To the editor,
Last February, Europe was affected by the first wave of the COVID-19 pandemic. Now a second outbreak has begun. Albeit a close relationship between the pandemic trend and the incidence of out-of-hospital cardiac arrest (OHCA) has been documented during the first surge in different countries such as Italy1, 2 the United States3, 4 and France,5 some elements still remain unclarified.
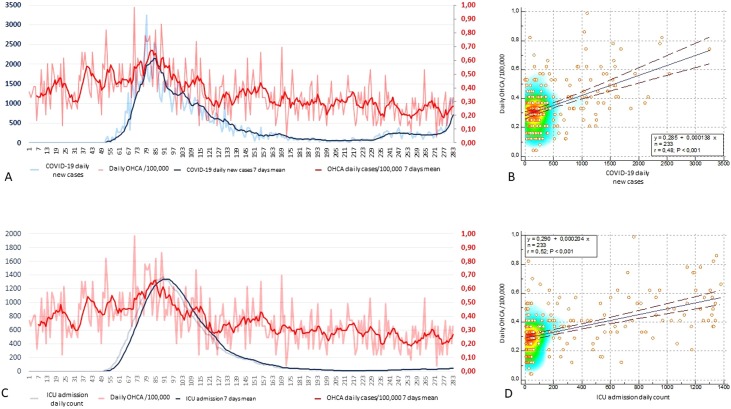
Our aims were (1) to confirm the correlation between the incidence of OHCA and COVID-19 across a longer time period including the downward phase of the pandemic; (2) to compare the incidence of OHCA in the post- and pre-pandemic peak and (3) to verify whether the incidence OHCA correlated more closely with daily COVID-19 diagnoses or with the rate of ICU admissions. We considered all events of OHCA enrolled in the out-of-hospital cardiac arrest register of the Lombardy region (Lombardia CARe; ClinicalTrials.gov Identifier: NCT03197142) from January 1st, 2020 to October 9th, 2020 that have occurred in the provinces of Pavia, Lodi, Cremona, Mantua and Varese (total area 9061 km2; total population of 2,435,939 inhabitants). The daily new cases of COVID-19 in the entire Lombardy region, as well as the daily count of COVID patients admitted in the intensive care units (ICU), were collected from National Department of Civil Protection (http://www.protezionecivile.gov.it/). During the study period, 2488 OHCAs occurred and resuscitation was attempted in 1629 of them (65.5%). The median age was 78 years (IQR 66–86 years); the event occurred at home in 1392 (85.5%); a medical aetiology was found in 1519 (93%); the event was witnessed in 756 (46.4%); the rhythm was non-shockable in 1393 (85.5%) and bystander CPR occurred in 519 (32%). As shown in Fig. 1 , the trend of OHCA has followed the trend of the pandemic during both the ascending and the descending phase. A statistically significant correlation was found across the 283 days of observation, reinforcing the deep relationship between the pandemic and OHCA incidence. The median daily incidence of OHCA after the first peak (from day 150 onwards) was lower than before the rising phase (before day 50) [0.3 (IQR 0.2−0.4) vs 0.5 (IQR 0.3−0.6), p < 0.001] and was aligned with 2019 [0.3 (IQR 0.3−0.4)]. This suggests an absence of delayed disease- or pandemic-related effects able to maintain the higher rates of OHCA during the low incidence phase after the first pandemic peak. Finally, the daily rate of OHCA correlated significantly both with the daily number of new COVID-19 cases and with the daily count of ICU patients, with a slightly stronger correlation with the latter. However, the number of daily positive cases may depend more on the number of pharyngeal swabs performed in the geographic region under investigation than on the real severity of the disease, which is likely better expressed by the number of patients requiring an ICU admission.
Fig. 1.
Panel A shows the daily OHCA incidence/100,000 (light red) and its 7-days mean (red) together with COVID-19 daily new cases (light blue) and its 7-days mean (blue) and their statistical correlation is provided in panel B. Panel C depicts the daily OHCA incidence/100,000 (light red) and its 7-days mean (red) together with the daily count of ICU patients (light blue) and its 7-days mean (blue) and their statistical correlation is provided in panel D.
In conclusion, the correlation between OHCA and COVID-19 pandemic has been confirmed over a longer period of observation. This observation could help in planning health strategies during the second surge and possible subsequent ones.
Conflict of interest
None.
Acknowlgement
Lombardia CARe is partially funded by the Fondazione Banca del Monte di Lombardia.
Appendix A.
Lombardia CARe researchers
Andrea Pagliosa, Guido Matiz, Guido Francesco Villa, Maurizio Migliori, Giuseppe Maria Sechi, Sara Compagnoni, Rosa Fracchia, Enrico Contri, Vincenza Ronchi, Antonella De Pirro, Simone Molinari, Vito Sgromo, Valeria Musella, Martina Paglino, Francesco Mojoli, Bruno Lusona, Michele Pagani, Moreno Curti, Stefano Buratti, Roberta Bertona, Livio Carnevale, Giueppe Bergamini, Irene Raimondi Cominesi, Simone Ruggeri, Daniele Bussi, Erika Taravelli, Gian Battista Danzi; Cristian Fava, Fabio Facchin, Giovanni Buetto, Antonio Cuzzoli, Sabina Campi, Guido Garzena Alessandra Russo, Andrea Lorenzo Vecchi, Cecilia Fantoni, Cinzia Franzosi, Claudio Vimercati, Dario Franchi, Enrico Storti, Fulvio Giovenzana, Marco Botteri, Salvatore Ivan Caico, Matteo Caresani, Mario Luppi, Paola Genoni, Roberto De Ponti, Arianna Marioni, Ilaria Passarelli, Marco Paiella, Umperto Piccolo, Giovanna Perrone, Gianluca Panni, Luca Bettari, Daniele Ghiraldin.
References
- 1.Baldi E., Sechi G.M., Mare C. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020;41(32):3045–3054. doi: 10.1093/eurheartj/ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baldi E., Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–498. doi: 10.1056/nejmc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holland M., Holland M., Burke J., Hulac S. Excess cardiac arrest in the community during the COVID-19 pandemic. JACC Cardiovasc Interv. 2020;13:1968–1969. doi: 10.1016/j.jcin.2020.06.022. Elsevier Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai P.H., Lai P.H., Lancet E.A., Weiden M.D. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020;11201:1–10. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marijon E., Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France : a population-based, observational study. Lancet Public Health. 2020;2667:1–7. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]