Abstract
Aims and objectives:
To evaluate the knowledge and attitudes towards sexual and gender minority (SGM) oncology patients’ needs among advanced practice providers (APPs).
Background:
SGM individuals experience health disparities, in part due to lack of access to knowledgeable providers. Despite the important role of APPs in cancer care, less is known about their attitudes and knowledge towards SGM cancer patients.
Design:
Cross-sectional study.
Methods:
A survey of APPs at a National Cancer Institute-Designated Comprehensive Cancer Center assessed self-reported demographics, attitudes, knowledge and postsurvey confidence in knowledge of SGM oncology patient needs. Reporting of this study adheres to STROBE guidelines.
Results:
Knowledge of health needs was low with an average of 2.56 (SD = 1.27) items answered correctly out of 6. The majority of APPs self-reported being comfortable treating SGM patients (93.6% and 87.2%, respectively), but less confident in knowledge of their health needs (68.0% and 53.8%, respectively). Although less than half of APPs believed education should be mandatory (44.9%), 79.5% were interested in education about SGMs’ unique health needs. Political affiliation, medical specialty, licensure, and having SGM friends or family were associated with various attitude items, but not knowledge. Moderation analyses indicated that APPs who had greater overall knowledge scores were more likely to agree, on average, that knowing sexual orientation, gender identity and sex assigned at birth are important to providing quality oncology care.
Conclusion:
APPs report being comfortable providing care for SGMs with cancer, but knowledge gaps remain that may inhibit the quality of care provided. Given the interest in education, results would support the development of SGM-related healthcare training for oncology APPs.
Relevance to clinical practice:
Targeted education for providers during training and continuing education is likely to improve the provision of quality care for SGMs with cancer.
Keywords: advanced practice professionals, cancer health, healthcare providers, LGBTQ, nurses, oncology, sexual and gender minorities
1 ∣. INTRODUCTION
There has been an emerging focus on health disparities among the lesbian, gay, bisexual, transgender and queer/questioning (LGBTQ) populations from multiple organisations including the National Institutes of Health, the National Academy of Medicine (formerly the Institute of Medicine) and the American Academy of Nursing (AANP, 2016; IOM, 2011; Pérez-Stable, 2016). Despite this focus, the LGBTQ population continues to experience greater mental health and substance use problems due to perceived stigma (Meyer, 2003), and reduced access to knowledgeable and culturally relevant health care (Kitts, 2010; Sanchez, Sanchez, & Danoff, 2009). LGBTQ individuals may be at increased risk for certain cancers due to behaviours such healthcare avoidance, sexual behaviours, higher rates of obesity, substance use and smoking (Ceres, Quinn, Loscalzo, & Rice, 2018; Hegazi & Pakianathan, 2018; Quinn et al., 2015; Wender, Sharpe, Westmaas, & Patel, 2016). With the growing burden of cancer among LGBTQ populations and increasing role of advanced practice providers in oncology care such as nurse practitioners, understanding the informational needs of these healthcare providers to create educational interventions is critical.
2 ∣. BACKGROUND
There are substantial gaps in formal and practical academic training for healthcare providers regarding LGBTQ health. A 2011 survey among U.S. medical schools showed approximately 33% reported zero LGBT-specific content in their clinical years (Obedin-Maliver et al., 2011). Eliason, Dibble, and DeJoseph (2010) suggest the nursing profession has also not kept up with other health professions in creating education to address the healthcare needs of the LGBTQ population. A national survey of faculty from U.S. nursing undergraduate schools showed 23%–63% reported they had not taught LGBTQ health-related topics in the past 2 years and devoted on average a total of two hours teaching time to LGBTQ health topics during the length of the program (Lim, Johnson, & Eliason, 2015).
Despite showing high self-reported comfort with treating LGBTQ patients, prior survey studies have shown oncologists and other healthcare providers at National Cancer Institute (NCI)-Designated Comprehensive Cancer Centers have low knowledge of LGBTQ health needs and lack understanding of the importance of inquiring about patients’ sexual orientation and gender identity (Banerjee, Walters, Staley, Alexander, & Parker, 2018; Schabath et al., 2019; Shetty et al., 2016). However, these studies also reveal that providers show a strong interest in receiving further education regarding LGBTQ health (Banerjee et al., 2018; Schabath et al., 2019; Shetty et al., 2016). When given the Implicit Association Test, heterosexual healthcare providers have demonstrated strong implicit preference for heterosexual patients vs. sexual minority patients, with heterosexual nurses showing the strongest implicit biases (Sabin, Riskind, & Nosek, 2015). In a sample of nurse educators, having self-reported negative attitudes towards sexual minorities was associated with lower perceived importance of teaching about sexual minority-related content, suggesting that nurses’ negative attitudes towards LGBTQ individuals may decrease their receptivity to receiving education on this population (Sirota, 2013).
The majority of research on attitudes, knowledge and practice behaviours of healthcare providers regarding LGBTQ populations has been conducted on physicians (Schabath et al., 2019; Shetty et al., 2016; Snelgrove, Jasudavisius, Rowe, Head, & Bauer, 2012). Advanced practice professionals (APPs), such as nurse practitioners and physician assistants, have a prominent role in cancer care (Fusco, 2015), and their cultural competency for LGBTQ patients is essential to the provision of quality care for this population. With the rising number of APPs in cancer care (Bruinooge et al., 2018), culturally relevant communication skills for APPs regarding LGBTQ populations are needed to improve the health of this underserved population. The current study aimed to evaluate the knowledge and attitudes towards LGBTQ health care among APPs at an NCI-Designated Comprehensive Cancer Center.
3 ∣. METHODS
Reporting of this study adheres to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines for reporting observational studies (Von Elm et al., 2014; See Supplementary File 1).
3.1 ∣. Sample and procedure
All APPs practicing at an NCI-Designated Cancer Center (n = 200) were invited via e-mail to participate in a cross-sectional web-based survey using the modified Dillman Method in which an initial informational e-mail described the purpose of the study followed by an e-mail with a link to the survey and two subsequent waves of reminder e-mails two weeks apart (Dillman, 1978). Among those invited, 78 surveys were completed. The survey was available online between January and March 2017. Participants could enter a raffle for one of six $50 gift cards by e-mailing the study staff after completing the study. To reduce social desirability and nonresponse bias, the survey was made anonymous. Respondents were asked not to provide identifying information and did not need to use their institutional e-mail address to be entered into the raffle. The study was approved by the Institutional Review Board.
3.2 ∣. Survey measures
The survey measures included demographics, attitudes, knowledge and postsurvey confidence in knowledge of LGBTQ health needs. Definitions of sexual orientation and gender identity obtained from Fenway (Bradford, Cahill, Grasso, & Makadon, 2012) and the National Academy of Medicine (IOM, 2011) were provided prior to starting the survey. Survey items were originally created based on published surveys and articles on LGBTQ health, reviewed by the institution's LGBTQ patient employee advisory group, and tested for comprehension and clarity with healthcare professionals (Schabath et al., 2019; Shetty et al., 2016).
Demographic questions included gender identity, age, race/ethnicity, sexual orientation, religious affiliation, the extent to which their religion influenced provision of care, whether or not they had family members or friends who identify as LGBTQ, political affiliation, licensure, year of graduation from professional school and practice-related information (e.g., cancer site treated).
Six items assessed knowledge of health-related information for LGBTQ populations: healthcare avoidance, HPV-related cervical dysplasia, anal cancer testing for gay/bisexual men, smoking prevalence, sun-seeking behaviour and access to health insurance for transgender individuals. Response options on a 5-point Likert scale ranged from strongly disagree to strongly agree with the additional option of “Don't know or prefer not to answer.” To create a total score for correct knowledge items, responses were also coded as “correct” and “incorrect” and summed (range 0 = none correct to 6 = all correct).
Twelve attitude items including subscales from our Attitude Summary Measure (Schabath et al., 2019) assessed respondents’ LGBTQ-related self-reported levels of comfort, confidence in knowledge, interest in education and perception of importance to care (see Table 2 for items). Item response options on a 5-point Likert scale ranged from “strongly disagree” to “strongly agree” with the additional option of “Don't know or prefer not to answer.” Exploratory factor analysis demonstrated preliminary internal consistency and construct validity of the Attitude Summary Measure using a national sample of oncologists, demonstrating that the measure has three reliable subscales (Schabath et al., 2019). The comfort-confidence subscale is the mean of responses to items 1–4 in Table 2 and represents providers’ average level of self-reported comfort with treating and confidence in their knowledge of LGBTQ patients’ health needs. The education-involvement subscale is the mean of items 5, 6 and 12 in Table 2 and characterises providers’ attitudes pertaining to being involved in LGBTQ competency efforts. The practice beliefs subscale is the mean of items 7–9 in Table 2 and indicates providers’ average perception of the importance of knowing patients’ sexual orientation, gender identity and sex assigned at birth to provide the best care. In the current study, internal consistency was acceptable for the three subscales: comfort-confidence (α = 0.78), education-involvement (α = 0.75) and practice beliefs (α = 0.75).
TABLE 2.
Attitudes towards LGBTQ health among surveyed advanced practice providers
| n (%) | Political affiliation | LGBTQ Friends/ Family |
Licensure | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Conservative | Moderate | Liberal | Otherc | Yes | No | Physician assistant |
Advanced registered nurse practitioner |
Anaesthesia-related licensure | |
| 1. I am comfortable treating LGB patients | ||||||||||
| Strongly Disagree/Disagree | 3 (3.8) | 0 (0.0) | 1 (7.7) | 1 (3.8) | 1 (9.1) | 3 (4.2) | 0 (0.0) | 2 (7.7) | 1 (2.9) | 0 (0.0) |
| Neutral | 2 (2.6) | 1 (3.7) | 1 (7.7) | 0 (0.0) | 0 (0.0) | 2 (2.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (9.1) |
| Strongly Agree/Agree | 73 (93.6) | 26 (96.3) | 11 (84.6) | 25 (96.2) | 10 (90.9) | 66 (93.0) | 5 (100.0) | 24 (92.3) | 34 (97.1) | 10 (90.9) |
| 2. I am confident in my knowledge of health needs of LGB patients | ||||||||||
| Strongly Disagree/Disagree | 7 (9.0) | 3 (11.1) | 1 (7.7) | 2 (7.7) | 1 (9.1) | 7 (9.9) | 0 (0.0) | 2 (7.7) | 4 (11.4) | 0 (0.0) |
| Neutral | 18 (23.1) | 6 (22.2) | 7 (53.8) | 1 (3.8) | 4 (36.4) | 14 (19.7) | 3 (60.0) | 6 (23.1) | 6 (17.1) | 4 (36.4) |
| Strongly Agree/Agree | 53 (67.9) | 18 (66.7) | 5 (38.5) | 23 (88.5) | 6 (54.5) | 50 (70.4) | 2 (40.0) | 18 (69.2) | 25 (71.4) | 7 (63.6) |
| 3. I am comfortable treating transgender patients | ||||||||||
| Strongly Disagree/Disagree | 3 (3.8) | 1 (3.7) | 1 (7.7) | 0 (0.0) | 1 (9.1) | 3 (4.2) | 0 (0.0) | 1 (3.8) | 1 (2.9) | 0 (0.0) |
| Neutral | 7 (9.0) | 4 (14.8) | 1 (7.7) | 0 (0.0) | 2 (18.2) | 4 (5.6) | 3 (60.0) | 4 (15.4) | 1 (2.9) | 1 (9.1) |
| Strongly Agree/Agree | 68 (87.2) | 22 (81.5) | 11 (84.6) | 26 (100.0) | 8 (72.7) | 64 (90.1) | 2 (40.0) | 21 (80.8) | 33 (94.3) | 10 (90.9) |
| 4. I am confident in my knowledge of health needs of transgender patients | ||||||||||
| Strongly Disagree/Disagree | 10 (12.8) | 5 (18.5) | 1 (7.7) | 2 (7.7) | 2 (18.2) | 10 (14.1) | 0 (0.0) | 5 (19.2) | 4 (11.4) | 0 (0.0) |
| Neutral | 26 (33.3) | 8 (29.6) | 8 (61.5) | 7 (26.9) | 3 (27.3) | 20 (28.2) | 5 (100.0) | 7 (26.9) | 13 (37.1) | 4 (36.4) |
| Strongly Agree/Agree | 42 (53.8) | 14 (51.9) | 4 (30.8) | 17 (65.4) | 6 (54.5) | 41 (57.7) | 0 (0.0) | 14 (53.8) | 18 (51.4) | 7 (63.6) |
| 5. I would be interested in education regarding the unique health needs of LGBTQ patients | ||||||||||
| Strongly Disagree/Disagree | 3 (3.8) | 1 (3.7) | 1 (7.7) | 0 (0.0) | 1 (9.1) | 3 (4.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (9.1) |
| Neutral | 13 (16.7) | 3 (11.1) | 6 (46.2) | 2 (7.7) | 2 (18.2) | 11 (15.5) | 2 (40.0) | 7 (26.9) | 2 (5.7) | 3 (27.3) |
| Strongly Agree/Agree | 62 (79.5) | 23 (85.2) | 6 (46.2) | 24 (92.3) | 8 (72.7) | 57 (80.3) | 3 (60.0) | 19 (73.1) | 33 (94.3) | 7 (63.6) |
| 6. I would be willing to be listed as an LGBTQ-friendly provider | ||||||||||
| Strongly Disagree/Disagree | 2 (2.6) | 1 (3.7) | 0 (0.0) | 0 (0.0) | 1 (9.1) | 2 (2.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (9.1) |
| Neutral | 15 (19.2) | 5 (18.5) | 5 (38.5) | 1 (3.8) | 4 (36.4) | 12 (16.9) | 3 (60.0) | 6 (23.1) | 4 (11.4) | 3 (27.3) |
| Strongly Agree/Agree | 61 (78.2) | 21 (77.8) | 8 (61.5) | 25 (96.2) | 6 (54.5) | 57 (80.3) | 2 (40.0) | 20 (76.9) | 31 (88.6) | 7 (63.6) |
| 7. The LGBTQ population is often more difficult to treat | ||||||||||
| Strongly Disagree/Disagree | 47 (60.3) | 14 (51.9) | 7 (53.8) | 18 (69.2) | 7 (63.6) | 43 (60.6) | 3 (60.0) | 17 (65.4) | 23 (65.7) | 4 (36.4) |
| Neutral | 22 (28.2) | 9 (33.3) | 5 (38.5) | 6 (23.1) | 2 (18.2) | 20 (28.2) | 2 (40.0) | 6 (23.1) | 10 (28.6) | 5 (45.5) |
| Strongly Agree/Agree | 9 (11.5) | 4 (14.8) | 1 (7.7) | 2 (7.7) | 2 (18.2) | 8 (11.3) | 0 (0.0) | 3 (11.5) | 2 (5.7) | 2 (18.2) |
| 8. It is important to know the sexual orientation of my patients to provide the best care | ||||||||||
| Strongly Disagree/Disagree | 22 (28.2) | 6 (22.2) | 4 (30.8) | 10 (38.5) | 1 (9.1) | 21 (29.6) | 0 (0.0) | 7 (26.9) | 7 (20.0) | 6 (54.5) |
| Neutral | 21 (26.9) | 6 (22.2) | 4 (30.8) | 8 (30.8) | 3 (27.3) | 19 (26.8) | 2 (40.0) | 5 (19.2) | 11 (31.4) | 3 (27.3) |
| Strongly Agree/Agree | 35 (44.9) | 15 (55.6) | 5 (38.5) | 8 (30.8) | 7 (63.6) | 31 (43.7) | 3 (60.0) | 15 (53.8) | 17 (48.6) | 2 (18.2) |
| 9. It is important to know the gender identity of my patients to provide the best care | ||||||||||
| Strongly Disagree/Disagree | 10 (12.8) | 3 (11.1) | 2 (15.4) | 4 (15.4) | 1 (9.1) | 10 (14.1) | 0 (0.0) | 4 (15.4) | 3 (8.6) | 0 (0.0) |
| Neutral | 15 (19.2) | 5 (18.5) | 3 (23.1) | 5 (19.2) | 2 (18.2) | 14 (19.7) | 1 (20.0) | 7 (26.9) | 4 (11.4) | 2 (18.2) |
| Strongly Agree/Agree | 53 (67.9) | 19 (70.4) | 8 (61.5) | 17 (65.4) | 8 (72.7) | 47 (66.2) | 4 (80.0) | 15 (57.7) | 28 (80.0) | 9 (81.8) |
| 10. It is important to know the patient's assigned sex at birth to provide the best care | ||||||||||
| Strongly Disagree/Disagree | 12 (15.4) | 1 (3.7) | 4 (30.8) | 6 (23.1) | 1 (9.1) | 11 (15.5) | 1 (20.0) | 3 (11.5) | 6 (17.1) | 1 (9.1) |
| Neutral | 15 (19.2) | 5 (18.5) | 0 (0.0) | 7 (26.9) | 3 (27.3) | 15 (21.1) | 0 (0.0) | 1 (3.8) | 9 (25.7) | 3 (27.3) |
| Strongly Agree/Agree | 51 (65.4) | 21 (77.8) | 9 (69.2) | 13 (50.0) | 7 (63.6) | 45 (63.4) | 4 (80.0) | 22 (84.6) | 20 (57.1) | 7 (63.6) |
| 11. Upon first encounter I assume a patient is heterosexual | ||||||||||
| Strongly Disagree/Disagree | 35 (44.9) | 13 (48.1) | 4 (30.8) | 14 (53.8) | 3 (27.3) | 31 (43.7) | 3 (60.0) | 12 (46.2) | 19 (54.3) | 2 (18.2) |
| Neutral | 20 (25.6) | 9 (33.3) | 2 (15.4) | 5 (19.2) | 4 (36.4) | 20 (28.2) | 0 (0.0) | 3 (11.5) | 10 (28.6) | 5 (45.5) |
| Strongly Agree/Agree | 23 (29.5) | 5 (18.5) | 7 (53.8) | 7 (26.9) | 4 (36.4) | 20 (28.2) | 2 (40.0) | 11 (42.3) | 6 (17.1) | 4 (36.4) |
| 12. There should be mandatory education on LGBTQ health needs at my workplace | ||||||||||
| Strongly Disagree/Disagree | 15 (19.2) | 6 (22.2) | 3 (23.1) | 3 (11.5) | 2 (18.2) | 11 (15.5) | 3 (60.0) | 8 (30.8) | 4 (11.4) | 2 (18.2) |
| Neutral | 26 (33.3) | 11 (40.7) | 5 (38.5) | 5 (29.2) | 5 (45.5) | 24 (33.8) | 2 (40.0) | 10 (38.5) | 8 (22.9) | 5 (45.5) |
| Strongly Agree/Agree | 37 (47.4) | 10 (37.0) | 5 (38.5) | 18 (69.2) | 4 (36.4) | 36 (50.7) | 0 (0.0) | 8 (30.8) | 23 (65.7) | 4 (36.4) |
| Subscales of Attitudes, M (SD) | ||||||||||
| Comfort | 4.11 (0.67) | 3.95 (0.57) | 3.94 (0.80) | 4.36 (0.52) | 4.00 (0.89) | 4.13 (0.67) | 3.65 (0.29) | 4.07 (0.68) | 4.15 (0.66) | 4.18 (0.50) |
| Education | 3.91 (0.78) | 3.77 (0.68) | 3.69 (0.88) | 4.28 (0.52) | 3.61 (1.13) | 3.95 (0.78) | 3.13 (0.51) | 3.77 (0.59)a | 4.23 (0.63)a,b | 3.64 (0.90)b |
| Practice beliefs | 3.57 (0.88) | 3.70 (0.77) | 3.54 (1.06) | 3.38 (0.93) | 3.76 (0.86) | 3.55 (0.90) | 3.87 (0.84) | 3.58 (0.94) | 3.67 (0.83) | 3.42 (0.82) |
Notes: Bold indicates significant difference with at an alpha level of <0.05. Significance tests used were chi-squared tests for test of proportion differences and one-way ANOVA with Brown-Forsythe adjusted F tests for mean differences by categories for attitudes subscales.
Same superscript indicates statistically significant difference in post hoc tests for mean differences with Bonferroni correction.
1 responded indicated "some other viewpoint," and 9 indicated they "prefer not to answer".
At the end of the survey, respondents were again asked about confidence in knowledge of health needs of (1) LGB patients and (2) transgender patients. These questions were asked twice because our pretesting of the survey showed respondents confidence often changed (decreased) once they had gone through the knowledge questions (Schabath et al., 2019).
3.3 ∣. Statistical analyses
Continuous demographic variables were categorised using median split, and categorical demographics were reduced to drop low cell counts and increase interpretability. For knowledge and attitudes, item responses were collapsed (“strongly disagree” with “disagree” and “strongly agree” with “agree”), and “don't know” and “prefer not to answer” were coded as “neutral.” Descriptive statistics were calculated for all survey measures. Chi-squared tests assessed the relationship between individual attitudes and knowledge items by respondent characteristics and subsequent Bonferroni-corrected z test comparing column proportions. One-way ANOVAs were conducted to determine differences between respondent characteristics and Attitude Summary Measure subscales. Correlations were computed between total knowledge and the Attitude Summary Measure subscales. Two moderation analyses were conducted to examine the main effects of total knowledge, comfort-confidence, and their interaction on education-involvement and practice beliefs using ordinary least-squares regression methods with the Hayes process macro—a regression path analysis modelling tool (Hayes, 2016). A paired sampled t test was conducted to determine the mean change in confidence of knowledge in LGB and transgender health needs from presurvey to postsurvey. IBM SPSS 24.0 was used for all analyses.
4 ∣. RESULTS
4.1 ∣. Demographics
Among the 78 APPs that completed the survey (response rate = 39%), the most frequent licensures were 35 Advanced Registered Nurse Practitioners (44.9%) and 26 Physician Assistants (33.3%), followed by 6 Certified Registered Nurse Anesthetists (7.7%) and 5 Anesthesiologist Assistants (6.4%; See Table 1 for descriptive statistics). Sixty-four (82.1%) APPs were female, 67 (85.9%) were heterosexual, 57 (73.1%) were non-Hispanic White, and 53 (67.9%) were Christian. Forty-one respondents (52.6%) indicated religious beliefs did not play a role in their practice/treatment of patients, and 71 (91.0%) indicated that they had an LGBTQ friend or family member. There was an even distribution of political affiliation from conservative (16.7%, n = 13) to very liberal (13.4%, n = 3) on a seven-point scale, although no one identified as very conservative. Year from graduation from professional school ranged from 1977 to 2016. Forty-nine (62.9%) respondents stated between 1% and 10% of their patients in the past year disclosed themselves as LGBTQ. Medical specialties represented were medical (33.3%, n = 26), surgical (25.6%, n = 20), and to a lesser extent radiation (2.6%, n = 2) and gynecological oncology (2.6%, n = 2), as well as 25 (32.1%) “other” specialties (e.g., anaesthesia, bone marrow transplant and palliative care). Because the survey was anonymous, we were unable to compare information between responders and nonresponders.
TABLE 1.
Characteristics of surveyed advanced practice providers (N = 78)
| Characteristic | ||
|---|---|---|
| Age, M (SD) | 42.8 (11.8) | |
| Gender, n (%) | ||
| Female | 64 (82.1) | |
| Male | 11 (14.1) | |
| Other | 1 (1.3) | |
| Prefer not to answer | 2 (2.6) | |
| Sexual Orientation, n (%) | ||
| Heterosexual | 67 (85.9) | |
| Bisexual | 3 (3.8) | |
| Lesbian | 1 (1.3) | |
| Gay | 1 (1.3) | |
| Not sure/Questioning | 1 (1.3) | |
| Prefer Not to Answer | 5 (6.4) | |
| Race/Ethnicity, n (%) | ||
| Hispanic | Not Hispanic | |
| Asian | 0 (0.0) | 4 (5.1) |
| Black or African American | 0 (0.0) | 4 (5.1) |
| White or Caucasian | 5 (6.4) | 57 (73.1) |
| Multiracial | 1 (1.3) | 0 (0.0) |
| Other/Not Surea | 1 (1.3) | 0 (0.0) |
| Religious Identity, n (%) | ||
| Atheist or Agnostic | 4 (5.1) | |
| Buddhist | 1 (1.3) | |
| Christian | 53 (67.9) | |
| Catholic | 2 (2.6) | |
| Hindu | 1 (1.3) | |
| Jewish | 1 (1.3) | |
| Not Religious | 7 (9.0) | |
| Prefer Not to Answer | 8 (10.3) | |
| Missing | 1 (1.3) | |
| Religious Beliefs Play Role in Practice/Treatment of Patients, n (%) | ||
| Strongly Disagree | 24 (30.8) | |
| Disagree | 17 (21.8) | |
| Neutral | 11 (14.1) | |
| Agree | 16 (20.5) | |
| Strongly Agree | 5 (6.4) | |
| Not Applicable | 4 (5.1) | |
| Missing | 1 (1.3) | |
| Family Member Identifies as LGBTQ, n (%) | ||
| Yes | 40 (51.3) | |
| No | 36 (46.2) | |
| Prefer Not to Answer | 1 (1.3) | |
| Missing | 1 (1.3) | |
| Friend Identifies as LGBTQ, n (%) | ||
| Yes | 70 (89.7) | |
| No | 6 (7.7) | |
| Prefer Not to Answer | 1 (1.3) | |
| Missing | 1 (1.3) | |
| Personal Political Affiliation, n (%) | ||
| Very Conservative | 0 (0.0) | |
| Conservative | 13 (16.7) | |
| Somewhat Conservative | 14 (17.9) | |
| Centrist/Moderate | 13 (16.7) | |
| Somewhat Liberal | 13 (16.7) | |
| Liberal | 10 (12.8) | |
| Very Liberal | 3 (13.4) | |
| Other Viewpoint | 1 (1.3) | |
| Prefer Not to Answer | 10 (12.8) | |
| Missing | 1 (1.3) | |
| Licensure | ||
| Physician Assistant | 26 (33.3) | |
| Advanced Registered Nurse Practitioner | 35 (44.9) | |
| Certified Registered Nurse Anesthetist | 6 (7.7) | |
| Anesthesiologist Assistant | 5 (6.4) | |
| Prefer Not to Answer | 6 (7.7) | |
| Years since Professional School Graduation, M (SD)b | 11.61 (9.29) | |
| Number of Patients Seen Each Week, n (%) | ||
| 0–25 | 29 (37.2) | |
| 26–50 | 40 (51.3) | |
| 51–75 | 0 (0.0) | |
| 76–100 | 5 (6.4) | |
| >100 | 3 (3.8) | |
| Missing | 1 (1.3) | |
| Percent of Patients that Identify as LGBTQ in Past Year, n (%) | ||
| None | 2 (2.6) | |
| 1%–5% | 30 (38.5) | |
| 6%–10% | 19 (24.4) | |
| 11%–15% | 4 (5.1) | |
| 16%–20% | 1 (1.3) | |
| >20% | 0 (0.0) | |
| Do Not Know | 20 (25.6) | |
| Missing | 2 (2.6) | |
| Medical Specialty, n (%) | ||
| Medical Oncology | 26 (33.3) | |
| Surgical Oncology | 20 (25.6) | |
| Radiation Oncology | 2 (2.6) | |
| Gynecological Oncology | 2 (2.6) | |
| Other | 25 (32.1) | |
| Missing | 3 (3.8) | |
| Cancer Sites Treated, n (%) | ||
| Breast | 25 (32.1) | |
| Penile | 13 (16.7) | |
| Anal | 18 (23.1) | |
| Thyroid | 15 (19.2) | |
| Sarcoma | 17 (21.8) | |
| Cervical | 13 (16.7) | |
| Prostate | 21 (26.9) | |
| Oesophageal/Gastric | 21 (26.9) | |
| Oral/Head and Neck | 17 (21.8) | |
| Malignant Haematology | 20 (25.6) | |
| Ovarian | 13 (16.7) | |
| Testicular | 13 (16.7) | |
| Kidney/Bladder | 20 (25.6) | |
| Neuroendocrine | 17 (21.8) | |
| Bone Marrow Transplant | 20 (25.6) | |
| Uterine | 14 (17.9) | |
| Colon/Rectal | 24 (30.8) | |
| Lung/Thoracic | 19 (24.4) | |
| Neuro-Oncology | 13 (16.7) | |
| Other | 14 (17.9) | |
| Number of Cancer Sites Treated, M (SD) | 4.86 (5.98) | |
| Treat LGBTQ Prevalent Cancer Site, n(%) | 42 (53.8) | |
| Age Groups Treated, n (%) | ||
| Paediatrics | 2 (2.6) | |
| Adolescent and Young Adult | 21 (26.9) | |
| Adult | 72 (92.3) | |
| Older Adult, Elderly | 53 (67.9) | |
Prefer not to answer for Ethnicity among “Other/Not Sure” Race = 5 (6.4%).
Prefer not to answer = 10 (12.8%); Missing = 1 (1.3%).
4.2 ∣. Attitude measures
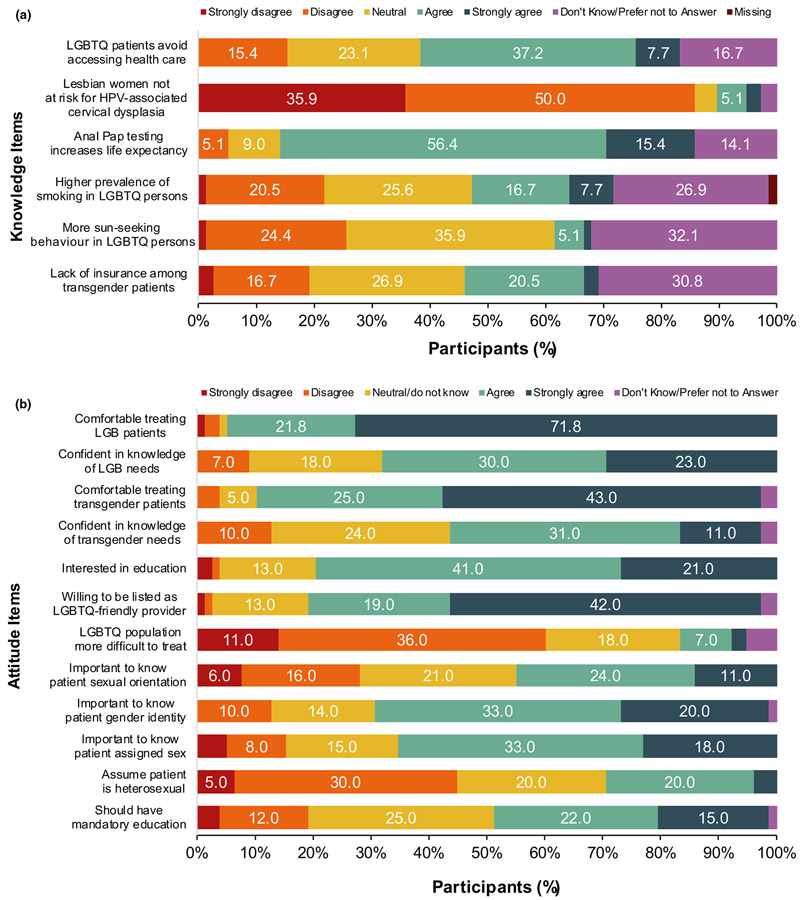
The majority of respondents self-reported that they were comfortable treating LGB (93.6%, n = 73) and transgender (87.2%, n = 68) patients and confident in their knowledge of LGB health needs (67.9%, n = 53), but only half (53.8%, n = 42) self-reported being confident in their knowledge of transgender health needs (Table 2; Figure 1a). Most APPs reported being interested in LGBTQ health education (79.5%, n = 62) and conveyed willingness to be listed as an LGBTQ-friendly provider (78.2%, n = 61). However, less than half indicated that education should be mandatory (47.4%, n = 37). Most reported that they did not believe LGBTQ patients were more difficult to treat (60.3%, n = 47), but nearly one-third indicated that they assume patients are heterosexual upon first encounter (29.5%, n = 23). Less than half reported that knowing patients’ sexual orientation was important to provide the best care (44.9%, n = 35), whereas more than half indicated that it was important to know patients’ gender identity (67.9%, n = 53) and sex assigned at birth (65.4%, n = 51).
FIGURE 1.
(a, b) Participant responses to attitude (a) and knowledge (b) items. Responses less than 5% are not labeled in the figure. All counts and percentages are presented in Table 2 for attitude items and Table 3 for knowledge items. LGBTQ, lesbian, gay, bisexual, transgender and queer/questioning. HPV, human papillomavirus
The Attitude Summary Measure subscale means were in the “agree” range: comfort-confidence (M = 4.11, SD = 0.67), education-involvement (M = 3.91, SD = 0.78) and beliefs about care (M = 3.57, SD = 0.88). The distribution of subscale scores was consistent with a normal distribution (skewness < ∣0.96∣ and kurtosis < ∣1.81∣; George & Mallery, 2016).
4.3 ∣. Knowledge measures
Respondents varied in their knowledge depending on the domain (Table 3; Figure 1b). Most respondents correctly indicated that HPV-associated cervical dysplasia is found among all women not just heterosexual women (85.9%, n = 67) and regularly screening gay/bisexual men for anal cancer can increase life expectancy (71.8%, n = 56). Less than half correctly indicated that LGBTQ patients avoid accessing health care due to difficulty communicating with providers (44.9%, n = 35). Less than a quarter correctly indicated that LGBTQ individuals have higher prevalence of smoking (24.4%, n = 19), transgender individuals are less likely to have health insurance (23.1%, n = 18), and LGBTQ individuals engage in more sun-seeking behaviours (6.4%, n = 5). The total score for correct responses ranged from 0 (none) to 5 out of 6 (M = 2.56, SD = 1.27).
TABLE 3.
Knowledge of LGBTQ health among surveyed advanced practice providers
|
n (%) |
Political affiliation |
LGBTQ Friends/Family |
Licensure |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Conservative | Moderate | Liberal | Otherc | Yes | No | Physician assistant |
Advanced registered nurse practitioner |
Anaesthesia-related licensure |
|
| 1. LGBTQ patients avoid accessing health care due to difficulty communicating with providers | ||||||||||
| Strongly Disagree/Disagree | 12 (15.4) | 4 (14.8) | 3 (23.1) | 3 (11.5) | 1 (9.1) | 10 (14.1) | 1 (20.0) | 1 (3.8) | 6 (17.1) | 4 (36.4) |
| Neutral | 31 (39.7) | 13 (48.1) | 6 (46.2) | 7 (26.9) | 5 (45.5) | 29 (40.8) | 2 (40.0) | 12 (46.2) | 11 (31.4) | 4 (36.4) |
| Strongly Agree/Agreea | 35 (44.9) | 10 (37.0) | 4 (30.8) | 16 (61.5) | 5 (45.5) | 32 (45.1) | 2 (40.0) | 13 (50.0) | 18 (51.4) | 3 (27.3) |
| 2. HPV-associated cervical dysplasia is only found in women with a history of heterosexual intercourse | ||||||||||
| Strongly Disagree/Disagreea | 67 (85.9) | 21 (77.9) | 12 (92.3) | 24 (92.3) | 10 (90.9) | 63 (88.7) | 4 (80.0) | 24 (92.3) | 28 (80.0) | 9 (81.8) |
| Neutral | 5 (6.5) | 3 (11.1) | 0 (0.0) | 2 (7.7) | 0 (0.0) | 4 (5.6) | 0 (0.0) | 0 (0.0) | 3 (8.6) | 2 (18.2) |
| Strongly Agree/Agree | 6 (7.7) | 3 (11.1) | 1 (7.7) | 0 (0.0) | 1 (9.1) | 4 (5.6) | 1 (20.0) | 2 (7.7) | 4 (11.4) | 0 (0.0) |
| 3. Regularly screening gay and bisexual men for anal cancer through anal Pap testing can increase life expectancy | ||||||||||
| Strongly Disagree/Disagree | 4 (5.1) | 1 (3.7) | 1 (7.7) | 2 (7.7) | 0 (0.0) | 4 (5.6) | 0 (0.0) | 2 (7.7) | 1 (2.9) | 0 (0.0) |
| Neutral | 18 (23.1) | 4 (14.8) | 3 (23.1) | 9 (34.6) | 2 (18.2) | 16 (22.5) | 2 (40.0) | 9 (34.6) | 6 (17.1) | 2 (18.2) |
| Strongly Agree/Agreea | 56 (71.8) | 22 (81.5) | 9 (69.2) | 15 (57.7) | 9 (81.8) | 51 (71.8) | 3 (60.0) | 15 (57.7) | 28 (80.0) | 9 (81.8) |
| 4. LGBTQ individuals tend to have a higher prevalence of smoking compared to non-LGBTQ individualsb | ||||||||||
| Strongly Disagree/Disagree | 17 (21.8) | 5 (18.5) | 3 (25.0) | 8 (30.8) | 0 (0.0) | 16 (22.9) | 0 (0.0) | 4 (15.4) | 9 (25.7) | 3 (27.3) |
| Neutral | 41 (52.6) | 14 (51.9) | 7 (58.3) | 10 (38.5) | 10 (90.9) | 37 (52.9) | 4 (80.0) | 17 (65.4) | 19 (54.3) | 3 (27.3) |
| Strongly Agree/Agreea | 19 (24.4) | 8 (29.6) | 2 (16.7) | 8 (30.8) | 1 (9.1) | 17 (24.3) | 1 (20.0) | 5 (19.2) | 7 (20.0) | 5 (45.5) |
| 5. LGBTQ individuals tend to engage in more sun-seeking behaviours compared to non-LGBTQ individuals | ||||||||||
| Strongly Disagree/Disagree | 20 (25.6) | 7 (25.9) | 5 (38.5) | 6 (23.1) | 1 (9.1) | 18 (25.4) | 1 (20.0) | 6 (23.1) | 10 (28.6) | 3 (27.3) |
| Neutral | 53 (67.9) | 17 (63.0) | 8 (61.5) | 18 (69.2) | 10 (90.9) | 49 (69.0) | 4 (80.0) | 19 (73.1) | 23 (65.7) | 6 (54.5) |
| Strongly Agree/Agreea | 5 (6.4) | 3 (11.1) | 0 (0.0) | 2 (7.7) | 0 (0.0) | 4 (5.6) | 0 (0.0) | 1 (3.8) | 2 (5.7) | 2 (18.2) |
| 6. Transgender individuals are less likely to have health insurance than other individuals | ||||||||||
| Strongly Disagree/Disagree | 15 (19.2) | 5 (18.5) | 4 (30.8) | 4 (15.4) | 1 (9.1) | 14 (19.7) | 0 (0.0) | 4 (15.4) | 9 (25.7) | 1 (9.1) |
| Neutral | 45 (57.7) | 19 (70.4) | 7 (53.8) | 12 (46.2) | 7 (63.6) | 42 (59.2) | 3 (60.0) | 17 (65.4) | 15 (42.9) | 8 (72.7) |
| Strongly Agree/Agreea | 18 (23.1) | 3 (11.1) | 2 (15.4) | 10 (38.5) | 3 (27.3) | 15 (21.1) | 2 (40.0) | 5 (19.2) | 11 (31.4) | 2 (18.2) |
Notes: Chi-squared tests indicated no significant differences.
Indicates correct response.
1 missing response resulted n = 77 for this item.
1 responded indicated "some other viewpoint," and 9 indicated they "prefer not to answer".
4.4 ∣. Stratified analyses
Among some of the attitude measures, significant differences were found by political affiliation, medical specialty, licensure, and having LGBTQ friends or family (Table 2). For political affiliation, significant differences were identified among confidence in knowledge of LGB health needs (p = .030), interest in education (p = .040) and being willing to be listed as an LGBTQ-friendly provider (p = .050). In comparisons of column proportions, liberals and conservatives reported significantly more confidence in their knowledge of health needs of LGB individuals and interest in education compared to moderates (p values <.05). Additionally, liberals were significantly more willing to be listed as an LGBTQ-friendly provider compared to moderates and those with other/unspecified viewpoints (p values <.05).
APPs with LGBTQ friends or family vs. without were more likely to endorse mandatory education (p = .022), and self-reported being more comfortable treating transgender patients (p < .001) and confident in their knowledge of transgender health needs (p = .004).
For comparisons among licensure, there were significant differences among interest in education (p = .019). Respondents with an Advanced Registered Nurse Practitioner license were more interested in LGBTQ-related education than those with an anaesthesia-related licensure (Anesthesiologist Assistant or Certified Registered Nurse Anesthetist; p values <.05). There were also overall differences among APPs who reported to assume patients are heterosexual upon first encounter (p = .045), but no significant column differences emerged after controlling for multiple comparisons.
For medical specialty, APPs in surgical oncology were more confident in their knowledge of transgender health (p = .008; 70.0%) vs. medical oncology (38.5%) or other specialties (52.0%; data not shown).
No differences by respondent characteristics were found among the knowledge items (p values >.05; Table 3). There were no consistent differences by age, years since graduation, religious practice, race/ethnicity, or sexual orientation for attitudes or knowledge items (p values >.05).
4.5 ∣. Attitude summary measure
A series of one-way ANOVAs were conducted with the significant demographics from the bivariate associations above as independent variables and the three Attitude Summary Measure subscales as dependent variables. Due to unequal group sizes, the adjusted F statistic—the Brown-Forsythe statistic—was used to determine group differences. Those with LGBTQ friends or family vs. without had a greater mean education-involvement score (M = 3.95 vs. M = 3.13; B-F[1, 5.44] = 11.39, p = .017) and comfort-confidence score (M = 4.13 vs. M = 3.65; B-F[1, 7.68] = 10.35, p = .013). By licensure, there were significant mean differences for education-involvement (B-F[2, 24.54] = 4.15, p = .028), with Bonferonni-adjusted post hoc tests indicating that Advanced Registered Nurse Practitioners had greater education interest (M = 4.23) than Physician Assistants (M = 3.77) and those with an anaesthesia-related licensure (M = 3.64).
Bivariate correlations indicate that total knowledge was significantly associated with practice beliefs (r = 0.34, p = .002), but not comfort-confidence or education-involvement (p values >.05) indicating that those who agreed that it is important to know patients’ sex assigned at birth, gender identity and sexual orientation are important to provide the best care tended to have greater overall knowledge.
4.6 ∣. Moderation analyses
Two moderation analyses examined the associations of knowledge, comfort-confidence and their interaction (knowledge × comfort-confidence) with education-involvement and practice beliefs. The model for practice beliefs was significant (F[3, 74] = 3.45, p = .021, R2 = 0.12). Specifically, greater total knowledge was positively related to higher practice belief scores (b = 0.23, p = .005), but comfort-confidence and the interaction term were not significant (p values >.05). This indicates that regardless of APPs’ average level of comfort-confidence, more overall knowledge correlated with stronger beliefs that knowing patients’ sexual orientation, gender identity and sex assigned at birth is important for providing the best care. The model for education-involvement was not significant (p = .206).
4.7 ∣. Pre–post confidence in LGB and transgender Health
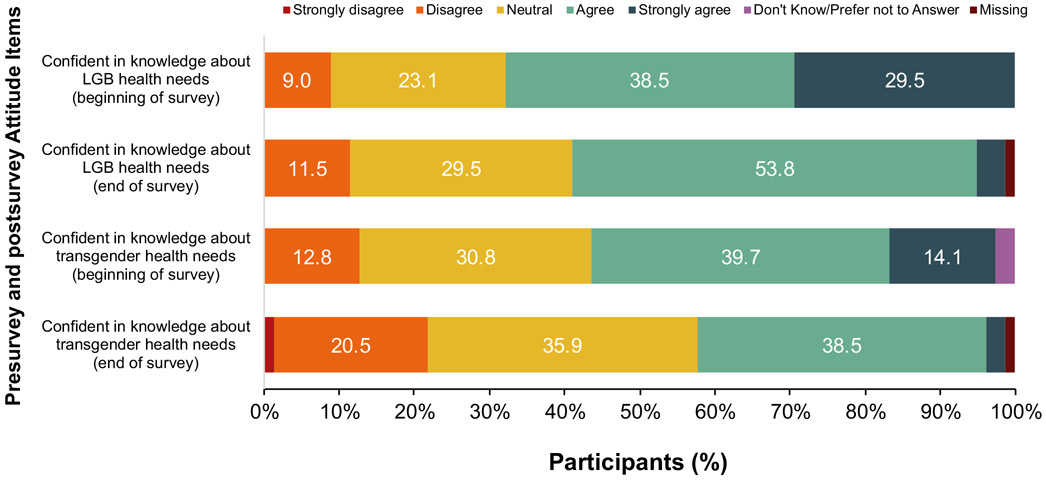
The average change in confidence in knowledge of LGB health presurvey and postsurvey significantly reduced from M = 3.88 (SD = 0.94) presurvey to M = 3.51 (SD = 0.75) postsurvey, t(76) = 4.41, p < .001. Likewise, respondents’ confidence in knowledge of transgender health significantly reduced from M = 3.55 (SD = 0.89) presurvey to M = 3.21 (SD = 0.85) postsurvey, t(76) = 3.35, p < .001 (Figure 2).
FIGURE 2.
Attitude items beginning and end of survey. Responses less than 5% are not labeled on the figure. LGB, lesbian, gay and bisexual
5 ∣. DISCUSSION
As APPs have an important and prominent role in oncology care, we conducted a survey of attitudes and knowledge of LGBTQ patient needs among a sample of APPs from an NCI-Designated Comprehensive Cancer Center. Overall, we found the majority of APPs reported being comfortable with and having confidence in their knowledge of LGBTQ health needs, but to a lesser extent, transgender patient needs. Most APPs were interested in further education in LGBTQ health needs, but fewer believed it should be mandatory. More APPs believed it is more important to know patients’ sex assigned at birth and gender identity than it is to know sexual orientation, to provide the best cancer care.
Overall knowledge was limited with no respondents answering all items correctly, and only 12% answering five out of six items correctly. However, this depended on the items with more respondents correctly indicating that HPV-associated cervical dysplasia was not only found in heterosexual women and less than half correctly indicating that LGBTQ individuals have a higher prevalence of smoking or that LGBTQ patients avoid health care due to difficulty communicating with their providers. This is consistent with published findings from surveys our team conducted among a national and regional sample of oncologists from NCI-Designated Comprehensive Cancer Centers (Schabath et al., 2019; Shetty et al., 2016), as well as other healthcare providers at an NCI-Designated Comprehensive Cancer Center in the Northeast United States that also demonstrated low knowledge of LGBTQ health needs (Banerjee et al., 2018). This lack of knowledge is not surprising given than one sample of nursing school baccalaureate faculty indicated low knowledge of and time devoted to teaching LGBTQ health (average of 2.12 hr; Lim et al., 2015). Despite low knowledge, APPs demonstrated a clear willingness and interest to receive more education. Qualitative findings among nurse practitioners indicate desire to provide quality care for LGBTQ patients, but low understanding of the unique healthcare needs and challenges balancing personal beliefs with acting professionally (Dorsen & Van Devanter, 2016).
Similar to previous studies among the general U.S. populations’ attitudes towards sexual and/or gender minorities, (Woodford, Silverschanz, Swank, Scherrer, & Raiz, 2012), individuals with LGBTQ friends/family and more liberal political affiliation had more positive attitudes in our sample. However, these factors were not associated with LGBTQ-related health knowledge as Banerjee et al. (2018) found in their study of healthcare providers in an NCI-Designated Cancer Center. Attitudes may be more influenced by respondent characteristics, whereas knowledge might be associated with exposure to LGBTQ-related content in education. Although having LGBTQ friends/family was not associated with knowledge in our sample, this may be due to the fact that there was not enough variability in this item; thus, conclusions are difficult to draw. This is important because healthcare providers’ negative attitudes and lack of knowledge regarding LGBTQ health may affect patients’ willingness to seek care, as well as the quality of care received. Previous negative experiences or fear of negative experiences, including discrimination in the healthcare setting, may discourage LGBTQ individuals to seek care or disclose important information about their sexual orientation, gender identity or sexual behaviours. In a qualitative study among U.K.-based LGBTQ people facing advanced illnesses, including cancer, participants reported that their decision to disclose their identity was shaped by prior negative experiences (Bristowe et al., 2018). In particular, transgender late-stage patients reported fear and anticipatory stress of disclosure and receiving intimate care, such as bathing (Bristowe et al., 2018). Exposure to discrimination among transgender individuals has been associated with delaying or avoiding seeking care, particularly among those who reported lack of access to a knowledgeable healthcare provider (Jaffee, Shires, & Stroumsa, 2016). While attitudes may be difficult to change, early education may strengthen the cultural competency of the workforce and potentially reduce the harmful impact of negative provider attitudes over time.
Greater overall LGBTQ health knowledge was associated with stronger beliefs that knowing patients’ sexual orientation and gender identity information is important to providing the best care, even when controlling for comfort/confidence as in the moderation analyses. Knowledge was not directly associated with other attitudes, such as comfort/confidence, interest in education or being listed as an LGBTQ-friendly provider. This may suggest that for APPs, knowledge is a mutable avenue for intervention development and increasing knowledge may increase understanding that sexual orientation and gender identity information is important to understand the “whole” patient, as suggested in the Meaningful Use standards 3 (CMS, 2015). Additionally, we observed a decrease in self-reported confidence in health needs of LGBTQ patients from presurvey to postsurvey. This may indicate that after to being exposed to knowledge items, APPs become aware that they may not be as knowledgeable as they first believed. It is unknown if this has an effect on comfort, but future studies should consider this when developing education interventions.
The role of APPs is increasingly important in the care of oncology patients, with APPs providing a variety of direct patient care services such as counselling, treatment management, evaluation of new patients, follow-up care and genetic counselling (Bruinooge et al., 2018). With this wide scope of practice, APPs have a unique opportunity to interact with patients and their caregivers throughout the cancer continuum. Knowledge of sexual orientation and gender identity information and comfort with working with LGBTQ patients is integral to the quality of care provided by the growing number of APPs. Education of APPs such as nurse practitioners and physician assistants should integrate LGBTQ-related health information in its curriculum that could perhaps be borrowed from new curricula developed for medical students (e.g., www.mededportal.org). For practicing clinicians, continuing education should be a priority and such training efforts are available from various online sources such as The National LGBT Health Education Organization (www.lgbthealtheducation.org); the Human Rights Campaign https://www.hrc.org/hei/staff-training-overview; and GLMA: Health Professionals Advancing LGBTQ Equality (previously known as the Gay & Lesbian Medical Association) www.glma.org.
5.1 ∣. Limitations and future directions
Despite the strengths, we acknowledge several limitations of this study . First, this study was conducted at one NCI-Designated Cancer Center; therefore, findings may not apply to other geographic or community-based oncology practices. Future studies should examine these relationships in diverse oncology settings to enhance generalisability. Second, sampling bias may have had an impact on findings since participation was voluntary and anonymous and it was not possible to compare responders to nonresponders. The relatively low response rate (39%) may indicate that those who participated were more interested or open to the topic than nonresponders. Although the Dillman Method was used, the response rate may reflect a divergence from the original mode (i.e., mailed paper survey vs. email) or general declining participation in survey research since the original publication. Third, the cross-sectional nature of the study, the small sample size and the large number of statistical tests limits confidence in the robustness of findings. In the future, larger prospective samples are recommended. Fourth, the measures used have not been formally tested for validity and reliability, although preliminary evidence has been presented in a national sample of oncologists (Schabath et al., 2019). Future studies should examine the psychometric properties of the items and as new evidence emerges, expand particularly the knowledge scale to improve the content validity. Finally, social desirability may have limited participants’ willingness to indicate negative attitudes, which may have underestimated the prevalence of negative attitudes and their association with knowledge. Future studies should utilise implicit measures and test their association with knowledge.
6 ∣. CONCLUSIONS
This study is the first to our knowledge to describe the knowledge and attitudes of LGBTQ health needs among a sample of oncology advanced practice providers. Overall, the responding APPs in this study were comfortable with LGBTQ patients, but knowledge was low. This is important because lower knowledge was associated with reduced belief that sexual orientation and gender identity information is important to providing the best care to patients, which is not in accord with current standards set forth by the Joint Commission (CMS, 2015). Certain provider characteristics may be linked to negative attitudes and continued emphasis on the importance of sexual orientation and gender identity data collection from the American Society of Clinical Oncology and the National Academy of Medicine is important to garner support for education efforts and ultimately improving the provision of quality care for LGBTQ individuals across the cancer continuum.
7 ∣. RELEVANCE TO CLINICAL PRACTICE
Oncology APPs should be prepared to treat cancer patients from a variety of backgrounds, including SGM patients. Awareness of LGBTQ health disparities is increasing, and oncology APPs display generally positive attitudes towards LGBTQ cancer patients, but gaps in knowledge of LGBTQ-specific health needs persist. Targeted education for APPs both during training and during continuing education and focusing on increasing knowledge is likely to lead to increased provision of quality care for LGBTQ patients.
Supplementary Material
What does this paper contribute to the wider global clinical community?
Oncology advanced practice providers have positive attitudes towards sexual and gender minority patients, but low knowledge regarding their health needs.
Education of advanced practice providers such as nurse practitioners and physician assistants should integrate sexual and gender minority-related health information in its curriculum and should be a priority in continuing education efforts.
Acknowledgments
Funding information
This study was funded by a Miles for Moffitt Milestone Award (principal investigators: G.P.Q. and M.B.S.) MES was funded by the National Cancer Institute (R25CA090314) and is currently funded by the Agency for Healthcare Research and Quality (T32HS026120). This work has also been supported in part by a Cancer Center Support Grant (CCSG) at the H. Lee Moffitt Cancer Center and Research Institute; an NCI designated Comprehensive Cancer Center (grant number P30CA76292).
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
REFERENCES
- American Academy of Nursing on Policy. (2016). Lesbian, gay, bisexual, and transgender health disparities are a global concern. Nursing Outlook, 64(3), 279–280. [Google Scholar]
- Banerjee SC, Walters CB, Staley JM, Alexander K, & Parker PA (2018). Knowledge, beliefs, and communication behavior of oncology health-care providers (HCPs) regarding lesbian, gay, bisexual, and transgender (LGBT) patient health care. Journal of Health Communication, 23(4), 329–339. 10.1080/10810730.2018.1443527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradford J, Cahill S, Grasso C, & Makadon H (2012). How to gather data on sexual orientation and gender identity in clinical settings. Retrieved from https://www.lgbthealtheducation.org/wp-content/uploads/policy_brief_how_to_gather.pdf [Google Scholar]
- Bristowe K, Hodson M, Wee B, Almack K, Johnson K, Daveson BA, … Harding R (2018). Recommendations to reduce inequalities for LGBT people facing advanced illness: ACCESSCare national qualitative interview study. Palliative Medicine, 32(1), 23–35. 10.1177/0269216317705102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruinooge SS, Pickard TA, Vogel W, Hanley A, Schenkel C, Garrett-Mayer E, … Williams SF (2018). Understanding the role of advanced practice providers in oncology in the United States. Journal of Oncology Practice, 14(9), e518–e532. 10.1200/jop.18.00181 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2015). Medicare and medicaid programs; Electronic health record incentive program-stage 3 and modifications to meaningful use in 2015 through 2017. Federal Register, 80, 62761–62955. [PubMed] [Google Scholar]
- Ceres M, Quinn GP, Loscalzo M, & Rice D (2018). Cancer screening considerations and cancer screening uptake for lesbian, gay, bisexual, and transgender persons. Seminars in Oncology Nursing, 34(1), 37–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA (1978). Mail and telephone surveys: The total design method. New York, NY: John Wiley & Sons. [Google Scholar]
- Dorsen C, & Van Devanter N (2016). Open arms, conflicted hearts: Nurse-practitioner’s attitudes towards working with lesbian, gay and bisexual patients. Journal of Clinical Nursing, 25, 3716–3727. [DOI] [PubMed] [Google Scholar]
- Eliason MJ, Dibble S, & DeJoseph J (2010). Nursing's silence on lesbian, gay, bisexual, and transgender issues: The need for emancipatory efforts. Advances in Nursing Science 33(3), 206–218. [DOI] [PubMed] [Google Scholar]
- Fusco E (2015). Nurse practitioners' growing role in oncology. Oncology Times, 37(7), 4–5. [Google Scholar]
- George D, & Mallery P (2016). IBM SPSS statistics 23 step by step: A simple guide and reference. New York, NY: Routledge. [Google Scholar]
- Hayes AF (2016). The PROCESS macro for SPSS and SAS. Retrieved from http://www.processmacro.org/index.html [Google Scholar]
- Hegazi A, & Pakianathan M (2018). LGBT sexual health. Medicine, 46(5), 300–303. [Google Scholar]
- Institute of Medicine (US) Committee on Lesbian G, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: National Academies Press (US). [PubMed] [Google Scholar]
- Jaffee KD, Shires DA, & Stroumsa D (2016). Discrimination and delayed health care among transgender women and men: Implications for improving medical education and health care delivery. Medical Care, 54(11), 1010–1016. [DOI] [PubMed] [Google Scholar]
- Kitts RL (2010). Barriers to optimal care between physicians and lesbian, gay, bisexual, transgender, and questioning adolescent patients. Journal of Homosexuality, 57(6), 730–747. 10.1080/00918369.2010.485872 [DOI] [PubMed] [Google Scholar]
- Lim F, Johnson M, & Eliason M (2015). A national survey of faculty knowledge, experience, and readiness for teaching lesbian, gay, bisexual, and transgender health in baccalaureate nursing programs. Nursing Education Perspectives, 36(3), 144–152. [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychology of Sexual Orientation and Gender Diversity, 1(S), 3–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, … Lunn MR (2011). Lesbian, gay, bisexual, and transgender-related content in undergraduate medical Education. Journal of the American Medical Association, 306(9), 971–977. [DOI] [PubMed] [Google Scholar]
- Pérez-Stable EJ (2016). Director’s message: Sexual and gender minorities formally designated as a health disparity population for research purposes. Retrieved from https://www.nimhd.nih.gov/about/directors-corner/messages/message_10-06-16.html [Google Scholar]
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, … Schabath MB (2015). Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA: A Cancer Journal for Clinicians, 65(5), 384–400. 10.3322/caac.21288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin JA, Riskind RG, & Nosek BA (2015). Health care providers' implicit and explicit attitudes toward lesbian women and gay men. American Journal of Public Health, 105(9), 1831–1841. 10.2105/ajph.2015.302631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez NF, Sanchez JP, & Danoff A (2009). Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. American Journal of Public Health, 99(4), 713–719. 10.2105/ajph.2007.132035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schabath MB, Blackburn CA, Sutter ME, Kanetsky PA, Vadaparampil SK, Simmons VN, … Sutton SK, Quinn GP (2019). National survey of oncologists at national cancer institute-designated comprehensive cancer centers: Attitudes, knowledge, and practice behaviors about lesbian, gay, bisexual, transgender, and queer/questioning patients with cancer. Journal of Clinical Oncology, 37(7), 547–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shetty G, Sanchez JA, Lancaster JM, Wilson LE, Quinn GP, & Schabath MB (2016). Oncology healthcare providers' knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Education and Counseling, 99(10), 1676–1684. 10.1016/j.pec.2016.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirota T (2013). Attitudes among nurse educators toward homosexuality. Journal of Nursing Education, 52(4), 219–227. 10.3928/01484834-20130320-01 [DOI] [PubMed] [Google Scholar]
- Snelgrove JW, Jasudavisius AM, Rowe BW, Head EM, & Bauer GR (2012). "Completely out-at-sea" with "two-gender medicine": A qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Service Research, 12, 110 10.1186/1472-6963-12-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, & Initiative, Strobe (2014). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. International Journal of Surgery, 12(12), 1495–1499.25046131 [Google Scholar]
- Wender R, Sharpe KB, Westmaas JL, & Patel AV (2016). The American Cancer Society's approach to addressing the cancer burden in the LGBT community. LGBT Health, 3(1), 15–18. [DOI] [PubMed] [Google Scholar]
- Woodford MR, Silverschanz P, Swank E, Scherrer KS, & Raiz L (2012). Predictors of heterosexual college students’ attitudes toward LGBT people. Journal of LGBT Youth, 9(4), 297–320. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.