Abstract
Background:
Amniotic band syndrome (ABS) is a rare condition of controversial etiology that is associated with varying degrees of anomalies. This study reports a case of a newborn with ABS associated with double encephalocele in the frontal region.
Case Description:
A 29-year-old primiparous woman with no history of prenatal infection or consanguineous marriage had a cesarean section at gestational week 38, giving birth to a newborn who was well but had limb anomalies (constriction rings, amputations, and syndactyly) and craniofacial anomalies, mainly double frontal encephalocele. The patient underwent surgical repair and subsequent placement of a ventriculoperitoneal shunt.
Conclusion:
Studies clarifying this uncommon association with double encephalocele are limited. ABS associated with double encephalocele is rare and even more complex when associated with other anomalies. Thus, the conditions in such children are severe and require multidisciplinary monitoring.
Keywords: Amniotic band syndrome, Amputations, Encephalocele, Syndactyly

INTRODUCTION
Amniotic band syndrome (ABS) is a rare congenital condition. Its incidence varies from 1:1200 to 1:15,000 live births, and it has an equal distribution between sexes. The occurrence of ABS is sporadic, and the prognosis of ABS depends on the severity of the anomalies and degree of involvement of the affected organs. The etiology of ABS is controversial, and several synonyms have been reported in the literature, including ADAM (Amniotic Deformity, Adhesions, and Mutilations) complex, amnion rupture sequence, amniotic band sequence, amniotic band disruption complex, congenital ring constriction, constriction ring syndrome, transverse limb defects, annular constriction bands, aberrant tissue bands, Streeter’s dysplasia or syndrome, and early amnion rupture spectrum.[1,2,5,9,22]
Portal was the first to report this malformation in 1685.[17] The first theory describing annular constrictions and other fetal abnormalities in this syndrome were proposed by Montgomery in 1832.[14] A wide variety of clinical manifestations have been reported, from simple constriction rings in the fingers with amputations to complex craniofacial malformations (cleft lip, encephalocele, hydrocephalus, and microcephaly) and visceral malformations (ectopia cordis, gastroschisis, renal agenesis, and anal atresia).[13,16]
The present study reports a case of a newborn with ABS associated with double frontal encephalocele, which is a rare malformation.
CASE DESCRIPTION
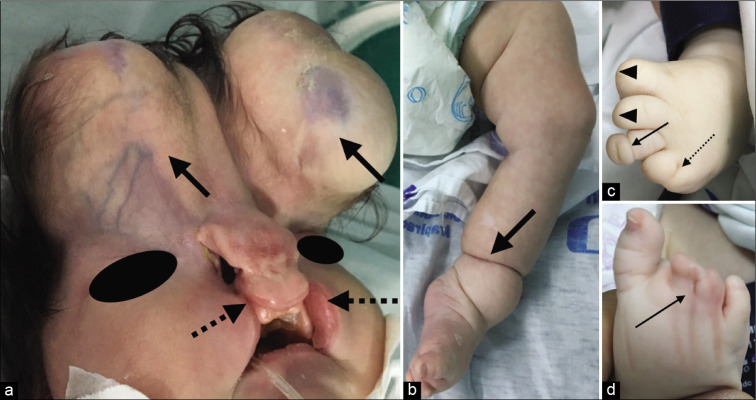
The mother was a 29-year-old primiparous woman with no history of infections during pregnancy, a consanguineous marriage, or exposure to teratogens. She was admitted to Santa Mônica Maternity School at gestation week 38; she underwent a cesarean section and delivered a female newborn who was well, with an APGAR scores were 8 and 9 at 1–5 min, respectively. Weight 3550 g, height 51 cm, non-measurable head circumference, and chest circumference 35 cm. The newborn had the following abnormalities: multiple craniofacial malformations such as bilateral cleft lip, hypertelorism, and bilateral frontal encephalocele [Figure 1a] and upper and lower limb malformations such as finger amputations, syndactyly, and constriction rings [Figure 1bd]. Echocardiography, chest computed tomography (CT) scan, and ultrasound examination of the abdomen were normal. Chromosome analysis revealed a normal 46, XX karyotype. In view of the phenotypic traits described above, the main diagnostic hypothesis was ABS.
Figure 1:
(a) Double frontal encephalocele (black arrow), bilateral complete cleft lip (dotted black arrow) and hypertelorism; (b) Left leg: constriction ring above ankle joints (black arrow); (c) Left foot: partial amputation of the 1st and 2nd fingers (black arrowheads), constriction ring of the 3rd finger (black arrow) and fenestrated syndactyly of the 4th and 5th fingers (dotted black arrow); (d) Right foot: fenestrated syndactyly of the 2nd, 3rd, and 4th fingers (black arrow).
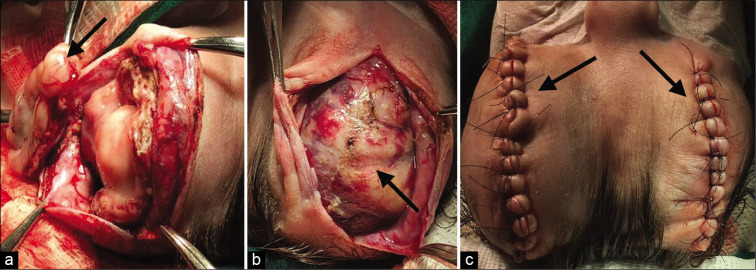
The patient underwent surgical repair of the double frontal encephaloceles (6 × 4 cm on the right and 6 × 5.5 cm on the left), with no complications [Figure 2]. At 30 days of age, the infant did not have craniosynostosis on 3D CT [Figure 3a], evidenced dysmorphic ventricle with open lip schizencephaly [Figure 3b], requiring ventriculoperitoneal shunt placement [Figure 3c], and satisfactory postoperative results were obtained [Figure 3d]. At present, the infant is scheduled to undergo cleft lip surgery and is being monitored by a multidisciplinary team.
Figure 2:
(a) Left frontal encephalocele repair with nonfunctional brain tissue removal (black arrow); (b) right frontal encephalocele repair; (c) postoperative after encephalocele resection.
Figure 3:
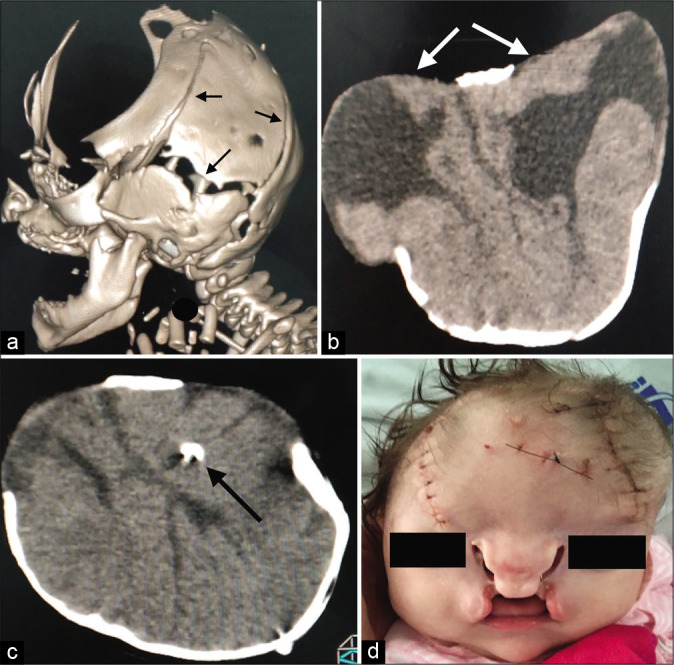
(a) and (b) Frontal cranial defect with open sutures (black arrows), without craniosynostosis showing two separate sacs with malformed neural tissue (white arrows): dysmorphic ventricle, open lip schizencephaly, lissencephaly spectrum, agenesis of the corpus callosum; (c) ventriculoperitoneal shunt placement (black arrow). (d) After shunt placement.
DISCUSSION
In an attempt to explain the etiopathogenesis of ABS, two theories have been proposed. The first is the intrinsic theory, proposed by George Streeter in 1930; this theory states that a dysfunction in embryogenesis would lead to imperfect histogenesis of the fetal tissue, resulting in the fibrous bands. However, it fails to explain most of the anomalies observed.[18,19] The second theory is the extrinsic theory, proposed by Torpin in 1965; this theory states that rupture of the amnion would result in the formation of fibrous tissue strings responsible for constriction bands, amputation, and other anomalies.[20] Depending on the stage of pregnancy, the amniotic rupture would be responsible for the extent of severe defects. For example, in the gestational week 3, the amniotic rupture could lead to more severe lesions such as anencephaly, encephalocele, meningocele, facial anomalies, eye defects, unusual cleft palate, ectopia cordis, and placental adhesion on the head, abdomen, or both. Amniotic rupture in the gestational week 7 may present less severe lesions such as craniostenosis, omphalocele, gastroschisis, amputations, limb hypoplasia, pseudosyndactyly, constriction rings with distal lymphedema, foot deformity, and hip dislocation.[3,12,22] Fetal death by cord strangulation has also been reported.[7]
Some risk factors associated with amniotic rupture include maternal abdominal injuries, surgical interventions before or during pregnancy, use of intrauterine devices, uterine malformation, collagen diseases (osteogenesis imperfecta and Ehlers-Danlos syndrome), drugs (clomiphene and contraceptives), and amniocentesis (chorionic villus biopsy).[5]
Other theories also try to explain the anomalies caused by ABS, such as the vascular disruption theory, proposed in 1987, according to which vascular damage during embryogenesis would lead to destruction of existing structures, thereby causing internal and external defects.[8,9]
A genetic basis has also been considered to explain these anomalies of ABS, theorizing that the cause could be a mutant gene, such as a human homolog of the Ds gene (“disorganization gene”) of mutant mice, which would cause a wide variety of anomalies.[6]
Some genetic syndromes involving cleft lip and palate can also present oral or facial fibrous bands. These include Van der Woude syndrome and popliteal pterygium syndrome, which involve IRF6 mutations, and Hay-Wells syndrome, with p63 mutations.[4]
According to Guzmán-Huerta et al.,[10] the most common anomalies associated with ABS are craniofacial defects such as holoprosencephaly, ventriculomegaly, hydrocephalus, acrania, encephalocele, and cleft lip and palate, which have been reported in 78% of cases.
In the present study, the rare craniofacial defect associated with ABS was double encephalocele, which is characterized by multiple neural tube defects of rare occurrence.[23] According to Van Allen et al.[21]and Nakatsu et al.,[15] there are several points of neural tube closure controlled by one or more genes, and the failure of one or more of them to close could lead to the formation of multiple neural tube defects. Unfortunately, this does not explain the relationship between double encephalocele and ABS. The theory proposed by Hunter et al.[11] focused on craniofacial anomalies; it states that in the presence of ABS, there is a deficiency in the primary ectoderm during embryogenesis that results in amnion-neural tube connection. This would possibly explain certain cranial defects, including encephalocele.
The diagnosis of ABS is most often made on the basis of the clinical findings of anatomical abnormalities. Chromosomal analysis is usually normal.[18] The treatment depends on the existing anomalies, which vary from those that are life threatening to those that impair function and esthetics. Prenatal treatment, such as fetoscopy for removing constriction bands, is still controversial, because there are few consistent studies. Furthermore, prenatal procedures require a multidisciplinary and complex structure.[9]
CONCLUSION
ABS may be associated with several anomalies ranging from the less severe defects such as constriction rings of the fingers to the most complex craniofacial malformations, as that reported in the present study. Double encephalocele in the presence of ABS is a rare condition, and in our case, it was accompanied by other existing anomalies (cleft lip, limb constriction rings, and amputations). Such conditions are severe, with high morbidity and mortality rates. Patients who survive such conditions require multidisciplinary monitoring to improve their quality of life.
Footnotes
How to cite this article: da Silva AJ, Silva CS, Mariano SC. Amniotic band syndrome with double encephalocele: A case report. Surg Neurol Int 2020;11:448.
Contributor Information
Aldo Jose Ferreira da Silva, Email: neuroajfs@bol.com.br.
Carolina S. Magalhães e Silva, Email: carolmagalhaes02@hotmail.com.
Sonaly C. R. Mariano, Email: sonalymariano@outlook.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Askins G, Ger E. Congenital constriction band syndrome. J Pediatr Orthop. 1988;8:461–6. doi: 10.1097/01241398-198807000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Burgess RC. Brachydactyly in acrosyndactyly. J Hand Surg Am. 1991;16:125–6. doi: 10.1016/s0363-5023(10)80026-7. [DOI] [PubMed] [Google Scholar]
- 3.Chen H, Gonzalez E, Opitz JM, Reynolds JF. Amniotic band sequence and its neurocutaneous manifestations. Am J Med Genet. 1987;28:661–73. doi: 10.1002/ajmg.1320280314. [DOI] [PubMed] [Google Scholar]
- 4.Cignini P, Giorlandino C, Padula F, Dugo N, Cafà EV, Spata A. Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. J Prenat Med. 2012;6:59–63. [PMC free article] [PubMed] [Google Scholar]
- 5.da Silva G, Cammarata SF, González-Coira M, Lacruz MA, Rendon B. Amniotic band syndrome: 3 case reports. Rev Chil Pediatr. 2008;79:172–80. [Google Scholar]
- 6.Donnai D, Winter RM. Disorganisation: A model for early amnion rupture? J Med Genet. 1989;26:421–5. doi: 10.1136/jmg.26.7.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foulkes GD, Reinker K. Congenital constriction band syndrome: A seventy-year experience. J Pediatr Orthop. 1994;14:242–8. doi: 10.1097/01241398-199403000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Goldfarb CA, Sathienkijkanchai A, Robin NH. Amniotic constriction band: A multidisciplinary assessment of etiology and clinical presentation. J Bone Joint Surg Am. 2009;91(Suppl 4):68–75. doi: 10.2106/JBJS.I.00339. [DOI] [PubMed] [Google Scholar]
- 9.González ZI, Padilla F. Complex of amniotic deformities, adhesions, mutilations: Endless debate. Bol Med Hosp Infant Mex. 2015;72:159–68. doi: 10.1016/j.bmhimx.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Guzmán-Huerta ME, Muro-Barragán SA, Acevedo-Gallegos S, Velázquez-Torres B, Gallardo-Gaona JM, Ramírez-Calvo JA, et al. Amniotic band sequence: Prenatal diagnosis, phenotype descriptions, and a proposal of a new classification based on morphologic findings. Rev Invest Clin. 2013;65:300–6. [PubMed] [Google Scholar]
- 11.Hunter AG, Seaver LH, Stevenson RE. Limb-body wall defect. Is there a defensible hypothesis and can it explain all the associated anomalies? Am J Med Genet A 2011 ; 155:2045–59. doi: 10.1002/ajmg.a.34161. [DOI] [PubMed] [Google Scholar]
- 12.Kulkarni ML, Gopal PV. Amniotic band syndrome. Indian Pediatr. 1990;27:471–6. [PubMed] [Google Scholar]
- 13.Lobato G. Amniotic band: Sonographic findings and correlations etiopathogenic. Femina. 2008;36:159–63. [Google Scholar]
- 14.Montgomery WF. Observation on the spontaneous amputation of the limbs of the fetus in utero, with an attempt to explain the occasional cause of its production. Dublin Med Chem Sci J. 1832;1:140–4. [Google Scholar]
- 15.Nakatsu T, Uwabe C, Shiota K. Neural tube closure in humans initiates at multiple sites: Evidence from human embryos and implications for the pathogenesis of neural tube defects. Anat Embryol (Berl) 2000;201:455–66. doi: 10.1007/s004290050332. [DOI] [PubMed] [Google Scholar]
- 16.Pardini AG, Santos MA, Freitas AD. Congenital constriction bands. Acta Ortop Bras. 2001;9:3–10. [Google Scholar]
- 17.Portal P. Paris: Gabriel Martin; 1685. La Pratique des Accouchements Soutenue d’un Grand Nombre D’observations. [PubMed] [Google Scholar]
- 18.Rebello CM, Leone CR, Zugaib M, Ramos JL, Gonzáles CH. Amniotic band syndrome. Pediatria (Säo Paulo) 1990;11:26–9. [Google Scholar]
- 19.Streeter GL. Focal deficiencies in fetal tissues and their relation to intrauterine amputation. Contrib Embryol Carnegie Inst. 1930;22:1–44. [Google Scholar]
- 20.Torpin R. Amniochorionic mesoblastic fibrous strings and amnionic bands: Associated constricting fetal malformations or fetal death. Am J Obstet Gynecol. 1965;91:65–75. doi: 10.1016/0002-9378(65)90588-0. [DOI] [PubMed] [Google Scholar]
- 21.van Allen MI, Kalousek DK, Chernoff GF, Juriloff D, Harris M, McGillivray BC, et al. Evidence for multi-site closure of the neural tube in humans. Am J Med Genet. 1993;47:723–43. doi: 10.1002/ajmg.1320470528. [DOI] [PubMed] [Google Scholar]
- 22.Walter JH, Jr, Goss LR, Lazzara AT. Amniotic band syndrome. J Foot Ankle Surg. 1998;37:325–33. doi: 10.1016/s1067-2516(98)80070-7. [DOI] [PubMed] [Google Scholar]
- 23.Yhoshu E, Dash V, Bawa M. Double encephalocele: An unusual presentation. J Pediatr Neurosci. 2018;13:264–6. doi: 10.4103/jpn.JPN_22_18. [DOI] [PMC free article] [PubMed] [Google Scholar]