Abstract
Background
The use of fine art in medical education has a long history. Numerous studies have investigated the potential benefits of incorporating art in medical education; however, there are gaps in knowledge regarding the efficacy, methodology, and clinical significance of these studies.
Objective
This scoping review of the literature aims to describe the available literature on the incorporation of art education in medical school and residency.
Methods
PubMed, Google Scholar, and MedEDPortal were queried from their inception dates through December 2019. English-language studies providing a detailed methodology and detailed analysis were included. A total of 37 studies were identified. Upon further screening of the studies' methodologies and results, 16 studies describing art education implemented with medical students and 12 studies describing art education implemented with residents were included for final review.
Results
Various methods of art education exist, including Visual Thinking Strategies (VTS), rigorous curricula, and unstructured roundtable discussions with art curators or artistically minded clinicians. Studies range in duration, art media, and type of analysis.
Conclusions
There has been an increasing effort to incorporate fine art education into medical training, primarily to enhance visual perception skills and empathy. Although there is limited research on its efficacy, and wide variations in study methodologies exist, results consistently indicate that participants find the incorporation of art into curricula beneficial. Further research analyzing which methodologies are most likely to yield statistically and clinically significant improvements in visual perception and empathy may lead to increased utilization of this teaching method.
Introduction
Physicians utilize pattern recognition and visual acuity skills to recognize physical examination findings and associate them with diagnoses. Examining and studying fine art could theoretically supplement a resident's training in this task. In the modern era of medical training, art has not been a curricular focus, despite having a role in the early days of medical training.1 Recently, however, there has been an effort to incorporate the use of fine art into medical training. Proponents purport that learning how to analyze fine art may improve not only clinicians' intellectual curiosity and critical thinking, but also their diagnostic skills and ability to empathize with patients.2
Observational skills may be especially useful in visually oriented specialties. Dermatologists must be skilled in pattern recognition in order to distinguish and diagnose cutaneous diseases, some with subtle differences in examination findings. Similar skills are required for radiologists in their examination of a variety of imaging modalities. With increasing use of telemedicine, it is important for physicians to be able to appreciate clinical situations in the absence of a full physical examination.
While there are numerous studies investigating art in medical education, there remain gaps in knowledge regarding the efficacy, methodology, and clinical significance of these courses. We discuss the results of a scoping review of the literature on the use of art education in medical training, highlighting the results of a few representative studies.
Methods
PubMed, Google Scholar, and MedEdPortal were queried from their inception dates through December 2019 using variable combinations of the keywords: art, art education, medical education, residency, and medical residency. Only articles published in English were included. Titles were then filtered for relevance, as the broad search terms yielded results that were not related to the research topic (Figure). Studies were excluded if they were reviews, lacked a postintervention assessment, the methodology was not described well enough to appropriately replicate, or the article was inaccessible via the institutional library. For example, some articles were excluded as the type of art intervention was not specified. This process was primarily performed by 1 author (Y.D.), with oversight by the other 2 authors (E.C.M. and E.A.R.).
Figure.
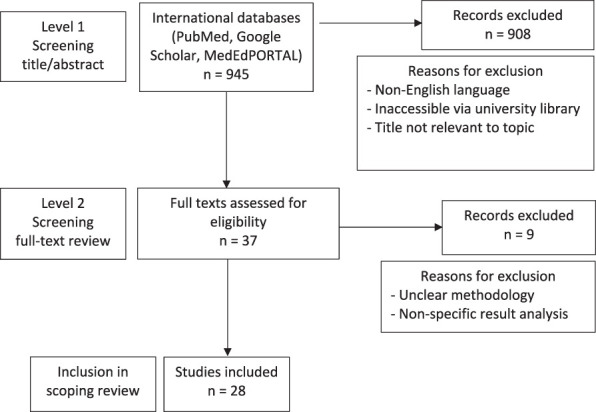
Flowchart of Identified Studies
Results
A total of 37 curricular interventions that discussed the implementation of art in medical education were identified for full-text screening. Upon further review, 28 articles3–30 were selected for inclusion owing to their detailed methodologies and analyses, including 16 describing art education with medical students (Table 1)3–11,13–19 and 12 involving residents (Table 2).12,20–30 Some interventions relied on professional art curators to teach fine art to participants, while others used artistically minded clinicians. The duration of the projects ranged from 1 to 17 sessions. The media of art also greatly varied.3,4 While most programs utilized art as a vehicle to increase observational skills, other interventions used art to directly depict medical conditions.31,32 The data were separated into 2 categories: interventions implemented among medical students and interventions implemented among residents. Details on research design, endpoints, and results are outlined in tables 1 and 2.
Table 1.
Studies of Medical Students
| Author(s), (y) | No. of Subjects | Participants | No. of Sessions | Goal | Art Medium and Intervention Style | Measurement | Results | Control Group |
| Bardes et al,7 (2001) | 8 | MS(1, 2, 4) | 3 | OS, descriptive skills, and interpretive skills | Visit to museum and discussion of FA, patient faces | Comparison of descriptions on pre- and posttests | Improved OS on subjective analysis of descriptions | No |
| Dolev et al,8 (2001) | 176 | MS(1) | 1 | CS | Visit to museum and discussion of FA | Comparison of descriptions on pre- and posttests | Increase in OSa | Yes |
| Elder et al,9 (2006) | 17 | MS(2) | 15–17 | CS | Visit to museum and discussion of art (genre not specified) | Subjective participant feedback | Improved CS and personal development | No |
| Shapiro et al,4 (2006) | 38 | MS(3) | 3 | OS and pattern recognition | Classroom discussion of FA, mixed media art, and clinical images | Subjective participant feedback | Improved OS, pattern recognition, and emotional recognition | No |
| Naghshineh et al,6 (2008) | 58 | MS(1, 2) | 9 | OS | Visit to museum and discussion of FA followed by simulated physical diagnosis lab | Comparison of descriptions and performance on pre- and posttests | Increased OS and analytical skills on subjective analysis of student feedback Improvement in number of observations made, sophistication of descriptions of artistic and clinical imagerya Improvement in participants who attended 8 or more sessions compared to 7 or fewera |
Yes |
| Klugman et al,5 (2011) | 32 | Medical and nursing students | 3 | OS, tolerance for ambiguity, interest in learning communication skills | Visit to museum and discussion of FA | Comparison of performance on pre- and posttests | Improvement in time spent looking at, number of words used to describe, and number of observations made in art and patient imagesa | No |
| Schaff et al,3 (2011) | N/A | MS(1, 2) | Not specified | Abstract thinking | Visit to museum and discussion of contemporary art | Subjective participant feedback | Students claimed the experience “very highly” fulfilled its objectives | No |
| Jasani and Saks,11 (2013) | 70 | MS(2) | 1 | OS | Classroom discussion of FA | Comparison of descriptions and performance on pre- and posttests | Increased OS on student feedback, and no statistically significant improvement in OS between pre and posttests | No |
| Klugman and Beckmann-Mendez,13 (2015) | 19 | Medical and nursing students | 5 | OS | Classroom discussions of FA, clinical images, and audio recordings; participants also created their own artwork | Comparison of descriptions and performance on pre- and posttests | Improved communication and patience according to participant feedback. Improvement in the number of observations made and number of words used between pre- and post-testa |
No |
| Bramstedt,14 (2016) | 66 | MS(2) | b | OS | Classroom discussion of FA, mixed media art, and essays | Subjective participant feedback | Improved reflective and OS | No |
| Kidd et al,15 (2016) | 12 | Various health care providers | 1 | Increasing empathy, respecting vulnerable persons | Discussion of “Sticky” by Margaret Sutherland at a conference | Subjective participant feedback | Increased tolerance of ambiguity and awareness of personal biases | No |
| Bentwich and Gilbey,10 (2017) | 67/120 | MS(1) | 1 | Tolerance of ambiguity, increasing empathy | Classroom discussion of FA | Subjective participant feedback | Increase in multiple domains, including OS and acceptance of multiple meanings in the post-intervention survey. Correlation between increased acceptance of multiple meanings and increased empathya | No |
| Gurwin et al,16 (2018) | 36 | MS(1) | 6 | OS | Visit to museum and discussion of FA led by art instructors | Comparison of descriptions on pre- and posttests | Improvement in OSa | Yes |
| Gowda et al,17 (2018) | 47 | MS(1) | 6 | OS, reflective skills, and self-care | Visit to museum and discussion of art led by art instructors | Comparison of pre- and post-self-assessment | Improvement in reflective abilitya Improvement in OS, TOA on subjective analysis of descriptions |
No |
| Cracolici et al,18 (2019) | 89 | MS(1) | N/A | Learning tool | Provided art supplies and encouragement to draw histological images | Comparison of descriptions on pre- and posttests | Increased desire to use art as a learning tool | Yes |
| Visscher et al,19 (2019) | 50 | MS(3) | 1 | Improve MS understanding of radiologists and radiology profession | VTS-led analysis of paintings depicting radiology encounters | Post-intervention survey | Reduced negative stereotypes by medical students of the radiology profession and of radiologists | No |
Abbreviations: MS, medical student (year); OS, observational skills; FA, fine arts; CS, clinical skills; N/A, no answer.
Indicates statistical significance.
Comprised a 50-minute workshop, written assignment, medical humanities week, and attendance of an art exhibit.
Table 2.
Studies of Residents in Training
| Author (y) | No. of Subjects | Participants | No. of Sessions | Goal | Art Medium and Intervention Style | Measurement | Results | Control Group |
| Reilly et al,20 (2005) | N/A | Family medicine residents and faculty | 1 | Team building | Visit to museum and discussion of FA | Subjective participant feedback | Improved team building and analytical thinking | No |
| Kirklin et al,21 (2007) | 68 | General practitioners and nurses | 1 | OS | Workshop where blindfolded participants described the feeling of household objects | Comparison of descriptions on pre- and posttests | Improvement in OSa | Yes |
| Huang et al,12 (2016) | 27 | Dermatology residents | 4 | Observational skills, description skills, awareness of assumptions, and tolerance of ambiguity | Visit to museum and discussion of FA and clinical images | Comparison of descriptions on pre- and posttests | Improvement between mean number of observationsa | No |
| Goodman and Kelleher,22 (2017) | 15 | Radiology residents | 1 | OS | Visit to museum and discussion of FA | Comparison of abnormality detections on pre- and posttests | Improvement detecting abnormalities on radiographsa | No |
| Griffin et al,23 (2017) | 7 | Dermatology residents | 5 | OS | Visit to museum and discussion of FA | Comparison of descriptions on pre- and posttests and subjective feedback | Improvement in OS according to participant feedback; no statistically significant improvement in pre and posttests scores that tested for OS | Yes |
| Zazulak et al,24 (2017) | 15 | OB-GYN and family medicine residents | 4 | Increase empathy, compassion, and mindfulness | Visit to museum and discussion of various art and dance led by art instructors; participants also created their own artwork | Comparison of pre- and post-surveys, and subjective participant feedback | No significant increase in overall empathy, compassion, or mindfulness Increase in subdomains of mindfulnessa |
Yes |
| Pristach et al,25 (2018) | N/A | Psychiatry residents | 1 | Increase OS, specifically regarding psychological themes | Visit to museum and discussion of various art led by art instructors | Subjective participant feedback | Increased OS that participants feel will be applicable in clinical setting | No |
| Yakhforoshha et al,26 (2018) | 19 | Oncology fellows | 1 | Communication skills | Lecture on communication skills, role playing, reflective writing, and small group discussion of art, music, film | Comparison of pre- and post-objective assessment | Improvement in 3 of 7 domains of the checklista | No |
| Harrison and Chiota-McCollum,27 (2019) | 18 | Neurology residents | 11 | Communication skills, OS, awareness of point of view, and appreciation of the narrative context of illness | Classroom discussion of various visual art and works of literature | Comparison of pre- and post-self-assessment | Increased CS, OS, and understanding of narrative medicine | No |
| Emami et al,28 (2019) | 19 | Oncology fellows | 1 | Communication skills | Various mediums and lectures by art and medical faculty | Comparison of pre- and post-self-assessment | Improved in all domains, with notable importance of communication in medical context and learninga | No |
| Marr et al,29 (2019) | 17 | Emergency medicine attendings, residents, midlevel providers | 2 | Reduce implicit bias, improve clinical skills with pain patients | Visit to museum and discussion of FA led by art and medical faculty | Subjective participant feedback | Positive change in how they make observations and communicate with patients | No |
| Orr et al,30 (2019) | 17 | Internal medicine residents | 1 | Combat burnout | Visit to museum and discussion of FA led by art instructors | Comparison or pre- and post-self-assessments | Decreased emotional exhaustion and depersonalization and increased sense of personal accomplishment | No |
Abbreviations: N/A, no answer; FA, fine arts; OS, observational skills; CS, clinical skills; OB-GYN, obstetrics and gynecology.
Indicates statistical significance.
Visual Art Implementation in Medical School
A variety of fine art curricula have been integrated into medical school education (Table 1). Four of the 12 student-based interventions utilized control groups.6,8,16,18 Three of these 4 achieved a statistically significant increase in observational skills.6,8,16 Thirteen3–7,9–11,13–15,17,19 of the 16 were led by art educators and were primarily qualitative in nature, while 9 incorporated a quantitative component.5–8,11,13,16–18 Two interventions (one quantitative and one qualitative) showed a dose-dependent response between the number of art sessions participants attended and the level of improvement in observational skills.5,6
In 2001, Bardes et al published the first study examining the use of fine arts in medical education.7 Their qualitative study demonstrated that students who participated in an art intervention improved their objective observational skills as well as their subjective ability to interpret facial expressions of patients.7 Subsequently, Dolev et al provided quantitative evidence of the benefits of fine art education in medical students.8 In this study, students described a photograph of a person with a medical disease both before and after an arts curriculum intervention, and responses were graded on a predefined objective scale. After the intervention, students made more detailed observations and less observational mistakes.8
Elder et al described an integrated program in which medical students attended a real patient-physician encounter, and then sketched a picture of the encounter.9 Bentwich and Gilbey investigated other effects of art education, such as increased empathy, tolerance of ambiguity, and teamwork.10 Their findings showed an increased tolerance for ambiguity among participants. They also found that the inherent ambiguity of fine art and the resultant “acceptance of multiple meanings” understood by students was the strongest factor correlated with the intervention, even more so than increased visual skills.10 Additional projects also demonstrated the benefits of fine arts interventions improving mindfulness, identification of patient story, and emotional awareness among participants.4,7,11 Across most interventions, medical student participants voiced satisfaction with the art programming.
Visual Art Implementation in Residency
There have been few studies evaluating the efficacy of fine arts education specifically in residency (Table 2). Three of the interventions used control groups, and one of those achieved a statistically significant increase in observational skills.32–34 Nine of the 12 contained a quantitative component, and 9 were led by professional art educators.
Some medical educators utilized Visual Thinking Strategies (VTS), a teaching paradigm to improve the visual literacy of both experienced and inexperienced art observers.35,36 VTS-trained educators encouraged participants to think in a structured format when viewing images by asking simple questions, such as “What is going on in this picture?” “What do you see that makes you say that?” and “What more can we find?”37 Curricula implemented at Harvard University utilized VTS-trained instructors from the Museum of Fine Arts, Boston, to teach dermatology residents, who attended 4 sessions each training year.12,38,39 The goal was to improve residents' observational skills and program camaraderie, and to gain more insight into their own observational biases. In a pilot study of this program by Huang et al, a test was administered prior to and after the intervention.12 The test asked participants to list as many observations about certain images as they could recall, and the responses were objectively graded to determine if there was a statistically significant change between pre- and post-intervention observations.12 The results did demonstrate a dose-dependent improvement in pretest and posttest scores, as residents who attended less than 3 sessions did not show a statistically significant improvement in the number of details they recalled, while those who attended 3 or 4 did (P < .034).12
Discussion
As described in the literature, various methods of utilizing fine art to advance medical student and resident education appear to be effective. Incorporating art into medical education appears to improve visual perception skills, empathy, and personal reflection among students. Such an intervention could improve diagnostic accuracy, ethical competency, identity formation, and psychological functioning in students and physicians.40,41 Despite the variation in these interventions, satisfaction-level outcomes have been generally positive: students have noted wide appreciation for fine art courses and advocated for their continued use.
This scoping review was limited by the keywords and databases used, exclusion of non-English studies, accessibility of the journal articles, and overall quality of the studies available. Many studies had small sample sizes, lacked control groups, and did not incorporate quantitative data. A more comprehensive systematic review was not pursued given the variable study populations and the highly heterogenous study designs, methodologies, and reported outcome measures, making inter-study comparisons and conclusions difficult to draw.
With increased use of technology and imaging in medicine, there is a growing need for physicians to observe minute differences in examination findings. Additionally, in aesthetic fields like dermatology, ophthalmology, and plastic surgery, many physicians perform cosmetic procedures that require a keen eye for observing fine details. Beyond enhancing visual perception, available research demonstrates that art education improves empathy among participants and may be a way for budding physicians to better connect with patients. Despite the growing available literature, there remain several unanswered questions regarding the benefit of art education interventions in medical training. Further research analyzing which methodologies are most likely to yield statistically and clinically significant improvements in visual perception and empathy may lead to increased utilization of this teaching method. Specifically, identifying the optimum point of intervention during medical education, as well as conducting follow-up studies to elucidate whether positive effects are lasting, would be beneficial.
In reviewing the current literature, best practices on how to incorporate fine arts in medical education appear to emerge. An ideal curriculum should encompass 4 domains: pattern recognition, deep seeing, facial expression, and pertinent negatives. These domains could be modified or adapted to suit curricula in visually intensive fields (eg, dermatology, radiology, endoscopic gastroenterology).
Pattern recognition is an experience-based process of perceptual learning whereby trainees recognize physical examination findings and associate them with diagnoses. Traditionally this is developed through studying countless clinical images and managing thousands of patients. Fine art curricula incorporating pattern recognition skills could help enhance diagnostic acumen and efficiency. Deep seeing involves the ability to perceive textures and colors that may not be immediately distinguishable. This can translate clinically to observing details beyond the most prominent colors and textures. Moreover, with the increasing use of telemedicine, it is important for residents to be able to “see” the textures in the absence of a full physical examination. Interpretation of facial expressions of a painting's subject(s) often helps identify the artist's intent or message. In medicine, similarly, accurate interpretation of facial expressions is likely to enhance empathy and quality of care. Finally, pertinent negatives are a critical aspect to forming a diagnosis as what is not found on physical examination can affect the differential diagnosis of the patient. When studying fine art, students are often encouraged to observe what the artist intentionally did not depict.
The framework of VTS seems to be effective, and the evidence suggests that instructors comprise both clinicians and art curators. Future efforts would benefit from a standardized curriculum and assessment guidelines.
Conclusions
An increasing effort to incorporate fine art education into medical training has yielded early data that suggest the possibility of enhanced visual perception skills and empathy. Although substantial limitations characterize the data and further work is needed, studies consistently indicated that participants found the incorporation of an art curriculum to be beneficial to medical education.
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
Contributor Information
Yoseph Dalia, Dermatology Resident, Department of Dermatology, University of Tennessee Health Science Center.
Emily C. Milam, Clinical Instructor, Ronald O. Perelman Department of Dermatology, New York University Langone Health.
Evan A. Rieder, Assistant Professor, Ronald O. Perelman Department of Dermatology, New York University Langone Health.
References
- 1.Goetz CG. Visual art in the neurologic career of Jean-Martin Charcot. Arch Neurol. 1991;48(4):421–425. doi: 10.1001/archneur.1991.00530160091020. [DOI] [PubMed] [Google Scholar]
- 2.Katz JT, Khoshbin S. Can visual arts training improve physician performance? Trans Am Clin Climatol Assoc. 2014;125:331–341. discussion 341–342. [PMC free article] [PubMed] [Google Scholar]
- 3.Schaff PB, Isken S, Tager RM. From contemporary art to core clinical skills: observation, interpretation, and meaning-making in a complex environment. Acad Med. 2011;86(10):1272–1276. doi: 10.1097/ACM.0b013e31822c161d. [DOI] [PubMed] [Google Scholar]
- 4.Shapiro J, Rucker L, Beck J. Training the clinical eye and mind: using the arts to develop medical students' observational and pattern recognition skills. Med Educ. 2006;40(3):263–268. doi: 10.1111/j.1365-2929.2006.02389.x. [DOI] [PubMed] [Google Scholar]
- 5.Klugman CM, Peel J, Beckmann-Mendez D. Art rounds: teaching interprofessional students visual thinking strategies at one school. Acad Med. 2011;86(10):1266–1271. doi: 10.1097/ACM.0b013e31822c1427. [DOI] [PubMed] [Google Scholar]
- 6.Naghshineh S, Hafler JP, Miller AR, Blanco MA, Lipsitz SR, Dubroff RP, et al. Formal art observation training improves medical students' visual diagnostic skills. J Gen Intern Med. 2008;23(7):991–997. doi: 10.1007/s11606-008-0667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bardes CL, Gillers D, Herman AE. Learning to look: developing clinical observational skills at an art museum. Med Educ. 2001;35(12):1157–1161. doi: 10.1046/j.1365-2923.2001.01088.x. [DOI] [PubMed] [Google Scholar]
- 8.Dolev JC, Friedlaender LK, Braverman IM. Use of fine art to enhance visual diagnostic skills. JAMA. 2001;286(9):1020–1021. doi: 10.1001/jama.286.9.1020. [DOI] [PubMed] [Google Scholar]
- 9.Elder NC, Tobias B, Lucero-Criswell A, Goldenhar L. The art of observation: impact of a family medicine and art museum partnership on student education. Fam Med. 2006;38(6):393–398. [PubMed] [Google Scholar]
- 10.Bentwich ME, Gilbey P. More than visual literacy: art and the enhancement of tolerance for ambiguity and empathy. BMC Med Educ. 2017;17(1):200. doi: 10.1186/s12909-017-1028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jasani SK, Saks NS. Utilizing visual art to enhance the clinical observation skills of medical students. Med Teach. 2013;35(7):e1327–e1331. doi: 10.3109/0142159X.2013.770131. [DOI] [PubMed] [Google Scholar]
- 12.Huang JT, Reynolds SD, DiGiovanni Evans B, Zimmermann C, CJ Joyce, Katz JT, et al. Fine arts curriculum improves observational skills of dermatology trainees: a pilot study. Br J Dermatol. 2016;175(4):815–817. doi: 10.1111/bjd.14616. [DOI] [PubMed] [Google Scholar]
- 13.Klugman CM, Beckmann-Mendez D. One thousand words: evaluating an interdisciplinary art education program. J Nurs Educ. 2015;54(4):220–223. doi: 10.3928/01484834-20150318-06. [DOI] [PubMed] [Google Scholar]
- 14.Bramstedt KA. The use of visual arts as a window to diagnosing medical pathologies. AMA J Ethics. 2016;18(8):843–854. doi: 10.1001/journalofethics.2016.18.8.imhl1-1608. [DOI] [PubMed] [Google Scholar]
- 15.Kidd M, Nixon L, Rosenal T, Jackson R, Pereles L, Mitchel I, et al. Using visual art and collaborative reflection to explore medical attitudes toward vulnerable persons. Can Med Educ J. 2016;7(1):e22–e30. [PMC free article] [PubMed] [Google Scholar]
- 16.Gurwin J, Revere KE, Niepold S, Bassett B, Mitchell R, Davidson S, et al. A randomized controlled study of art observation training to improve medical student ophthalmology skills. Ophthalmology. 2018;125(1):8–14. doi: 10.1016/j.ophtha.2017.06.031. [DOI] [PubMed] [Google Scholar]
- 17.Gowda D, Dubroff R, Willieme A, Swan-sein A, Capello C. Art as sanctuary: a four-year mixed-methods evaluation of a visual art course addressing uncertainty through reflection. Acad Med. 2018 doi: 10.1097/ACM.0000000000002379. 93(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 57th Annual Research in Medical Education Sessions):8–13. [DOI] [PubMed]
- 18.Cracolici V, Judd R, Golden D, Cipriani NA. Art as a learning tool: medical student perspectives on implementing visual art into histology education. Cureus. 2019;11(7):e5207. doi: 10.7759/cureus.5207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Visscher KL, Bloom LF, Ladonna KA, Faden L, Rakhra KS. How can artistic paintings broaden medical students' understanding of the radiology profession? Acad Radiol. 2019;26(12):1718–1725. doi: 10.1016/j.acra.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Reilly JM, Ring J, Duke L. Visual thinking strategies: a new role for art in medical education. Fam Med. 2005;37(4):250–252. [PubMed] [Google Scholar]
- 21.Kirklin D, Duncan J, McBride S, Hunt S, Griffin M. A cluster design controlled trial of arts-based observational skills training in primary care. Med Educ. 2007;41(4):395–401. doi: 10.1111/j.1365-2929.2007.02711.x. [DOI] [PubMed] [Google Scholar]
- 22.Goodman TR, Kelleher M. Improving novice radiology trainees' perception using fine art. J Am Coll Radiol. 2017;14(10):1337–1340. doi: 10.1016/j.jacr.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 23.Griffin LL, Chiang NYZ, Tomlin H, Young HS, Griffiths CEM. A visual literacy course for dermatology trainees. Br J Dermatol. 2017;177(1):310–311. doi: 10.1111/bjd.15073. [DOI] [PubMed] [Google Scholar]
- 24.Zazulak J, Sanaee M, Frolic A, Knibb N, Tesluk E, Hughes E, et al. The art of medicine: arts-based training in observation and mindfulness for fostering the empathic response in medical residents. Med Humanit. 2017;43(3):192–198. doi: 10.1136/medhum-2016-011180. [DOI] [PubMed] [Google Scholar]
- 25.Pristach CA, Del Regno PA, Dubovsky S. More than meets the eye: using art to teach psychotherapy. Acad Psychiatry. 2019;43(1):119–122. doi: 10.1007/s40596-018-0958-7. [DOI] [PubMed] [Google Scholar]
- 26.Yakhforoshha A, Emami SAH, Shahi F, Shahsavari S, Cheraghi M, Mojtahedzadeh R, et al. Effectiveness of integrating simulation with art-based teaching strategies on oncology fellows' performance regarding breaking bad news. J Cancer Educ. 2019;34(3):463–471. doi: 10.1007/s13187-018-1324-x. [DOI] [PubMed] [Google Scholar]
- 27.Harrison MB, Chiota-mccollum N. Education research: an arts-based curriculum for neurology residents. Neurology. 2019;92(8):e879–e883. doi: 10.1212/WNL.0000000000006961. [DOI] [PubMed] [Google Scholar]
- 28.Emami SAH, Shirazi M, Yakhforoshha A. Effectiveness of integrating simulation with art-based teaching on attitudes of oncology fellows for learning communication skills: a pilot study [published online ahead of print August 2, 2019] J Cancer Educ. doi: 10.1007/s13187-019-01594-3. [DOI] [PubMed]
- 29.Marr B, Mickey SH, Blythe SG, Baruch J. The weight of pain: what does a 10 on the pain scale mean? An innovative use of art in medical education to enhance pain management. J Pain Symptom Manage. 2019;57(6):1182–1187. doi: 10.1016/j.jpainsymman.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 30.Orr AR, Moghbeli N, Swain A, Bassett B, Niepold S, Rizzo A, et al. The Fostering Resilience through Art in Medical Education (FRAME) workshop: a partnership with the Philadelphia Museum of Art. Adv Med Educ Pract. 2019;10:361–369. doi: 10.2147/AMEP.S194575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mostow EN. The “ABCs” of dermatology: using art, bird-watching, and computers to enhance the teaching and learning of dermatology. Clin Dermatol. 2008;26(1):97–99. doi: 10.1016/j.clindermatol.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 32.Sandhu VK. Inspection–a fine art. JAMA Dermatol. 2018;154(5):630. doi: 10.1001/jamadermatol.2018.0307. [DOI] [PubMed] [Google Scholar]
- 33.Kirklin D, Duncan J, McBride S, Hunt S, Griffin M. A cluster design controlled trial of arts-based observational skills training in primary care. Med Educ. 2007;41(4):395–401. doi: 10.1111/j.1365-2929.2007.02711.x. [DOI] [PubMed] [Google Scholar]
- 34.Griffin LL, Chiang NYZ, Tomlin H, Young HS, Griffiths CEM. A visual literacy course for dermatology trainees. Br J Dermatol. 2017;177(1):310–311. doi: 10.1111/bjd.15073. [DOI] [PubMed] [Google Scholar]
- 35.Flood J, Brice-Heath S, Lapp D. Handbook of Research on Teaching Literacy through the Communicative and Visual Arts. New York, NY: Routledge;; 2015. [Google Scholar]
- 36.Visual Thinking Strategies. 2020 https://vtshome.org/ Accessed September 21.
- 37.Yenawine P. Visual Thinking Strategies Using Art to Deepen Learning across School Disciplines. Cambridge, MA: Harvard Education Press;; 2013. [Google Scholar]
- 38.Braverman IM. To see or not to see: how visual training can improve observational skills. Clin Dermatol. 2011;29(3):343–346. doi: 10.1016/j.clindermatol.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 39.Zimmermann C, Huang JT, Buzney EA. Refining the eye: dermatology and visual literacy. J Mus Educ. 2016;41(2):116–122. doi: 10.1080/10598650.2016.1163189. [DOI] [Google Scholar]
- 40.Genovese JM, Berek JS. Can arts and communication programs improve physician wellness and mitigate physician suicide? J Clin Oncol. 2016;34(15):1820–1822. doi: 10.1200/JCO.2015.65.1778. [DOI] [PubMed] [Google Scholar]
- 41.Kumagai AK. Perspective: acts of interpretation: a philosophical approach to using creative arts in medical education. Acad Med. 2012;87(8):1138–1144. doi: 10.1097/ACM.0b013e31825d0fd7. [DOI] [PubMed] [Google Scholar]


