Abstract
BACKGROUND:
Duffy’s Quality-Caring Model guides nursing practice at the H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL. No published studies using this model in oncology were found.
OBJECTIVES:
The purpose of this article is to determine patients’ perceptions of nurse caring behaviors at the time of discharge after surgery.
METHODS:
A descriptive correlational design was used. Data were collected using Duffy’s Caring Assessment Tool (CAT). Simple regression analyses were performed.
FINDINGS:
Spearman’s correlation coefficients between the scores and age, length of stay, and number of nurses caring for the patients were not significant. No significant association was found between surgical site and CAT scores, nor between gender, race, and disposition posthospitalization. Appreciation of unique meanings and mutual problem solving showed need for improvement.
Keywords: caring, nursing, surgical oncology, Quality-Caring Model
the art of caring for patients is fundamental to nursing. Caring is the adjective used most frequently by students and nurses to describe the nursing profession and is a major component of nursing curricula (Duffy & Hoskins, 2003). Nursing care includes attending to patients’ physical and psychological needs. The concept of nursing care may be interpreted differently by each patient, depending on his or her specific culture, socioeconomic status, gender, race, ethnicity, or age. Nurses often face barriers, including increased patient workload and patient acuity and decreased patient length of hospital stay, that may affect their ability to fulfill caring. In this era of emphasis on quality outcomes and patient satisfaction, exploring patients’ perceptions of caring is important to ensure that nurses are providing care according to what the patients want or expect and not what nurses perceive.
Although caring has been termed as the essence and core of nursing, the concept of caring was not studied until the 1950s (Larson, 1995). In the late 1970s, the first national caring research conference convened. Research on caring became more plentiful with the work of Jean Watson in the 1980s. In 1988, caring was added as a term in CINAHL® (Brilowski & Wendler, 2005). However, little is known about patients’ perspectives on caring. Although several studies regarding the caring patient–nurse relationship have been published during the past 30 years, few focused specifically on the perspective of patients with cancer.
The limited research found regarding perceptions of patients with cancer included studies that used instruments, such as the Caring Assessment Report Evaluation Q-sort (CARE-Q), developed specifically for use with patients with cancer, and the Caring Behaviors Inventory (CBI) (Zamanzadeh, Azimzadeh, Rahmani, & Valizadeh, 2010). This research has yielded mixed results regarding patients’ and nurses’ perceptions of caring.
In a systematic review of nurses’ caring behaviors from an adult patient perspective, a contrast between patients’ and nurses’ perceptions of caring was found (Papastavrou, Efstathiou, & Charalambous, 2011). Overall, patients value instrumental and technical skills, including competency in performing activities, more than nurses themselves; nurses perceive their psychological skills and expressive caring behaviors as being more important than patients do.
One study by Patiraki et al. (2014) suggested a possible link between perception of caring and length of stay (LOS). Chang, Lin, Chang, & Lin (2005) used the CARE-Q to study perceptions of Chinese nurses and patients with cancer experiencing pain. Both groups ranked being accessible as the number one caring behavior, but the groups did not concur on the importance of the other items. Although this study was limited by its small sample size, the agreement between patients and nurses when ranking being accessible (in contrast to other studies) may have been influenced by symptoms like pain and suffering, which often are experienced by patients with cancer. When patients experience pain and suffering, they may need and receive more frequent contact, monitoring, and follow-up from nurses than patients with other symptoms and diagnoses (Chang et al., 2005).
Zamanzadeh et al. (2010) used the 57-item CARE-Q evaluation with patients with cancer and staff. The researchers found that nurses and patients identified “monitors follow-through” and “being accessible” as important behaviors. Patients indicated that the CARE-Q form was lengthy. Zamanzadeh et al. (2010) suggested that the consistency in the ratings may be because patients with cancer and nurses interact during a long period of time. Their long-term relationship may account for more consistent perceptions regarding the importance of caring behaviors (Zamanzadeh et al., 2010).
A cross-cultural study of the concept of caring using the 24-item CBI was carried out in six different European Union countries (Papastavrou et al., 2011). The authors found differences between nurses’ and surgical patients’ perceptions of caring; although both valued knowledge and skills, the nurses scored that subscale higher than the patients did (p < 0.005). Significant differences on the CBI were found among the six participating countries. Two studies used data from Papastavrou et al. (2011). Their results provided a link between measures of caring and patient satisfaction. One study found that positive connectedness was the greatest predictor of satisfaction (Palese et al., 2011). Behaviors that indicate positive connectedness include giving instruction or teaching the patient, helping the patient grow, being patient, and including the patient in the plan of care. The strongest predictors of CBI, related to patient satisfaction by the authors, were type of admission (planned versus emergency), age, and perceived health condition (Patiraki et al., 2014). Patients with a bad health condition perceived their care less positively than patients who reported their condition as good. Other findings from studies using the CBI include gender and cultural differences in perceptions of caring (Merrill, Hays, Clukey, & Curtis, 2012) and additional support for a statistically significant relationship between measures of caring and patient satisfaction with nursing care (Rafii, Hajinezhad, & Haghani, 2008).
Duffy (2013) developed the Caring Assessment Tool (CAT) to measure patient perception of nursing care. Duffy’s Quality-Caring Model has been used to develop a caring-based intervention for older adults with heart failure (Duffy, Hoskins, & Dudley-Brown, 2005) and to study the feasibility of electronic data collection in hospitalized older adults (Duffy, Kooken, Wolverton, & Weaver, 2012). CAT was used to test the longitudinal effect of interventions designed to improve patients’ perceptions of caring (O’Nan, Jenkins, Morgan, Adams, & Davis, 2014). Scores were found to improve during a 22-month period. No published studies were found that used CAT to measure the perception of patients with cancer on nurses’ caring behaviors.
Investigation of the patients’ viewpoints of caring behaviors needs further exploration. Given the emphasis on patient-centered care for patients with cancer and the dearth of studies on perceptions of caring, research measuring perceptions of caring is necessary. Specifically, associations between caring patient–nurse relationships, patient satisfaction, and hospitalized patient outcomes have surfaced as an important research topic. Given the conflicting data regarding perception of caring and LOS, the relationship between patient perception of caring and LOS in patients with cancer after surgery should be explored.
The purpose of the current study is to survey patients with cancer at the time of discharge after surgery to determine their perceptions of nurse caring behaviors. In addition, demographic and clinical variables were explored as potential predictors of perceptions.
Conceptual Model
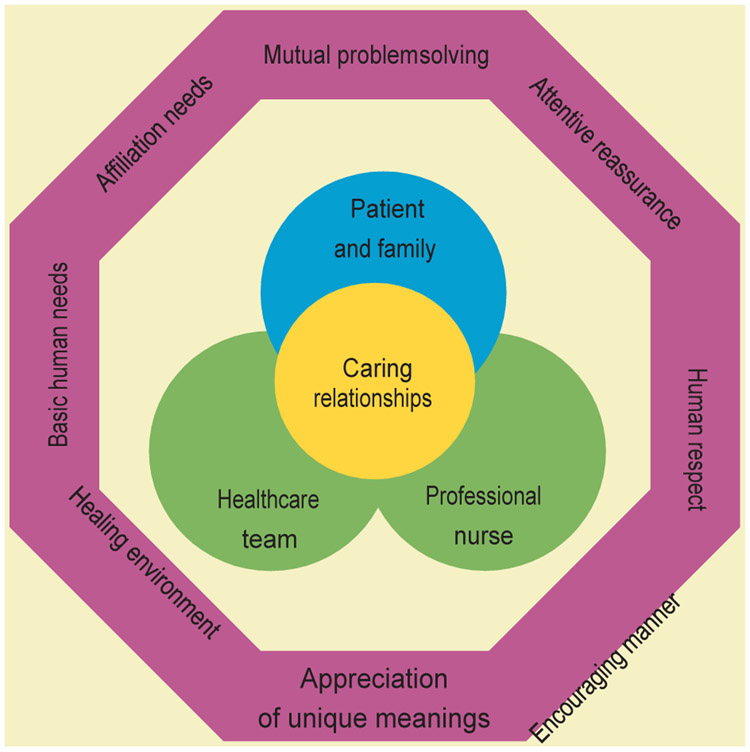
Duffy’s Quality-Caring Model serves as the theoretical foundation for nursing care at the study site, H. Lee Moffitt Cancer Center and Research Institute in Tampa, Florida, and is the conceptual framework for the current study. Figure 1 depicts relationship-centered professional encounters. Patients’ perceptions of nurses’ caring behaviors is the focus of the current study. Patient- and family-centered care is the core and goal of oncology nursing practice and reflects nurses’ caring. Oncology nurses at the study center embrace personalized patient- and family-centered care and the fundamental principles of dignity, respect, information sharing, participation, collaboration, safety, and professionalism. Duffy’s framework supports the concept, for patients, that being cared for matters and is an essential performance indicator of quality of care. Duffy (2013) advocates that professionalism is about the varied relationships nurses have with others and that the patient–nurse relationship, otherwise known as nursing care, is at the center of practice. Evaluation of the patient–nurse relationship and the perception of caring is necessary for designing strategies to improve the quality of practice in a continuously changing healthcare setting.
FIGURE 1. QUALITY-CARING MODEL.
Note. From Quality Caring in Nursing and Health Systems: Implications for Clinicians, Educators, and Leaders (3rd ed., p. 35) by J.R. Duffy, 2013, New York, NY: Springer Publishing Company. Copyright 2013 by Springer Publishing Company. Reprinted with permission.
Methods
A descriptive correlational design was used for the current study, with a single set of measurements from surgical inpatients with cancer at the time of discharge. The study was conducted on a 24-bed surgical oncology unit at the Moffitt Cancer Center. This patient population primarily consisted of postsurgical patients from the gastrointestinal (GI), head and neck, and genitourology services.
Sample
A convenience sample of 80 inpatients was surveyed. With this sample size, power is greater than 0.8 to detect an r greater than 0.31 with an alpha of 0.05 and using a two-sided test. Inclusion criteria were the following:
Being aged 18 years or older
Being a postoperative surgical patient from the GI, head and neck, or genitourology services
Being admitted for longer than 24 hours
Being able to read informed consent and complete CAT (version V) in English
Exclusion criteria were having received direct nursing care by the principal investigator and being transferred to the unit from another inpatient unit.
Instruments
Demographic and clinical data were collected from the electronic health record. The selected variables were age, gender, ethnicity, type of surgery (GI, head and neck, or genitourinary), LOS (days that a patient was hospitalized during this hospitalization), patient discharge disposition (the location of the patient’s discharge: home, home with home health care, rehabilitation center, skilled nursing facility, or hospice), and the number of nurses who cared for the patient while on the unit. These variables were taken from the literature. Significant associations between any demographic variable and perceptions of caring can help to identify ways in which caring can be improved.
The outcome variable is the inpatient’s self-reported perception of caring, measured by CAT. CAT measures a single construct of a patient’s perception of the patient–nurse relationship (Duffy, Brewer, & Weaver, 2014). The instrument has 27 items, administered in paper-and-pencil format. The instrument can be self-administered or completed with assistance. Items are rated on a five-point Likert-type scale ranging from 1 (never) to 5 (always). Summation scores range from 27–135, with higher scores indicating greater caring, as perceived by hospitalized patients.
Early versions of CAT attempted to measure eight independent factors. Confirmatory factor analysis and exploratory factor analysis of CAT (version IV) resulted in an acceptable fit of the 36 items in a single factor (Duffy et al., 2014). The single factor accounted for 70% of the variance reproduced, and the comparative fit index was 0.98. Further analysis supported the formation of a 27-item instrument (CAT, version V). Seventy-three percent of the variance was reproduced by this single factor (coefficient α = 0.967). These results suggest that all items are measuring the same construct. Duffy recommends the use of CAT (version V) with acceptable psychometric properties and decreased burden for patients completing the instrument. The Department of Nursing Research purchased a license to use CAT (version V) in the current study.
Data Collection
To reduce bias, the data collector did not provide direct care to any of the patients on the study unit. Each day, the data collector consulted the clinical leader regarding scheduled discharges. Inclusion and exclusion criteria were reviewed to determine eligibility. The data collector introduced herself, explained the study to the patient, and answered questions. Informed consent was obtained from patients who agreed to participate. The data collector reviewed the instructions for completing CAT to the participant and family, if present, and provided a copy and pen. Participants were instructed to complete the survey themselves. It was reinforced that family or friends should not complete the survey for the patient.
Ethical Considerations
Regulatory approval was obtained from the center’s scientific review committee and institutional review board. A copy of the informed consent was provided to the participants. Survey results were nonidentifiable, and completed surveys were kept locked in the office of the director of nursing research. Participation was voluntary.
Data Analysis
Descriptive, bivariate, and correlational statistical analyses were conducted using SAS, version 9.4. Demographics and survey responses were summarized using means, standard deviations, and percentages based on the variable type. Inferential analyses of group differences and covariation were conducted with an alpha of 0.05.
Results
At the time of the study, the unit had a total of 32 RNs. Patient assignments were usually 4:1 in the day (7 am to 7 pm) and 5:1 or 4:1 at night (7 pm to 7 am).
Eighty CATs were completed. Of those, seven had less than 21 of 27 scorable responses and were dropped from the analysis. The sample size for analysis was 73. Although CAT does not provide a mechanism to choose not applicable (N/A) as a response, a number of N/A responses were handwritten by participants to many of the 27 CAT items. Therefore, rather than a summed total score, the CAT score was the average response value (1–5) for items with a response other than N/A.
The negatively skewed distribution of many item responses necessitated the use of nonparametric statistics. Spearman’s correlation coefficient was used to assess covariation of CAT scores with age, the number of nurses caring for the patient, and LOS. For categorical variables, the Wilcoxon rank-sum test was used to compare CAT scores for the binary variables of gender, ethnicity, and postdischarge situation. The Kruskal-Wallis test was used to assess the relationship of primary cancer site (three levels) on caring.
The sample consisted of men (n = 41) and women (n = 32) with a mean age of 62.1 years. Sixty-five participants were White and non-Hispanic. The surgeries represented in the sample were GI (n = 41), head and neck (n = 17), and genitourinary (n = 15). The average number of nurses caring for the participants during their hospitalization was 6.2, with a range of 2–13. The average LOS was 6.1 days, with a range of 1–19.
At the time of discharge from the hospital, 51 patients were discharged to their home and 17 returned to their home with home health care. The remaining five participants went to nursing homes, rehabilitation centers, or hospice. Only the participants discharged to their home or to their home with home health care were used to analyze the relationship between disposition and the caring score.
The mean CAT score was 4.5 (SD = 0.49). Scores ranged from 3.3–5 (on a 1–5-point scale). Twenty-three items had an average score of 5, the maximum value.
Spearman’s correlation coefficients between the CAT scores and age (r = 0.07), LOS (r = 0.19), and the number of different nurses caring for the patient (r = 0.11) were not significant (p > 0.1). A significant association was not found between surgical site and scores on CAT (χ2 = 1.6, p > 0.44). No significant relationship (p > 0.32) was found between CAT scores and gender (Wilcoxon Z = −0.37), race (Z = −0.99), and disposition posthospitalization (Z = 0.78).
Although CAT does not ask for independent comments related to care, study participants (n = 10) wrote positive comments in the margins. The following are excerpts from comments:
“The nursing staff I have dealt with during this stay has been beyond excellent.”
“The entire staff who took care of me was exceptional.”
“The nurses and techs were wonderful and very caring professionals.”
“I was treated with highest respect.”
“For me, the most important thing is nurses who are positive, willingness to help, and high emotional attitude. All of these we found in abundance.”
The factors that the study team thought may affect patient perception of caring did not have an effect in the current study. Although the study unit has consistently high HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) scores, the study team considered questions from CAT that may suggest potential areas of improvement. A decision was made to look at the five statements with the lowest-scoring level of agreement, which were the following:
Help me believe in myself.
Help me explore alternate ways of dealing with my health problems.
Ask me what I know about my illness.
Help me figure out questions to ask other healthcare professionals.
Ask me how I think my healthcare treatment is going.
One additional way to assess the low-scoring statements would be to examine all of those for which “always” was the response chosen by less than 60% of the participants. This method yielded the following additional five statements to examine:
Support me with my beliefs.
Acknowledge my inner feelings.
Help me understand how I am thinking about my illness.
Help me deal with my bad feelings.
Know what is important to me.
See Table 1 for the 10 survey items, participants responding “always,” and mean scores.
TABLE 1.
SURVEY ITEMS WHEN LESS THAN 60% OF PARTICIPANTS ANSWERED “ALWAYS” (N = 73)
| SINCE I HAVE BEEN A PATIENT HERE, THE NURSES | n | SCORE |
|---|---|---|
| Know what is important to me. | 44 | 4.35 |
| Ask me how I think my healthcare treatment is going. | 43 | 4.25 |
| Help me deal with my bad feelings. | 42 | 4.26 |
| Acknowledge my inner feelings. | 41 | 4.32 |
| Help me believe in myself. | 41 | 4.25 |
| Help me understand how I am thinking about my illness. | 40 | 4.32 |
| Support me with my beliefs. | 38 | 4.28 |
| Help me explore alternate ways of dealing with my health problems. | 32 | 3.94 |
| Ask me what I know about my illness. | 30 | 3.88 |
| Help me figure out questions to ask other healthcare professionals. | 28 | 3.9 |
Note. Items were rated on a five-point Likert-type scale ranging from 1 (never) to 5 (always).
Discussion
The average response values provided by the study participants indicate a very positive perception of caring. The variables the investigators thought may influence CAT score (age, gender, ethnicity, number of nurses caring for the patient, primary cancer site, and disposition postdischarge) were not significant in the current study.
Duffy (2013) does not ascribe particular questions in CAT (version V) for the eight caring factors. However, when analyzing the low-scoring items and comparing them with Duffy’s eight caring factors, it appears that areas for improvement in caring for the study unit can be found in the factors of mutual problem solving and appreciation of unique needs. Mutual problem solving is behavior that helps patients and caregivers understand how to confront, learn, and think about their health and illness (Duffy, 2013). Those behaviors can include exploring alternatives and deciding on questions to ask. This caring factor appears to be measured in the following statements, among others:
Help me understand how I am thinking about my illness.
Help me explore alternate ways of dealing with my health problems.
Ask me what I know about my illness.
Help me figure out questions to ask other healthcare professionals.
Appreciation of unique meaning is concerned with a person’s context or worldview. A behavior associated with this factor is knowing what is important to the patient (Duffy, 2013). The following statements may measure this factor:
Help me believe in myself.
Support me with my beliefs.
Acknowledge my inner feelings.
Ask me how I think my healthcare treatment is going.
Help me deal with my bad feelings.
Know what is important to me.
Implications for Nursing
For the study unit, assisting patients with mutual problem solving and appreciating their unique needs may improve patients’ perceptions of caring. Behaviors to implement may include asking patients if they have specific questions about their illness and treatment, helping them craft questions for other healthcare providers, and exploring the meaning of the illness to the patients. This may include exploring the impact on their life and the lives of their family members.
The previous discussion is based on the premise that the issues in the low-scoring questions are important to patients with cancer after surgery. For many of these patients, the goal may be to be discharged home with a potential for further treatment as needed. In that case, exploring other options, belief in oneself, and thoughts about how health treatment is going may not be important during the hospitalization. These issues may be more important in the clinic setting when the patient comes for follow-up.
Limitations
The data were collected on only one surgical oncology unit. This particular unit routinely receives very positive patient satisfaction scores, as measured by Press Ganey (www.pressganey.com), which provides data to hospitals related to patient satisfaction. The short patient stay on the study unit relative to other units at the Moffitt Cancer Center may have affected the time necessary to develop caring relationships. In addition, most participants (n = 65) were White and non-Hispanic, which is representative of the patient population. Additional studies should increase diversity by targeting treatment facilities that have a more diverse patient population and by offering the survey in other languages.
Conclusion
Understanding patients’ perceptions of caring behaviors can highlight areas for improvement for the nursing team in developing relationships and improving quality of life for patients and their families. Recommendations for future research include exploring the importance of some of the questions in CAT to patients with cancer who had surgery, as well as perceptions of surgical oncology nurses regarding what nursing behaviors they believe demonstrate caring to patients. Understanding the nurses’ perception of caring and comparing it the patients’ may provide insight to developing educational opportunities for the nurses. The effect of implementing behaviors designed to help patients with problem solving and appreciation of unique needs should be studied. Although CAT is designed for inpatient settings, studies to examine perceptions of caring in clinics, home health care, or other ambulatory settings are recommended.
IMPLICATIONS FOR PRACTICE.
Understand patients’ perceptions of caring behaviors to highlight areas of improvement in developing relationships and improving quality of life for patients and their families.
Ask patients if they have questions about their illness or treatment, and help them come up with questions for other healthcare providers.
Explore what the meaning of the illness is to patients, including the impact on their and their family members’ lives.
CNE ACTIVITY.
EARN 0.5 CONTACT HOURS
ONS members can receive free CNE for reading this article and completing an evaluation online. To do so, visit cjon.ons.org/cne to link to this article and then access its evaluation link after logging in.
Certified nurses can claim no more than 0.5 total ILNA points for this program. Up to 0.5 ILNA points may be applied to Professional Practice. See www.oncc.org for complete details on certification.
QUESTIONS FOR DISCUSSION.
USE THIS ARTICLE FOR JOURNAL CLUB
Journal club programs can help to increase your ability to evaluate the literature and translate those research findings to clinical practice, education, administration, and research. Use the following questions to start the discussion at your next journal club meeting.
Based on Duffy’s concept that patients’ perceptions define nurses’ caring behaviors, what do you perceive as your most effective caring behaviors?
Mutual problem solving emerged from the current study as a perceived caring behavior. What are examples from your practice of mutual problem solving with your patients?
The current study’s findings were based primarily on responses from White, non-Hispanic participants; how would you design a study to better determine non-White, Hispanic patients’ perceptions of caring behaviors?
How does the current study of nurses’ caring behaviors with inpatients with cancer undergoing surgery inform nurses’ caring behaviors in other settings (e.g., home health care, clinics, outpatient infusion centers)?
Visit http://bit.ly/1vUqbVj for details on creating and participating in a journal club. Photocopying of this article for discussion purposes is permitted.
Footnotes
The authors take full responsibility for this content and did not receive any honoraria or disclose any relevant financial relationships. The article has been reviewed by independent peer reviewers to ensure that it is objective and free from bias.
Contributor Information
Emily K. Compton, Patient Care Services Department, H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL..
Karen Gildemeyer, Patient Care Services Department, H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL..
Tina M. Mason, Department of Nursing Research, H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL..
Susan R. Hartranft, Department of Nursing Research, H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL..
Steven K. Sutton, Department of Biostatistics and Bioinformatics, H. Lee Moffitt Cancer Center and Research Institute in Tampa, FL..
REFERENCES
- Brilowski GA, & Wendler MC (2005). An evolutionary concept analysis of caring. Journal of Advanced Nursing, 50, 641–650. 10.1111/j.1365-2648.2005.03449.x [DOI] [PubMed] [Google Scholar]
- Chang Y, Lin YP, Chang HJ, & Lin CC (2005). Cancer patient and staff ratings of caring behaviors: Relationship to level of pain intensity. Cancer Nursing, 28, 331–339. [DOI] [PubMed] [Google Scholar]
- Duffy JR (2013). Quality caring in nursing and health systems: Implications for clinicians, educators, and leaders (2nd ed.). New York, NY: Springer. [Google Scholar]
- Duffy JR, Brewer BB, & Weaver MT (2014). Revision and psychometric properties of the caring assessment tool. Clinical Nursing Research, 23, 80–93. [DOI] [PubMed] [Google Scholar]
- Duffy JR, & Hoskins LM (2003). The Quality-Caring Model: Blending dual paradigms. Advances in Nursing Science, 26, 77–88. 10.1097/00012272-200301000-00010 [DOI] [PubMed] [Google Scholar]
- Duffy JR, Hoskins LM, & Dudley-Brown S (2005). Development and testing of a caring-based intervention for older adults with heart failure. Journal of Cardiovascular Nursing, 20, 325–333. 10.1097/00005082-200509000-00006 [DOI] [PubMed] [Google Scholar]
- Duffy JR, Kooken WC, Wolverton CL, & Weaver MT (2012). Evaluating patient-centered care: Feasibility of electronic data collection in hospitalized older adults. Journal of Nursing Care Quality, 47, 307–315. 10.1097/NCQ.0b013e31825ba9d4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson PJ (1995). Important nurse caring behaviors perceived by patients with cancer. Oncology Nursing Forum, 22, 481–487. [PubMed] [Google Scholar]
- Merrill AS, Hays JS, Clukey L, & Curtis D (2012). Do they really care? How trauma patients perceive nurses’ caring behaviors. Journal of Trauma Nursing, 19, 33–37. [DOI] [PubMed] [Google Scholar]
- O’Nan CL, Jenkins K, Morgan LA, Adams T, & Davis BA (2014). Evaluation of Duffy’s Quality Caring Model on patients’ perceptions of nurse caring in a community hospital. International Journal of Human Caring, 18, 27–34. 10.20467/1091-5710-18.1.27 [DOI] [Google Scholar]
- Palese A, Tomietto M, Suhonen R, Efstahiou G, Tsangari H, Mrekouris A, … Papastavrou E (2011). Surgical patient satisfaction as an outcome of nurses’ caring behaviors: A descriptive and correlational study in six European countries. Journal of Nursing Scholarship, 43, 341–350. 10.1111/j.1547-5069.2011.01413.x [DOI] [PubMed] [Google Scholar]
- Papastavrou E, Efstathiou G, & Charalambous A (2011). Nurses’ and patients’ perceptions of caring behaviours: Quantitative systematic review of comparative studies. Journal of Advanced Nursing, 67, 1191–1205. [DOI] [PubMed] [Google Scholar]
- Patiraki E, Karlou C, Efstathiou G, Tsangari H, Merkouris A, Jarosova D, … Papastarvou E (2014). The relationship between surgical patients and nurses characteristics with their perceptions of caring behaviors: A European survey. Clinical Nursing Research, 23, 132–152. [DOI] [PubMed] [Google Scholar]
- Rafii F, Hajinezhad ME, & Haghani H (2008). Nurse caring in Iran and its relationship with patient satisfaction. Australian Journal of Advanced Nursing, 26, 75–84. [Google Scholar]
- Zamanzadeh V, Azimzadeh R, Rahmani A, & Valizadeh L (2010). Oncology patients’ and professional nurses’ perceptions of important nurse caring behaviors. BMC Nursing, 9, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]