PURPOSE
We performed an open-label randomized controlled phase III study comparing treatment outcome and toxicity between radiotherapy (RT) with concomitant cisplatin versus concomitant cetuximab in patients with locoregionally advanced head and neck squamous cell carcinoma (HNSCC; stage III-IV according to the Union for International Cancer Control TNM classification, 7th edition).
MATERIALS AND METHODS
Eligible patients were randomly assigned 1:1 to receive either intravenous cetuximab 400 mg/m2 1 week before start of RT followed by 250 mg/m2/wk, or weekly intravenous cisplatin 40 mg/m2, during RT. RT was conventionally fractionated. Patients with T3-T4 tumors underwent a second random assignment 1:1 between standard RT dose 68.0 Gy to the primary tumor or dose escalation to 73.1 Gy. Primary end point was overall survival (OS) evaluated using adjusted Cox regression analysis. Secondary end points were locoregional control, local control with dose-escalated RT, pattern of failure, and adverse effects.
RESULTS
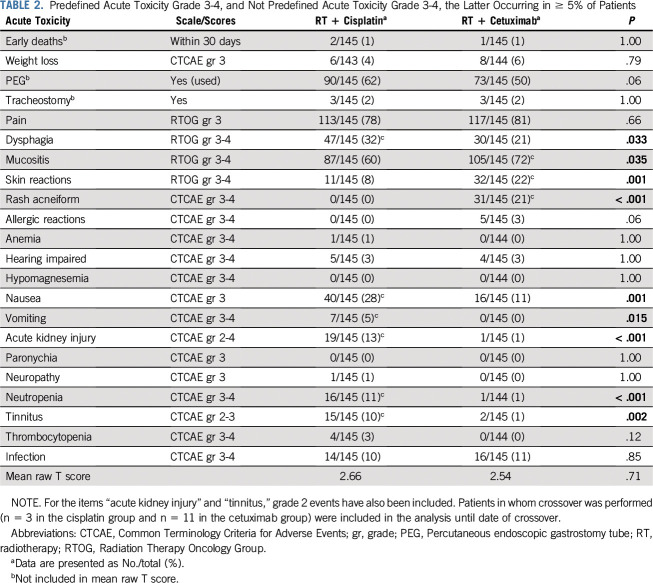
Study inclusion was prematurely closed after an unplanned interim analysis when 298 patients had been randomly assigned. At 3 years, OS was 88% (95% CI, 83% to 94%) and 78% (95% CI, 71% to 85%) in the cisplatin and cetuximab groups, respectively (adjusted hazard ratio, 1.63; 95% CI, 0.93 to 2.86; P = .086). The cumulative incidence of locoregional failures at 3 years was 23% (95% CI, 16% to 31%) compared with 9% (95% CI, 4% to 14%) in the cetuximab versus the cisplatin group (Gray’s test P = .0036). The cumulative incidence of distant failures did not differ between the treatment groups. Dose escalation in T3-T4 tumors did not increase local control.
CONCLUSION
Cetuximab is inferior to cisplatin regarding locoregional control for concomitant treatment with RT in patients with locoregionally advanced HNSCC. Additional studies are needed to identify possible subgroups that still may benefit from concomitant cetuximab treatment.
INTRODUCTION
Head and neck squamous cell cancer (HNSCC) is the seventh most common malignancy worldwide, with a global incidence of > 800,000 new cases annually.1 Treatment remains a challenge in patients with locoregionally advanced disease (stage III-IV according to the Union for International Cancer Control [UICC] TNM Classification of Malignant Tumors, 7th edition).2 Surgery combined with radiotherapy (RT) is the preferred treatment in locoregionally advanced oral cancer and a treatment option in cancers of the oropharynx, hypopharynx, and larynx. However, because of unresectable disease, and also because of an ambition to preserve affected organs and their function, definitive RT often remains the treatment of choice. Addition of concomitant cisplatin to RT improves outcome, with an absolute gain in overall survival (OS) of 6.5% at 5 years.3 Cisplatin administered intravenously at a dose of 100 mg/m2 every third week is the most established regimen, although several other schedules, mainly weekly low-dose regimens, have been reported.4-6
CONTEXT
Key Objective
To compare curative treatment with radiotherapy plus cisplatin versus radiotherapy plus cetuximab in patients with locoregionally advanced (stage III-IV according to the Union for International Cancer Control TNM classification, 7th edition) head and neck squamous cell carcinoma.
Knowledge Generated
The cumulative incidence of locoregional failures at 3 years was more than twice as high in the cetuximab group compared with the cisplatin group. Distant failures and overall survival did not differ. Toxicity burden, as estimated with the TAME method, was similar in the treatment groups.
Relevance
Our study supports that concurrent cisplatin should remain standard treatment of patients with locoregionally advanced head and neck squamous cell carcinoma.
In 2006, with an additional long-term follow-up in 2010, Bonner et al7,8 showed that RT combined with the epidermal growth factor receptor (EGFR) antibody cetuximab rendered an absolute benefit of 9.2% in OS at 5 years compared with RT alone (ie, similar to that of concomitant cisplatin). When the ARTSCAN III study was initiated in November 2013, these two treatment regimens had not been directly compared, and our study was undertaken to upfront compare outcome between RT and concomitant cisplatin with RT and concomitant cetuximab in a randomized controlled phase III trial.
Because of retrospective studies from comparable patient groups and settings indicating inferior disease control of RT plus cetuximab compared with RT plus cisplatin,9 an unplanned interim analysis was performed by the study’s independent safety data monitoring committee. Following their recommendation, patient inclusion was prematurely closed in March 2018. With a median follow-up of 3.2 years, we here report treatment outcome, pattern of failure, and acute and late treatment-related morbidity for treatment with RT plus cisplatin compared with RT plus cetuximab.
MATERIALS AND METHODS
Study Design
ARTSCAN III is an open-label randomized controlled phase III study conducted in Sweden with 11 participating centers. Patients were randomly assigned 1:1 between the treatment groups, and the randomization was stratified by study center, tumor site (oropharynx v nonoropharynx), T stage (1-2 v 3-4), and WHO/Eastern Cooperative Oncology Group (ECOG) performance status (0 v 1-2) using a minimization algorithm.10 Patients with T3-T4 tumors underwent a second random assignment 1:1 between standard radiation dose of 68.0 Gy and 73.1 Gy to the primary tumor.
Objectives
The primary objective of the study was to investigate OS in patients treated with RT plus cisplatin compared with RT plus cetuximab. Secondary objectives were to compare locoregional control, pattern of failure, acute and late adverse effects, and quality of life (QL) between the treatment groups and to study local control with dose-escalated RT compared with standard-dose RT in locally advanced (T3-T4) tumors.
Patients
Patients age ≥ 18 years with previously untreated squamous cell carcinoma of the oropharynx, hypopharynx, or larynx, stage III-IV according to UICC TNM classification, 7th edition, without distant metastases and aimed for curative treatment with definitive RT were eligible for inclusion. Patients with oral cavity cancer who had unresectable disease or were otherwise not amenable for surgery were also eligible. Performance status of 0-2 according to WHO/ECOG and adequate renal, bone marrow, and liver function were required. Patients with severe cardiac illness, previous malignancies, pre-existing hearing loss, or pre-existing peripheral neuropathy were excluded. In women of childbearing age, potential pregnancy had to be excluded before entering the study. All patients received oral and written information about the study and signed a written informed consent before study inclusion. For assessment of clinical tumor stage, all patients underwent a biopsy to confirm the diagnosis and a computed tomography (CT) scan of the head-neck and thorax regions. p16 analysis was mandatory and used as surrogate marker of human papillomavirus (HPV)-related disease. The study was approved by the regional ethical committee in Lund (2013/110) and registered at ClinicalTrials.gov (NCT01969877).
Treatment
Cisplatin was administered intravenously at a dose of 40 mg/m2, with a maximum dose of 70 mg, during the 7 weeks of RT. Cetuximab therapy started with an intravenous loading dose of 400 mg/m2 1 week before start of RT followed by seven weekly doses of 250 mg/m2.7 Criteria for dose reductions were prespecified in the Protocol (Data Supplement, online only). Prescribed RT doses were 68.0 Gy to the primary tumor and lymph node metastases and 54.4 Gy to elective neck volumes, given as daily fractions of 2.0 Gy and 1.6 Gy, respectively, 5 days per week. Patients with T3-T4 tumors underwent a second random assignment between either the standard radiation dose of 68.0 Gy and 73.1 Gy to the primary tumor, given as daily fractions of 2.15 Gy. Details regarding RT preparation, including target delineation instructions and dose-volume objectives and constraints, are described in the Data Supplement. All patients were treated with either intensity-modulated RT, volumetric arc therapy, or helical tomotherapy.
Assessment of adverse effects was made at baseline and weekly during RT with the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 4.0 and with selected items from the Radiation Therapy Oncology Group (RTOG) Acute Radiation Morbidity Scoring Criteria.11
Neck dissection after RT was allowed as part of the primary treatment and could be performed according to local routines at the participating hospitals either as an adjuvant procedure or because of remaining lymphadenopathy.
Follow-Up
Three months after treatment completion, assessment of response was performed by clinical examination and positron emission tomography–CT, CT, or magnetic resonance imaging, according to local routines at the treating hospital. Patients were then followed up every third month for 2 years, and thereafter every sixth month until 5 years. Acute adverse effects were assessed until 3 months after completion of radiotherapy. Late adverse effects were then monitored by CTCAE v4.0, and items from the RTOG Late Radiation Morbidity Scoring Criteria11 and the Late Effects Normal Tissue Task Force-Subjective, Objective, Management, Analytic scales12 at 6 and 12 months after completion of treatment, and then yearly until 5 years. QL was measured with the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (QLQ-C30, version 3.0) and Quality of Life Head and Neck module (QLQ-H&N35), MD Anderson Dysphagia Inventory, and Hospital Anxiety and Depression Scale at baseline and at 6, 12, and 24 months and 5 years after treatment; these results will be reported separately.
Statistical Analysis
The trial was designed as a superiority study that aimed to show a 10% absolute increase (from 50% to 60%) in OS at 5 years for concomitant cetuximab compared with concomitant cisplatin. Assuming exponential distributions, a significance level α = .05, and 80% power, 275 primary events were required. To reach this number of events, 618 patients needed to be randomly assigned.
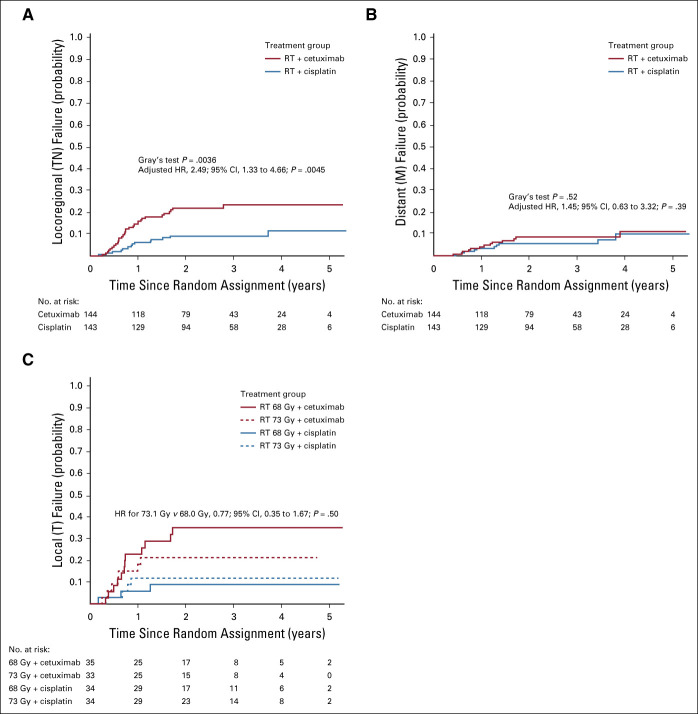
The intention-to-treat (ITT) population was used for efficacy analyses and contains all patients meeting eligibility criteria. Six patients included and randomly assigned in the study who were later found to be not eligible for inclusion and one patient who withdrew consent before start of treatment were not included in the ITT population (Fig 1). Crossover was not predefined in the Protocol but was performed in 14 patients, three in the cisplatin group and 11 in the cetuximab group. These patients were analyzed according to randomization for efficacy analyses but were only included in the analyses of adverse events until the date of crossover. Time to event was calculated from date of randomization in all analyses. Median follow-up time was calculated with the reverse Kaplan-Meier method. For the primary end point OS, and for event-free survival, the treatment groups were compared by means of a Cox proportional hazards model stratified for tumor site and adjusted for T stage/dose escalation and WHO/ECOG performance status. Proportional hazards assumptions were tested by Schoenfeld residuals tests. The Kaplan-Meier method was used to illustrate OS, and the log-rank test was used to compare treatment groups. Cumulative incidence functions for locoregional control with distant metastases and death as competing events were estimated and compared by means of Gray’s test. Cumulative incidence functions for distant metastases with locoregional progression and death as competing events were analyzed analogously. Cause-specific event rates were analyzed with adjusted Cox regression analyses. Dose escalation in T3-T4 tumors was evaluated by means of Cox regression analysis, stratified for treatment group. Adverse events were compared with Fisher’s exact test and with mean raw T scores (for acute adverse events) and mean raw A scores (for late adverse events) according to the TAME method.13 No corrections for multiple testing were applied.
FIG 1.
Trial profile. RT, radiotherapy.
RESULTS
Patients
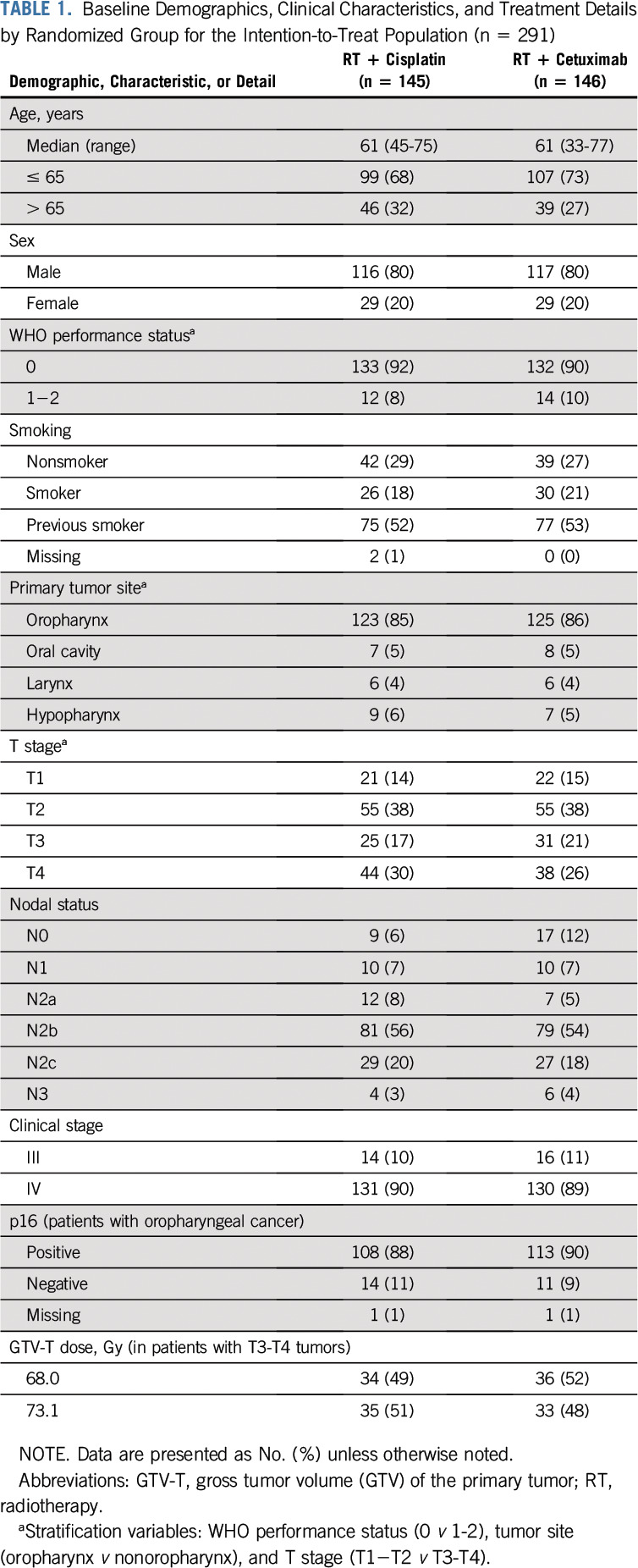
Between November 2013 and March 2018, 298 patients were recruited into the study, 149 in each treatment group. Seven patients were excluded before start of treatment, leaving 291 patients for the ITT analysis: 145 and 146 patients in the RT plus cisplatin and the RT plus cetuximab arms, respectively (Fig 1). Baseline characteristics of the patients were well balanced between the treatment groups (Table 1). Eighty-five percent of the patients had oropharyngeal cancer, of whom 221 patients (89%) were p16 positive. At the time of analysis, median follow-up was 38 months (interquartile range [IQR], 28-53 months) in the cisplatin group and 39 months (IQR, 30-54 months) in the cetuximab group.
TABLE 1.
Baseline Demographics, Clinical Characteristics, and Treatment Details by Randomized Group for the Intention-to-Treat Population (n = 291)
As described above, an unplanned interim analysis was performed in 2018. The recommendation to terminate patient inclusion was mainly based on a clear difference in locoregional events (12 v 28 for the cisplatin v cetuximab group). A conditional power analysis also yields a much-reduced power to show superiority for the cetuximab group.
Treatment Compliance
Of the patients completing RT (n = 289), 99% received 68.0 Gy or 73.1 Gy. One patient in the cetuximab group was excluded from the study during treatment after an anaphylactic reaction, and one patient in the cisplatin group died during treatment. Median total RT treatment time was 46 days in both treatment groups. Eighty-nine percent of the patients received RT per protocol or with acceptable deviations: 127 of 144 patients (88%) in the cisplatin group and 130 of 145 patients (90%) in the cetuximab group. Quality assurance criteria and protocol deviations are described in the Data Supplement.
Eight doses of cetuximab were administered in 98 of 145 patients (68%). One hundred twenty-six patients (87%) received at least seven doses, and the median dose was 2,087 mg/m2 (IQR, 1,896-2,150 mg/m2). The most common reasons for dose reduction were hypersensitivity reactions (n = 9) and rash and infection (n = 5 each). In the RT plus cisplatin group, dose reduction was performed in 63 of 144 patients (44%). The median cisplatin dose was 196 mg/m2 (IQR, 160-227 mg/m2). Dose reductions were mainly due to hematologic (n = 27) and renal (n = 19) toxicity.
Twenty patients underwent neck dissections as part of their primary treatment: nine in the RT plus cisplatin arm and 11 in the RT plus cetuximab arm.
Treatment Outcome
During the follow-up, 20 deaths occurred in the RT plus cisplatin group and 32 in the RT plus cetuximab group. Overall survival at 3 years was 88% (95% CI, 83% to 94%) and 78% (95% CI, 71% to 85%), respectively (log-rank P = .075; adjusted hazard ratio [HR], 1.63; 95% CI, 0.93 to 2.86; P = .086; Fig 2).
FIG 2.
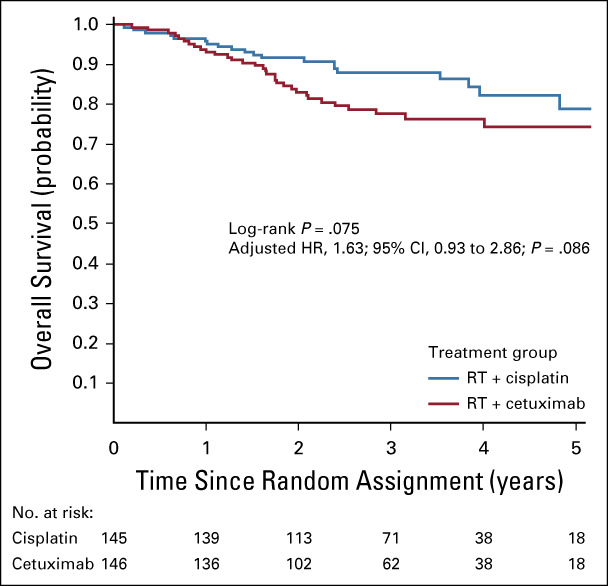
Overall survival in the intention-to-treat (ITT) population by treatment group. Adjusted hazard ratio (HR) is determined with Cox regression stratified for tumor site (oropharynx or nonoropharynx) and adjusted for T stage/dose escalation (T1-T2;T3-T4/68.0 Gy;73.1Gy) and WHO/Eastern Cooperative Oncology Group performance status (WHO 0;WHO 1-2).
Two hundred eighty-seven patients were eligible for tumor response evaluation (Fig 1). Sixty-one patients developed disease progression during the follow-up period: 20 in the cisplatin group and 41 in the cetuximab group. The cumulative incidence of locoregional failures at 3 years was more than twice as high in the cetuximab group: 23% (95% CI, 16% to 31%) compared with 9% (95% CI, 4% to 14%) in the cisplatin group (Gray’s test, P = .0036; adjusted cause-specific HR, 2.49; 95% CI, 1.33 to 4.66; P = .0045; Fig 3A). In contrast, the cumulative incidence of distant failures did not differ between the treatment groups. Distant failures had occurred in 6% (95% CI, 2% to 9%) and 9% (95% CI, 4% to 13%) at 3 years in the cisplatin and cetuximab groups, respectively (Gray’s test P = .52; adjusted cause-specific HR, 1.45; 95% CI, 0.63 to 3.32; P = .39; Fig 3B). Event-free survival at 3 years was 85% (95% CI, 79% to 91%) in the RT plus cisplatin group versus 67% (95% CI, 59% to 76%) in the RT plus cetuximab group, (log-rank P = .0054; adjusted HR, 1.99; 95% CI, 1.23 to 3.22; P = .0053). There was no significant difference in local control between patients who received dose escalation to 73.1 Gy to the primary tumor compared with patients treated with standard radiation dose 68.0 Gy (HR stratified by cisplatin/cetuximab group, 0.77; 95% CI, 0.35 to 1.67; P = .50; Fig 3C). The figure suggests an effect in the cetuximab group but not in the cisplatin group, but this difference is not supported by an interaction test (P = .41).
FIG 3.
Cumulative incidences of (A) locoregional failures and (B) distant failures by treatment group, and (C) cumulative incidence of local failures in T3-T4 tumors, with and without dose escalation. In C, the hazard ratio (HR) refers to the comparison of the two radiation dose groups, stratified for cisplatin/cetuximab. RT, radiotherapy.
Post hoc subgroup analyses of OS and locoregional control by treatment group are presented in the Data Supplement. HR for the end point OS was 5.70 (95% CI, 1.67 to 19.5; P for interaction = .03) for patients with p16-positive oropharyngeal cancer treated with RT plus cetuximab versus cisplatin. The corresponding figure for patients with p16-negative oropharyngeal cancer was 1.03 (95% CI, 0.36 to 3.00), and for patients with nonoropharyngeal cancer it was 1.02 (95% CI, 0.41 to 2.58; Data Supplement).
Toxicity
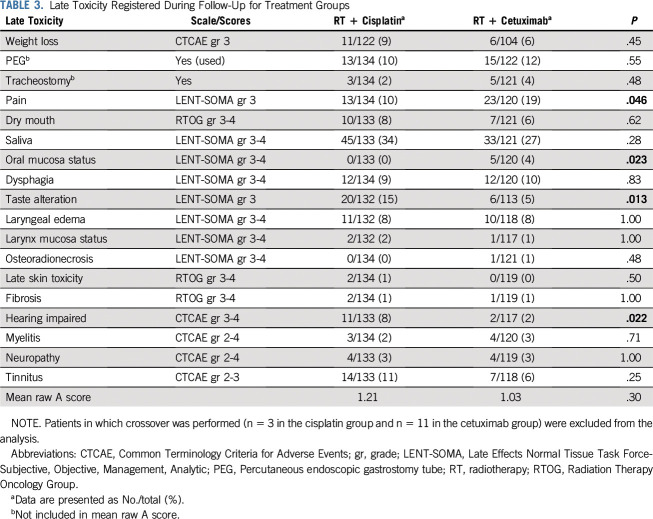
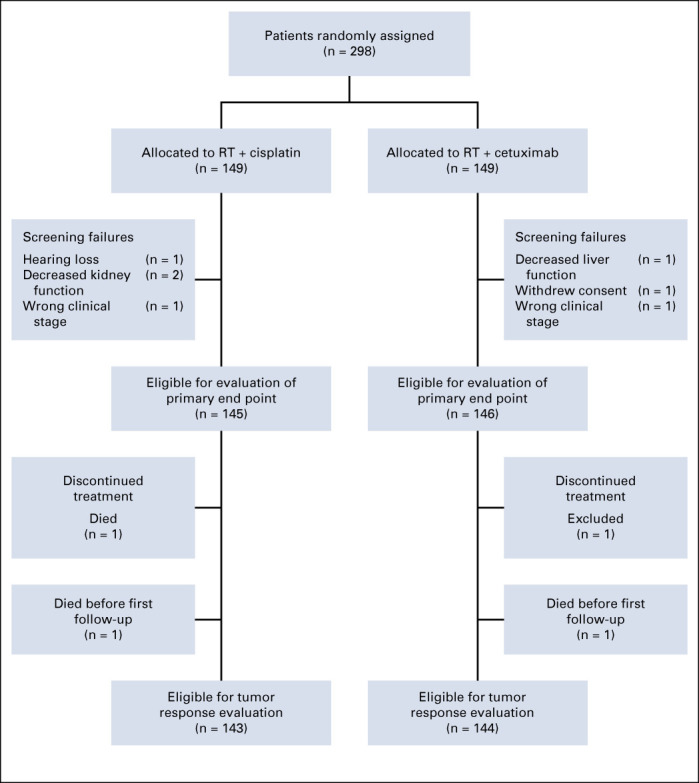
There were two early deaths (within 30 days after finished treatment) in the cisplatin group and one in the cetuximab group. Predefined acute and late adverse events grade 3-4 and not predefined adverse events grade 3-4, the latter occurring in at least 5% of the patients, are presented in Tables 2 and 3. As expected, acute toxicity profiles differed between the treatment groups, with significantly more events of nausea, vomiting, acute kidney injury, neutropenia, tinnitus, and dysphagia in patients treated with cisplatin, whereas patients treated with cetuximab had significantly more events of mucositis, skin reactions, and acneiform rashes. When estimated with the TAME method, acute toxicity did not differ significantly between the two treatment groups (P = .71). Regarding late adverse events, four items (pain, taste alteration, oral mucosa status, and hearing impairment) differed significantly between the treatment groups. However, there was no significant difference in mean raw A scores. There was no significant difference in late toxicity between patients with T3-T4 tumors randomly assigned between 68.0 Gy and 73.1 Gy (Data Supplement).
TABLE 2.
Predefined Acute Toxicity Grade 3-4, and Not Predefined Acute Toxicity Grade 3-4, the Latter Occurring in ≥ 5% of Patients
TABLE 3.
Late Toxicity Registered During Follow-Up for Treatment Groups
DISCUSSION
This study comparing RT plus cisplatin and RT plus cetuximab in patients with locally advanced HNSCC found significantly inferior locoregional control for patients treated with concurrent cetuximab. This finding is in agreement with recent studies of patients with HPV-positive locally advanced oropharyngeal cancer.14,15 Previous studies including both HPV-positive and HPV-negative patients have reported more divergent results,16-18 which may in part be caused by retrospective design, small patient cohorts, and older age and more comorbidities in patients receiving cetuximab.17,19,20 A meta-analysis of 1,808 patients from 15 different trials found superior treatment outcome for cisplatin compared with cetuximab regarding 2-year progression-free survival (PFS; risk ratio [RR], 0.68; 95% CI, 0.53 to 0.87; P = .002) and 2-year OS (RR, 0.66; 95% CI, 0.46 to 0.94; P = .02).21 The majority of the trials included in the meta-analysis did not report p16 or HPV status. In the TREMPLIN trial (ClinicalTrials.gov identifier: NCT00169247), a randomized phase II study in which patients with stage III-IV laryngeal or hypopharyngeal cancer after response to induction chemotherapy were randomly assigned between RT plus cisplatin and RT plus cetuximab, no differences were found in the primary end point larynx preservation at 3 months (95% v 93%) or in the secondary end points larynx function preservation (87% v 82%) and OS (92% v 89%) at 18 months.22
Patient inclusion in the ARTSCAN III study was prematurely terminated, and the primary end point OS did not reach statistical significance between the treatment groups in this first analysis of the study. In contrast, event-free survival, known to be strongly correlated with OS,23 was highly significant in favor of cisplatin treatment. Oropharynx was the predominant tumor subsite in our study, and the majority of the patients had p16-positive tumors. The main patient group investigated was thus similar to those of the RTOG 1016 (ClinicalTrials.gov identifier: NCT01302834) and the De-ESCALaTE (ClinicalTrials.gov identifier: NCT01874171) trials.14,15 Although with different study designs and primary end points, their findings were similar to our results; both studies found worse PFS and also OS for patients treated with cetuximab versus cisplatin. There is thus level I evidence speaking in favor of concurrent cisplatin compared with cetuximab for HPV-related oropharyngeal cancer, while the situation is less clear for remaining subgroups of patients with HNSCC. When combining the patients with p16-negative oropharyngeal cancer and nonoropharyngeal cancer in our study, this subgroup is too small (n = 68) to allow any outcome analysis. A recent retrospective analysis of treatment outcome in patients with HPV-negative oropharyngeal, laryngeal, and hypopharyngeal cancer showed inferior results for concurrent cetuximab compared with concurrent cisplatin or carboplatin,24 but evidence from randomized phase III studies is still lacking. Considering that EGFR overexpression is often found in HNSCC and constitutes a negative prognostic factor,25 and that cetuximab can enhance tumor response to RT in vitro26 as well as in a randomized clinical setting,7 it may still be possible that concurrent cetuximab can be at least an equal option compared with concurrent cisplatin for a subgroup of patients with HNSCC.
Patients with advanced stage T3-T4 primary tumors have a worse prognosis compared with lower T stages,27 and accelerated RT, resulting in a higher biologically effective dose, has been shown to be more beneficial in the treatment of more advanced tumors.28 The efficacy of dose escalation to 73.1 Gy to the primary tumor was a secondary objective of this study. The prematurely stopped inclusion in the trial prevents this analysis.
Regarding treatment intensity, 44% of the patients in the current study received reduced doses of cisplatin because of toxicity, whereas the corresponding figure in the cetuximab group was 32%. Many previous studies have reported that cisplatin, when administered at 100 mg/m2 every third week, causes hematologic, renal, and hearing toxicity and that dose reductions have been common.29,30 Consequently, lower weekly doses have been presented as an alternative31 and were used in our study. A cumulative cisplatin dose of 200 mg/m2 has often been regarded to be needed to obtain effect of the concurrent treatment.32 This dose was only achieved in 48% of our patients. In spite of this, there was a clear benefit in recurrence-free survival for concurrent cisplatin.
In early reports, cetuximab toxicity was reported to be lower compared with cisplatin.7 This finding has not been confirmed in later studies.14,15 The toxicity profiles differ between the study drugs, which makes the comparisons of their impact more delicate. However, by estimation with the TAME method, the toxicity burden of concurrent cetuximab appears to be similar to that of concurrent cisplatin in our study.
In summary, this randomized phase III study comparing concurrent cisplatin with concurrent cetuximab in patients with locally advanced HNSCC showed a significantly better locoregional control with concurrent cisplatin, which should remain the standard treatment for patients with p16-positive or p16-negative HNSCC.
ACKNOWLEDGMENT
We thank Harald Anderson, Department of Clinical Sciences Lund, Cancer Epidemiology, Lund University, Lund, Sweden and Oskar Hagberg, Department of Translational Medicine, Lund University, Malmö, Sweden for statistical advice.
Björn U. Zackrisson
Leadership: ScandiDos
No other potential conflicts of interest were reported.
SUPPORT
Supported by the Swedish Cancer Society and the Mrs. Berta Kamprad Cancer Foundation.
EQUAL CONTRIBUTION
B.Z. and P.N. contributed equally to this work.
CLINICAL TRIAL INFORMATION
See accompanying Oncology Grand Rounds on page 7
AUTHOR CONTRIBUTIONS
Conception and design: Maria Gebre-Medhin, Eva Brun, Hedda Haugen Cange, Lalle Hammarstedt-Nordenvall, Johan Reizenstein, Jan Nyman, Signe Friesland, Helena Sjödin, Karin Söderkvist, Björn Zackrisson, Per Nilsson
Administrative support: Signe Friesland, Karin Söderkvist
Provision of study material or patients: Maria Gebre-Medhin, Lalle Hammarstedt-Nordenvall, Jan Nyman, Edvard Abel, Signe Friesland, Helena Sjödin, Karin Söderkvist
Collection and assembly of data: Maria Gebre-Medhin, Eva Brun, Per Engström, Hedda Haugen Cange, Lalle Hammarstedt-Nordenvall, Johan Reizenstein, Jan Nyman, Edvard Abel, Signe Friesland, Helena Sjödin, Karin Söderkvist, Marcus Thomasson, Björn Zackrisson, Per Nilsson
Data analysis and interpretation: Maria Gebre-Medhin, Lalle Hammarstedt-Nordenvall, Henrik Carlsson, Björn Zackrisson, Per Nilsson
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
ARTSCAN III: A Randomized Phase III Study Comparing Chemoradiotherapy With Cisplatin Versus Cetuximab in Patients With Locoregionally Advanced Head and Neck Squamous Cell Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Björn U. Zackrisson
Leadership: ScandiDos
No other potential conflicts of interest were reported.
REFERENCES
- 1. Ferlay J, Ervik M, Lam F, et al (eds): Cancer Today (powered by GLOBOCAN 2018). Lyon, France, 2018. [Google Scholar]
- 2. Sobin LH, Gospodarowicz MK, Wittekind C (eds): International Union Against Cancer (UICC): TNM Classification of Malignant Tumours (ed 7). Oxford, Wiley-Blackwell, 2009. [Google Scholar]
- 3.Pignon JP le Maître A Maillard E, et al. : Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): An update on 93 randomised trials and 17,346 patients. Radiother Oncol 92:4-14, 2009 [DOI] [PubMed] [Google Scholar]
- 4.Ho KF, Swindell R, Brammer CV: Dose intensity comparison between weekly and 3-weekly Cisplatin delivered concurrently with radical radiotherapy for head and neck cancer: A retrospective comparison from New Cross Hospital, Wolverhampton, UK. Acta Oncol 47:1513-1518, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Lau H Brar S Hao D, et al. : Concomitant low-dose cisplatin and three-dimensional conformal radiotherapy for locally advanced squamous cell carcinoma of the head and neck: Analysis of survival and toxicity. Head Neck 28:189-196, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Rütten H Pop LA Janssens GO, et al. : Long-term outcome and morbidity after treatment with accelerated radiotherapy and weekly cisplatin for locally advanced head-and-neck cancer: Results of a multidisciplinary late morbidity clinic. Int J Radiat Oncol Biol Phys 81:923-929, 2011 [DOI] [PubMed] [Google Scholar]
- 7.Bonner JA Harari PM Giralt J, et al. : Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med 354:567-578, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Bonner JA Harari PM Giralt J, et al. : Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol 11:21-28, 2010 [DOI] [PubMed] [Google Scholar]
- 9. Barney C, Walston S, Zamora P, et al: Cetuximab versus platinum-based chemoradiation in locally advanced p16 positive oropharyngeal cancer. Presented at the ESTRO 36, Vienna, Austria, May 5-9, 2017. [Google Scholar]
- 10.Pocock SJ: Clinical Trials: A Practical Approach. New York, Wiley, 1983 [Google Scholar]
- 11.Cox JD, Stetz J, Pajak TF: Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 31:1341-1346, 1995 [DOI] [PubMed] [Google Scholar]
- 12. LENT SOMA scales for all anatomic sites. Int J Radiat Oncol Biol Phys 31:1049-1091, 1995. [DOI] [PubMed]
- 13.Trotti A Pajak TF Gwede CK, et al. : TAME: Development of a new method for summarising adverse events of cancer treatment by the Radiation Therapy Oncology Group. Lancet Oncol 8:613-624, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Gillison ML Trotti AM Harris J, et al. : Radiotherapy plus cetuximab or cisplatin in human papillomavirus-positive oropharyngeal cancer (NRG Oncology RTOG 1016): A randomised, multicentre, non-inferiority trial. Lancet 393:40-50, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehanna H Robinson M Hartley A, et al. : Radiotherapy plus cisplatin or cetuximab in low-risk human papillomavirus-positive oropharyngeal cancer (De-ESCALaTE HPV): An open-label randomised controlled phase 3 trial. Lancet 393:51-60, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caudell JJ Sawrie SM Spencer SA, et al. : Locoregionally advanced head and neck cancer treated with primary radiotherapy: A comparison of the addition of cetuximab or chemotherapy and the impact of protocol treatment. Int J Radiat Oncol Biol Phys 71:676-681, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Koutcher L Sherman E Fury M, et al. : Concurrent cisplatin and radiation versus cetuximab and radiation for locally advanced head-and-neck cancer. Int J Radiat Oncol Biol Phys 81:915-922, 2011 [DOI] [PubMed] [Google Scholar]
- 18.Strom TJ Trotti AM Kish J, et al. : Comparison of every 3 week cisplatin or weekly cetuximab with concurrent radiotherapy for locally advanced head and neck cancer. Oral Oncol 51:704-708, 2015 [DOI] [PubMed] [Google Scholar]
- 19.Levy A Blanchard P Bellefqih S, et al. : Concurrent use of cisplatin or cetuximab with definitive radiotherapy for locally advanced head and neck squamous cell carcinomas. Strahlenther Onkol 190:823-831, 2014 [DOI] [PubMed] [Google Scholar]
- 20.Tang C Chan C Jiang W, et al. : Concurrent cetuximab versus platinum-based chemoradiation for the definitive treatment of locoregionally advanced head and neck cancer. Head Neck 37:386-392, 2015 [DOI] [PubMed] [Google Scholar]
- 21.Petrelli F Coinu A Riboldi V, et al. : Concomitant platinum-based chemotherapy or cetuximab with radiotherapy for locally advanced head and neck cancer: A systematic review and meta-analysis of published studies. Oral Oncol 50:1041-1048, 2014 [DOI] [PubMed] [Google Scholar]
- 22.Lefebvre JL Pointreau Y Rolland F, et al. : Induction chemotherapy followed by either chemoradiotherapy or bioradiotherapy for larynx preservation: The TREMPLIN randomized phase II study. J Clin Oncol 31:853-859, 2013 [DOI] [PubMed] [Google Scholar]
- 23.Michiels S Le Maître A Buyse M, et al. : Surrogate endpoints for overall survival in locally advanced head and neck cancer: Meta-analyses of individual patient data. Lancet Oncol 10:341-350, 2009 [DOI] [PubMed] [Google Scholar]
- 24.Beckham TH Barney C Healy E, et al. : Platinum-based regimens versus cetuximab in definitive chemoradiation for human papillomavirus-unrelated head and neck cancer. Int J Cancer 147:107-115, 2020 [DOI] [PubMed] [Google Scholar]
- 25.Ang KK Berkey BA Tu X, et al. : Impact of epidermal growth factor receptor expression on survival and pattern of relapse in patients with advanced head and neck carcinoma. Cancer Res 62:7350-7356, 2002 [PubMed] [Google Scholar]
- 26.Milas L Mason K Hunter N, et al. : In vivo enhancement of tumor radioresponse by C225 antiepidermal growth factor receptor antibody. Clin Cancer Res 6:701-708, 2000 [PubMed] [Google Scholar]
- 27.Lok BH Setton J Caria N, et al. : Intensity-modulated radiation therapy in oropharyngeal carcinoma: Effect of tumor volume on clinical outcomes. Int J Radiat Oncol Biol Phys 82:1851-1857, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horiot JC Bontemps P van den Bogaert W, et al. : Accelerated fractionation (AF) compared to conventional fractionation (CF) improves loco-regional control in the radiotherapy of advanced head and neck cancers: Results of the EORTC 22851 randomized trial. Radiother Oncol 44:111-121, 1997 [DOI] [PubMed] [Google Scholar]
- 29.Adelstein DJ Li Y Adams GL, et al. : An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol 21:92-98, 2003 [DOI] [PubMed] [Google Scholar]
- 30.Bernier J Domenge C Ozsahin M, et al. : Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med 350:1945-1952, 2004 [DOI] [PubMed] [Google Scholar]
- 31.Beckmann GK Hoppe F Pfreundner L, et al. : Hyperfractionated accelerated radiotherapy in combination with weekly cisplatin for locally advanced head and neck cancer. Head Neck 27:36-43, 2005 [DOI] [PubMed] [Google Scholar]
- 32.Ang KK: Concurrent radiation chemotherapy for locally advanced head and neck carcinoma: Are we addressing burning subjects? J Clin Oncol 22:4657-4659, 2004 [DOI] [PubMed] [Google Scholar]