Abstract
Background
Although the potential effects of long-term and low-dose radiation exposure on physical health have attracted considerable attention, few systematic evaluations have been reported regarding the mental health of occupational groups. This study sought to investigate the effects of occupational radiation exposure on job stress and job burnout of medical radiation staff.
Material/Methods
Using cluster random sampling, a total of 1573 medical radiation workers were initially selected from 10 hospitals in Xinjiang, China, and 1396 valid questionnaires were finally collected. Job stress and job burnout were assessed using the Effort-Reward Imbalance (ERI) questionnaire and the Chinese Maslach Burnout Inventory (CMBI), respectively.
Results
The percentages of medical radiation staff experiencing job stress and job burnout were 53.08% and 63.32%, respectively. A statistically significant difference in job stress was observed in association with age, ethnicity, professional title, marital status, radiation work type, radiation working years, family history, hypertension, obesity, smoking, and drinking (P<0.05). A statistically significant difference in job burnout was observed in association with age, sex, ethnicity, professional title, educational level, marital status, job post, radiation work type, radiation working years, family history, hypertension, diabetes, and obesity (P<0.05). Female (odds ratio [OR]=0.75, 95% confidence interval [CI]: 0.58–0.98), senior professional title (OR=0.64, 95% CI: 0.43–0.96), and radiation work types of nuclear medicine (OR=0.15, 95% CI: 0.07–0.33) and radiotherapy (OR=0.54, 95% CI: 0.36–0.79) were protective factors, and job stress (OR=4.57, 95% CI: 3.55–5.91) was the risk factor for job burnout of medical radiation staff.
Conclusions
Medical radiation staff experience high levels of job stress and job burnout. The interventions of occupational physical examination, personal dose monitoring, occupational health education, and management optimization are recommended to relieve job stress and job burnout and enhance occupational health of medical radiation staff.
MeSH Keywords: Burnout, Professional; Medical Staff; Occupational Exposure; Radiation, Ionizing; Stress, Physiological
Background
Job stress refers to a pressure state in physiology and psychology when job demands extend beyond individual resources, needs, abilities, and knowledge [1]. Job burnout refers to physical or mental exhaustion caused by overwork or stress [2]. With a sustained rise in anxiety and mood disorders within professional populations, the effects of negative occupational factors on job stress and job burnout have drawn growing interest in the field of public health [3,4], and a large number of studies have confirmed that job stress occurs in many professions [5–7]. Job stress and job burnout have become problems that cannot be ignored in the field of occupational health.
Medical radiation workers belong to a special occupational group that has dual roles as health care workers and radiation workers. Health care workers are among the most stressed professionals owing to their risk of infections, high job demands, dissatisfied patients, and intensely competitive promotions [8,9]. More than half of US physicians were found to have at least one symptom of burnout, which was significantly higher than in the general population [10]. Furthermore, exposure to several physical, chemical, and biological risk factors exacerbate the psychological burden in certain occupational groups. Radiation is widely regarded as a physical risk factor with both deterministic and stochastic effects on physical health that increase the prevalence of cancer, cardiovascular diseases, and cataract [11,12]. With the improvement of health services and an aging population, the use of radioisotopes and ionizing radiation in diagnosis and treatment have steadily increased [13]. Global estimates show that approximately 3.6 billion radiation examinations on average were conducted annually from 2000 to 2007, and the use of diagnostic procedures involving radiation has more than doubled during the past 25 years in many countries [14–16]. Thus, medical radiation workers have gradually become the largest occupational group exposed to artificial radiation sources [17].
With the technical improvements of radiological equipment, radiation shielding, and radiation protection tools, high-dose occupational radiation exposure and occupational radiation accidents are uncommon [18,19]. The average annual effective dose of medical radiation workers in various countries is much lower than the annual effective dose limit of the international standards (20 mSv/y) [13,20]. However, radiation still has negative effects on people even under safety limits. The World Health Organization (WHO) and the International Labour Organization (ILO) have expressed concern about the potential effects of long-term and low-dose radiation exposure on physiological and psychological risks [21–23]. Psychosocial changes usually happen before physiological disorders are apparent, and there is often a lack of attention and intervention to address them [24]. Thus, the focus of occupational health management is not only on physical health, but also on mental health [25]. It is hence important to provide data on risk of stress and burnout for specific professional categories.
For medical radiation workers, some studies have found that job stress and the risk of anxiety or depression among radiographers and oncologists in hospitals were much higher than in the general population [26,27]. However, few studies have systematically evaluated job stress and job burnout of medical radiation staff in different work roles using validated questionnaires. In this study, a cross-sectional study was conducted to investigate job stress and job burnout of medical radiation staff in diagnostic radiology, nuclear medicine, radiotherapy, interventional radiology, and other types of work involving radiation in Xinjiang, China, to provide a theoretical basis for alleviating job stress and job burnout and thereby promoting occupational health of medical radiation staff.
Material and Methods
Participants
This cross-sectional study was carried out from May to October 2019. With the assistance of radiation protection managers in the hospitals, a total of 1573 medical radiation workers from 10 hospitals in Urumqi City, Changji Prefecture, Yili Prefecture, Aksu Region, Bayingolin Prefecture, Kashgar Area, and Hotan Region were initially selected using a cluster sampling method. An informed consent form explaining the questionnaire, survey purpose, and the principle of voluntary participation was distributed to the workers, and 1536 participants volunteered to complete the questionnaire survey. The study included 1506 participants who were licensed as radiation workers and had more than 1 year of occupational radiation exposure. By on-the-spot inquiry during distribution of questionnaires, workers with psychiatric disease or a family history of such diseases and those taking psychoactive drugs were excluded. Based on the inclusion and exclusion criteria, 1489 medical radiation workers were enrolled in this survey. A total of 1396 valid questionnaires were collected (93.75% response rate). Figure 1 presents a flowchart of participant selection.
Figure 1.
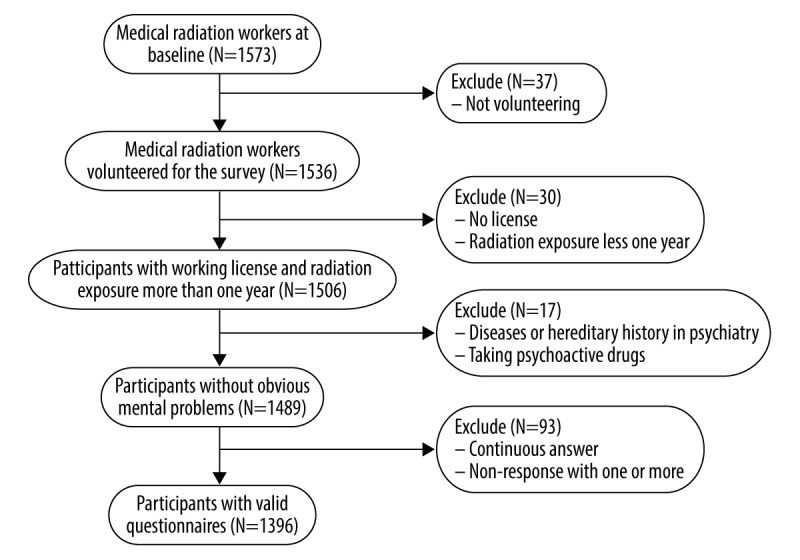
Definition of the study participants.
Research methods
General investigation
The general investigation included participants’ age, sex, ethnicity, professional title, educational level, marital status, job post, radiation work type, radiation working years, family history, smoking, drinking, hypertension, diabetes, and obesity.
Job stress
The Effort-Reward Imbalance (ERI) questionnaire has been widely used in assessing job stress [28,29]. This questionnaire was developed by Siegrist [30] on the basis of the imbalance between effort and reward causing a series of changes in physiological, psychological, cognitive functions, and body health. In our study, Cronbach’s alpha and split half reliability were used to test the internal consistency, and factor analysis was used to test the structure validity of ERI. The Cronbach α of ERI was 0.88, the split-half reliability coefficient was 0.78, and Kaiser-Meyer-Olkin statistics (KMO)=0.893. The ERI questionnaire consisted of 23 items with 3 dimensions: effort (E), reward (R), and overcommitment. Each item was assigned a score ranging from 1 (completely unfitting) to 5 (completely fitting). The ERI ratio was calculated by formula ERI=E/(R×C), and C was the ratio of the number of E items to the number of R items; C=6/11 in this paper. The ERI ratio at >1, 1, and <l indicated a high effort/low reward return, a balanced effort-reward return, and a low effort/high reward return, respectively. An ERI ratio >1 suggested job stress [31].
Job burnout
The Chinese Maslach Burnout Inventory (CMBI) was established by Li [32] on the basis of the Maslach Burnout Inventory and had good reliability and validity [33]. In our study, the Cronbach α of CMBI was 0.79, the split-half reliability coefficient was 0.81, and KMO=0.911. The CMBI consisted of 15 items in 3 dimensions: emotional exhaustion, depersonalization, and reduced personal accomplishment. Each item was assigned a score ranging from 1 (completely fitting) to 7 (completely unfitting). According to the critical values (emotional exhaustion ≥25, depersonalization ≥11, and reduced personal accomplishment ≥16), job burnout was divided into 4 levels: none (each dimension was lower than the critical value), mild (any 1 dimension was equal to or higher than the critical value), moderate (any 2 dimensions were equal to or higher than the critical values), and severe (3 dimensions were equal to or higher than the critical values) [34, 35].
Quality control
The pre-investigation was conducted before the formal investigation, and all the investigators were trained before the survey. Written informed consent was provided to each respondent to explain the purpose of the questionnaire survey and the principle of voluntary participation. The investigators distributed and collected questionnaires on site. Questionnaires with the continuous answers or nonresponse for 1 or more items were excluded.
Statistical analysis
All survey data were input into an Epidata3.1 database, and statistical analysis was performed using R (Version 3.4.4). The comparison of categorical data was conducted by the chi-squared test. Multivariate analysis was conducted by multiple logistics regression. The significance level (α) was set at 0.05.
Results
General demographic characteristics of medical radiation staff
Among the 1396 medical radiation staff, 796 were men (57.02%) and 600 were women (42.98%); 834 were doctors (59.74%), 208 were nurses (14.90%), 320 were radiographers (22.92%), and 34 held other positions (2.44%). The radiation work types involved diagnostic radiology (58.09%), nuclear medicine (2.72%), radiotherapy (10.53%), interventional radiology (23.21%), and others (5.44%), respectively. ERIs of ≤1 and >1 were 655 (46.92%) and 741 (53.08%). CMBIs of none, mild, moderate, and severe were 512 (36.68%), 459 (32.88%), 341 (24.43%), and 84 (6.02%) (Table 1).
Table 1.
Demographic characteristics of medical radiation staff.
| Items | Groups | N | Percentage (%) |
|---|---|---|---|
| Total | 1396 | ||
| Age | <30 | 311 | 22.28 |
| <40 | 571 | 40.90 | |
| <50 | 353 | 25.29 | |
| ≥50 | 161 | 11.53 | |
| Sex | Male | 796 | 57.02 |
| Female | 600 | 42.98 | |
| Ethnicity | Han | 995 | 71.28 |
| Minority | 401 | 28.72 | |
| Professional title | None or primary | 521 | 37.32 |
| Middle | 501 | 35.89 | |
| Senior | 374 | 26.79 | |
| Educational level | Junior college and below | 317 | 22.71 |
| Undergraduate | 683 | 48.93 | |
| Postgraduate | 396 | 28.37 | |
| Marital status | Unmarried | 275 | 19.70 |
| Married | 1090 | 78.08 | |
| Divorced or widowed | 31 | 2.22 | |
| Job post | Doctor | 834 | 59.74 |
| Nurse | 208 | 14.90 | |
| Radiographer | 320 | 22.92 | |
| Others | 34 | 2.44 | |
| Radiation work type | Diagnostic radiology | 811 | 58.09 |
| Nuclear medicine | 38 | 2.72 | |
| Radiotherapy | 147 | 10.53 | |
| Interventional radiology | 324 | 23.21 | |
| Others | 76 | 5.44 | |
| Radiation working years (years) | <5 | 422 | 30.23 |
| <10 | 465 | 33.31 | |
| <20 | 302 | 21.63 | |
| ≥20 | 207 | 14.83 | |
| Family history | No | 1292 | 92.55 |
| Yes | 104 | 7.45 | |
| Hypertension | No | 1224 | 87.68 |
| Yes | 172 | 12.32 | |
| Diabetes | No | 1360 | 97.42 |
| Yes | 36 | 2.58 | |
| Obesity | BMI <24 | 1205 | 86.32 |
| BMI ≥24 | 191 | 13.68 | |
| Smoking | No | 1000 | 71.63 |
| Yes | 396 | 28.37 | |
| Drinking | No | 622 | 44.56 |
| Yes | 774 | 55.44 | |
| ERI | No | 655 | 46.92 |
| Yes | 741 | 53.08 | |
| CMBI | None | 512 | 36.68 |
| Mild | 459 | 32.88 | |
| Moderate | 341 | 24.43 | |
| Severe | 84 | 6.02 |
Comparison of job stress of medical radiation staff in different populations
The results showed that job stress increased with age before 50 years old and then appeared to decline slightly (P<0.001). Job stress increased with advancements in professional title (P<0.001). Married and divorced or widowed individuals had higher levels of job stress compared with unmarried individuals (P<0.001). Job stress was the highest in the interventional radiology group among all the radiation work types (P=0.015). The variation in job stress based on working years was similar to that in age (P<0.001). There were statistically significant differences in job stress among medical radiation staff in association with family history (P<0.001), smoking (P=0.029), drinking (P=0.001), hypertension (P<0.001), and obesity (P<0.001) (Table 2).
Table 2.
Comparison of job stress in different populations.
| Items | N | ERI | Detection rate (%) | Chi-squared value | P-value | |
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Age | ||||||
| <30 | 311 | 222 | 89 | 28.62 | 116.202 | 0.000 |
| <40 | 571 | 259 | 312 | 54.64 | ||
| <50 | 353 | 107 | 246 | 69.69 | ||
| ≥50 | 161 | 67 | 94 | 58.39 | ||
| Sex | ||||||
| Male | 796 | 371 | 425 | 53.39 | 0.046 | 0.830 |
| Female | 600 | 284 | 316 | 52.67 | ||
| Ethnicity | ||||||
| Han | 995 | 447 | 548 | 55.08 | 5.261 | 0.022 |
| Minority | 401 | 208 | 193 | 48.13 | ||
| Professional title | ||||||
| None or primary | 521 | 323 | 198 | 38.00 | 76.313 | 0.000 |
| Middle | 501 | 195 | 306 | 61.08 | ||
| Senior | 374 | 137 | 237 | 63.37 | ||
| Educational level | ||||||
| Junior college and below | 317 | 165 | 152 | 47.95 | 4.570 | 0.102 |
| Undergraduate | 683 | 314 | 369 | 54.03 | ||
| Postgraduate | 396 | 176 | 220 | 55.56 | ||
| Marital status | ||||||
| Unmarried | 275 | 180 | 95 | 34.55 | 47.846 | 0.000 |
| Married | 1090 | 464 | 626 | 57.43 | ||
| Divorced or widowed | 31 | 11 | 20 | 64.52 | ||
| Job post | ||||||
| Doctor | 834 | 387 | 447 | 53.60 | 3.589 | 0.309 |
| Nurse | 208 | 89 | 119 | 57.21 | ||
| Radiographer | 320 | 163 | 157 | 49.06 | ||
| Others | 34 | 16 | 18 | 52.94 | ||
| Radiation work type | ||||||
| Diagnostic radiology | 811 | 387 | 424 | 52.28 | 12.307 | 0.015 |
| Nuclear medicine | 38 | 18 | 20 | 52.63 | ||
| Radiotherapy | 147 | 68 | 79 | 53.74 | ||
| Interventional radiology | 324 | 134 | 190 | 58.64 | ||
| Others | 76 | 48 | 28 | 36.84 | ||
| Radiation working years (years) | ||||||
| <5 | 422 | 294 | 128 | 30.33 | 153.461 | 0.000 |
| <10 | 465 | 213 | 252 | 54.19 | ||
| <20 | 302 | 84 | 218 | 72.19 | ||
| ≥20 | 207 | 64 | 143 | 69.08 | ||
| Family history | ||||||
| No | 1292 | 629 | 663 | 51.32 | 20.738 | 0.000 |
| Yes | 104 | 26 | 78 | 75.00 | ||
| Hypertension | ||||||
| No | 1224 | 601 | 623 | 50.90 | 18.279 | 0.000 |
| Yes | 172 | 54 | 118 | 68.60 | ||
| Diabetes | ||||||
| No | 1360 | 644 | 716 | 52.65 | 3.327 | 0.068 |
| Yes | 36 | 11 | 25 | 69.44 | ||
| Obesity | ||||||
| BMI <24 | 1205 | 595 | 610 | 50.62 | 20.647 | 0.000 |
| BMI ≥24 | 191 | 60 | 131 | 68.59 | ||
| Smoking | ||||||
| No | 1000 | 488 | 512 | 51.20 | 4.741 | 0.029 |
| Yes | 396 | 167 | 229 | 57.83 | ||
| Drinking | ||||||
| No | 622 | 323 | 299 | 48.07 | 10.944 | 0.001 |
| Yes | 774 | 332 | 442 | 57.11 | ||
Comparison of job burnout levels of medical radiation staff in different populations
The results showed that the total rate of job burnout among medical radiation staff was 63.32%, with mild and moderate levels of job burnout as the majority. Job burnout was higher for individuals with a middle professional title and an undergraduate degree than for those with other professional titles (P=0.022) and educational levels (P=0.047). Job burnout was higher for doctors than nurses and radiographers (P<0.001). Job burnout was the highest in the interventional radiology group and second highest in the diagnostic radiology group (P<0.001). Job burnout increased along with the number of radiation working years before 20 years and then decreased slightly (P<0.001). There were statistically significant differences in job burnout among medical radiation staff in association with family history (P=0.003), hypertension (P=0.002), diabetes (P<0.001), and obesity (P=0.001) (Table 3).
Table 3.
Comparison of job burnout levels in different populations.
| Items | N | CMBI | Detection rate (%) | Chi-squared value | P-value | |||
|---|---|---|---|---|---|---|---|---|
| None | Mild | Moderate | Severe | |||||
| Age | ||||||||
| <30 | 311 | 142 | 89 | 69 | 11 | 54.34 | 23.336 | 0.005 |
| <40 | 571 | 192 | 190 | 143 | 46 | 66.37 | ||
| <50 | 353 | 129 | 120 | 83 | 21 | 63.46 | ||
| ≥50 | 161 | 49 | 60 | 46 | 6 | 69.57 | ||
| Sex | ||||||||
| Male | 796 | 268 | 254 | 220 | 54 | 66.33 | 14.727 | 0.002 |
| Female | 600 | 244 | 205 | 121 | 30 | 59.33 | ||
| Ethnicity | ||||||||
| Han | 995 | 348 | 318 | 255 | 74 | 65.03 | 17.279 | 0.001 |
| Minority | 401 | 164 | 141 | 86 | 10 | 59.10 | ||
| Professional title | ||||||||
| None or primary | 521 | 210 | 150 | 133 | 28 | 59.69 | 14.770 | 0.022 |
| Middle | 501 | 169 | 181 | 111 | 40 | 66.27 | ||
| Senior | 374 | 133 | 128 | 97 | 16 | 64.44 | ||
| Educational level | ||||||||
| Junior college and below | 317 | 121 | 110 | 74 | 12 | 61.83 | 12.768 | 0.047 |
| Undergraduate | 683 | 237 | 219 | 171 | 56 | 65.30 | ||
| Postgraduate | 396 | 154 | 130 | 96 | 16 | 61.11 | ||
| Marital status | ||||||||
| Unmarried | 275 | 122 | 69 | 75 | 9 | 55.64 | 18.768 | 0.005 |
| Married | 1090 | 376 | 381 | 260 | 73 | 65.50 | ||
| Divorced or widowed | 31 | 14 | 9 | 6 | 2 | 54.84 | ||
| Job post | ||||||||
| Doctor | 834 | 298 | 297 | 201 | 38 | 64.27 | 39.269 | 0.000 |
| Nurse | 208 | 78 | 75 | 49 | 6 | 62.50 | ||
| Radiographer | 320 | 124 | 83 | 77 | 36 | 61.25 | ||
| Others | 34 | 12 | 4 | 14 | 4 | 64.71 | ||
| Radiation work type | ||||||||
| Diagnostic radiology | 811 | 279 | 281 | 183 | 68 | 65.60 | 61.867 | 0.000 |
| Nuclear medicine | 38 | 28 | 4 | 4 | 2 | 26.32 | ||
| Radiotherapy | 147 | 68 | 50 | 27 | 2 | 53.74 | ||
| Interventional radiology | 324 | 108 | 104 | 102 | 10 | 66.67 | ||
| Others | 76 | 29 | 20 | 25 | 2 | 61.84 | ||
| Radiation working years (years) | ||||||||
| <5 | 422 | 193 | 120 | 98 | 11 | 54.27 | 43.802 | 0.000 |
| <10 | 465 | 165 | 151 | 113 | 36 | 64.52 | ||
| <20 | 302 | 90 | 113 | 69 | 30 | 70.20 | ||
| ≥20 | 207 | 64 | 75 | 61 | 7 | 69.08 | ||
| Family history | ||||||||
| No | 1292 | 487 | 424 | 310 | 71 | 62.31 | 14.094 | 0.003 |
| Yes | 104 | 25 | 35 | 31 | 13 | 75.96 | ||
| Hypertension | ||||||||
| No | 1224 | 470 | 397 | 289 | 68 | 61.60 | 14.860 | 0.002 |
| Yes | 172 | 42 | 62 | 52 | 16 | 75.58 | ||
| Diabetes | ||||||||
| No | 1360 | 508 | 442 | 334 | 76 | 62.65 | 25.400 | 0.000 |
| Yes | 36 | 4 | 17 | 7 | 8 | 88.89 | ||
| Obesity | ||||||||
| BMI <24 | 1205 | 460 | 394 | 289 | 62 | 61.83 | 17.316 | 0.001 |
| BMI ≥24 | 191 | 52 | 65 | 52 | 22 | 72.77 | ||
| Smoking | ||||||||
| No | 1000 | 382 | 320 | 240 | 58 | 61.80 | 3.601 | 0.308 |
| Yes | 396 | 130 | 139 | 101 | 26 | 67.17 | ||
| Drinking | ||||||||
| No | 622 | 242 | 204 | 148 | 28 | 61.09 | 5.991 | 0.112 |
| Yes | 774 | 270 | 255 | 193 | 56 | 65.12 | ||
Exploration of factors related to job burnout of medical radiation staff
Multiple logistic regression analysis was used to evaluate the effects of general demographic characteristics and job stress on job burnout of medical radiation staff. All independent variables were stratified. The results showed that sex (P=0.034), senior professional title (P=0.029), radiation work type in nuclear medicine (P<0.001) and radiotherapy (P=0.002), and ERI (P<0.001) affected job burnout of medical radiation staff. Female, senior professional title, and radiation work types of nuclear medicine and radiotherapy were protective factors and ERI was a risk factor related to job burnout of medical radiation staff (Table 4).
Table 4.
Effects of general demographic characteristics and job stress on job burnout of medical radiation staff according to the results of multiple logistics regression.
| Variable | β (CI 95%) | S.E. | OR (CI 95%) | Wald | P-value |
|---|---|---|---|---|---|
| Intercept | −0.01 (−0.35, 0.34) | 0.18 | 0.99 (0.70, 1.40) | −0.043 | 0.966 |
| Sex | |||||
| Male | |||||
| Female | −0.29 (−0.55, −0.02) | 0.14 | 0.75 (0.58, 0.98) | −2.121 | 0.034 |
| Professional title | |||||
| None or primary | |||||
| Middle | −0.22 (−0.53, 0.10) | 0.16 | 0.80 (0.59, 1.10) | −1.342 | 0.179 |
| Senior | −0.45 (−0.85, −0.05) | 0.20 | 0.64 (0.43, 0.96) | −2.180 | 0.029 |
| Marital status | |||||
| Unmarried | |||||
| Married | 0.22 (−0.14, 0.58) | 0.18 | 1.25 (0.87, 1.79) | 1.211 | 0.226 |
| Divorced or widowed | −0.39 (−1.26, 0.47) | 0.44 | 0.68 (0.28, 1.60) | −0.891 | 0.373 |
| Job post | |||||
| Doctor | |||||
| Nurse | −0.05 (−0.43, 0.32) | 0.19 | 0.95 (0.65, 1.37) | −0.287 | 0.774 |
| Radiographer | −0.05 (−0.37, 0.27) | 0.16 | 0.95 (0.69, 1.31) | −0.325 | 0.745 |
| Others | 0.05 (−0.81, 0.91) | 0.44 | 1.05 (0.44, 2.49) | 0.116 | 0.908 |
| Radiation work type | |||||
| Diagnostic radiology | |||||
| Nuclear medicine | −1.92 (−2.71, −1.12) | 0.41 | 0.15 (0.07, 0.33) | −4.717 | 0.000 |
| Radiotherapy | −0.62 (−1.01, −0.23) | 0.20 | 0.54 (0.36, 0.79) | −3.136 | 0.002 |
| Interventional radiology | −0.05 (−0.36, 0.26) | 0.16 | 0.95 (0.70, 1.30) | −0.328 | 0.743 |
| Others | 0.12 (−0.44, 0.69) | 0.29 | 1.13 (0.64, 1.99) | 0.430 | 0.667 |
| Radiation working years (years) | |||||
| <5 | |||||
| <10 | 0.10 (−0.24, 0.43) | 0.17 | 1.11 (0.79, 1.54) | 0.570 | 0.568 |
| <20 | 0.29 (−0.13, 0.71) | 0.21 | 1.34 (0.88, 2.03) | 1.362 | 0.173 |
| ≥20 | 0.24 (−0.24, 0.73) | 0.25 | 1.27 (0.78, 2.07) | 0.976 | 0.329 |
| ERI | |||||
| No | |||||
| Yes | 1.52 (1.27, 1.78) | 0.13 | 4.57 (3.55, 5.91) | 11.685 | 0.000 |
Discussion
Occupational health is a diverse specialization of health care for improving the relationship between work and the physical and psychological health of employees [25]. Several studies have confirmed that job stress is a risk factor for adverse physiological function and psychological reaction [36,37]. Health care workers have been reported to experience high levels of job stress and job burnout in the United States, the United Kingdom, Australia, and Germany, and long working hours, rigid routines, emotional nature of patient demands, and heavy tasks in clinical and teaching were the main contributory factors [38–40]. With the continuous expansion of radiation technology and its application in medicine, increasingly more medical staff in different work types engage in radiation diagnostics and treatment. Long-term radiation exposure aggravates the psychological burden and thereby exacerbates the job stress and job burnout in this occupational group. Our research indicated that 53.08% and 63.32% of medical radiation staff experienced job stress and job burnout, and these rates were higher than those of nonmedical workers in China (copper-nickel miners, job stress 42.65% [41]; civil servants, job burnout 45.0% [42]) and physicians in the United States based a survey of 15 000 individuals (job burnout 42%) [43]. A survey of 1054 oncology physicians in the MENA showed a similar prevalence of burnout of around 68% [44]. Some studies suggested that requirements of the National Health Service, such as increasing volume of examinations, increased range of procedures but reduced waiting times, and multidisciplinary team work, have increased demands on the radiography departments, leading to more pressure on medical radiation workers [45].
This survey investigated job stress among medical staff in different types of radiation work. The results showed that medical radiation staff over 30 years old were more likely to develop job stress, and a similar development was observed for radiation working years, which was in agreement with a previous report of radiographers in Jordan [26]. Ahn et al. [46] showed that exposure to occupational hazards adversely affects individuals’ health and exacerbates job insecurity. Thus, the increase of radiation working years aggravated the occupational psychological burden of medical radiation staff. The job stress among individuals with middle and senior professional titles was significantly higher than among those with a primary professional title or below, which was similar to findings on other medical workers in the wider literature [47]. Like other general medical workers, medical radiation staff with a higher professional title are usually responsible for more difficult parts in operations, which require intense concentration and involve greater radiation exposure. Moreover, individuals with higher professional titles often have the additional workload of teaching and training clinical students, which adds to job stress [48]. Nurses have often been reported to have higher stress compared with other health professionals due to their lower hierarchy of decision-making in patient care, disruptions to circadian rhythms, and lower income [49]. Although nurses had higher job stress in our study, the difference among doctors, nurses, radiographers, and other positions was not statistically significant. As to the radiation work types, the interventional radiology group had the highest job stress, and the radiotherapy group came second. A study about radiographers and physiotherapists also found excess symptoms of stress [50]. In particular, Siegal et al. [51] found that frequent use of heavy lead aprons and imaging equipment in the interventional radiology group increased the risk for repetitive stress injury. The detection rate of job stress was significantly higher in those with family history, hypertension, or obesity. It was suggested that radiation workers might need more support in health care and protection education from employers.
This survey investigated job burnout levels among medical radiation staff. The results showed that medical staff who had longer radiation working years had a higher rate of job burnout, especially those with 10–20 years and more than 20 years. A survey of 15 000 physicians also reported the greatest incidence of burnout in the 45- to 54-year-old age group [43]. This finding can be explained by the fact that, these groups are at the peak of work productivity and practices and are more eager to increase personal income or seek promotion opportunities. However, meeting expectations is difficult and thereby increases the risk of job burnout, which was previously noted in similar studies [52]. The rates of job burnout among different job posts were all at a correspondingly high level. A study of radiation oncology departments in New Zealand also showed high scores in burnout among oncologists, therapists, nurses, and physicists [53]. In our study, the rate of job burnout in the other job positions was the highest, followed by doctors. For medical staff in the other job positions, they were not only responsible for medical work, but also many trivial duties in their own departments. As for doctors, Shanafelt et al. [54] confirmed that doctors experience symptoms of burnout at significantly higher rates compared with doctoral-level professionals in other fields. Doctors interact with colleagues or patients every day, but the focus of communication is almost always on the disease development, leaving them little time and few tools to relieve stress [8]. As to the radiation work types, interventional radiology was the largest group with job burnout, followed by diagnostic radiology. Radiation exposure is a recognized risk factor for medical staff performing fluoroscopically guided cardiovascular procedures due to the highest radiation dose in the application of diagnostic X-rays [12,55]. Long-term radiation exposure in bedside manipulation increased the psychological uneasiness of medical staff, resulting in the increase of job burnout. In the diagnostic radiology group, most workers were alone in an equipment operation room that was shielded by radiation protection but narrow in space and poor in air circulation. Chronic diseases, such as hypertension, diabetes, and obesity, could cause changes in the body’s functioning that could make workers feel more tired at work [56].
The results of multiple logistic regression analysis showed that the risk of job burnout for women and individuals with a senior professional title were 0.75 and 0.64 times those of men and individuals with a primary professional title and below, respectively. This could be attributed to women being more likely to relieve stress by communicating with others, and people with senior professional titles having a better ability to control their work [57]. The risks of job burnout in the nuclear medicine group and the radiotherapy group were 0.15 times and 0.54 times that of the diagnostic radiology group. A lower burnout rate among radiation oncologists compared with diagnostic radiologists was also reported by Harolds et al. [58]. This finding could be explained by the fact that compared with the diagnostic radiology group, medical physicists of nuclear medicine and radiotherapy were highly involved in the performance of individual diagnosis and treatment, and played a leading role in the implementation and safe utilization of advanced technologies [59,60], which enhanced job control and accomplishment. In this study, the risk of job burnout was 4.57 times higher among medical radiation staff with job stress. A high stress level can be a predictor of burnout at the workplace. Similar results have been reported for emergency room physicians, anesthesiologists, general internists, general surgeons, radiologists, oncologists, and even medical students and residents [61]. The excess stress and high responsibility of medical staff have been shown to lead to mismanagement of their psychological and physiological health and to cause adverse physiological function and psychological reaction, resulting in medical errors, job attrition, lack of professionalism, and even substance abuse [62].
Effective prevention and intervention of occupational health management for medical radiation staff should be implemented from social medicine and occupational medicine. First, strengthening occupational physical examination, personal dose monitoring, and continuing education are beneficial for improving the coping ability and thereby reducing the job stress of medical radiation staff. Second, employers should promote education about occupational health to enhance workers’ awareness about self-protection in long-term occupational radiation exposure. Third, the safety of the working environment, reasonable arrangement of workload and working hours, and optimization of the promotion system should be taken into consideration to improve the job satisfaction of medical radiation staff.
The present study has some limitations that could be addressed in future studies. First, because of the imbalance of economic development, the distribution of hospitals and medical radiation staff were uneven, resulting in a larger number of participants in relatively developed areas. In addition, the sample sizes of all the radiation work types were not uniform due to the different workload of radiation diagnosis and treatment, which may cause bias in groups with small sample size. Second, the cross-sectional investigation cannot prove causality between variables; the relationship between the factors and job burnout need further investigation. Third, some influencing factors, such as radiation dose value, frequency of shift work, and monthly income, were not considered in this study. Finally, further study will be conducted to compare the status of medical staff who are exposed to and not exposed to occupational radiation in the same department.
Conclusions
Health care providers around the world are under pressure and face increasing expectations and requirements to provide evidence-based and high-quality health service. Although the development and application of radiation medicine has brought great benefits for the prevention and treatment of diseases, the mental health of medicine radiation staff, who are one of the most stressed professional groups as well as the largest occupational group exposed to artificial radiation sources, should get more attention not only for the demands of occupational health management, but also for the safe use of radioisotopes and ionizing radiation. Similar levels of job stress and job burnout of medical radiation staff were demonstrated in Xinjiang, China, compared with many other countries. Radiation working types and increasing radiation working years contributed to high job stress and job burnout, and job stress significantly aggravated job burnout of medical radiation staff. Familiarity with the factors influencing mental health can be conductive to developing strategies from both social and occupational medicine for promoting health and wellness of medical radiation staff.
Footnotes
Source of support: The study was funded by the National Natural Science Foundation of China (grant number: 8176120048) and the Xinjiang Uygur Autonomous Region’s 13th Five-Year Plan (key disciplines of public health and preventive medicine; 99-11091113404#)
References
- 1.Desouky D, Allam H. Occupational stress, anxiety and depression among Egyptian teachers. J Epidemiol Glob Health. 2017;7(3):191–98. doi: 10.1016/j.jegh.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ofei-Dodoo S, Kellerman R, Gilchrist K, et al. Burnout and quality of life among active member physicians of the medical society of Sedgwick County. Kansas J Med. 2019;12(2):33–39. [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang Y, Cui C, Ge H, et al. Effect of 5-HT2A receptor polymorphisms and occupational stress on self-reported sleep quality: A cross-sectional study in Xinjiang, China. Sleep Med. 2016;20:30–36. doi: 10.1016/j.sleep.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Fontalba-Navas A, Lucas-Borja ME, Gil-Aguilar V, et al. Incidence and risk factors for post-traumatic stress disorder in a population affected by a severe flood. Public Health. 2017;144:96–102. doi: 10.1016/j.puhe.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Singh S, Sharma T. Effect of adversity quotient on the occupational stress of IT managers in India. Procedia Comput Sci. 2017;122:86–93. [Google Scholar]
- 6.Stanley IH, Boffa JW, Smith LJ, et al. Occupational stress and suicidality among firefighters: Examining the buffering role of distress tolerance. Psychiatry Res. 2018;266:90–96. doi: 10.1016/j.psychres.2018.05.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehrabian F, Baghizadeh K, Alizadeh I. The relationship between empowerment, occupational burnout, and job stress among nurses in Rasht Medical Education Centers: A dataset. Data Brief. 2018;20:1093–98. doi: 10.1016/j.dib.2018.08.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson AR, Jayappa R, James M, et al. Do low self-esteem and high stress lead to burnout among health-care workers? Evidence from a tertiary hospital in Bangalore, India. Saf Health Work. 2020;11(3):347–52. doi: 10.1016/j.shaw.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khamisa N, Peltzer K, Ilic D, et al. Effect of personal and work stress on burnout, job satisfaction and general health of hospital nurses in South Africa. Health SA Gesondheid. 2017;22:252–58. [Google Scholar]
- 10.DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: A systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384–408. doi: 10.1016/j.mayocpiqo.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Badawy MK, Deb P, Chan R, et al. A review of radiation protection solutions for the staff in the cardiac catheterisation laboratory. Heart Lung Circ. 2016;25(10):961–67. doi: 10.1016/j.hlc.2016.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Stewart FA, Hoving S, Russell NS. Vascular damage as an underlying mechanism of cardiac and cerebral toxicity in irradiated cancer patients. Radiat Res. 2010;174(6b):865–69. doi: 10.1667/RR1862.1. [DOI] [PubMed] [Google Scholar]
- 13.Nassef MH, Kinsara AA. Occupational radiation dose for medical workers at a university hospital. J Taibah Univ Sci. 2018;11(6):1259–66. [Google Scholar]
- 14.Ahmed TAN, Taha S. Radiation exposure, the forgotten enemy: Toward implementation of national safety program. Egypt Heart Journal. 2017;69(1):55–62. doi: 10.1016/j.ehj.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brady Z, Cain TM, Johnston PN. Paediatric CT imaging trends in Australia. J Med Imaging Radiat Oncol. 2011;55(2):132–42. doi: 10.1111/j.1754-9485.2011.02242.x. [DOI] [PubMed] [Google Scholar]
- 16.Leuraud K, Richardson DB, Cardis E, et al. Ionising radiation and risk of death from leukaemia and lymphoma in radiation-monitored workers (INWORKS): An international cohort study. Lancet Haematol. 2015;2(7):276–81. doi: 10.1016/S2352-3026(15)00094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dauer LT. Exposed medical staff: challenges, available tools, and opportunities for improvement. Health Phys. 2014;106(2):217–24. doi: 10.1097/HP.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 18.Etzel R, König AM, Keil B, et al. Effectiveness of a new radiation protection system in the interventional radiology setting. Eur J Radiol. 2018;106:56–61. doi: 10.1016/j.ejrad.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Ria F, Bergantin A, Vai A, et al. Awareness of medical radiation exposure among patients: A patient survey as a first step for effective communication of ionizing radiation risks. Physica Medica. 2017;43:57–62. doi: 10.1016/j.ejmp.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Vitalija S, Vydmantas A, Juozas K, et al. Occupational exposure of medical radiation workers in Lithuania, 1950–2003. Radiat Prot Dosim. 2008;130:239–43. doi: 10.1093/rpd/ncm490. [DOI] [PubMed] [Google Scholar]
- 21.Gerić M, Popić J, Gajski G, et al. Cytogenetic status of interventional radiology unit workers occupationally exposed to low-dose ionising radiation: A pilot study. Mutat Res Genet Toxicol Environ Mutagen. 2019;843:46–51. doi: 10.1016/j.mrgentox.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 22.Dalah EZ, Mahdi O, Elshami W, et al. Occupational doses to cardiologists performing fluoroscopically-guided procedures. Radiat Phys Chem. 2018;153:21–26. [Google Scholar]
- 23.Salomaa S, Averbeck D, Ottolenghi A, et al. European low-dose radiation risk research strategy: future of research on biological effects at low doses. Radiat Prot Dosim. 2015;164(1–2):38–41. doi: 10.1093/rpd/ncu350. [DOI] [PubMed] [Google Scholar]
- 24.Pan C, Zhao J. Comprehensive evaluation on occupational hazards for steel rolling workshops with the interactive effects of multiple hazards. Procedia Eng. 2012;43:143–49. [Google Scholar]
- 25.de Jager N, Nolte AGW, Temane A. Strategies to facilitate professional development of the occupational health nurse in the occupational health setting. Health SA Gesondheid. 2016;21:261–70. [Google Scholar]
- 26.Ashong GGNA, Rogers H, Botwe BO, Anim-Sampong S. Effects of occupational stress and coping mechanisms adopted by radiographers in Ghana. Radiography. 2016;22:112–17. [Google Scholar]
- 27.Alhasan M, Abdelrahman M, Alewaidat H, et al. Work-related stress, musculoskeletal disorder complaints, and stress symptoms among radiographers in the northern part of Jordan. J Med Imaging Radiat Sci. 2014;45(3):291–98. doi: 10.1016/j.jmir.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Inoue M, Tsurugano S, Yano E. Job stress and mental health of permanent and fixed-term workers measured by effort-reward imbalance model, depressive complaints, and clinic utilization. J Occup Health. 2011;53:93–101. doi: 10.1539/joh.l10098. [DOI] [PubMed] [Google Scholar]
- 29.van der Meij L, Gubbels N, Schaveling J, et al. Hair cortisol and work stress: Importance of workload and stress model (JDCS or ERI) Psychoneuroendocrinology. 2018;89:78–85. doi: 10.1016/j.psyneuen.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 30.Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27–41. doi: 10.1037//1076-8998.1.1.27. [DOI] [PubMed] [Google Scholar]
- 31.Siegrist J, Wege N, Pühlhofer F, et al. A short generic measure of work stress in the era of globalization: Effort-reward imbalance. Int Arch Occup Environ Health. 2009;82:1005–13. doi: 10.1007/s00420-008-0384-3. [DOI] [PubMed] [Google Scholar]
- 32.Li YX, Wu MZ. [A structural study of job burnout]. Psychol Sci. 2005;28:454–47. [in Chinese] [Google Scholar]
- 33.Wang SX, Ding GF, Gu XX. [Job burnout and job performance in uncivilized behavior targets]. Chin Ment Health J. 2014;28(7):535–40. [in Chinese] [Google Scholar]
- 34.Maslach C, Jackson S, Leiter M. MBI Maslach burnout inventory manual. 3rd ed. Mountain View, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 35.Li Y. [Relationship among locus of control, coping style and job burnout of nurses]. China J Health Psychol. 2007;15(6):532–33. [in Chinese] [Google Scholar]
- 36.Poitras VJ, Pyke KE. The impact of acute mental stress on vascular endothelial function: Evidence, mechanisms and importance. Int J Psychophysiol. 2013;88(2):124–35. doi: 10.1016/j.ijpsycho.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 37.Zhang W. Causation mechanism of coal miners’ human errors in the perspective of life events. Int J Mining Sci Tech. 2014;24(4):581–86. [Google Scholar]
- 38.Lenthall S, Wakerman J, Dollard MF, et al. Reducing occupational stress among registered nurses in very remote Australia: A participatory action research approach. Collegian. 2018;25:181–91. [Google Scholar]
- 39.Akroyd D, Caison A, Adams R. Patterns of burnout among U.S. radiographers. Radiol Tech. 2002;73(1):215–23. [Google Scholar]
- 40.Siegrist J, Shackelton R, Link C, et al. Work stress of primary care physicians in the US, UK and German health care systems. Soc Sci Med. 2010;71(2):298–304. doi: 10.1016/j.socscimed.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li Y, Sun X, Ge H, et al. The status of occupational stress and its influence the quality of life of copper-nickel miners in Xinjiang, China. Int J Environ Res Public Health. 2019;16(3):353–62. doi: 10.3390/ijerph16030353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guan S, Xiaerfuding X, Ning L, et al. Effect of job strain on job burnout, mental fatigue and chronic diseases among civil servants in the Xinjiang Uygur Autonomous Region of China. Int J Environ Res Public Health. 2017;14:872. doi: 10.3390/ijerph14080872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nicholls M. Cardiologists and the burnout scenario. Eur Heart J. 2019;40(1):5–6. doi: 10.1093/eurheartj/ehy788. [DOI] [PubMed] [Google Scholar]
- 44.Abusanad AM, Bensalem A, Shash E, et al. 1579P Burnout among oncology professionals in the Middle East and North Africa (MENA) Ann Oncol. 2020;31(Suppl 4):S959. [Google Scholar]
- 45.Verrier W, Harvey J. An investigation into work related stressors on diagnostic radiographers in a local district hospital. Radiography. 2010;16:115–24. [Google Scholar]
- 46.Ahn J, Kim NS, Lee BK, et al. Relationship of occupational category with risk of physical and mental health problems. Saf Health Work. 2019;10(4):504–11. doi: 10.1016/j.shaw.2019.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong AMF. Beyond burnout: Looking deeply into physician distress. Can J Ophthalmol. 2020;55(3 Suppl 1):7–16. doi: 10.1016/j.jcjo.2020.01.014. [DOI] [PubMed] [Google Scholar]
- 48.Chingarande GR, Ndlovu B. The prevalence and antecedents of occupational stress among radiographers in Zimbabwe: Interplay of economics and culture. International Journal of Medical Research & Health Sciences. 2013;2(2):233. [Google Scholar]
- 49.Ferreira B, Maharaj S, Simpson A, et al. The metabolic role of depression and burnout in nurses. Transl Metab Syn Res. 2020;3:9–11. [Google Scholar]
- 50.Tarlo SM, Liss GM, Greene JM, et al. Work-attributed symptom clusters (darkroom disease) among radiographers versus physiotherapists: Associations between self-reported exposures and psychosocial stressors. Am J Ind Med. 2004;45:513–21. doi: 10.1002/ajim.20015. [DOI] [PubMed] [Google Scholar]
- 51.Siegal DS, Levine D, Siewert B, et al. Repetitive stress symptoms among radiology technologists: Prevalence and major causative factors. J Am Coll Radiol. 2010;7(12):956–60. doi: 10.1016/j.jacr.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 52.Lee CY, Wua JH, Du JK. Work stress and occupational burnout among dental staff in a medical center. J Dent Sci. 2019;14(3):295–301. doi: 10.1016/j.jds.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jasperse M, Herst P, Dungey G. Evaluating stress, burnout and job satisfaction in New Zealand radiation oncology departments. Eur J Cancer Care. 2014;23(1):82–88. doi: 10.1111/ecc.12098. [DOI] [PubMed] [Google Scholar]
- 54.Shanafelt TD, Sinsky C, Dyrbye LN, et al. Burnout among physicians compared with individuals with a professional or doctoral degree in a field outside of medicine. Mayo Clin Proc. 2019;94(3):549–51. doi: 10.1016/j.mayocp.2018.11.035. [DOI] [PubMed] [Google Scholar]
- 55.Andreassi MG, Piccaluga E, Guagliumi G, et al. Occupational health risks in cardiac catheterization laboratory workers. Circ Cardiovasc Interv. 2016;9(4):e003273. doi: 10.1161/CIRCINTERVENTIONS.115.003273. [DOI] [PubMed] [Google Scholar]
- 56.Lu Y, Zhang Z, Gao S, et al. The status of occupational burnout and its influence on the psychological health of factory workers and miners in Wulumuqi, China. Biomed Res Int. 2020;2020 doi: 10.1155/2020/6890186. 6890186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Paiva LC, Canário AC, China EL, et al. Burnout syndrome in health-care professionals in a university hospital. Clinics. 2017;72(5):305–9. doi: 10.6061/clinics/2017(05)08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harolds JA, Parikh JR, Bluth EI, et al. Burnout of radiologists: Frequency, risk factors, and remedies: A report of the ACR Commission on Human Resources. J Am Coll Radiol. 2016;13(4):411–16. doi: 10.1016/j.jacr.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 59.Franco P, Tesio V, Bertholet J, et al. Professional quality of life and burnout amongst radiation oncologists: the impact of alexithymia and empathy. Radiother Oncol. 2020;147:162–68. doi: 10.1016/j.radonc.2020.05.017. [DOI] [PubMed] [Google Scholar]
- 60.Tella MD, Tesio V, Bertholet J, et al. Professional quality of life and burnout among medical physicists working in radiation oncology: The role of alexithymia and empathy. Phys Imaging in Radiat Oncol. 2020;15:38–43. doi: 10.1016/j.phro.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yates SW. Physician stress and burnout. Am J Med. 2020;133(2):160–64. doi: 10.1016/j.amjmed.2019.08.034. [DOI] [PubMed] [Google Scholar]
- 62.Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–51. doi: 10.1097/ACM.0000000000000134. [DOI] [PubMed] [Google Scholar]


