Abstract
COVID-19 causes severe respiratory and multiorgan failure, including liver damage and elevated transaminase levels. This article addresses the potential causes of liver function abnormalities in patients diagnosed with COVID-19 and management approaches for NPs focusing on preventing and alleviating liver injury.
Keywords: chronic liver disease, coronavirus, COVID-19, cytokine storm, elevated aminotransferase levels, liver enzymes, SARS-CoV-2
COVID-19 causes severe respiratory and multiorgan failure, including liver damage and elevated transaminase levels. This article addresses the potential causes of liver function abnormalities in patients diagnosed with COVID-19 and management approaches for NPs focusing on preventing and alleviating liver injury.
Figure.
No caption available.
The novel coronavirus disease 2019 (COVID-19) is an infection caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which originated in Wuhan, China, and has now become a global pandemic.1 As of November 20, 2020, over 57 million people worldwide have been infected by this virus with 1.3 million deaths.2 In the US, over 12 million people have been infected with the virus, and over 255,000 people have died as of November 23, 2020.3 Individuals infected with COVID-19 present with a myriad of symptoms that are variable between patients, such as a cough, shortness of breath, fever, chills, myalgia, sore throat, loss of taste, and anosmia. Gastrointestinal symptomatology may also be present in the form of nausea, vomiting, and diarrhea.4 Viral shedding can also occur in those who are asymptomatic, and these individuals may unknowingly spread the disease to others.5,6 COVID-19, in its most severe form, has a mortality of 3% due to massive alveolar damage and progressive respiratory failure; yet patients with milder symptoms may show quick resolution.1 The long-term consequences of COVID-19 infections are unknown.
Normal ranges of select liver tests
| Values | Normal ranges |
|---|---|
| ALT | 29-33 U/L |
| AST | 10-40 U/L |
| ALP | 45-115 U/L |
| GGT | 8-61 U/L |
| TBIL | 0.0-1.0 mg/dL |
Abbreviations: ALP, alkaline phosphatase; GGT, gamma-glutamyl transferase; TBIL, total bilirubin
Note: normal reference ranges may vary between different laboratories.
While the lungs are the primary target, this disease involves multiple other organs, including the cardiovascular system, kidneys, and liver.7 Up to 11% of patients with COVID-19 have liver comorbidities and 14% to 53% show elevated transaminase levels (alanine aminotransferase [ALT] and aspartate aminotransferase [AST]) during the progression of the illness (see Normal ranges of select liver tests).1 Accumulating evidence suggests that there is a strong correlation between the severity of the viral infection and the degree of liver enzyme elevation.1 Those with a mild case of the virus may have no abnormality or only slightly elevated aminotransferase levels, while those with more severe cases can present with higher elevations.8 Transient liver damage is also seen in mild cases of COVID-19, though the liver can return to normal with minimal treatment effort.1
For the 4.5 million people in the US who have been diagnosed with one of the many forms of liver disease, COVID-19 infection can be particularly serious.9,10 Patients with chronic liver disease are at risk for particularly critical outcomes if they contract COVID-19.11,12 Transplant recipients and those with hepatocellular carcinoma are especially at risk for developing severe illness. Many of these patients are immunocompromised either by the chronicity of the illness or by the treatment regimen for the condition.1,13 For these patients, the viral impact is overwhelming and can result in death.
While the cause of liver injury related to SARS-CoV-2 infection is unclear, some potential causes have been hypothesized. Here, we describe the hepatic effects of COVID-19. This information will help NPs understand possible factors that cause elevations in liver enzymes seen in those with COVID-19 and describe implications for practice. The goal should be swift intervention, which will limit liver injury.
Potential causes of liver involvement in COVID-19
Angiotensin-converting enzyme 2 (ACE2)
Angiotensin-converting enzyme 2 (ACE2) receptors are found in organs throughout the body, including the heart, kidney, liver, and central nervous system.14,15 The SARS-CoV-2 spike protein, which protrudes from the virus, binds to ACE2, which serves as a “door” to provide access to the interior of human cells. Once the virus enters the cell, it hijacks cellular machinery to replicate, kills the host cell, and spreads.1,15
ACE2 is found in abundance on the surface of lung cells, making the lungs a primary target for SARS-CoV-2.1,15 However, epithelial cells of the bile duct and liver also express ACE2, providing an easy access point for SARS-CoV-2 to bind directly to ACE2-positive cholangiocytes and disrupt liver function.1 Elevation of AST and ALT levels have been noted in patients with COVID-19, indicating some degree of liver impairment caused by the virus.16
Hepatotoxic drugs
Many medications have been used in an attempt to treat COVID-19 or its symptoms, such as antipyretics, antibiotics, antivirals, and steroids. Some of these medications have shown promise, while others have been less successful. Drug-induced liver injury has been noted as the cause of some of the liver abnormalities seen with COVID-19.17 Histology reveals moderate microvascular steatosis and mild hepatic inflammation that may reflect drug-induced damage to the liver from treatment of the virus or its symptoms.17 Despite the longstanding history of acetaminophen as the most common cause of acute liver failure and toxicity, it has been the drug of choice for treating fever and myalgia associated with COVID-19.18,19 However, it has been suspected that acetaminophen is a culprit in drug-induced liver injury in patients with COVID-19.17 Nonsteroidal anti-inflammatory drugs (NSAIDs), another drug often used for fevers and myalgia, have not been used as much as acetaminophen in symptomatic treatment of COVID-19, as they were initially thought to exacerbate the virus.20
Other medications intended to treat COVID-19 are known to cause hepatotoxicity even in the absence of overdose.18 Several antiviral medications have been initiated in the treatment of SARS-CoV-2 infection (for example, oseltamivir, abidol, lopinavir/ritonavir, and hydroxychloroquine), and all may show some degree of hepatotoxicity.18 On May 1, 2020, the FDA authorized emergency use of remdesivir for the treatment of patients hospitalized with severe COVID-19, and on October 22, 2020, the FDA approved remdesivir to treat COVID-19 in patients age 12 and older weighing at least 40 kg and requiring hospitalization.21,22 This antiviral, which was once used to treat Ebola and hepatitis C (without success), has been shown to reduce the time to recovery in cases of COVID-19 in hospitalized patients who had evidence of lower respiratory tract infection.23 Despite its success in reducing recovery times, it has not proven to be curative.24 Like other antiviral medications, it too can cause elevations in liver enzymes as an adverse reaction.21,22
Systemic inflammatory response
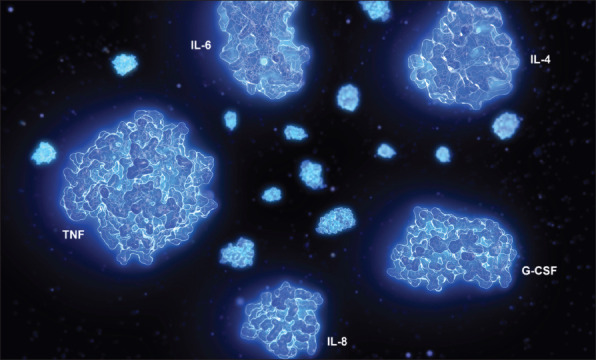
A systemic inflammatory response is thought to be another potential cause for liver injury in those infected with SARS-CoV-2. In this situation, acute lung injury and acute respiratory distress syndrome (ARDS) are caused by an uncontrolled overproduction of inflammatory cytokines, which triggers a “cytokine storm.”25 Cytokine storms are most often seen in the critically ill, but this crisis is often underdiagnosed and therefore undertreated.26 The release of multiple cytokines results in the development of flulike symptoms, such as fever and cough, as is seen in COVID-19.25 While the immune system works to suppress and eradicate the virus, immunopathologic damage occurs to the tissues and organs.25 The more inflammatory cytokines are released, the greater the magnitude of tissue and organ injury and death.25 Therefore, a cytokine storm is seen as a progression of the illness that can potentially injure the lungs, gut, and liver (as evidenced by elevation of liver enzymes) and lead to death.17,27
Hypoxic liver injury
While those infected with SARS-CoV-2 can be asymptomatic, symptomatic patients often present with a cough, flulike symptoms, fever, and may report dyspnea that can progress to ARDS.6 Hypoxia is one of the defining features of ARDS. “Silent hypoxia” can also occur in which oxygen saturation levels are as low as 50% with effortless breathing.28 But in many cases when hypoxia is evident, mechanical ventilation is required.29 On a computed tomography scan, unilateral or bilateral peripheral ground-glass opacities and consolidation are often seen in the lungs.6
Typically, the liver is protected from ischemic injury, as it has dual methods of oxygenation provided by redundant blood flow from the portal vein and hepatic artery.30 The portal vein contributes to 75% to 85% of the liver's blood supply, while the hepatic artery contributes to 20% to 25%.30 During systemic stress, hepatic blood flow decreases and is insufficient to supply the demands of the liver. The liver is unable to adequately increase oxygen extraction, which leads to hepatocellular hypoxia. With pneumonia-associated hypoxia in COVID-19, a secondary hypoxic liver injury occurs due to ARDS, a hyperinflammatory response, and multiple organ failure.31,32
Hypoxic liver injury in critical illnesses, such as severe forms of COVID-19, causes marked elevations in aminotransferase levels, metabolic acidosis, calcium overloading, and changes of mitochondrial membrane permeability.27,30
Implications for practice
Currently, there is no cure for COVID-19. To date, no vaccine has been approved that can prevent or reduce viral transmission, though several may be close to authorization at the time of this publication. Therefore, prevention of viral entry into the body is the key to reduce transmission and avoid infection.33 Educating patients on the benefits of prevention is paramount. Social distancing, washing hands with water and soap for at least 20 seconds, wearing masks, staying home as much as possible, cleaning and disinfecting surfaces at home, and avoiding contact with those infected are all preventive strategies that should be practiced by everyone.
Care will mostly be managed in the ambulatory care setting for those exhibiting mild symptoms and in the acute care setting for those with more severe symptoms. NPs in both settings must be vigilant in managing the illness. Careful attention should be paid to several hepatic effects. Elevated liver enzymes could indicate an acute liver injury associated with COVID-19, but NPs should recognize that other etiologies could be the culprit, such as hepatitis B or C.34 Therefore, not only should testing be conducted related to determining the effects of COVID-19, but other etiologies, such as viral and autoimmune causes, should be ruled out.
Attention should also be given to the progression in the elevation of transaminase levels, as this can be an indicator of disease progression.8,35 One study found nearly half of patients with COVID-19 had abnormalities of certain liver tests, such as ALT, AST, total bilirubin, and gamma-glutamyl transferase, on admission to the hospital. Liver test abnormalities tended to be mild, at 1 to 2 times the upper limit of normal (ULN), on admission, but the prevalence of more severe abnormalities, in some cases greater than 3 times ULN, increased during hospitalization. Patients with liver test abnormalities were found to be more likely to develop severe COVID-19.35 Transaminase levels should also be used to determine therapeutic dosages of medications given to the patient to manage the disease. Frequent and careful monitoring of liver function testing can provide early insight into the possibility of liver injury.7 Other factors should also be considered, as described below.
Medication management
A myriad of therapies are being evaluated for COVID-19. Drugs such as chloroquine and hydroxychloroquine and interferon therapies have been used to manage the inflammatory process of COVID-19.25,36,37 However, these are no longer being used as their adverse reactions outweighed the benefits or they were found to be ineffective.38,39 Another therapeutic modality being evaluated is convalescent plasma, which contains neutralizing antibodies and for which there is currently an emergency use authorization for hospitalized patients with COVID-19.25,40
Currently, antivirals like remdesivir are recommended for certain hospitalized patients.29,41 Remdesivir has been found to shorten the time to recovery in adults hospitalized with COVID-19 who had lower respiratory tract infection.23 Still, the use of this drug is not considered curative.42 Elevations in transaminase levels have been observed with remdesivir in clinical trials. Rarely elevations up to 10 times the baseline values have been seen.34 Remdesivir should not be started in patients whose ALT levels are five times or more the ULN at baseline and should be discontinued in those who develop an ALT five times or more the ULN during therapy.34 It should also be discontinued in patients who have an elevation of ALT with signs or symptoms of liver inflammation, or with increasing bilirubin, alkaline phosphatase, or international normalized ratio.34 Therapy can be restarted once the ALT level is less than five times ULN.34
Flulike symptoms can also be managed. Acetaminophen should be given as needed up to a maximum dose of 2 to 3 g/day, as it is considered the preferred analgesic and antipyretic. Once thought to exacerbate the condition, NSAIDs are now also considered acceptable as part of the management of fever and discomfort related to the infection and can be used as indicated.34
Managing inflammatory reaction and cytokine storm
To manage the inflammatory response and potential cytokine storm, NPs must have a keen eye in evaluating the patient's labs, as they can provide early indication of a cytokine storm. Although often missed, the prompt detection and management of this syndrome increases chance of survival.43 Level of ferritin, which is an inflammatory marker, can be used as an initial screening tool to assess for the presence of the cytokine storm related to COVID-19.41 The ferritin level is usually less than 200 ng/mL, but in cytokine storms related to COVID-19, it may be 500 or higher.44 Other biomarkers that may be indicative of inflammation, such as C-reactive protein, erythrocyte sedimentation rate, d-dimer, and tumor necrosis factor-alpha, are usually also elevated.12,43 A complete blood cell count should be assessed for the presence of lymphocytopenia and leukopenia.17 Elevations can be seen in interferon-gamma as well as lactate dehydrogenase in the cytokine storm.43 Liver enzymes can also become elevated. Labs should be carefully monitored for the development of cytokine storm as a marker of progression of the disease.
A two-dimensional approach should be used to address a cytokine storm: prevention as well as treatment of the underlying cause. Prevention of the cytokine storm is crucial and it is hypothesized that prevention may be achieved by use of alpha-blockers upon appearance of first symptoms. Non-peer-reviewed retrospective analyses found an association between treatment with alpha-blockers (for other indications) and decreased mortality in hospitalized patients with acute respiratory distress and pneumonia.45 In addition to supportive therapy with supplemental oxygen, fluid management, and antimicrobials as indicated for the management of COVID-19 pneumonia, various therapies, as previously addressed, have been used in an attempt to treat the cytokine storm.25 The underlying cause of this inflammatory cycle is the SARS-CoV-2 infection; therefore, finding an effective COVID-19 treatment could subdue or halt the cytokine storm.41
Dexamethasone has now been seen as a treatment champion in calming the cytokine storm by acting on the immune system to prevent massive inflammation seen in severely ill patients.46 Initially, steroids were not thought to be useful in treating COVID-19, as they could impair the immune system's ability to attack the virus. However, dexamethasone is now seen as being most effective in those requiring oxygen or mechanical ventilation, and hence, the first medication considered to reduce likelihood of death in severely ill patients.47 Hospitalized patients not requiring oxygen or ventilator support see no benefits with dexamethasone.47
Managing hypoxic liver injury
Hypoxic liver injury can occur when there is hypoperfusion of the liver due to respiratory failure or hypoxemia, such as in COVID-19.48 Again, NPs must be vigilant in ordering the correct lab tests to detect this phenomenon. Aminotransferase levels are elevated to 25 to 50 times ULN.48 Lactate dehydrogenase levels rise massively and early in this process.48 Management includes treating the underlying cause, thus restoring hemodynamic function.48
Patient education
Patient education is vital in yielding good outcomes for any patient who is afflicted with an illness. With COVID-19 being an ill-defined illness, patient education takes on new urgency. Diagnosis of COVID-19 can create feelings of doom and despair for many. Therefore, NPs in both the ambulatory and acute care settings have an enormous responsibility in ensuring that patients and their family members are knowledgeable about the disease process and the course of action that will be taken to manage the disease.
In the outpatient care arena, NPs should assess patients for suitability to remain at home, and if found suitable, they should be educated on mitigating the spread of the virus and the importance of monitoring for emergency warning signs and symptoms. These may include dyspnea, chest pain, confusion, changes in level of consciousness, and cyanosis, and indicate disease progression and a need for hospitalization.49 Also, patients should be advised to notify the provider if there is abdominal pain, jaundice, progression of nausea and vomiting, and changes in the color of their urine or stool as this could indicate hepatobiliary injury.
Hospitalized patients and their family members should be educated on their status, plan of care (such as diagnostic tests and medication management), and potential adverse reactions to medications. Patients and their family members should also be provided with daily updates of “next steps” in the management of illness until discharge.
Conclusion
Various ways in which the virus affects the liver have been discussed, and the influence of ACE2, hepatotoxicity, systemic inflammatory response, and hypoxic liver injury are impactful in explaining this phenomenon. While there is currently no cure for COVID-19 and no vaccines have yet been approved, medications are emerging that have the potential to be helpful in managing symptoms, controlling the inflammatory response, and reducing time in the inpatient setting. More studies are needed to understand the impact of ACE2, hepatotoxicity, systemic inflammatory response, and hypoxic liver injury, and to find a proper treatment for preventing organ injury and failure associated with SARS-CoV-2. Further studies should aim to define how preexisting chronic liver diseases impact the clinical course and prognosis for those with COVID-19.
REFERENCES
- 1.Zhang C, Shi L, Wang F-S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update sr. 2020. www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 3.Centers for Disease Control and Prevention. Cases and deaths in the U.S. 2020. www.cdc.gov/coronavirus/2019-ncov/cases-updates/us-cases-deaths.html.
- 4.Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) symptoms of coronavirus. 2020. www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
- 5.Auwaerter P. Coronavirus COVID-19 (SARS-CoV-2). 2020. www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540747/all/Coronavirus_COVID_19__SARS_CoV_2_. [Google Scholar]
- 6.Cennimo D. Coronavirus disease 2019 (COVID-19): practice essentials, background, route of transmission. 2020. https://emedicine.medscape.com/article/2500114-overview#a9. [Google Scholar]
- 7.Rismanbaf A, Zarei S. Liver and kidney injuries in COVID-19 and their effects on drug therapy; a letter to editor. Arch Acad Emerg Med. 2020;8(1):e17. [PMC free article] [PubMed] [Google Scholar]
- 8.Mantovani A, Beatrice G, Dalbeni A. Coronavirus disease 2019 and prevalence of chronic liver disease: a meta-analysis. Liver Int. 2020;40(6):1316–1320. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. FastStats - chronic liver disease or cirrhosis. 2013. www.cdc.gov/nchs/fastats/liver-disease.htm.
- 10.American Liver Foundation. Your liver and COVID-19. 2020. https://liverfoundation.org/for-patients/about-the-liver/health-wellness/your-liver-and-covid-19-novel-coronavirus/.
- 11.Centers for Disease Control and Prevention. What to know about liver disease and COVID-19. 2020. www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/liver-disease.html.
- 12.McIntosh K, Hirsch M, Bloom A. Coronavirus disease 2019 (COVID-19): clinical features. 2020. www.uptodate.com/contents/coronavirus-disease-2019-covid-19-clinical-features?search=coronavirus+disease+20 19+%28Covid-19%29%3A+clinical+features+and+diagnosis. [Google Scholar]
- 13.Center for Disease Control and Prevention. Certain medical conditions and risk for severe COVID-19 illness. www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html.
- 14.Zaim S, Chong JH, Sankaranarayanan V, Harky A. COVID-19 and multiorgan response. Curr Probl Cardiol. 2020;45(8):100618. doi:10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;215:108427. doi:10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Hu Y, Yu J, Ma T. Retrospective analysis of laboratory testing in 54 patients with severe- or critical-type 2019 novel coronavirus pneumonia. Lab Invest. 2020:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li J, Fan J-G. Characteristics and mechanism of liver injury in 2019 coronavirus disease. J Clin Transl Hepatol. 2020;8(1):13–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boeckmans J, Rodrigues RM, Demuyser T, Piérard D, Vanhaecke T, Rogiers V. COVID-19 and drug-induced liver injury: a problem of plenty or a petty point. Arch Toxicol. 2020;94:1367–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dennis Lee MD. Tylenol liver damage: signs, symptoms, dosage, treatment. MedicineNet. 2016. www.medicinenet.com/tylenol_liver_damage/article.htm. [Google Scholar]
- 20.U.S. Food and Drug Administration. FDA advises patients on use of non-steroidal anti-inflammatory drugs (NSAIDs) for COVID-19. 2020. www.fda.gov/drugs/drug-safety-and-availability/fda-advises-patients-use-non-steroidal-anti-inflammatory-drugs-nsaids-covid-19.
- 21.U.S. Food & Drug Administration. Remdesivir EUA letter of authorization. 2020. www.fda.gov/media/137564/download.
- 22.U.S. Food and Drug Administration. FDA approves first treatment for COVID-19. 2020. https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-covid-19.
- 23.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19 - final report. N Engl J Med. 2020;383(19):1813–1826. doi:10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Szabo L. Chasing the elusive dream of a COVID cure. Kaiser Health News. 2020. https://khn.org/news/chasing-the-elusive-dream-of-a-covid-cure/. [Google Scholar]
- 25.Sun X, Wang T, Cai D, et al. Cytokine storm intervention in the early stages of COVID-19 pneumonia. Cytokine Growth Factor Rev. 2020;53:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020;80(6):607–613. doi:10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feng G, Zheng KI, Yan Q-Q, et al. COVID-19 and liver dysfunction: current insights and emergent therapeutic strategies. J Clin Transl Hepatol. 2020;8(1):18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Teo J. Early detection of silent hypoxia in Covid-19 pneumonia using smartphone pulse oximetry. J Med Syst. 2020;44(8):134. doi:10.1007/s10916-020-01587-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Institutes of Health. National Institutes of Health COVID-19 treatment guidelines. www.covid19treatmentguidelines.nih.gov. [PubMed]
- 30.Horvatits T, Drolz A, Trauner M, Fuhrmann V. Liver injury and failure in critical illness. Hepatology. 2019;70(6):2204–2215. [DOI] [PubMed] [Google Scholar]
- 31.Friedman LS. Pathogenesis of liver injury in circulatory failure. 2020. https://www-uptodate-com.ezproxy.uthsc.edu/contents/pathogenesis-of-liver-injury-in-circulatory-failure?search=pathogenesis%20of%20liver%20injury%20in%20circulatory%20failure&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. [Google Scholar]
- 32.Portincasa P, Krawczyk M, Machill A, Lammert F, Ciaula AD. Hepatic consequences of COVID-19 infection. Lapping or biting. Eur J Intern Med. 2020;77:18–24. doi:10.1016/j.ejim.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19) how to protect yourself and others. 2019. www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention-H.pdf.
- 34.Fix OK, Hameed B, Fontana RJ, et al. Clinical best practice advice for Hepatology and Liver Transplant Providers during the COVID-19 pandemic: AASLD expert panel consensus statement. Hepatology. 2020;72(1):287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cai Q, Huang D, Yu H, et al. COVID-19: abnormal liver function tests. J Hepatol. 2020;73(3):566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hydroxychloroquine: MedlinePlus drug information. https://medlineplus.gov/druginfo/meds/a601240.html.
- 37.Interferons (Alfa, Beta). 2020. www.covid19treatmentguidelines.nih.gov/immune-based-therapy/immunomodulators/interferons/.
- 38.National Institutes of Health. Chloroquine: MedlinePlus drug information. MedlinePlus. 2020. https://medlineplus.gov/druginfo/meds/a682318.html.
- 39.Mayo Clinic. Hydroxychloroquine (Oral Route) side effects. 2020. www.mayoclinic.org/drugs-supplements/hydroxychloroquine-oral-route/side-effects/drg-20064216?p=1.
- 40.U.S. Food and Drug Administration. FDA issues emergency use authorization for convalescent plasma as potential promising Covid-19 treatment, another achievement in administration's fight against pandemic. 2020. www.fda.gov/news-events/press-announcements/fda-issues-emergency-use-authorization-convalescent-plasma-potential-promising-covid-19-treatment.
- 41.Cullison C. The storm within: cytokine storm and COVID-19. 2020. www.emdocs.net/the-storm-within-cytokine-storm-and-covid-19/. [Google Scholar]
- 42.Highleyman L. Updated: remdesivir cleared for emergency use to treat COVID-19. 2020. www.poz.com/article/remdesivir-appears-promising-covid19-treatment. [Google Scholar]
- 43.Cytokine Storm: the sudden crash in patients with COVID-19. Physician's Weekly. 2020. www.physiciansweekly.com/cytokine-storm-the-sudden-crash-in-patients-with-covid-19/.
- 44.Estes C. What is the cytokine storm and why is it so deadly for coronavirus patients? Forbes. 2020. https://www.forbes.com/sites/claryestes/2020/04/16/what-is-the-cytokine-stormand-why-is-it-so-deadly-for-covid-19-patients/#6f382d79460f. Accessed June 30, 2020. [Google Scholar]
- 45.Koenecke A, Powell M, Xiong R, et al. Alpha-1 adrenergic receptor antagonists to prevent hyperinflammation and death from lower respiratory tract infection. https://arxiv.org/abs/2004.10117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gaze D. Dexamethasone: what is the breakthrough treatment for COVID-19? 2020. https://theconversation.com/dexamethasone-what-is-the-breakthrough-treatment-for-covid-19-140966. [Google Scholar]
- 47.World Health Organization. WHO welcomes preliminary results about dexamethasone use in treating critically ill COVID-19 patients. 2020. www.who.int/news-room/detail/16-06-2020-who-welcomes-preliminary-results-about-dexamethasone-use-in-treating-critically-ill-covid-19-patients.
- 48.Friedman L. Ischemic hepatitis, hepatic infarction, and ischemic cholangiopathy. 2020. https://www-uptodate-com.ezproxy.uthsc.edu/contents/ischemic-hepatitis-hepatic-infarction-and-ischemic-cholangiopathy?search=Ischemic%20hepatitis,%20hepatic%20infarction,%20and%20ischemic%20cholangiopathy&source=search_result&selectedTitle=1~120&usage_type=default&display_rank=1. [Google Scholar]
- 49.Center for Disease Control and Prevention. Symptoms of coronavirus. 2020. www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.


