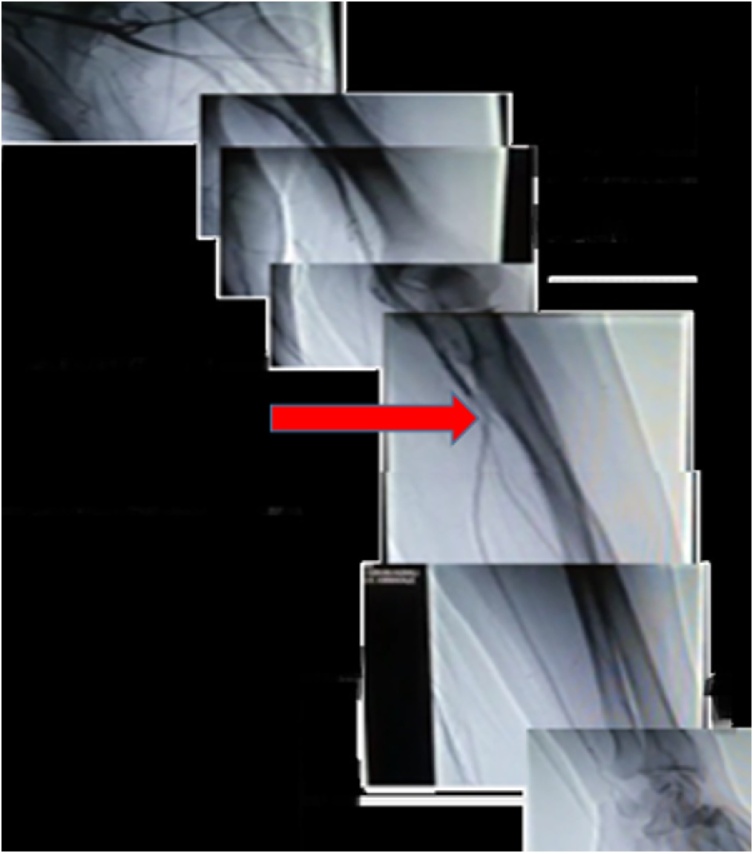
Fig. 1.
During the percutaneous intravascular angiographic intervention, the image taken before treatment showed that the flow in the brachial artery distal decreased due to occlusion.
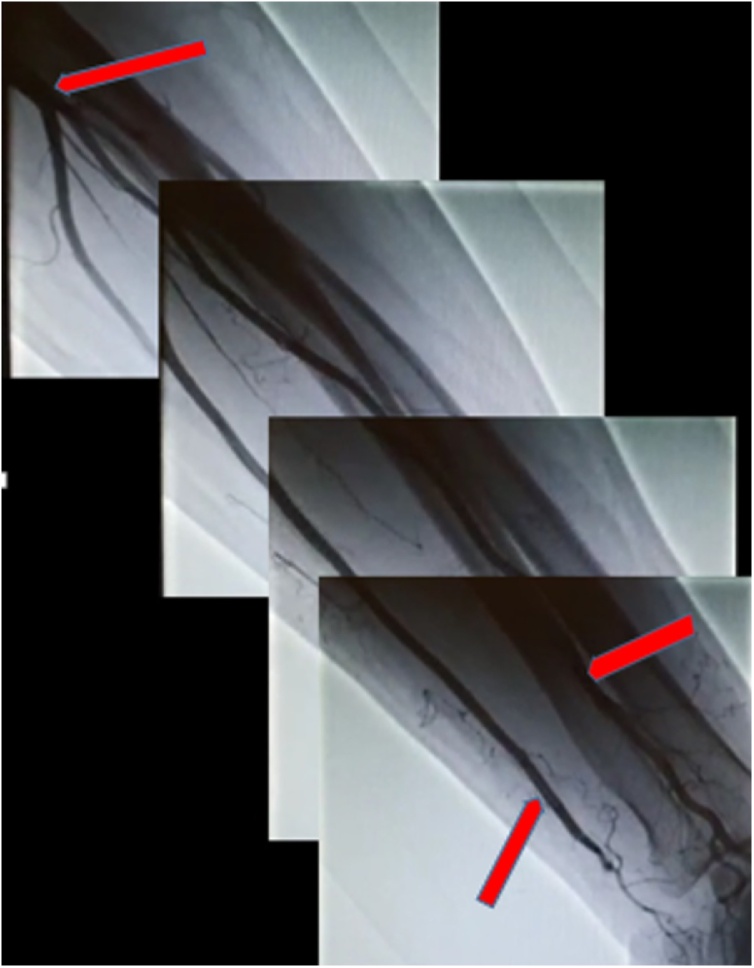
Fig. 2.
During percutaneous intravascular angiographic intervention, the image taken after treatment showed a significant increase in flow in the distal of the brachial artery.
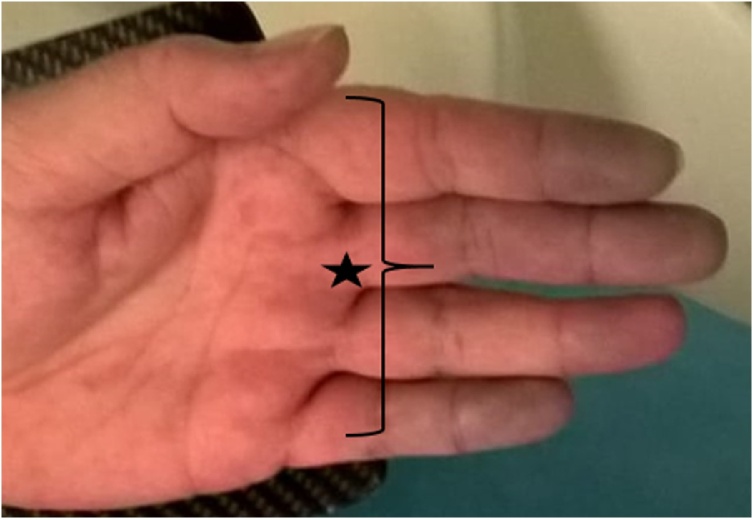
Fig. 3.
Cyanotic hand fingers are observed in the patient's emergency image taken before angiography.
Fig. 4.
In the image taken after the angiography of the patient, it is observed that the cyanosis in the toes disappeared.
3. Discussion
After an allergic reaction to bee sting; skin reaction symptoms (erythema, itching, urticaria and angioedema), respiratory system effects (larynx edema and bronchospasm) and cardiovascular (myocardial depression, hypotension and shock) and gastrointestinal tract events (nausea, vomiting, fecal incontinence) may occur [[4], [5], [6], [7]]. Consequently, severe anaphylactic shock may also lead to cerebral or myocardial ischemia accompanied by permanent sequelae [8]. The clinical picture of bee sting may rarely include diffuse alveolar bleeding, rhabdomyolysis, thrombocytopenic purpura, and vasculitis [[5], [6], [7], [8]]. Although our case did not have any history, it was found appropriate to present because vasospasm and thrombosis developed in the brachial artery following bee sting. This is a very rare clinical presentation of bee stings according to the literature. It contains various chemical components that contribute to the clinical picture such as bee venom, enzymes (phospholipases, hyaluronidase) and biological amines (histamine, serotonin, dopamine, norepinephrine and acetylcholine) (9). Our patient was admitted to the emergency department with a bruise extending from his left hand to his arm after bee stings and was generally thought to be related to the dose of this poison.
It is associated with a variety of reasons that can activate the pathways of hypersensitivity and induce the degranulation of mast cells. In the light of this information, the results of our case were interpreted as toxic findings. Providing life support should be a priority in cases of anaphylaxis. Oxygen delivery, adrenaline (0.5 mg intramuscularly in 1/1000 adult), intervals of 10−15 min, diphenhydramine, prednisolone, ranitidine, fluids or, if necessary, positive inotropes in the presence of bronchospasm. It is recommended to give 2 agonists and aminophylline [9]. In the emergency department, anti-allergic and prophylactic anti-anaphylactic treatments were applied in line with the treatment protocols recommended to our patient.
Phospholipase A2 is a key enzyme for the activation of the metabolism of arachidonic acid. During the metabolism of arachidonic acid, a number of cytokines and chemokines are released. These include leukotrienes via lipoxygenase and prostaglandins such as thromboxane via cyclooxygenase. These mediators have been accused in many clinical and laboratory studies to induce coronary artery spasm and / or acute myocardial infarction. This shows that the event in our case occurred thrombosis in the vascular bed and secondary vasospasm. Acute allergic attack after bee sting, such as Type II variant of Kounis syndrome, most likely caused plaque erosion or rupture, and vasospasm developed distal to the brachial artery after thrombosis formation [10]. Our study has been reported according to SCARE 2018 criteria [11]. We did not have any limitations in our approach to this case in terms of our treatment strategy, potential risks and complications.
4. Conclusion
The case presented here, albeit rarely, emphasizes the fact that thrombosis may occur due to bee stings and that emergency services should recognize these cases.
Note
Conflicts of Interest do not exist between authors. No funding source was included in this study. All procedures were done with prior permission from the hospital and the patient.
Conflicts of interest
There is no financial disclosures of the authors.
Author Mehmet Hüseyin Akgül declares that he has no conflict of interest.
Author Eldar Bağırov declares that he has no conflict of interest.
Sources of funding
There is no funding sources of the study.
Ethical approval
Ethics committee no approval was obtained. This studies is case report.
Consent
İnformed consent is take to patient.
Author contribution
All studies was wrote from to writer.
Registration of research studies
Not applicable.
Guarantor
The writer was guarantor. The name is Mehmet Hüseyin Akgül and Eldar Bağırov.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Truskinovsky A.M., Dick J.D., Hutchins G.M. Fatal infection after a bee sting. Clin. Infect. Dis. 2001;32:36–38. doi: 10.1086/318451. [DOI] [PubMed] [Google Scholar]
- 2.Ellis A.K., Day J.H. Clinical reactivity to insect stings. Curr. Opin. Allergy Clin. Immunol. 2005;5:349–354. doi: 10.1097/01.all.0000174159.55756.58. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal V., DCruz S., Sachdev A., Singh R., Kapoor V. Quadriparesis following wasp sting: an unusual reaction. Indian J. Med. Sci. 2005;59:117–119. [PubMed] [Google Scholar]
- 4.Lam S.M. Acute pulmonary hemorrhage following a honeybee sting: a case report. J. Microbiol. Immunol. Infect. 1998;31:133–136. [PubMed] [Google Scholar]
- 5.Bilo M.B., Bonifazi F. The natural history and epidemiology of insect venom allergy: clinical implications. Clin. Exp. Allergy. 2009;39:1467–1476. doi: 10.1111/j.1365-2222.2009.03324.x. [DOI] [PubMed] [Google Scholar]
- 6.Reisman R.E. Unusual reactions to insect stings. Curr. Opin. Allergy Clin. Immunol. 2005;5:355–358. doi: 10.1097/01.all.0000173782.35283.b6. [DOI] [PubMed] [Google Scholar]
- 7.Gandolfo G., Lambeau G., Lazdunski M., Gottesmann C. Effects on behaviour and EEG of single chain phospholipases A2 from snake and bee venoms injected into rat brain: search for a functional antagonism. Pharmacol. Toxicol. 1996;78:341–347. doi: 10.1111/j.1600-0773.1996.tb01386.x. [DOI] [PubMed] [Google Scholar]
- 8.Kounis N.G., Zavras G.M. Histamine-induced coronary artery spasm: the concept of allergic angina. Br. J. Clin. Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 9.Golden D.B., Valentine M.D., Kagey-Sobotka A. Regimens of hymenoptera venom immunotherapy. Ann. Intern. Med. 1980;5:620–624. doi: 10.7326/0003-4819-92-5-620. [DOI] [PubMed] [Google Scholar]
- 10.Nikolaidis L.A., Kounis N.G., Gradman A.H. Allergic angina and allergic myocardial infarction: a new twist on an old syndrome. Can. J. Cardiol. 2002;18:508–511. [PubMed] [Google Scholar]
- 11.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]