A 62-year-old patient with a medical history of dyslipidemia, arterial hypertension and bipolar disorder was admitted to our intensive care unit on March 31th 2020 for a respiratory distress syndrome related to SARS-CoV-2 pneumonia. Symptoms appeared 10 days earlier with fever and cough. The SARS-CoV-2 nasopharyngeal swab PCR was positive and a thoracic CT scan confirmed pneumonia with extensive ground-glass opacities and areas of consolidation. Mechanical ventilation with orotracheal intubation was initiated on April 4th with rapid improvement of respiratory parameters and no requirement for prone-position ventilation. However, intubation was complicated of multiple ventilation-associated pneumonia with favorable evolution upon treatment with antibiotics. Finally, weaning from mechanical ventilation was possible after tracheotomy with a total of 24 days of invasive ventilation.
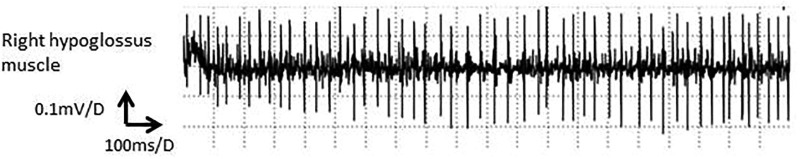
Afterwards, we noted dysarthria and swallowing difficulties. A nasofibroscopy found a paralysis of the left vocal cord revealing left recurrent laryngeal nerve paralysis. Furthermore, neurologic evaluation revealed a complete inability to move and protrude the tongue (Video 1) with no evidence of other central or cranial nerve involvement. A diagnosis of bilateral hypoglossal nerve paralysis was considered. A brain MRI and cervical CT scan found no signs for a central cause or extrinsic nerve compression. Comprehensive blood tests did not suggest among others an autoimmune etiology. Cerebral spinal fluid was not analyzed. Electromyographic (EMG) evaluation of genioglossus muscles using a needle electrode via the submental route found no spontaneous activity and no active contraction. Five months later, while swallowing and dysarthria improved, tongue paralysis remained. A second needle EMG found no spontaneous activity but a neurogenic recruitment pattern with polyphasic motor units (Fig. 1 ) suggesting re-innervation signs without active denervation.
Clinical manifestation of bilateral Tapia syndrome in our patient. The video shows an inability to protrude or laterally move the tongue, and no lateral deviation of the tongue at rest. Moreover, a flaccid tongue is noted when manipulated by a wooden tongue depressor.
Fig. 1.
EMG of the right genioglossus muscle showing neurogenic abnormality. Electromyographic (EMG) evaluation of genioglossus muscles using a needle electrode via the submental route found no spontaneous activity but a neurogenic recruitment pattern with polyphasic motor units suggesting re-innervation signs without active denervation.
We herein report a case of post-orotracheal intubation complication that is known under the name of Tapia syndrome and that consists of a synchronous affection of the X and XII nerves occurring mainly after orotracheal intubation (Coninckx et al., 2015). While unilateral XII nerve paralysis is often described, in particular in prolonged lateral flexion situations such as in prone-position ventilation, bilateral paralysis has only been rarely reported (Turan et al., 2012). The frequency of such complications is expected to rise during the SARS-CoV-2 pandemic, because of prolonged intubation and repeated prone positioning. Prior to the publication of this report, one group reported a case of unilateral Tapia syndrome in a 62-year old male patient who was intubated for 16 days and required prone-positioning in context of acute respiratory distress syndrome related to a SARS-CoV-2 infection (Decavel et al., 2020). The authors concluded that the Tapia syndrome in their case was due to a traumatic etiology, such as stretching of the nerves during lateral head flexion. Our patient did not require prone-position ventilation but underwent intubation for a long period of 24 days and paralysis could be the result of direct nerve compression against cervical bones; another attractive etiology is related to SARS-CoV-2 tropism (Puelles et al., 2020). Indeed, SARS-CoV-2 has been reported to infect many different organs including the central and the peripheral nervous system (Paterson et al., 2020), resulting in a variety of neurological syndromes reported in the literature. Moreover, immune-mediated neuropathology has also been suggested (Guilmot et al., 2020).
Overall, our case provides evidence for lower cranial neuropathy post-intubation in the context of critical SARS-CoV-2, which may have resulted from traumatic and/or SARS-CoV-2-mediated toxicity. This report is an additional contribution to the literature supporting a potential neurological tropism for SARS-CoV-2 (Pezzini and Padovani, 2020), and underpins the need for a systematic and thorough neurological evaluation of SARS-CoV-2 patients. Early recognition of SARS-CoV-2-related neurological syndromes is crucial for the development of adapted rehabilitation procedures that may accelerate recovery and improve life quality.
1. Consent
Written informed consent and permission to reproduce the photographs was obtained from the patient.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We acknowledge all health-care workers involved in the diagnosis and treatment of patients in Avicennes University Hospital, especially in the intensive care department.
References
- Coninckx M., Cardoen S., Hemelsoet D. Tapia’s syndrome in the intensive care unit: a rare cause of combined cranial nerve palsy following intubation. Acta Neurol Belg. 2015;115:533–537. doi: 10.1007/s13760-015-0500-6. [DOI] [PubMed] [Google Scholar]
- Decavel P., Petit C., Tatu L. Tapia syndrome at the time of the COVID-19 pandemic: Lower cranial neuropathy following prolonged intubation. Neurology. 2020;95:312–313. doi: 10.1212/WNL.0000000000010011. [DOI] [PubMed] [Google Scholar]
- Guilmot A., Maldonado Slootjes S., Sellimi A., Bronchain M., Hanseeuw B., Belkhir L. Immune-mediated neurological syndromes in SARS-CoV-2-infected patients. J Neurol. 2020 doi: 10.1007/s00415-020-10108-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson RW, Group for the UQSNH for N and NC-19 S, Brown RL, Group for the UQSNH for N and NC-19 S, Benjamin L, Group for the UQSNH for N and NC-19 S, et al. The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain 2020;143:3104–20. https://doi.org/10.1093/brain/awaa240. [DOI] [PMC free article] [PubMed]
- Pezzini A., Padovani A. Lifting the mask on neurological manifestations of COVID-19. Nat Rev Neurol. 2020;16:636–644. doi: 10.1038/s41582-020-0398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puelles V.G., Lütgehetmann M., Lindenmeyer M.T., Sperhake J.P., Wong M.N., Allweiss L. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020;383:590–592. doi: 10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan I., Yildirim Z.K., Tan H. Bilateral tapia syndrome secondary to oropharyngeal intubation. J Neurosurg Anesthesiol. 2012;24:78. doi: 10.1097/ANA.0b013e31823769ef. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Clinical manifestation of bilateral Tapia syndrome in our patient. The video shows an inability to protrude or laterally move the tongue, and no lateral deviation of the tongue at rest. Moreover, a flaccid tongue is noted when manipulated by a wooden tongue depressor.