In The Lancet, Laura Hammitt and colleagues1 describe a reduction of pneumococcal disease burden in all ages by childhood immunisation with ten-valent pneumococcal conjugate vaccine (PCV) in Kenya, a low-income country (LIC), which adds to the body of evidence for this effect, which is well described to date only in high-income2 and middle-income3 countries.
Their longitudinal surveillance study established a comprehensive clinical and microbiological surveillance system within the Kilifi Health and Demographic Surveillance System (KHDSS) that encompassed a population of 284 826 in 2016, where blood and cerebrospinal fluid were obtained using a detailed protocol in individuals admitted to the sole government hospital; cross-sectional nasopharyngeal (NP) carriage surveys were conducted annually on 500 randomly selected individuals of all ages; and vaccination data were linked to children’s identification in the KHDSS at the 26 clinics administering vaccines. Using this thorough surveillance system, Hammitt and colleagues1 show significant reductions in vaccine-type (VT) invasive pneumococcal disease (IPD) and VT carriage in all age groups, although VT carriage persisted in 6% of children younger than 5 years of age. In Hammitt and colleagues’ study, introduction of the ten-valent pneumococcal conjugate vaccine with a catch-up campaign for children younger than 5 years and without a booster dose reduced the incidence of VT IPD in children aged up to 5 years by 92% (95% CI 78–97) and in unvaccinated children by 74% (41–89) in the 5–14-year age group and by 81% (49–93) in the 15 years and older age group. The strength of this study lies in the establishment of the surveillance and laboratory systems, and their linkage to a well functioning health and demographic surveillance system, leading to high-quality, reliable evidence of vaccine effectiveness. The major limitation to extending this study to other LICs is that although direct measurement of changes in IPD is important to assess vaccine effectiveness and the effect of serotype replacement,1–3 the need for a well established infrastructure that includes policies to obtain blood and cerebrospinal fluid samples and sophisticated microbiology laboratories, presents a formidable challenge in many LICs. NP carriage is easier to detect and evaluation of reductions in VT carriage, as also reported by Hammitt and colleagues,1 can provide a surrogate marker of PCV effectiveness and herd protection in LICs.
Hammitt and colleagues1 show the effect of the PCV10 programme on IPD and the similar effect on NP carriage, both in vaccinated and unvaccinated populations, thus adding to extensive data that herd protection is induced by prevention of transmission of PCV serotypes, which is mediated by reduction in carriage. This study also supports the evidence that reduction in VT carriage among children aged 3–5 years, who were part of the catch-up population in Kilifi, might be the best predictor of reductions in invasive pneumococcal disease among all ages.4 The importance of these inferences from Hammitt’s study is that they would allow cross-sectional measurement of VT carriage in children aged younger than 5 years following PCV programme implementation, which is a valuable tool, and perhaps the only widely accessible tool to assess new strategies to sustain immunisation programmes in LICs, especially those graduating from financial support from Gavi, the Vaccine Alliance.
As noted by Hammitt and colleagues,1 the residual VT colonisation in Kilifi is higher than that seen in high-income countries such as the USA5 and the UK,6 where booster dose-containing schedules, either three or four doses (2 + 1 or 3 + 1), lead to residual VT carriage in less than 5% of children younger than 5 years. A rapid decrease in VT carriage was seen in this age group in South Africa, a middle-income country, where only 1 year after implementation of a three-dose booster-containing schedule, VT colonisation in children aged 3 months to 2 years decreased from 40. 8% to 13.8%.7 By contrast, data from Mozambique 2 years post implementation of a three-dose PCV regimen administered at 6, 10, and 14 weeks of age without a booster and without catchup (3 + 0) showed a residual VT carriage prevalence of 20.7%.8 Even in more mature PCV programmes in Malawi9 and The Gambia,10 which use a 3 + 0 schedule, residual VT carriage remains high at 16.5% (3 years after introduction) and 11.4% (5 years following introduction). The 6% residual VT carriage described by Hammitt and colleagues in children younger than 5 years in Kilifi may be secondary to rapid induction of herd protection due to catch-up vaccination of older children aged 1–5 years, despite the lack of administration of a booster dose.
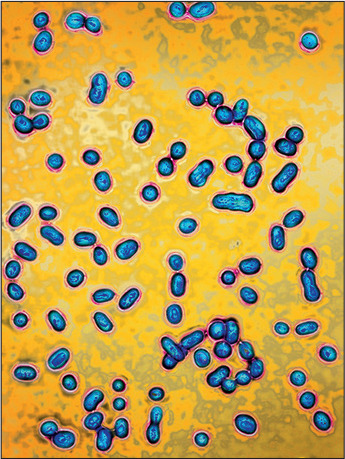
James Cavallini/Science Photo Library
Although the benefits of a catch-up PCV programme are apparent here in Kilifi, contributing to data that have led Gavi to belatedly accept catch-up as an introduction strategy, the long-term effect of this approach on residual VT transmission is unknown, and a more affordable long-term approach, such as a 2 + 1 strategy, might be needed to achieve and maintain population protection. In countries with low levels of VT disease and carriage, a further iteration of population protection might be to eliminate a further infant dose for a 1 + 1 strategy, as suggested by the UK11—provided that the second dose is a booster—to maintain population protection through low levels of VT carriage in children. For countries without boosters, a population-based approach might be to first change to the three-dose booster containing a 2 + 1 regimen to achieve and then maintain carriage of VT at low levels, followed by the two-dose booster containing a 1 + 1 regimen, which might provide a more sustainable and affordable option. In support of this idea, the Bill & Melinda Gates Foundation is funding studies to evaluate the immunogenicity and effect on carriage of the two-dose (1 + 1) regimen in The Gambia, India, South Africa, and Vietnam. Thus far, similar immunogenicity to that seen in the UK of this two-dose regimen has been shown in South Africa (Shabir Madhi, Medical Research Council, Respiratory and Meningeal Pathogens Research Unit, University of the Witwatersrand and Department of Science/National Research Foundation: Vaccine Preventable Diseases, Faculty of Health Science, University of the Witwatersrand, Johannesburg, South Africa, personal communication). Further data on VT disease and carriage will, we hope, elucidate the cost–benefit criteria for a two-dose future comprising more affordable, booster-containing PCV regimens for maintenance of pneumococcal VT herd protection in LICs.
References
- 1.Hammitt LL, Etyang AO, Morpeth SC, et al. Effect of ten-valent pneumococcal conjugate vaccine on invasive pneumococcal disease and nasopharyngeal carriage in Kenya: a longitudinal surveillance study. Lancet 2019; published online April 15 10.1016/S0140-6736(18)33005-8 [DOI] [PMC free article] [PubMed]
- 2.Moore MR, Link-Gelles R, Schaffner W, et al. Effect of use of 13-valent pneumococcal conjugate vaccine in children on invasive pneumococcal disease in children and adults in the USA: analysis of multisite, population-based surveillance. Lancet Infect Dis 2015; 15: 301–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.von Gottberg A, de Gouveia L, Tempia S, et al. Effects of vaccination on invasive pneumococcal disease in South Africa. N Engl J Med 2014; 371: 1889–99. [DOI] [PubMed]
- 4.Weinberger DM, Pitzer VE, Regev-Yochay G, Givon-Lavi N, Dagan R. Association between the decline in pneumococcal disease in unimmunized adults and vaccine-derived protection against colonization in toddlers and preschool-aged children. Am J Epidemiol 2018; 188: 160–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Loughlin AM, Hsu K, Silverio AL, Marchant CD, Pelton SI. Direct and indirect effects of PCV13 on nasopharyngeal carriage of PCV13 unique pneumococcal serotypes in Massachusetts’ children. Pediatr Infect Dis J 2014; 35: 504–10. [DOI] [PubMed] [Google Scholar]
- 6.Southern J, Andrews N, Sandu P, et al. Pneumococcal carriage in children and their household contacts six years after introduction of the 13-valent pneumococcal conjugate vaccine in England. PLoS One 2018; 13: e0195799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nzenze SA, Madhi SA, Sheri T, et al. Imputing the direct and indirect effectiveness of childhood pneumococcal conjugate vaccine against invasive pneumococcal disease by surveying temporal changes in nasopharyngeal pneumococcal colonization. Am J Epidemiol 2017; 186: 435–44. [DOI] [PubMed] [Google Scholar]
- 8.Sigauque B, Moiane B, Massora S, et al. Early declines in vaccine type pneumococcal carriage in children less than 5 years old after introduction of 10-valent pneumococcal conjugate vaccine in Mozambique. Pediatr Infect Dis J 2018; 37: 1054–60. [DOI] [PubMed] [Google Scholar]
- 9.Heinsbroek E, Tafatatha T, Phiri A, et al. Pneumococcal carriage in households in Karonga District, Malawi, before and after introduction of 13-valent pneumococcal conjugate vaccination. Vaccine 2018; 36: 7369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Usuf E, Bottomly C, Bojang E, et al. Persistence of nasopharyngeal pneumococcal vaccine serotypes and increase of nonvaccine serotypes among vaccinated infants and their mothers 5 years after introduction of pneumococcal conjugate vaccine 13 in The Gambia. Clin Infect Dis 2018; published online August 24 DOI: 10.1093/cid/ciy726. [DOI] [PMC free article] [PubMed]
- 11.Goldblatt D, Southern J, Andrews N, et al. Pneumococcal conjugate vaccine 13 delivered as one primary and one booster dose (1 + 1) compared with two primary doses and a booster (2 + 1) in UK infants: a multicentre, parallel group randomised controlled trial. Lancet Infect Dis 2018; 18: 171–79. [DOI] [PMC free article] [PubMed] [Google Scholar]


