Abstract
Background
Sugar-sweetened beverage (SSB) consumption contributes to obesity, a risk factor for 13 cancers. Although SSB taxes can reduce intake, the health and economic impact on reducing cancer burdens in the United States are unknown, especially among low-income Americans with higher SSB intake and obesity-related cancer burdens.
Methods
We used the Diet and Cancer Outcome Model, a probabilistic cohort state-transition model, to project health gains and economic benefits of a penny-per-ounce national SSB tax on reducing obesity-associated cancers among US adults aged 20 years and older by income.
Results
A national SSB tax was estimated to prevent 22 075 (95% uncertainty interval [UI] = 16 040-28 577) new cancer cases and 13 524 (95% UI = 9841-17 681) cancer deaths among US adults over a lifetime. The policy was estimated to cost $1.70 (95% UI = $1.50-$1.95) billion for government implementation and $1.70 (95% UI = $1.48-$1.96) billion for industry compliance, while saving $2.28 (95% UI = $1.67-$2.98) billion cancer-related healthcare costs. The SSB tax was highly cost-effective from both a government affordability perspective (incremental cost-effectiveness ratio [ICER] = $1486, 95% UI = -$3516-$9265 per quality-adjusted life year [QALY]) and a societal perspective (ICER = $13 220, 95% UI = $3453-$28 120 per QALY). Approximately 4800 more cancer cases and 3100 more cancer deaths would be prevented, and $0.34 billion more healthcare cost savings would be generated among low-income (federal poverty-to-income ratio [FPIR] ≤ 1.85) than higher-income individuals (FPIR > 1.85).
Conclusions
A penny-per-ounce national SSB tax is cost-effective for cancer prevention in the United States, with the largest health gains and economic benefits among low-income Americans.
Obesity is an established risk factor for 13 types of cancers (1, 2). Overweight and obesity-associated cancers account for 40% of all new cancer cases diagnosed in 2014 in the United States (3). The estimated medical spending for cancer care exceeds $130 billion in 2020 (4). The economic burden of cancer will further increase if the trends for obesity-associated cancers continue (5). Thus, it is critical to identify effective and cost-effective strategies to reduce obesity-associated cancer burdens in the United States.
High consumption of sugar-sweetened beverage (SSB) is an important contributor to the obesity epidemic in the United States (6,7). Despite some recent declines (8,9), SSB consumption remains the largest source of added sugar in American’s diets (9–12). High SSB consumption and obesity disproportionately affect individuals of low socioeconomic status (9,13,14), contributing to widening health disparities (1). Decreasing SSB consumption serves as an important target for preventing obesity-associated cancer burden and reducing cancer disparities in the United States.
Taxes on SSBs have risen to the forefront of public health efforts and policy debates in recent years (15,16). The beverage industry has aggressively lobbied for the repeal of national taxes (16–18). Understanding the potential health impacts, costs, and cost-effectiveness of such taxes for cancer prevention would inform policy discussions and debates in the United States and elsewhere.
Although prior studies have evaluated the potential impact of a national SSB tax on cardiovascular diseases (19,20), its potential effects on obesity-related cancer burdens remain unknown. To address this question, we used a population-based Diet and Cancer Outcome Model (DiCOM) to estimate the health gains and cost-effectiveness of a national penny-per-ounce SSB tax, overall and by age, sex, race and ethnicity, and income on preventing obesity-associated cancer burdens and reducing cancer disparities.
Methods
Study Overview and Model
We used the DiCOM, a probabilistic cohort state-transition model, to evaluate the effect of a national penny-per-ounce SSB excise tax on reducing obesity-associated cancer burdens and disparities among US adults over a lifetime. The DiCOM projects the population impact of implementing nutrition policies on health and economic outcomes. Starting from cancer-free individuals representative of the US population, the model simulates the development and progression of cancer as the individuals transition through different health states over a lifetime and tracks life expectancy, cancer-related quality of life, and health-related costs under alternative policy scenarios (Supplementary Figure 1, available online) (21).
To assess policy impact, the model compared 2 scenarios: implementing a national penny-per-ounce SSB tax and status quo (no policy). The DiCOM incorporates data on national population demographics, SSB intakes, estimated effects of SSB intake on obesity and obesity on cancer risk, policy implementation costs, and health-related costs (see Table 1). This study was exempt from the institutional review board review.
Table 1.
Key input parameters and data sources for the Diet and Cancer Outcome Model (DiCOM) a
| Model input parameters | Description | Data sources | |
|---|---|---|---|
| Population demographic characteristics of US adults | Age, sex, and race/ethnicity distribution among US adults aged 20 years and older, stratified by income | NHANES 2013-2016 | |
| Percent of overweight or obese (BMI ≥ 25 kg/m2) among US adults | Age-, sex-, and race/ethnicity-specific prevalence of overweight and obesity among US adults aged 20 years and older, stratified by income | NHANES 2013-2016 | |
| SSB consumption among US adults | Age-, sex-, and race/ethnicity-specific SSB consumption among US adults aged 20+ years and older, stratified by income | NHANES 2013-2016 Supplementary Methods (available online) Supplementary Table 3 (available online) | |
| Policy specification | The national penny-per-ounce tax on SSB | Supplementary Table 2 (available online) | |
| Policy effect size estimates, % (95 % CI) | Change in SSB intake per 10% change in price |
Supplementary Methods (available online) Supplementary Table 4 (available online) Wada et al., 2015 (22) |
|
| Total US adult population | −0.66 (-0.95 to -0.36) | ||
| Low-income US adults (FPIR ≤ 1.85) | −1.03 (-1.58 to -0.47) | ||
| Higher-income US adults (FPIR > 1.85) | −0.51 (-0.95 to -0.36) | ||
| Policy implementation costs, $ millions, annually |
Supplementary Methods (available online) Supplementary Table 5 (available online) Reports from Muni services |
||
| Government administration costs | 1% of SSB tax revenue | ||
| Industry compliance costs | 1% of SSB tax revenue | ||
| Cancer incidence and survival | Incidence and 5-year relative survival rates for each cancer type by age, sex, and race/ethnicity |
SEER Supplementary Methods (available online) |
|
| Effect size estimates of SSB-BMI, kg/m2 | β (95% CI), per 1 serving/d increase in SSB |
Mozzafarian et al., 2011 (23) |
|
| Individuals with BMI <25 kg/m 2 | 0.10 (0.05 to 0.15) | ||
| Individuals with BMI ≥ 25 kg/m 2 | 0.23 (0.14 to 0.32) | ||
| Relative risk (95% CI) estimates of BMI-cancerrisk, per 5 kg/m2 increase in BMI | |||
| Endometrial cancer | 1.50 (1.42 to 1.59) | WCRF/AICR, 2018 (24) Lauby-Secretan et al., 2016 (2) | |
| Esophageal adenocarcinoma | 1.48 (1.35 to 1.62) | ||
| Kidney cancer | 1.30 (1.25 to 1.35) | ||
| Liver cancer | 1.30 (1.16 to 1.46) | ||
| Gallbladder cancer | 1.25 (1.15 to 1.37) | ||
| Stomach cancer (gastric cardia) | 1.23 (1.07 to 1.40) | ||
| Female breast cancer (postmenopausal) | 1.12 (1.09 to 1.15) | ||
| Pancreatic cancer | 1.10 (1.07 to 1.14) | ||
| Multiple myeloma | 1.09 (1.03 to 1.16) | ||
| Advanced prostate cancer | 1.08 (1.04 to 1.12) | ||
| Thyroid cancer | 1.06 (1.02 to 1.10) | ||
| Ovarian cancer | 1.06 (1.02 to 1.11) | ||
| Colorectal cancer | 1.05 (1.03 to 1.07) | ||
| Health-related costs, $ million, per year | Health-related cost estimates for individuals with cancer for each cancer type and the general population based on published literature | Supplementary Methods (available online) | |
| Direct medical costs | Direct medical costs associated with cancer by the phase of care (initial, continuing, and end year of life) for individuals with cancer, and direct medical costs for the general population, by sex and age (younger than 65 and 65 years and older) |
SEER-Medicare Mariotto et al., 2011 (4) Hogan et al., 2001 (25) |
|
| Productivity loss costs | Productivity loss costs for individuals with cancer and the general population |
MEPS Zheng et al., 2016 (26) Guy et al., 2013 (27) |
|
| Patient time costs | Patient time costs for individuals with cancer and the general population |
MEPS Yabroff et al., 2014 (28) |
|
| Health-related quality of life (HRQOL) | HRQOL estimates for each cancer type based on published literature assessing HRQOL using EQ-5D |
Supplementary Methods (available online) Supplementary Table 7 (available online) |
|
SSBs were defined as any nonalcoholic, carbonated, or noncarbonated beverages with added caloric sweetener including sodas, energy drinks, sports drinks, and fruit drinks. (23) Dietary intake of SSBs was derived from 1 or 2 valid 24-hour dietary recalls using NHANES 2013-2016 data. The mean intake of 8 oz serving/day of SSB consumption was estimated for each of the 32 demographic subgroups and by income status. AICR = American Institute for Cancer Research; BMI = Body Mass Index; CI = Confidence Interval; MEPS = Medical Expenditures Panel Survey; NHANES = National Health and Nutrition Examination Survey; FPIR = Federal Poverty-to-Income Ratio; RR = Relative Risk; SEER = Surveillance, Epidemiology, and End Results Program; SSB = Sugar-sweetened Beverages; WCRF = World Cancer Research Fund.
Population Characteristics
We estimated the frequency distribution of 32 population subgroups by age (20-44, 45-54, 55-64, and 65 years and older), sex, and race and ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other) from the two most recent cycles (2013-2014 and 2015-2016) of the National Health and Nutrition Examination Survey (NHANES), a cross-sectional national survey representing the noninstitutionalized population of the United States. The population was further stratified by the federal poverty-to-income ratio (FPIR) into low-income (≤1.85) and higher-income (>1.85) groups. We also estimated the proportion of US adults with overweight or obese (body mass index [BMI] ≥ 25 kg/m2) in each subgroup and by income status. The NHANES survey weights were adjusted in all analyses (29).
Sugar-Sweetened Beverage Consumption
SSBs were defined as any nonalcoholic, carbonated, or noncarbonated beverages with added caloric sugar including sodas, fruit drinks, sweetened teas, sports drinks, and energy drinks (Supplementary Methods and Supplementary Table 1, available online) (30). We further defined caloric as at least 5 grams of added sugar per 12-ounce serving (Supplementary Table 2, available online). The mean consumption of SSBs was estimated based on dietary data collected from 1 or 2 valid 24-hour diet recalls among participants of NHANES 2013-2016. Energy-adjusted mean intake of SSB consumption was estimated for each subgroup and by income status (Supplementary Table 3, available online) (31).
Policy Effects
Reduction in SSB consumption post tax was estimated based on price elasticity estimates, which correspond to change in SSB consumption in response to an increase in SSB price (Supplementary Methods, available online) (22). Higher price elasticity was applied to low-income compared with higher-income individuals (22). Based on price elasticities and national average SSB price (32), we estimated a 10.8%, 16.8%, and 8.3% decrease in SSB intake for the total US adult population, low-income, and higher-income individuals, respectively, in response to penny-per-ounce SSB tax (Supplementary Table 4, available online). The policy was assumed to result in a one-time reduction in SSB consumption during the first year, and the policy effect was maintained in future years.
Cancer Statistics and Cancer-Related Quality of Life
We obtained incidence rates for 13 obesity-related cancers in 2015 from the Surveillance, Epidemiology, and End Results (SEER) and the Centers for Disease Control and Prevention’s National Program of Cancer Registries (Supplementary Methods, available online) (33). We projected future cancer incidence rates using the average annual percent change method for each cancer type over the next 15 years (from 2016 to 2030) and held the incidence rate constant for subsequent years (4, 34). The 5-year relative survival for each cancer type was obtained from SEER and converted to annual probabilities of dying assuming a constant hazard rate [35]. The health-related quality of life for each cancer type was extracted from published literature (Supplementary Methods and Supplementary Table 5, available online) (36–38).
Diet-BMI and BMI-Cancer Effect Sizes
The effects of changes in SSB intake on changes in BMI were estimated from a pooled analysis of 120 977 men and women in 3 prospective cohort studies in the United States, including separate estimates for individuals who were normal weight and overweight or obese at baseline (23,39). Relative risk estimates of BMI and cancer risk were based on meta-analysis and systematic reviews of cohort studies published by the World Cancer Research Fund/American Institute for Cancer Research and International Agency for Research on Cancer (Supplementary Table 6, available online) (2,24,40).
Policy Costs
The total implementation costs of SSB tax included the government cost for tax administration and the beverage industry compliance costs to comply with tax regulations (Supplementary Methods and Supplementary Table 7, available online). We estimated the overall cost of implementing the national SSB tax policy as 2% of the annual SSB tax revenue (41–43), with 1% each for the government administrative and industry compliance costs.
Health-Related Costs
We estimated the health-related costs in 2015 including the direct healthcare costs and indirect patient time and productivity loss costs, estimated separately for individuals with and without cancer (Supplementary Methods, available online). For individuals with cancer, the direct healthcare costs were obtained by age (younger than 65 years and 65 years and older), sex, and phase of cancer care (initial, continuing, and end year of life) from nationally representative claim data of Medical Expenditure Panel Survey data and Medicare linked to SEER (4). For individuals without cancer, the direct healthcare costs were estimated by age (younger than 65 years and 65 years and older) and sex from the national Medical Expenditure Panel Survey data (25). Health-related costs were projected from 2016 to 2025 with no further increase beyond 2025. All costs were adjusted to 2015 US dollars using the personal healthcare index.
Cost-Effectiveness Analysis
We used the DiCOM model to estimate the health gains including the number of new cancer cases prevented, cancer deaths averted, quality-adjusted life-years (QALYs) gained, total life years saved, and the cost-effectiveness using the incremental cost-effectiveness ratio (ICER). The ICER was calculated as the ratio of net costs to QALYs gained, all discounted at 3% annually. These net costs reflect cancer-related costs only and do not include health-related costs saved or spent on other diseases due to SSB tax. We evaluated the cost-effectiveness from both the government affordability and societal perspectives. The government affordability perspective included the government implementation costs and direct health-care costs of cancer care. The societal perspective added industry compliance costs and indirect productivity loss and patient time costs. Willingness-to-pay thresholds were defined as cost-effective when falling below $150 000 per QALY and highly cost-effective if less than $50 000 per QALY (44). We further compared the health gains, costs, and ICERs among age, sex, and race and ethnicity subgroups and by income status.
We performed one-way sensitivity analyses to address structural uncertainties in the model assumptions. We used empirical estimates synthesized from reported changes in SSB volume sold after SSB tax implemented in Philadelphia, Pennsylvania; Cook County, Illinois; and Seattle, Washington, as the policy effect (-11.4%) (Supplementary Methods, available online). To explore to what extent the estimates were driven by assuming cancer incidence continuing with the current trend, we performed a sensitivity analysis by assuming no time trends in cancer incidence and survival over the study period. We also performed analyses with a shorter time horizon and evaluated at which year the policy would reach the cost-effectiveness threshold (44). Besides, we conducted probabilistic sensitivity analyses that jointly accounted for the uncertainties around model inputs and assumptions. Following 1000 model simulations, the results reported 95% uncertainty intervals (UI). All analyses and model development were conducted in Stata, version 14 (College Station, TX) and R, version 3.3.1 (Vienna, Austria) (45,46).
Results
Population Characteristics and SSB Intake
The mean age of US adults was 47.7 (SE = 0.34) years, about two-thirds (65.3%) were non-Hispanic White, two-thirds (70.3%) were overweight or obese, and one-third (33.5%) were low income. The population mean intake of SSBs was 1.17 (SE = 0.05) 8-oz servings per day among all US adults, with higher intakes among low-income (1.32 [SE = 0.09] 8-oz servings per day) than higher-income (1.05 [SE = 0.04] 8-oz servings per day) individuals.
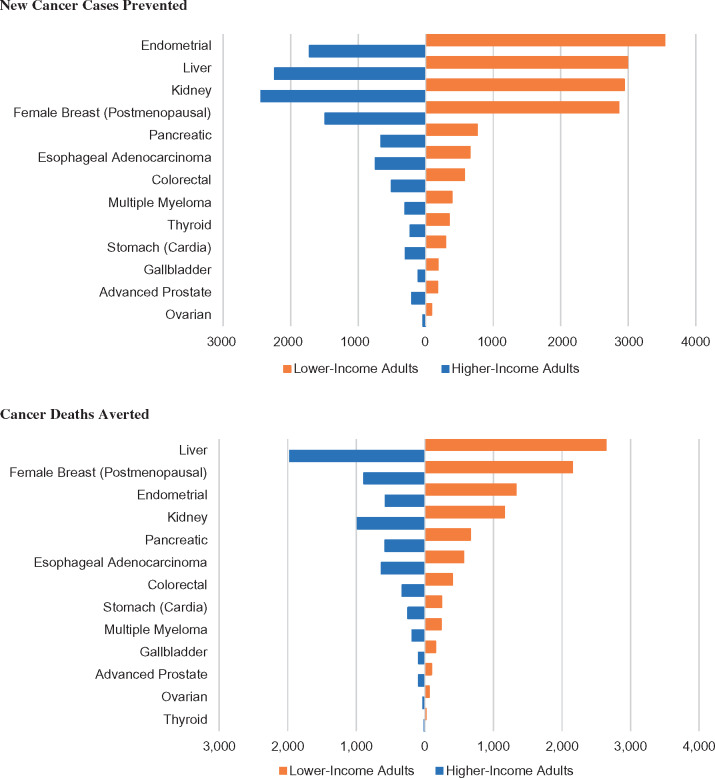
Health Gains
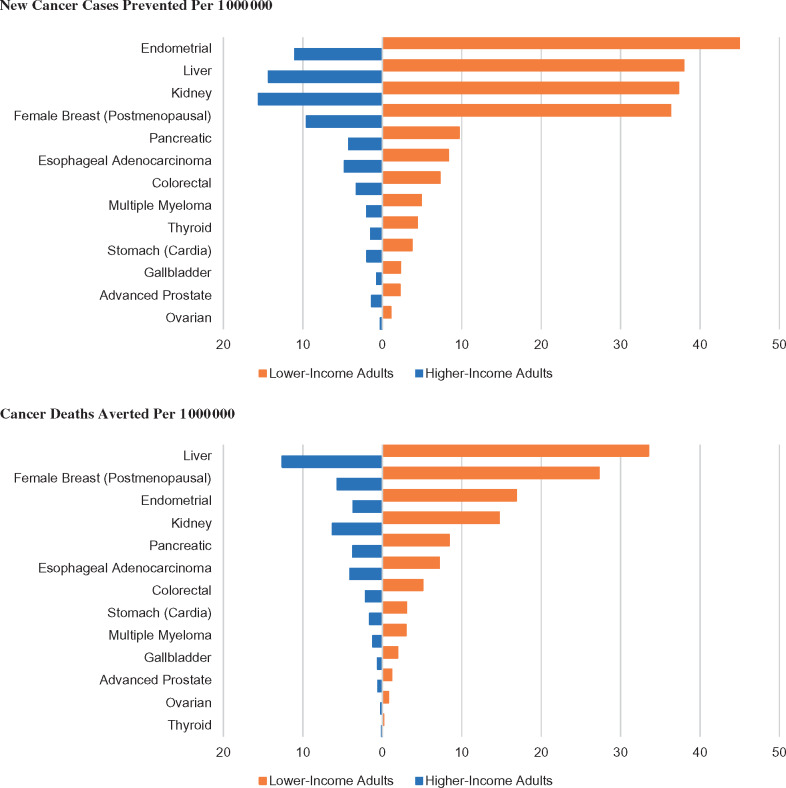
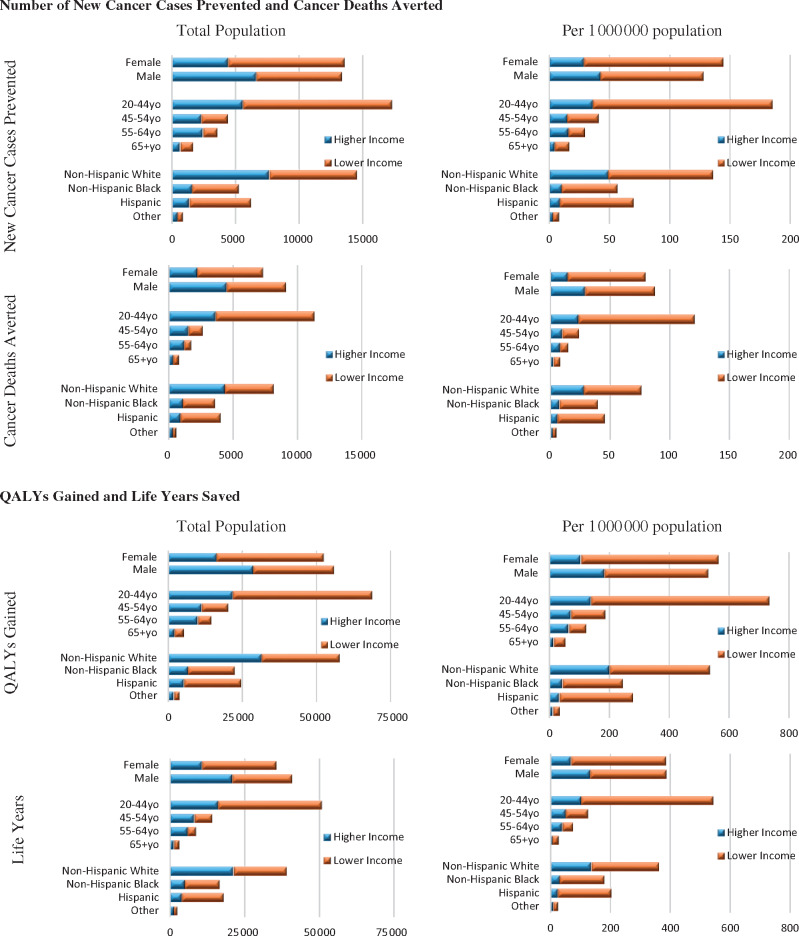
Over a lifetime, a national penny-per-ounce SSB tax would prevent 22 075 (95% UI = 16 040-28 577) new cancer cases, avert 13 524 (95% UI = 9841-17 681) cancer deaths, and gain 86 542 (95% UI = 62 220-113 147) QALYs (Table 2). Approximately 4800 more new cancer cases and 3100 more cancer deaths were averted among low-income adults (15 806, 95% UI = 12 888-19 020 new cancer cases; 9714, 95% UI = 7904-11 805 cancer deaths) than higher-income adults (10 965, 95% UI = 7577-14 884 new cancer cases; 6609, 95% UI = 4594-9018 cancer deaths) (Table 2 and Figure 1). Per 1 million population, greater health gains were observed among low-income (201, 95% UI = 164-241 new cancer cases; 123, 95% UI = 100-150 cancer deaths) compared with higher-income adults (70, 95% UI = 48-95 new cancer cases; 42, 95% UI = 29-58 cancer deaths), overall and across age, sex, and race and ethnicity subgroups (Figure 2). The QALYs gained and life-years saved were also consistently greater among low- than higher-income individuals (Table 2). Women and minorities were estimated to have the largest health gains among all population subgroups (Figure 3).
Table 2.
Estimated health gains, costs, and cost-effectiveness of a penny-per-ounce national sugar-sweetened beverage (SSB) tax on reducing cancer burden among US adults aged 20 years or older over a lifetimea
| Health gains and cost-effectiveness |
|
|
|
|---|---|---|---|
| Overall health outcomes | |||
| New cancer cases prevented | 22 075 (16 040 to 28 577) | 15 806 (12 888 to 19 020) | 10 965 (7577 to 14 884) |
| Cancer deaths averted | 13 524 (9841 to 17 681) | 9714 (7904 to 11 805) | 6609 (4594 to 9018) |
| Life-years saved | 60 407 (43 089 to 79 594) | 44 768 (36 171 to 54 390) | 31 186 (21 479 to 42 304) |
| QALYs gained | 86 542 (62 220 to 113 147) | 63 277 (51 833 to 76 727) | 44 980 (31 148 to 61 632) |
| Policy implementation costs, $ millionsb | |||
| Government administration costs | 1704 (1502 to 1948) | 670 (586 to 774) | 1000 (880 to 1133) |
| Industry compliance costs | 1695 (1476 to 1955) | 666 (576 to 772) | 994 (871 to 1135) |
| Cancer-related healthcare costs, $ millions | |||
| Direct medical costs | −1586 (-2069 to -1160) | −1092 (-1306 to -914) | −879 (-1209 to -615) |
| Productivity loss costs | −607 (-794 to -435) | −441 (-529 to -364) | −331 (-451 to -266) |
| Patient time costs | −98 (-129 to -69) | −71 (-84 to -58) | −54 (-75 to -36) |
| Net costs, $ millionsc | |||
| Government affordability perspective | 125 (-383 to 605) | −422 (-639 to -223) | 111 (-225 to 421) |
| Societal perspectivec | 1126 (388 to 1814) | −272 (-580 to 28) | 723 (236 to 1145) |
| ICER, $ | |||
| Government affordability perspectiveb | 1486 (-3516 to 9265) | Cost-saving | 2486 (-3733 to 13 458) |
| Societal perspectivec | 13 220 (3453 to 28 120) | Cost-saving | 16 203 (3902 to 36 085) |
Low-income was defined as the federal poverty-to-income ratio (FPIR) ≤ 1.85, and higher-income was defined as FPIR > 1.85. ICER = incremental cost-effectiveness ratio; QALYs = quality-adjusted life years; UI, uncertainty interval.
Policy implementation costs represent the net present value over a lifetime with a 3% discount rate. The tax policy was assumed to have a one-time effect on reducing SSB consumption that lasts for subsequent years with no further reduction.
The government affordability perspective reflects the difference between the government costs for implementing the policy and direct healthcare costs saved for cancer care. The societal perspective reflects the difference between the policy implementation costs (including both government administration costs and industry compliance costs) and the health-related costs saved (including direct healthcare costs, productivity loss costs, and patient time costs).
Figure 1.
Estimated number of new cancer cases and cancer deaths averted over a lifetime among US adults by a nationwide penny-per-ounce sugar-sweetened beverage tax among low-income and higher-income individuals. Low-income was defined as the federal poverty-to-income ratio (FPIR) ≤ 1.85 and higher-income as FPIR > 1.85.
Figure 2.
Estimated number of new cancer cases and cancer deaths averted over a lifetime among US adults per 1 000 000 by a penny-per-ounce national sugar-sweetened beverage tax among low-income and higher-income individuals. Low-income was defined as the federal poverty-to-income ratio (FPIR) ≤ 1.85 and higher-income as FPIR > 1.85.
Figure 3.
Estimated health gains per 1 000 000 US adults over a lifetime by a penny-per-ounce national sugar-sweetened beverage tax by age, sex, race and ethnicity, and income. Low-income was defined as the federal poverty-to-income ratio (FPIR) ≤ 1.85 and higher-income as FPIR > 1.85. QALY = quality-adjusted life-years.
Cost-Effectiveness
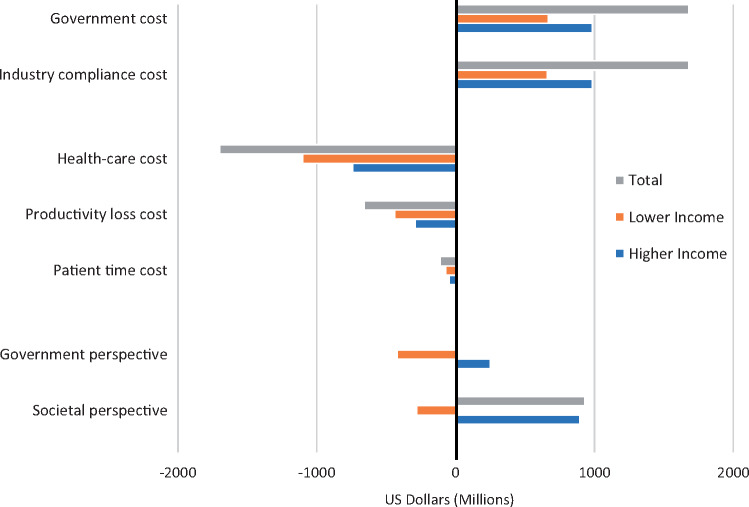
Implementation of a national penny-per-ounce SSB tax was estimated to cost the government $1.70 billion (95% UI = 1.50-1.95) in administrative costs and the beverage industry $1.70 billion (95% UI = 1.48-1.96) in compliance costs (Figure 4). At the same time, the policy was estimated to save $2.28 billion (95% UI = 1.67-2.98) in cancer-related healthcare costs from fewer new cancer cases and deaths. Cancer-related healthcare costs saved were $1.60 billion (95% UI = 1.33-1.92) among low-income adults, which was approximately $0.34 billion more than the healthcare costs saved ($1.26 billion, 95% UI = 0.88-1.74) among higher-income adults.
Figure 4.
Estimated costs and net costs of a penny-per-ounce national sugar-sweetened beverage tax on reducing cancer burden among US adults over a lifetime by income status. The net costs ($ million in 2015 US dollars) under the government affordability perspective were calculated as the difference between government costs for implementing the policy and direct medical costs for cancer care. The net savings under the societal perspective were calculated as the difference between policy implementation costs (including both government costs and industry compliance costs) and health-related cancer costs (including direct medical costs, productivity loss, and patient time costs). Low-income was defined as the federal poverty-to-income ratio (FPIR) ≤ 1.85 and higher-income as FPIR > 1.85.
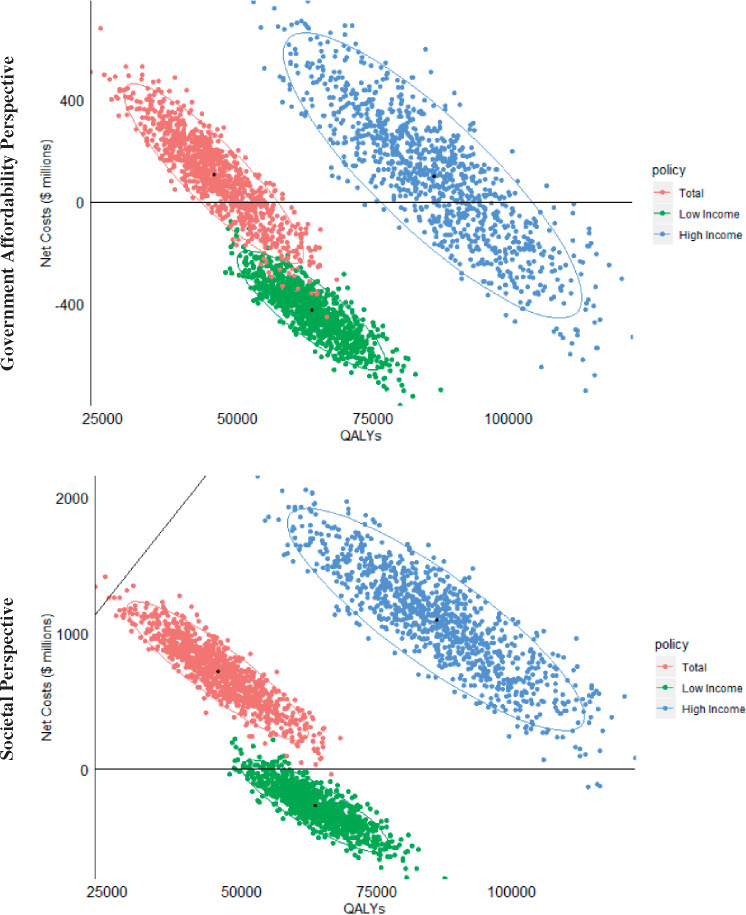
From a government affordability perspective, the SSB tax was estimated to be highly cost-effective (ICER = 1486 perQALY, 95% UI = -$3516-$9265 per QALY), not including the tax revenues generated (Table 2). From a societal perspective (omitting the tax revenues and adding industry compliance costs along with indirect costs saved because of fewer cancer cases and deaths), the SSB tax was also highly cost-effective (ICER = $13 220perQALY, 95% UI = $3453-$28 120perQALY) (Figure 5). Among low-income individuals, the SSB tax was cost-saving, with net savings of $422 million (95% UI = $223-$639) and $272 million (95% UI = -$28-$580) from the government affordability and societal perspectives, respectively. Among higher-income individuals, the policy was highly cost-effective from the government affordability (ICER = $2486perQALY, 95% UI = -$3733-$13 458perQALY) and societal perspectives (ICER = $16 203perQALY, 95% UI = $3902-$36 085 perQALY).
Figure 5.
Estimated incremental cost-effectiveness ratio (ICER) of a penny-per-ounce national sugar-sweetened beverage tax among US adults over a lifetime by income status. ICER was calculated as the ratio of net costs ($ million in 2015 US dollars) divided by quality-adjusted life-years (QALYs) gained. Blue dots correspond to the ICERs among the total US adult population, green dots among low-income adults, and red dots among higher-income adults. Low-income was defined as the federal poverty-to-income ratio (FPIR) ≤ 1.85 and higher-income as FPIR > 1.85.
Sensitivity Analyses
Using empirical evidence from implementing SSB taxes as the policy effect size, the number of new cancer cases and cancer deaths prevented among US adults over a lifetime would double, with $1.11 (95% UI = $0.55-$1.74) billion and $683 (95% UI = -$142-$1619) million net savings from the government affordability and societal perspectives, respectively (Supplementary Table 8, available online). Assuming no trends in cancer incidence and survival over time, the estimated health gains and economic impact of the SSB tax were smaller but remained highly cost-effective (Supplementary Table 9, available online). When a shorter time horizon was modeled, the policy was highly cost-effective at both 10 and 15 years from the government affordability perspective. From the societal perspective, the policy was not cost-effective over 10 years but achieved cost-effectiveness over 15 years (ICER = $136 837 perQALY, 95% UI = $84 127-$219 067 perQALY) (Supplementary Table 10, available online).
Discussion
Our nationally representative simulation model estimated that a national penny-per-ounce excise tax on SSB would prevent more than 22 000 new cancer cases and 13 500 cancer deaths and save $2.28 billion in healthcare costs for cancer care among US adults over a lifetime. Accounting for costs of policy implementation, the SSB tax is highly cost-effective from both government affordability and societal perspectives (not including $6.6 billion in tax revenues). Greater health gains and economic benefits were consistently seen among low-income compared with higher-income individuals.
Based on strong evidence linking body fatness and cancer risk (24), the latest World Cancer Research Fund/American Institute for Cancer Research Expert Report includes maintaining a healthy weight and avoiding weight gain in adulthood as one of the key recommendations for cancer prevention. Similarly, the American Society of Clinical Oncology considers obesity to be an underappreciated risk factor for cancer and advocates for effective strategies to help patients lose weight and make other healthy lifestyle changes (47). Yet, obesity-related cancer burdens have been increasing in the United States, particularly among younger adults (5). If the current trends continue, it is estimated that obesity will become the leading cause of preventable cancer-related death (5). However, the public remains generally unaware of the strong links between obesity and cancer (48). Cost-effective population-based strategies are needed to reduce obesity and related cancer burdens in the United States.
Leading US health organizations including the American Heart Association and American Academy of Pediatrics have endorsed the implementation of SSB taxes (49). Both feasibility and effectiveness in reducing SSB intakes are supported by the seven US cities and locales that have adopted volume-based SSB taxes (18,50); Berkeley, California, was the first city in the United States to levy a penny-per-ounce SSB tax in 2015 and has resulted in a 19.8% reduction in SSB consumption after 1 year of policy implementation (51). Two years later, Philadelphia, Pennsylvania, enacted a 1.5 cents-per-ounce tax that was associated with a 38% reduction in the volume of taxed beverages sold (52). The most recent publications on SSB taxes reported a 21% reduction in SSB sales after implementing a penny-per-ounce tax in Cook County, Illinois, and a 22% reduction in SSB sales after implementing a 1.75 cents-per-ounce tax in Seattle, Washington (53). We modeled a much more conservative policy effect size (10.8% reduction overall, including 16.8% among low-income adults and 8.3% among higher-income adults). When the empirical evidence from the SSB taxes currently implemented in the US cities and locales was used, the estimated health gains doubled, and the policy became cost-saving.
Our findings suggest that a national SSB tax would reduce cancer disparities in the United States, with larger benefits among low-income populations. These findings are consistent with the empirical experience following Mexico’s national SSB tax (54,55) and a modeling study in Australia (56). Additionally, we found that women would experience larger health benefits than men related to postmenopausal breast cancer and especially endometrial cancer. Overall, the estimated health gains and economic benefits for a national penny-per-ounce SSB tax were smaller than those estimated for cigarette taxes (57). The greater benefits of cigarette taxes could be due to a larger disease burden attributable to cigarette smoking (58). The cigarette is also taxed at a much higher rate (nearly half of the pretax price) (59) than the current SSB tax (about 20% of the pretax price) (60). Compared with other food tax policies such as 10% excise tax on processed meat (21), the impact of SSB tax was also smaller, which is likely due to a much larger relative risk estimate of high processed meat (24) vs high SSB consumption on cancer risk (23,39).
Nevertheless, a national penny-per-ounce SSB tax is still a highly cost-effective approach for cancer prevention. In response to the increasing attention around SSB taxes, the beverage industry has been focusing its efforts to prevent additional soda taxes from being implemented (17). Establishing and operating campaigns and lobbying against SSB taxes is a well-established strategy of the industry (61–63). A national SSB excise tax would eliminate the heterogeneity across states and locales and the threat of state preemption. If the estimated $6.6 billion annual tax revenues could be used for programs to increase access to affordable and healthy foods for low-income families or toward educational campaigning (64,65), greater health gains and economic benefits could be obtained at the national level. Additionally, a higher tax rate (eg, 2 cents-per-ozcents per oz) or tiered volume tax could also generate greater health gains and economic benefits than the penny-per-ounce tax.
Potential limitations should also be considered. First, although using the best available data, the actual magnitude of the policy effect depends on the validity of data inputs used. We conducted probabilistic sensitivity analyses to account for uncertainties around the model inputs and one-way sensitivity analyses to evaluate the extent to which structure uncertainties in the model assumptions affect the results. Second, we did not model health gains from reduced cardiovascular diseases, type 2 diabetes, or dental caries that are associated with high SSB consumption (19,20, 64,66–68) and potential health gains resulting from leveraging the SSB tax revenue for other public health actions. In addition, policy implementation may lead to increases in healthcare costs (and thus fewer savings) if the policy contributes to a longer lifespan as a result of lower cancer incidence. The overall policy impact remains unknown, and our findings only represent costs and health gains for obesity-associated cancers. Third, our analysis did not account for potential policy impacts on reducing SSB consumption in children and subsequent childhood obesity. This was largely because of the lack of well-established evidence on how the trajectory of childhood obesity lasts into adulthood and the lack of evidence on childhood obesity and cancer risk. Thus, the current policy effect could be underestimated. Fourth, we did not consider alternative SSB tax structures such as tiered volume taxes or sugar content taxes, which may incentivize manufacturers to reformulate products and partly reduce the sugar content (68). Fifth, we did not integrate changes in population demographics such as income, education, and race and ethnicity over time. However, the main results of cost-effectiveness will remain relatively stable regardless of demographic shifts, because the analysis is comparing the policy scenario to a status quo, which tends to cancel out the demographic changes because they equally occur in both scenarios.
Despite these limitations, our study provides the first-line estimates that incorporated nationally representative data on demographics, SSB consumption, and cancer incidence. We evaluated multiple phases of cancer including initial diagnosis and treatment, continuous care, and end year of life, incorporating health transitions and healthcare costs of 13 types of obesity-related cancer. Our model integrated conservative policy effect estimates and included etiologic effects of BMI on cancer risk from well-conducted systematic reviews and meta-analyses of prospective cohort studies. In addition to direct healthcare costs, we also incorporated the indirect costs of patient time and productivity loss to provide a societal perspective. We compared the health gains and economic impacts by age, sex, race and ethnicity, and income to assess whether the policy may reduce cancer disparities.
A national penny-per-ounce SSB tax is estimated to be cost-effective on reducing cancer burden and disparities in the United States, with the largest health gains and economic benefits among low-income Americans.
Funding
This work was supported by NIH/NIMHD 1R01MD011501 (FFZ).
Notes
Role of the funder: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Disclosures:RM reports research funding from National Institutes of Health (NIH), Bill & Melinda Gates Foundation, and Unilever and personal fees from the World Bank and Bunge. DM reports research funding from the National Institutes of Health and the Gates Foundation; personal fees from the Global Organization for EPA and DHA Omega-3s (GOED), Nutrition Impact, Pollock Communications, Bunge, Indigo Agriculture, Amarin, Acasti Pharma, Cleveland Clinic Foundation, America’s Test Kitchen, and Danone; scientific advisory board, Elysium Health (with stock options), Omada Health, and DayTwo; and chapter royalties from UpToDate, all outside the submitted work. The other authors have no conflicts of interest to declare.
Author contributions: MD contributed to the data curation, formal analysis, visualization, manuscript writing, review and editing; CFG contributed to the data curation, formal analysis, visualization, and original draft preparation; DDK, FC, and HE contributed to the model development; MR and YL contributed to data curation; DDK, JBW, PEW, DSM, RM, and DM contributed to the review and editing; FFZ contributed the conceptualization, methodology, review and editing, supervision, and funding acquisition.
Data availability statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Supplementary Material
References
- 1. Siegel RL, Miller KD, Jemal A.. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
- 2. Lauby-Secretan B, Scoccianti C, Loomis D, et al. Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steele CB, Thomas CC, Henley SJ, et al. Vital signs: trends in incidence of cancers associated with overweight and obesity—United States, 2005-2014. Mmwr Morb Mortal Wkly Rep. 2017;66(39):1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mariotto AB, Robin Yabroff K, Shao Y, Feuer EJ, Brown ML.. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sung H, Siegel RL, Rosenberg PS, Jemal A.. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health. 2019;4(3):e137–e147. [DOI] [PubMed] [Google Scholar]
- 6. Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar‐sweetened beverage consumption will reduce the prevalence of obesity and obesity‐related diseases. Obes Rev. 2013;14(8):606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Malik VS, Pan A, Willett WC, Hu FB.. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98(4):1084–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bleich SN, Vercammen KA, Koma JW, Li Z.. Trends in beverage consumption among children and adults, 2003‐2014. Obesity. 2018;26(2):432–441. [DOI] [PubMed] [Google Scholar]
- 9. Kit BK, Fakhouri TH, Park S, Nielsen SJ, Ogden CL.. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010. Am J Clin Nutr. 2013;98(1):180–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Welsh JA, Sharma AJ, Grellinger L, Vos MB.. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr. 2011;94(3):726–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bailey R, Fulgoni V, Cowan A, Gaine P.. Sources of added sugars in young children, adolescents, and adults with low and high intakes of added sugars. Nutrients. 2018;10(1):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huth PJ, Fulgoni VL, Keast DR, Park K, Auestad N.. Major food sources of calories, added sugars, and saturated fat and their contribution to essential nutrient intakes in the US diet: data from the national health and nutrition examination survey (2003-2006). Nutr J. 2013;12(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Han E, Powell LM.. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet. 2013;113(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rosinger A, Herrick K, Gahche J, Park S, Frenk SM, Percentage of Total Daily Kilocalories Consumed from Sugar-Sweetened Beverages Among Children and Adults, by Sex and Income Lever-National Health and Nutrition Examination Survey, United States, 2011-2014. Atlanta, GA: Centers for Disease Control and Prevention; Atlanta, GA; 2017.
- 15. Backholer K, Vandevijvere S, Blake M, Tseng M.. Sugar-sweetened beverage taxes in 2018: a year of reflections and consolidation. Public Health Nutr. 2018;21(18):3291–3295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Backholer K, Blake M, Vandevijvere S.. Sugar-sweetened beverage taxation: an update on the year that was 2017. Public Health Nutr. 2017;20(18):3219–3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Du M, Tugendhaft A, Erzse A, Hofman KJ.. Focus: nutrition and food science: sugar-sweetened beverage taxes: industry response and tactics. Yale J Biol Med. 2018;91(2):185. [PMC free article] [PubMed] [Google Scholar]
- 18. Pomeranz JL, Wilde P, Huang Y, Micha R, Mozaffarian D.. Legal and administrative feasibility of a federal junk food and sugar-sweetened beverage tax to improve diet. Am J Public Health. 2018;108(2):203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wilde P, Huang Y, Sy S, et al. Cost-effectiveness of a US national sugar-sweetened beverage tax with a multistakeholder approach: who pays and who benefits. Am J Public Health. 2019;109(2):276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Long MW, Gortmaker SL, Ward ZJ, et al. Cost effectiveness of a sugar-sweetened beverage excise tax in the US. Am J Prev Med. 2015;49(1):112–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kim DD, Wilde PE, Michaud DS, et al. Cost effectiveness of nutrition policies on processed meat: implications for cancer burden in the U.S. Am J Prev Med. 2019;57(5):e143–e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wada R, Han E, Powell LM. Associations between soda prices and intake: Evidence from 24-h dietary recall data. Food Policy. 2015;55(1):54–60. [Google Scholar]
- 23. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB.. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25): 2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report 2018 Body fatness and weight gain and the risk of cancer World Cancer Research Fund/American Institute for Cancer Research; 2018.
- 25. Hogan C, Lunney J, Gabel J, Lynn J.. Medicare beneficiaries’ costs of care in the last year of life. Health Aff. 2001;20(4):188–195. [DOI] [PubMed] [Google Scholar]
- 26. Zheng Z, Yabroff KR, Guy GP, et al. Annual medical expenditure and productivity loss among colorectal, female breast, and prostate cancer survivors in the United States. J Natl Cancer Inst. 2016;108(5):djv382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guy GP Jr, Ekwueme DU, Yabroff KR, et al. Economic burden of cancer survivorship among adults in the United States. J Clin Oncol. 2013;31(30):3749–3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yabroff KR, Guy GP Jr, Ekwueme DU, et al. Annual patient time costs associated with medical care among cancer survivors in the United States. Med Care. 2014;52(7):594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention; National Center for Health Statistics. National Health and Nutrition Examination Survey: Analytic Guidelines, 2011-2016. 2018. [cited July 26, 2019].
- 30. Centers for Disease Control and Prevention. The CDC Guide to Strategies for Reducing the Consumption of Sugar-Sweetened Beverages Atlanta, GA: Centers for Disease Control and Prevention; 2010.
- 31. Tooze JA, Kipnis V, Buckman DW, et al. A mixed‐effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29(27):2857–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Powell L, Isgor Z, Rimkus L, Chaloupka F, Sugar-Sweetened Beverage Prices: Estimates from a National Sample of Food Outlets Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago; 2014.
- 33. Centers for Disease Control and Prevention. United States Cancer Statistics (USCS). Public Use Databases. https://www.cdc.gov/cancer/uscs/public-use/. Accessed November 9, 2018.
- 34. Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK.. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28(29):3670–3682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: November 2018 Submission, National Cancer Institute, DCCPS, Surveillance Research Program. https://seer.cancer.gov/data-software/documentation/seerstat/nov2018/. Accessed September 16, 2020. [Google Scholar]
- 36. Longworth L, Yang Y, Young T, et al. Use of generic and condition-specific measures of health-related quality of life in NICE decision-making: a systematic review, statistical modelling and survey. Health Technol Assess. 2014;18(9):1–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Naik H, Howell D, Su S, et al. EQ-5D health utility scores: data from a comprehensive Canadian Cancer Centre. Patient. 2017;10(1):105–115. [DOI] [PubMed] [Google Scholar]
- 38. Pickard AS, Jiang R, Lin HW, Rosenbloom S, Cella D.. Using patient-reported outcomes to compare relative burden of cancer: EQ-5D and functional assessment of cancer therapy-general in eleven types of cancer. Clin Ther. 2016;38(4):769–777. [DOI] [PubMed] [Google Scholar]
- 39. Micha R, Shulkin ML, Penalvo JL, et al. Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One. 2017;12(4):e0175149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang FF, Cudhea F, Shan Z, et al. Preventable cancer burden associated with poor diet in the United States. JNCI Cancer Spectrum. 2019;3(2):pkz034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Framework A. Table 5.3 Cost of collection ratios (administrative costs/net revenue), in Tax Administration 2013: Comparative Information on OECD and Other Advanced and Emerging Economies Paris: OECD Publishing; 2013.
- 42. World Health Organization. Scaling up Action Against NCDs: How Much Will It Cost? WHO report 2011. Switzerland: WHO Press; 2011.
- 43. Aaron H, Gale W.. Economic Effects of Fundamental Tax Reform. Washington, D.C.: Brookings Institution Press; 2010. [Google Scholar]
- 44. Anderson JL, Heidenreich PA, Barnett PG, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(21):2304–2322. [DOI] [PubMed] [Google Scholar]
- 45. Schwingshackl L, Hoffmann G, Schwedhelm C, et al. Consumption of dairy products in relation to changes in anthropometric variables in adult populations: a systematic review and meta-analysis of cohort studies. PLoS One. 2016;11(6):e0157461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schnabel RB, Maas R, Wang N, et al. Asymmetric dimethylarginine, related arginine derivatives, and incident atrial fibrillation. Am Heart J. 2016;176(1):100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ligibel JA, Alfano CM, Courneya KS, et al. American Society of Clinical Oncology position statement on obesity and cancer. J Clin Oncol. 2014;32(31):3568–3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Merom D, Gebel K, Fahey P, et al. Neighborhood walkability, fear and risk of falling and response to walking promotion: the Easy Steps to Health 12-month randomized controlled trial. Prev Med Rep. 2015;2(1):704–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Muth ND, Dietz WH, Magge SN, et al. Public policies to reduce sugary drink consumption in children and adolescents. Pediatrics. 2019;143(4):e20190282. [DOI] [PubMed] [Google Scholar]
- 50. Cawley J, Thow AM, Wen K, Frisvold D.. The economics of taxes on sugar-sweetened beverages: a review of the effects on prices, sales, cross-border shopping, and consumption. Annu Rev Nutr. 2019;39(1):317–338. [DOI] [PubMed] [Google Scholar]
- 51. Silver LD, Ng SW, Ryan-Ibarra S, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: a before-and-after study. PLoS Med. 2017;14(4):e1002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Roberto CA, Lawman HG, LeVasseur MT, et al. Association of a beverage tax on sugar-sweetened and artificially sweetened beverages with changes in beverage prices and sales at chain retailers in a large urban setting. JAMA. 2019;321(18):1799–1810. [DOI] [PubMed] [Google Scholar]
- 53. Powell LM, Leider J.. The impact of Seattle’s sweetened beverage tax on beverage prices and volume sold. Econ Hum Biol. 2020;37(1):100856. [DOI] [PubMed] [Google Scholar]
- 54. Colchero MA, Molina M, Guerrero-López CM.. After Mexico implemented a tax, purchases of sugar-sweetened beverages decreased and water increased: difference by place of residence, household composition, and income level. J Nutr. 2017;147(8):1552–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Colchero MA, Popkin BM, Rivera JA, Ng SW.. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ. 2016;352:H6704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lal A, Mantilla-Herrera AM, Veerman L, et al. Modelled health benefits of a sugar-sweetened beverage tax across different socioeconomic groups in Australia: a cost-effectiveness and equity analysis. PLoS Med. 2017;14(6):e1002326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ahmad S, Franz GA.. Raising taxes to reduce smoking prevalence in the US: a simulation of the anticipated health and economic impacts. Public Health. 2008;122(1):3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; 2014. https://www.cdc.gov/tobacco/basic_information/health_effects/index.htm. Accessed April 23, 2020.
- 59. Boonn A, Campaign for Tobacco-Free Kids: State Excise and Sales Taxes per Pack of Cigarettes Total Amounts and State Rankings 2020. https://www.tobaccofreekids.org/assets/factsheets/0097.pdf. Accessed April 23, 2020.
- 60. Powell LI, Rimkus L, Chaloupka FJ, Sugar-Sweetened Beverage Prices: Estimates from a National Sample of Food Outlets. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago; 2014.
- 61. Ronayne K. Capital rivals: the cola wars in Washington. OpenSecrets.org. 2011. https://www.opensecrets.org/news/2011/09/the-cola-wars-in-washington/. Accessed April 23, 2020.
- 62. Taylor BE, McClave SA, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med. 2016;44(2):390–438. [DOI] [PubMed] [Google Scholar]
- 63. Bistrian BR. Comment on “Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient.” JPEN J Parenter Enteral Nutr. 2010;34(3):348–349. Author reply 350–352. [DOI] [PubMed] [Google Scholar]
- 64. Mozaffarian D, Liu J, Sy S, et al. Cost-effectiveness of financial incentives and disincentives for improving food purchases and health through the US Supplemental Nutrition Assistance Program (SNAP): a microsimulation study. PLoS Med. 2018;15(10):e1002661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Peñalvo JL, Cudhea F, Micha R, et al. The potential impact of food taxes and subsidies on cardiovascular disease and diabetes burden and disparities in the United States. BMC Med. 2017;15(1):208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wang YC, Coxson P, Shen Y-M, Goldman L, Bibbins-Domingo K.. A penny-per-ounce tax on sugar-sweetened beverages would cut health and cost burdens of diabetes. Health Aff. 2012;31(1):199–207. [DOI] [PubMed] [Google Scholar]
- 67. Veerman JL, Sacks G, Antonopoulos N, Martin J.. The impact of a tax on sugar-sweetened beverages on health and health care costs: a modelling study. PLoS One. 2016;11(4):e0151460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lee Y, Mozaffarian D, Sy S, et al. Health Impact and Cost-Effectiveness of Volume, Tiered, and Absolute Sugar Content Sugar-Sweetened Beverage Tax Policies in the United States: A Microsimulation Study. Circulation. 2020;142(6):523-534. doi:10.1161/CIRCULATIONAHA.119.042956 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.