Abstract
Background
Excessive inpatient administrative tasks can lead to adverse consequences for residents and their patients. Furthermore, this burden has been linked to depersonalization, a major component of physician burnout.
Objective
To describe the development, implementation, feasibility, acceptability, and early outcomes of Resident Team Assistant (RTA) programs.
Methods
Three large academic medical centers created RTA programs in which administrative assistants are incorporated into inpatient medical teams. First steps included a needs assessment and driver diagram creation to identify key issues and to solidify goals. Program directors were assigned, and RTAs were hired, trained, and incorporated into inpatient teams at each institution (2003, 2016, 2018). Program leadership and institutional stakeholders met regularly to discuss development and quality assurance. Surveys and direct interviews were performed to evaluate impact and acceptability. Institutional goals in accordance to RTAs tasks were also investigated.
Results
Resident surveys and interviews have shown acceptability with RTAs completing a large percentage of resident administrative tasks while promoting time spent in direct clinical care and job satisfaction. Hospital-specific improvements have included increase in referring physician communication rate and decrease in work hour violations. The programs have maintained high feasibility and sustainability with a relatively low time commitment from leadership and cost for the institutions.
Conclusions
The RTA programs at the 3 institutions have continued to be sustained over time with perceived improvements in administrative task burden and job satisfaction for the residents. They have maintained high acceptability and feasibility in terms of effort and costs for the hospitals.
Introduction
As electronic health records and work hour restrictions have become commonplace, time demands for residents have increased substantially.1–3 With the need to balance multiple responsibilities, administrative duties often take precedence over time spent in direct clinical care and educational activities.4 This failure to prioritize direct physician-patient interactions can have detrimental effects not only on communication with the patients and families but also on medical care outcomes.5 Furthermore, this burden of nonclinical tasks has been linked to depersonalization, a major component of physician burnout.6
The associated effects of burnout are detrimental, leading to higher levels of job dissatisfaction, negative attitudes toward patients, and more medical errors.7 Despite the association of depersonalization with nonclinical tasks, there have been limited research and initiatives focused on decreasing the administrative burden at the institution level, which in turn transform the volume and type of work demanded of the residents.
As nonclinical tasks continue to require substantial time and contribute to physician burnout, institutions and residency programs must find new ways to support their trainees.8,9 The implementation of a Resident Team Assistant (RTA) program allows residency programs to innovatively address challenges that their trainees frequently face, including excessive administrative burdens, time management issues, and physician burnout. This article describes the development, implementation, feasibility, acceptability, and early outcomes of RTA programs.
Methods
Three large, urban, academic tertiary pediatric medical centers created RTA programs in which administrative assistants were incorporated into inpatient medical teams to optimize patient care and promote physician wellness. These programs were established independently at different times (2003, 2016, 2018), but are collectively discussed in this article.
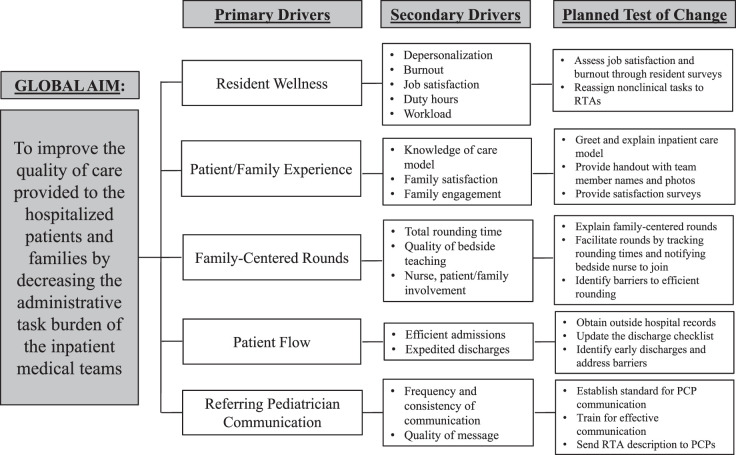
The first steps in program development included a thorough needs assessment performed by direct observation, peer review, and gap analysis, with extensive time dedicated to identifying specific ways RTAs could affect resident efficiency and wellness. A driver diagram was created to identify key issues and to solidify program goals (Figure). The role was piloted to clarify tasks and hurdles.
Figure.
Driver Diagram for Resident Team Assistant Program
Note: Figure edited to encompass all 3 institutions.
Abbreviations: RTA, resident team assistant; PCP, primary care pediatrician.
Once program objectives were established, an RTA program director was assigned for each institution (residency program director at one hospital, general pediatrics hospitalist attendings at the others), and RTAs were hired. Targeted applicants included recent college graduates looking into matriculating to a graduate health degree program and hospital clerical employees with enthusiasm and ability to anticipate patient and team needs. Job-specific training included electronic health record training and structured shadowing with residents and program leaders. Once established proficiency and competency markers were met, RTAs were incorporated into inpatient medical teams to help address nonclinical tasks (Box).
Box Resident Team Assistant Task List
Duties of the resident team assistant include (but are not limited to):
Participating in patient care rounds while calling bedside nurse and keeping track of rounding times to promote timeliness and rounding efficiency.
Scheduling inpatient tests and procudures as well as post-discharge appointments.
Obtaining medical records/test results from emergency department and referring hospitals.
Helping notify patients' primary care providers of their patients' admission via phone or institution-specific messaging system.
Greeting newly admitted patients and their families upon arrival to the inpatient floor and providing eduation on the care model as well as family-centered rounds.
Working with medical team to expedite pateint discharges (ie, early identification of transportation and other social work needs).
Helping primary team with preauthorizations, delivery of scripts/medications.
Assisting with team orientation for medical students and interns.
Calling tech support for issues with team computers and equipment.
Given the novelty of an RTA program, the feasibility of creating such a program was closely evaluated by residency leadership and institution stakeholders (eg, hospital operational leaders, division chiefs) with the goal to establish a low-cost/-effort, high-impact program. Its acceptability was evaluated by annual surveys distributed to the residents on inpatient services (provided as online supplemental material). Direct feedback was also solicited from hospital staff members (eg, nurses, unit leadership), hospitalized patients and families, and community pediatricians by telephone and/or in-person outreach. Institutional goals in accordance to the RTA tasks were also investigated.
The programs did not meet the criteria for human subjects' research based on our hospitals' institutional review board policies and were exempt from review.
Results
The RTA programs have generated sustained improvements across various measures. A resident-wide survey distributed at one of the institutions in spring 2018 found that RTAs completed a large percentage of daily administrative tasks: Nearly 50% of residents surveyed reported more than 40% of their administrative tasks being done by RTAs, with one-third reporting more than 60%. All the residents agreed or strongly agreed that RTAs allowed for more time in direct patient care. Nearly all residents agreed or strongly agreed that the discharge process was more efficient. All strongly agreed or agreed that RTAs contributed to higher job satisfaction, with no residents expressing neutral or negative effects (figures provided as online supplemental material).
Feedback from other hospital staff members, patients and families, and referring pediatricians has also been positive. Many hospitalized families expressed appreciation for RTA involvement. Primary care physicians frequently thanked the program for the more consistent notifications of their patients' hospitalizations and discharge plans. Primary pediatrician communication rates rose from an average of 70% pre-RTA to 88% post-RTA implementation (Figure provided as online supplemental material). Work hour compliance, based on the rate of 80-hour work week and 24+6-hour violations, decreased on the 2006 annual Accreditation Council for Graduate Medical Education residency surveys compared to pre-implementation in 2013 (Figure provided as online supplemental material).
Regarding feasibility, the program director position required considerable time commitment initially (12–16 hours/week) with frequent meetings to discuss development and quality assurance. However, the role became less time intensive following implementation (commitment of around 6–8 hours/week). Furthermore, the financial burden on each institution (average of 8–9 RTAs per program making $16–20/hour, 40 hours/week covering 7 days/week) has been reasonable, especially when considering the need to potentially hire other higher-paying positions (eg, case management, social work) to complete some of the tasks offloaded by RTAs.
Discussion
The RTA programs continue to be sustained with high resident, staff, and patient and family acceptability. They have led to improved administrative burden for residents, work hour compliance, and communication with community pediatricians.
Although some institutions have incorporated individuals to support the inpatient teams with specific tasks (eg, research assistant, discharge planner), RTAs can work across interdisciplinary teams in a cost-effective manner with flexible responsibilities depending on day-to-day team needs. To the authors' knowledge, there are no similar roles previously described in literature.
Initial challenges of implementation included fostering a shared understanding of specific RTA contributions and their integration into teams. The residency programs made conscientious efforts to solidify RTA roles and overcome initial suboptimal utilization. Given the role's novelty, it was also vital for RTA responsibilities to be iteratively refined with input from RTAs and physician partners.
An unexpected outcome has been the positive effect on the RTAs themselves. Whether the RTA is interested in matriculating to a graduate health degree program or is a hospital employee internally promoted to an RTA, the position has allowed for invaluable clinical exposure and more direct involvement with residents, patients, and families. The position has facilitated personal development and individual growth within and outside the typical pipeline of medicine.
One limitation to the RTA programs is that they may not be generalizable to all institutions, particularly smaller non-academic centers. The resident survey questions were not tested for validity evidence, so they may not have been interpreted as intended. In addition, other concurrent interventions underway may have been responsible in part for improvements in work hour adherence.
Aligned with the continued growth of the programs at our institutions, future directions include establishing an RTA curriculum that further fosters personal and professional development, generating additional quantitative data demonstrating program benefits, and expanding to other institutions.
Conclusions
The RTA programs implemented to support the trainees at our 3 institutions have positively impacted the administrative task burden and job satisfaction of the residents while maintaining high acceptability from the hospital staff, patients, families, and community pediatricians. They have been considerably feasible in terms of costs and effort by the institutions, a notion supported by their continued growth within each of the hospitals.
Supplementary Material
Footnotes
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The content of this article was previously presented at the Association for Pediatric Program Directors Annual Spring Meeting, New Orleans, Louisiana, March 29, 2019.
The authors would like to thank all past and current resident assistants/care team assistants for their hard work and dedication to the program; Dr. Evan Fieldston, Ms. Susan Kolb, Dr. Allison Ballantine, Dr. Lisa Zaoutis, Ms. Anna Markovich, Ms. Kelly Bowman, Ms. April Taylor, Ms. Claire Sanzone, Dr. Mary Bozynski Hernandez, and Dr. Hilary Haftel for their invaluable contributions.
Contributor Information
Ryosuke Takei, Attending Physician, Division of General Pediatrics, and Director, Care Team Assistant Program, Children's Hospital of Philadelphia; Assistant Professor of Clinical Pediatrics, Perelman School of Medicine, University of Pennsylvania.
George Dalembert, Attending Physician, Division of General Pediatrics, and Associate Program Director, Pediatric Residency Program, Children's Hospital of Philadelphia; Assistant Professor of Clinical Pediatrics, Perelman School of Medicine, University of Pennsylvania.
Jeanine Ronan, Attending Physician, Division of General Pediatrics, and Program Director, Pediatric Residency Program, Children's Hospital of Philadelphia; Associate Professor of Clinical Pediatrics, Perelman School of Medicine, University of Pennsylvania.
Nicole Washington, Attending Physician, Division of General Pediatrics, and Associate Program Director, Pediatric Residency Program, Children's Hospital of Philadelphia; Assistant Professor of Clinical Pediatrics, Perelman School of Medicine, University of Pennsylvania.
Stuti Tank, Supervising Care Team Assistant, Children's Hospital of Philadelphia.
Michael Perry, Attending Physician, Division of Hospital Pediatrics, and Director, Resident Assistant Program, Nationwide Children's Hospital; Assistant Professor of Clinical Pediatrics, The Ohio State University College of Medicine.
John D. Mahan, Attending Physician, Division of Pediatric Nephrology, and Director, Center for Faculty Development, Nationwide Children's Hospital; Professor of Pediatrics, The Ohio State University College of Medicine.
David A. Stewart, Attending Physician, Division of Pediatric Hospital Medicine, and Associate Program Director, Pediatric Residency Program, University of Michigan; Clinical Assistant Professor, Department of Pediatrics, University of Michigan Medical School.
Heather L. Burrows, Attending Physician, Division of General Pediatrics, and Program Director, Pediatric Residency Program, University of Michigan; Clinical Associate Professor, Department of Pediatrics, University of Michigan Medical School.
References
- 1.Philibert I, Friedmann P, Williams WT. ACGME Work Group on Resident Duty Hours. New requirements for resident duty hours. JAMA. 2002;288(9):1112–1114. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 2.Nasca TJ, Day SH, Amis ES; ACGME Duty Hour Task Force. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363(2):e3. doi: 10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 3.Henry J, Pylpchuck Y, Searcy T, Patel V. Adoption of electronic health record systems among US non-federal acute care hospitals: 2008–2015. ONC Data Brief. 2020 https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-ehr-adoption-2008-2015.php Accessed November 2.
- 4.Tipping MD, Forth VE, O'Leary KJ, Malkenson DM, Magill DB, Englert K, et al. Where did the day go?—A time-motion study of hospitalists. J Hosp Med. 2010;5(6):323–328. doi: 10.1002/jhm.790. [DOI] [PubMed] [Google Scholar]
- 5.Thorne SE, Bultz BD, Baile WF. SCRN Communication Team. Is there a cost to poor communication in cancer care?: A critical review of the literature. Psychooncology. 2005;14(10):875–884. doi: 10.1002/pon.947. [DOI] [PubMed] [Google Scholar]
- 6.Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: a review. Behav Sci (Basel) 2018;8(11):98. doi: 10.3390/bs8110098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mahan JD. Burnout in pediatric residents and physicians: a call to action. Pediatrics. 2017 doi: 10.1542/peds.2016-4233. 139(3)e20164233. [DOI] [PubMed]
- 8.Rao SK, Kimball AB, Lehrhoff SR, Hidrue MK, Colton DG, Ferris TG, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92(2):237–243. doi: 10.1097/ACM.0000000000001461. [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Hasan O, Dyrbye LN, Sinsky C, Satele D, Sloan J, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.